The Impact of Probiotics and Prebiotics on Dry Eye Disease Signs and Symptoms
Abstract
:1. Introduction
2. Materials and Methods
3. Results
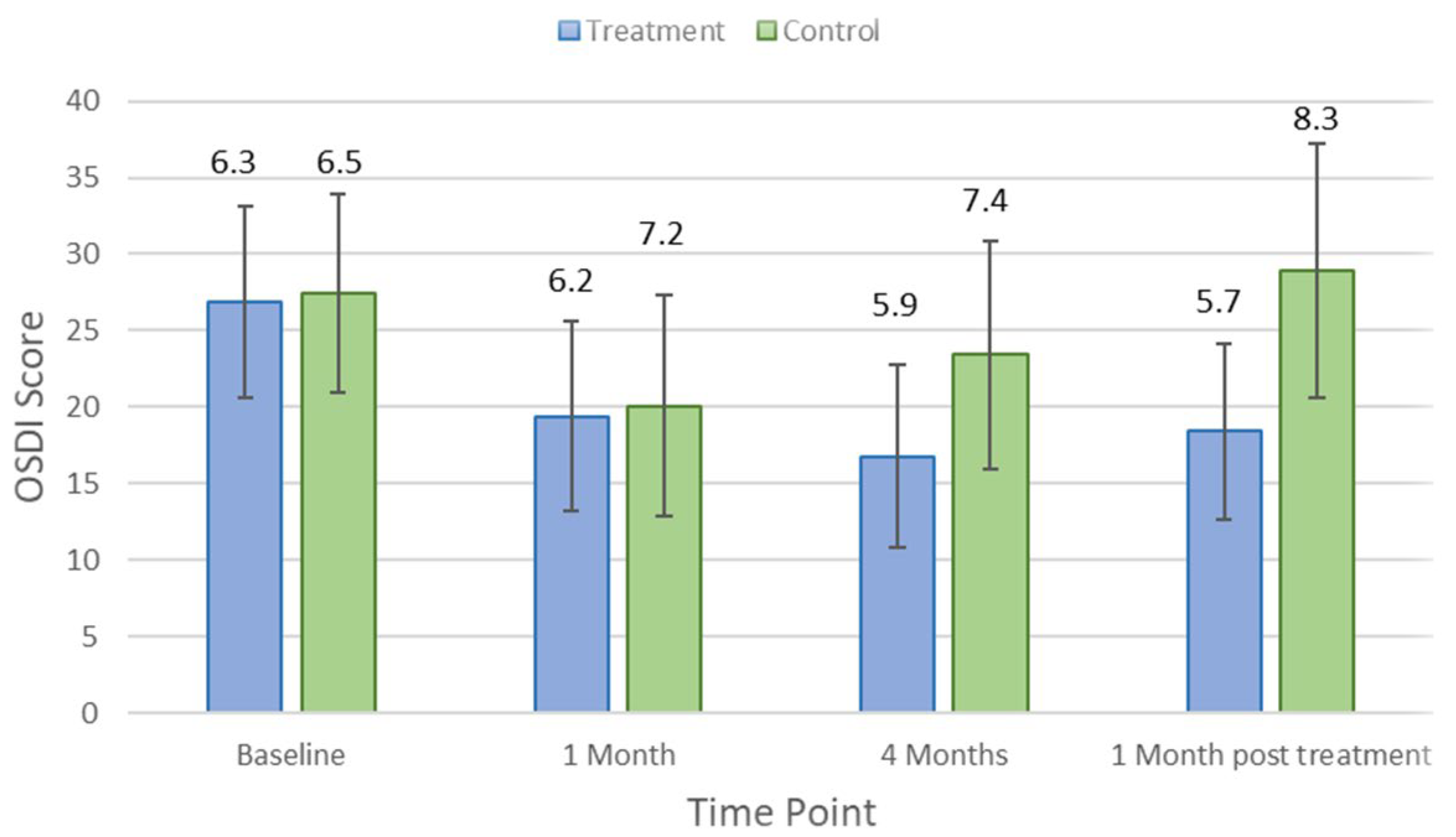
3.1. Dry Eye Symptoms
3.2. Dry Eye Signs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Papas, E.B. The global prevalence of dry eye disease: A Bayesian view. Ophthalmic Physiol. Opt. 2021, 41, 1254–1266. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.-K.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K.; et al. TFOS DEWS II Definition and Classification Report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, F.; Alves, M.; Bunya, V.Y.; Jalbert, I.; Lekhanont, K.; Malet, F.; Na, K.-S.; Schaumberg, D.; Uchino, M.; Vehof, J.; et al. TFOS DEWS II epidemiology report. Ocul. Surf. 2017, 15, 334–365. [Google Scholar] [CrossRef]
- Willcox, M.D.; Argüeso, P.; Georgiev, G.A.; Holopainen, J.M.; Laurie, G.W.; Millar, T.J.; Papas, E.B.; Rolland, J.P.; Schmidt, T.A.; Stahl, U.; et al. TFOS DEWS II Tear Film Report. Ocul. Surf. 2017, 15, 366–403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogawa, Y.; Perez, V.; Uchino, Y.; Yokoi, N.; Zoukhri, D.; Sullivan, D.A. TFOS DEWS II pathophysiology report. Ocul. Surf. 2017, 15, 438–510. [Google Scholar] [CrossRef]
- Messmer, E.M. The Pathophysiology, Diagnosis, and Treatment of Dry Eye Disease. Dtsch. Ärzteblatt Int. 2015, 112, 71–82. [Google Scholar] [CrossRef] [Green Version]
- Stern, M.E.; Schaumburg, C.S.; Pflugfelder, S.C. Dry Eye as a Mucosal Autoimmune Disease. Int. Rev. Immunol. 2013, 32, 19–41. [Google Scholar] [CrossRef]
- Guzmán, M.; Keitelman, I.; Sabbione, F.; Trevani, A.S.; Giordano, M.N.; Galletti, J.G. Desiccating stress-induced disruption of ocular surface immune tolerance drives dry eye disease. Clin. Exp. Immunol. 2016, 184, 248–256. [Google Scholar] [CrossRef] [Green Version]
- Floyd, J.L.; Grant, M.B. The Gut–Eye Axis: Lessons Learned from Murine Models. Ophthalmol. Ther. 2020, 9, 499–513. [Google Scholar] [CrossRef]
- Mendez, R.; Watane, A.; Farhangi, M.; Cavuoto, K.M.; Leith, T.; Budree, S.; Galor, A.; Banerjee, S. Gut microbial dysbiosis in individuals with Sjögren’s disease. bioRxiv 2019. [Google Scholar] [CrossRef]
- Mandl, T.; Marsal, J.; Olsson, P.; Ohlsson, B.; Andréasson, K. Severe intestinal dysbiosis is prevalent in primary Sjögren’s syndrome and is associated with systemic disease activity. Arthritis Res. Ther. 2017, 19, 237. [Google Scholar] [CrossRef] [PubMed]
- Tsigalou, C.; Stavropoulou, E.; Bezirtzoglou, E. Current Insights in Microbiome Shifts in Sjogren’s Syndrome and Possible Therapeutic Interventions. Front. Immunol. 2018, 9, 1106. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.; Choi, S.H.; Yoon, C.H.; Kim, M.K. Gut dysbiosis is prevailing in Sjögren’s syndrome and is related to dry eye severity. PLoS ONE 2020, 15, e0229029. [Google Scholar] [CrossRef]
- De Paiva, C.S.; Jones, D.B.; Stern, M.E.; Bian, F.; Moore, Q.L.; Corbiere, S.; Streckfus, C.F.; Hutchinson, D.S.; Ajami, N.J.; Petrosino, J.F.; et al. Altered Mucosal Microbiome Diversity and Disease Severity in Sjögren Syndrome. Sci. Rep. 2016, 6, 23561. [Google Scholar] [CrossRef] [PubMed]
- Baqai, A.F.; Fishman, H. Dry Eye Disease Associated with Lower Gut Microbiome Diversity. Investig. Ophthalmol. Vis. Sci. 2019, 60, 2760. [Google Scholar]
- Moon, J.; Yoon, C.H.; Choi, S.H.; Kim, M.K. Can Gut Microbiota Affect Dry Eye Syndrome? Int. J. Mol. Sci. 2020, 21, 8443. [Google Scholar] [CrossRef]
- Chisari, G.; Rampello, L.; Chisari, E.M.; Catania, V.E.; Greco, C.; Stagni, E.; Chisari, C.G. Microbiology synergism between tear substitutes and symbiotic treatment of patients with irritable bowel syndrome. Acta Med. Mediterr. 2016, 32, 865. [Google Scholar] [CrossRef]
- Chisari, G.; Chisari, E.; Francaviglia, A.; Chisari, C. The mixture of bifidobacterium associated with fructo- oligosaccharides reduces the damage of the ocular surface. Clin. Ter. 2017, 168, 181–185. [Google Scholar] [CrossRef]
- Kawashima, M.; Nakamura, S.; Izuta, Y.; Inoue, S.; Tsubota, K. Dietary Supplementation with a Combination of Lactoferrin, Fish Oil, and Enterococcus faecium WB2000 for Treating Dry Eye: A Rat Model and Human Clinical Study. Ocul. Surf. 2016, 14, 255–263. [Google Scholar] [CrossRef]
- Wolffsohn, J.S.; Arita, R.; Chalmers, R.; Djalilian, A.; Dogru, M.; Dumbleton, K.; Gupta, P.K.; Karpecki, P.; Lazreg, S.; Pult, H.; et al. TFOS DEWS II Diagnostic Methodology report. Ocul. Surf. 2017, 15, 539–574. [Google Scholar] [CrossRef]
- Gamage, H.K.; Tetu, S.G.; Chong, R.W.W.; Bucio-Noble, D.; Rosewarne, C.P.; Kautto, L.; Ball, M.S.; Molloy, M.P.; Packer, N.H.; Paulsen, I.T. Fiber Supplements Derived from Sugarcane Stem, Wheat Dextrin and Psyllium Husk Have Different In Vitro Effects on the Human Gut Microbiota. Front. Microbiol. 2018, 9, 1618. [Google Scholar] [CrossRef] [PubMed]
- Palacios, T.; Vitetta, L.; Coulson, S.; Madigan, C.D.; Denyer, G.S.; Caterson, I.D. The effect of a novel probiotic on metabolic biomarkers in adults with prediabetes and recently diagnosed type 2 diabetes mellitus: Study protocol for a randomized controlled trial. Trials 2017, 18, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rose-Nussbaumer, J.; Lietman, T.M.; Shiboski, C.H.; Shiboski, S.C.; Bunya, V.Y.; Akpek, E.K.; Srinivasan, M.; Mascarenhas, J.; Massaro-Giordano, G.; McNamara, N.A.; et al. Inter-grader Agreement of the Ocular Staining Score in the Sjögren’s International Clinical Collaborative Alliance (SICCA) Registry. Am. J. Ophthalmol. 2015, 160, 1150–1153.e3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamamoto, Y.; Shiraishi, A.; Sakane, Y.; Ohta, K.; Yamaguchi, M.; Ohashi, Y. Involvement of Eyelid Pressure in Lid-Wiper Epitheliopathy. Curr. Eye Res. 2016, 41, 171–178. [Google Scholar] [CrossRef]
- PEN. I-PEN Osmolarity System User Manual. Dollard Des Ormeaux QI-MPI. 2017. Available online: https://imedpharma.com/wp-content/uploads/2018/08/I-PEN_0718_UserManual_8.5x5.5_EN.pdf (accessed on 20 June 2022).
- Tavakoli, A.; Markoulli, M.; Flanagan, J.; Papas, E. The validity of point of care tear film osmometers in the diagnosis of dry eye. Ophthalmic Physiol. Opt. 2022, 42, 140–148. [Google Scholar] [CrossRef]
- Papas, E.B. Key factors in the subjective and objective assessment of conjunctival erythema. Investig. Ophthalmol. Vis. Sci. 2000, 41, 687–691. [Google Scholar]
- Fieguth, P.; Simpson, T. Automated measurement of bulbar redness. Investig. Ophthalmol. Vis. Sci. 2002, 43, 340–347. [Google Scholar]
- Amparo, F.; Wang, H.; Emami-Naeini, P.; Karimian, P.; Dana, R. The Ocular Redness Index: A Novel Automated Method for Measuring Ocular Injection. Investig. Ophthalmol. Vis. Sci. 2013, 54, 4821–4826. [Google Scholar] [CrossRef] [Green Version]
- Choi, S.H.; Oh, J.W.; Ryu, J.S.; Kim, H.M.; Im, S.-H.; Kim, K.P.; Kim, M.K. IRT5 Probiotics Changes Immune Modulatory Protein Expression in the Extraorbital Lacrimal Glands of an Autoimmune Dry Eye Mouse Model. Investig. Ophthalmol. Vis. Sci. 2020, 61, 42. [Google Scholar] [CrossRef] [Green Version]
- Boccardo, L. Self-reported symptoms of mask-associated dry eye: A survey study of 3605 people. Contact Lens Anterior Eye 2022, 45, 101408. [Google Scholar] [CrossRef]
- Krolo, I.; Blazeka, M.; Merdzo, I.; Vrtar, I.; Sabol, I.; Vickovic, I. Mask-Associated Dry Eye During COVID-19 Pandemic-How Face Masks Contribute to Dry Eye Disease Symptoms. Med Arch. 2021, 75, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Fan, Q.; Liang, M.; Kong, W.; Zhang, W.; Wang, H.; Chu, J.; Fang, X.; Song, Y.; Gao, W.; Wang, Y. Wearing face masks and possibility for dry eye during the COVID-19 pandemic. Sci. Rep. 2022, 12, 6214. [Google Scholar] [CrossRef] [PubMed]
- Aksoy, M.; Simsek, M. Evaluation of Ocular Surface and Dry Eye Symptoms in Face Mask Users. Eye Contact Lens 2021, 47, 555–558. [Google Scholar] [CrossRef]
- Akkaya, S.; Atakan, T.; Acikalin, B.; Aksoy, S.; Ozkurt, Y. Effects of long-term computer use on eye dryness. North. Clin. Istanb. 2018, 5, 319. [Google Scholar] [CrossRef] [PubMed]
- Colagiuri, B.; Schenk, L.A.; Kessler, M.D.; Dorsey, S.G.; Colloca, L. The placebo effect: From concepts to genes. Neuroscience 2015, 307, 171–190. [Google Scholar] [CrossRef] [Green Version]
- van der Meulen, T.A.; Harmsen, H.J.; Vila, A.V.; Kurilshikov, A.; Liefers, S.C.; Zhernakova, A.; Fu, J.; Wijmenga, C.; Weersma, R.K.; de Leeuw, K.; et al. Shared gut, but distinct oral microbiota composition in primary Sjögren’s syndrome and systemic lupus erythematosus. J. Autoimmun. 2019, 97, 77–87. [Google Scholar] [CrossRef]
- MacGregor, G.; Smith, A.J.; Thakker, B.; Kinsella, J. Yoghurt biotherapy: Contraindicated in immunosuppressed patients? Postgrad. Med. J. 2002, 78, 366–367. [Google Scholar] [CrossRef]
- Shivaji, S. Connect between gut microbiome and diseases of the human eye. J. Biosci. 2019, 44, 110. [Google Scholar] [CrossRef]
- Lin, P. The role of the intestinal microbiome in ocular inflammatory disease. Curr. Opin. Ophthalmol. 2018, 29, 261–266. [Google Scholar] [CrossRef]


| Variable | Baseline | 1st Month | 4th Month | 1 Month Post Treatment | ||||
|---|---|---|---|---|---|---|---|---|
| Control | Treatment | Control | Treatment | Control | Treatment | Control | Treatment | |
| OSDI (0–100) | 27.4 ± 14.0 | 26.9 ± 15.3 | 20.1 ± 14.7, 0.02 | 19.4 ± 14.5, 0.03 | 23.4 ± 13.7, 0.05 | 16.8 ± 13.2, 0.01 | 28.9 ± 12.7, 0.03 | 18.4 ± 12.7, 0.22 |
| DEQ-5 (0–22) | 10.2 ± 3.1 | 11.0 ± 3.4 | 8.8 ± 3.1, 0.03 | 9.7 ± 3.7,0.08 | 9.6 ± 3.3, 0.40 | 8.8 ± 4.1, 0.06 | 8.7 ± 3.2, 0.41 | 10.1 ± 3.4, 0.35 |
| LLT (nm) | 57.4 ± 17.2 | 72.6 ± 21.8 | 48.9 ± 15.9, 0.04 | 67.2 ± 23.3, 0.18 | 60.3 ± 23.4, 0.40 | 70.3 ± 18.9, 0.80 | 55.7 ± 17.4, 0.22 | 71.8 ± 22.6, 0.89 |
| TMH (mm) | 0.3 ± 0.1 | 0.2 ± 0.1 | 0.3 ± 0.1,0.60 | 0.2 ± 0.1,0.30 | 0.2 ± 0.1, 0.02 | 0.2 ± 0.1, 0.84 | 0.3 ± 0.1, 0.60 | 0.3 ± 0.1, 0.75 |
| NIKBUT (s) | 6.7 ± 3.3 | 8.4 ± 4.2 | 5.8 ± 2.9, 0.20 | 8.6 ± 3.9,0.90 | 5.5 ± 2.7, 0.03 | 9.1 ± 5.0, 0.30 | 6.8 ± 2.7, 0.67 | 8.4 ± 4.2, 0.44 |
| TO (mOsm/l) | 298.9 ± 19.8 | 299.7 ± 14.6 | 301.4 ± 14.8, 0.60 | 301.4 ± 3.6, 0.63 | 304.3 ± 16.5, 0.22 | 301.8 ± 14.5, 0.51 | 309.1 ± 12.1, 0.60 | 297.8 ± 14.0, 0.75 |
| CCS | 0.7 ± 1.1 | 0.9 ± 0.8 | 0.9 ± 1.2, 0.50 | 0.8 ± 0.9, 0.80 | 0.7 ± 0.8, 0.94 | 0.8 ± 0.9, 0.85 | 0.6 ± 0.7, 0.60 | 0.8 ± 0.9, 0.76 |
| LS | 0.8 ± 1.0 | 0.7 ± 0.9 | 1.0 ± 1.0, 0.60 | 0.6 ± 0.8, 0.90 | 0.8 ± 0.7, 0.56 | 0.6 ± 0.9, 0.76 | 0.8 ± 0.9, 0.45 | 0.8 ± 0.9, 0.37 |
| BR (mm2) | 0.9 ± 0.5 | 1.0 ± 0.5 | 0.9 ± 0.6, 0.80 | 0.9 ± 0.5, 0.14 | 0.9 ± 0.6, 0.40 | 0.9 ± 0.4, 0.91 | 1.0 ± 0.5, 0.10 | 1.0 ± 0.5, 0.11 |
| MGS | 2.7 ± 0.8 | 2.4 ± 1.1 | 2.9 ± 0.3, 0.13 | 2.6 ± 0.8, 0.32 | 2.8 ± 0.7, 0.98 | 2.5 ± 1.0, 0.56 | 2.8 ± 0.4, 0.40 | 2.3 ± 1.0, 0.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tavakoli, A.; Markoulli, M.; Papas, E.; Flanagan, J. The Impact of Probiotics and Prebiotics on Dry Eye Disease Signs and Symptoms. J. Clin. Med. 2022, 11, 4889. https://doi.org/10.3390/jcm11164889
Tavakoli A, Markoulli M, Papas E, Flanagan J. The Impact of Probiotics and Prebiotics on Dry Eye Disease Signs and Symptoms. Journal of Clinical Medicine. 2022; 11(16):4889. https://doi.org/10.3390/jcm11164889
Chicago/Turabian StyleTavakoli, Azadeh, Maria Markoulli, Eric Papas, and Judith Flanagan. 2022. "The Impact of Probiotics and Prebiotics on Dry Eye Disease Signs and Symptoms" Journal of Clinical Medicine 11, no. 16: 4889. https://doi.org/10.3390/jcm11164889
APA StyleTavakoli, A., Markoulli, M., Papas, E., & Flanagan, J. (2022). The Impact of Probiotics and Prebiotics on Dry Eye Disease Signs and Symptoms. Journal of Clinical Medicine, 11(16), 4889. https://doi.org/10.3390/jcm11164889





