Lumbosacral Transitional Vertebrae Influence on Acetabular Orientation and Pelvic Tilt
Abstract
:1. Introduction
2. Materials and Methods
2.1. Image Assessment
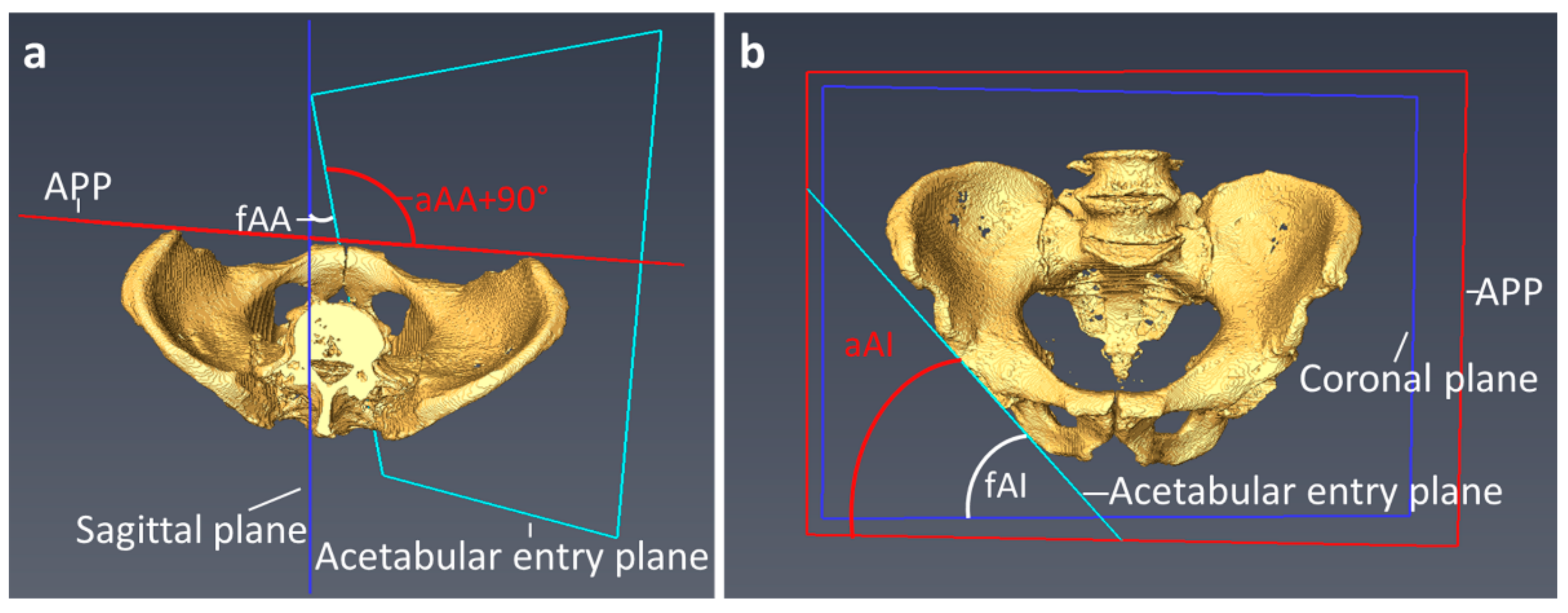
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Demographics
3.2. Influence of the Pelvic Tilt on the Acetabular Orientation in the Entire Cohort
3.3. Influence of Pelvic Incidence on Acetabular Orientation
3.4. Influence of LSTV on Acetabular Orientation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Matson, D.M.; Maccormick, L.M.; Sembrano, J.N.; Polly, D.W. Sacral Dysmorphism and Lumbosacral Transitional Vertebrae (LSTV) Review. Int. J. Spine Surg. 2020, 14, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Konin, G.P.; Walz, D.M. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. AJNR Am. J. Neuroradiol. 2010, 31, 1778–1786. [Google Scholar] [CrossRef]
- Apazidis, A.; Ricart, P.A.; Diefenbach, C.M.; Spivak, J.M. The prevalence of transitional vertebrae in the lumbar spine. Spine J. 2011, 11, 858–862. [Google Scholar] [CrossRef]
- Castellvi, A.E.; Goldstein, L.A.; Chan, D.P. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine 1984, 9, 493–495. [Google Scholar] [CrossRef] [PubMed]
- Tini, P.G.; Wieser, C.; Zinn, W.M. The transitional vertebra of the lumbosacral spine: Its radiological classification, incidence, prevalence, and clinical significance. Rheumatol. Rehabil. 1977, 16, 180–185. [Google Scholar] [CrossRef]
- Haffer, H.; Becker, L.; Putzier, M.; Wietholter, M.; Ziegeler, K.; Diekhoff, T.; Pumberger, M.; Hardt, S. Changes of Fixed Anatomical Spinopelvic Parameter in Patients with Lumbosacral Transitional Vertebrae: A Matched Pair Analysis. Diagnostics 2021, 11, 59. [Google Scholar] [CrossRef]
- Becker, L.; Adl Amini, D.; Ziegeler, K.; Muellner, M.; Diekhoff, T.; Hughes, A.P.; Pumberger, M. Approach-related anatomical differences in patients with lumbo-sacral transitional vertebrae undergoing lumbar fusion surgery at level L4/5. Arch. Orthop. Trauma Surg. 2022. [CrossRef]
- Price, R.; Okamoto, M.; Le Huec, J.C.; Hasegawa, K. Normative spino-pelvic parameters in patients with the lumbarization of S1 compared to a normal asymptomatic population. Eur. Spine J. 2016, 25, 3694–3698. [Google Scholar] [CrossRef]
- Yokoyama, K.; Kawanishi, M.; Yamada, M.; Tanaka, H.; Ito, Y.; Kawabata, S.; Kuroiwa, T. Spinopelvic alignment and sagittal balance of asymptomatic adults with 6 lumbar vertebrae. Eur. Spine J. 2016, 25, 3583–3588. [Google Scholar] [CrossRef]
- Abola, M.V.; Teplensky, J.R.; Cooperman, D.R.; Bauer, J.M.; Liu, R.W. Pelvic Incidence in Spines With 4 and 6 Lumbar Vertebrae. Glob. Spine J. 2019, 9, 708–712. [Google Scholar] [CrossRef] [Green Version]
- Schwab, F.; Ungar, B.; Blondel, B.; Buchowski, J.; Coe, J.; Deinlein, D.; DeWald, C.; Mehdian, H.; Shaffrey, C.; Tribus, C.; et al. Scoliosis Research Society-Schwab adult spinal deformity classification: A validation study. Spine 2012, 37, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Legaye, J.; Duval-Beaupere, G.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Radcliff, K.E.; Kepler, C.K.; Hellman, M.; Restrepo, C.; Jung, K.A.; Vaccaro, A.R.; Albert, T.J.; Parvizi, J. Does spinal alignment influence acetabular orientation: A study of spinopelvic variables and sagittal acetabular version. Orthop. Surg. 2014, 6, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Murray, D.W. The definition and measurement of acetabular orientation. J. Bone Jt. Surg. Br. 1993, 75, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Biedermann, R.; Tonin, A.; Krismer, M.; Rachbauer, F.; Eibl, G.; Stockl, B. Reducing the risk of dislocation after total hip arthroplasty: The effect of orientation of the acetabular component. J. Bone Jt. Surg. Br. 2005, 87, 762–769. [Google Scholar] [CrossRef]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Zahn, R.K.; Grotjohann, S.; Pumberger, M.; Ramm, H.; Zachow, S.; Putzier, M.; Perka, C.; Tohtz, S. Influence of pelvic tilt on functional acetabular orientation. Technol. Health Care 2017, 25, 557–565. [Google Scholar] [CrossRef]
- Ross, J.R.; Tannenbaum, E.P.; Nepple, J.J.; Kelly, B.T.; Larson, C.M.; Bedi, A. Functional acetabular orientation varies between supine and standing radiographs: Implications for treatment of femoroacetabular impingement. Clin. Orthop. Relat. Res. 2015, 473, 1267–1273. [Google Scholar] [CrossRef]
- Zhu, J.; Wan, Z.; Dorr, L.D. Quantification of pelvic tilt in total hip arthroplasty. Clin. Orthop. Relat. Res. 2010, 468, 571–575. [Google Scholar] [CrossRef]
- Higgins, S.W.; Spratley, E.M.; Boe, R.A.; Hayes, C.W.; Jiranek, W.A.; Wayne, J.S. A novel approach for determining three-dimensional acetabular orientation: Results from two hundred subjects. J. Bone Jt. Surg. Am. 2014, 96, 1776–1784. [Google Scholar] [CrossRef]
- Lee, C.; Jang, J.; Kim, H.W.; Kim, Y.S.; Kim, Y. Three-dimensional analysis of acetabular orientation using a semi-automated algorithm. Comput. Assist. Surg. 2019, 24, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Merle, C.; Grammatopoulos, G.; Waldstein, W.; Pegg, E.; Pandit, H.; Aldinger, P.R.; Gill, H.S.; Murray, D.W. Comparison of native anatomy with recommended safe component orientation in total hip arthroplasty for primary osteoarthritis. J. Bone Jt. Surg. Am. 2013, 95, e172. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.I.; Gladnick, B.P.; Lee, Y.Y.; Lyman, S.; Wright, T.M.; Mayman, D.J.; Padgett, D.E. Cup position alone does not predict risk of dislocation after hip arthroplasty. J. Arthroplast. 2015, 30, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Hevesi, M.; Wyles, C.C.; Rouzrokh, P.; Erickson, B.J.; Maradit-Kremers, H.; Lewallen, D.G.; Taunton, M.J.; Trousdale, R.T.; Berry, D.J. Redefining the 3D Topography of the Acetabular Safe Zone: A Multivariable Study Evaluating Prosthetic Hip Stability. J. Bone Jt. Surg. Am. 2021, 104, 239–245. [Google Scholar] [CrossRef]
- Tezuka, T.; Heckmann, N.D.; Bodner, R.J.; Dorr, L.D. Functional Safe Zone Is Superior to the Lewinnek Safe Zone for Total Hip Arthroplasty: Why the Lewinnek Safe Zone is not Always Predictive of Stability. J. Arthroplast. 2019, 34, 3–8. [Google Scholar] [CrossRef]
- Dandachli, W.; Ul Islam, S.; Richards, R.; Hall-Craggs, M.; Witt, J. The influence of pelvic tilt on acetabular orientation and cover: A three-dimensional computerised tomography analysis. Hip. Int. 2013, 23, 87–92. [Google Scholar] [CrossRef]
- Maratt, J.D.; Esposito, C.I.; McLawhorn, A.S.; Jerabek, S.A.; Padgett, D.E.; Mayman, D.J. Pelvic tilt in patients undergoing total hip arthroplasty: When does it matter? J. Arthroplast. 2015, 30, 387–391. [Google Scholar] [CrossRef]
- Haffer, H.; Wang, Z.; Hu, Z.; Hipfl, C.; Perka, C.; Pumberger, M. Total Hip Replacement Influences Spinopelvic Mobility: A Prospective Observational Study. J. Arthroplast. 2022, 37, 316–324.e312. [Google Scholar] [CrossRef]
- Haffer, H.; Wang, Z.; Hu, Z.; Hipfl, C.; Pumberger, M. Acetabular cup position differs in spinopelvic mobility types: A prospective observational study of primary total hip arthroplasty patients. Arch. Orthop. Trauma Surg. 2021, 1–11. [Google Scholar] [CrossRef]
- Muellner, M.; Becker, L.; Wang, Z.; Hu, Z.; Hardt, S.; Pumberger, M.; Haffer, H. Spinopelvic mobility is influenced by pre-existing contralateral hip arthroplasty: A matched-pair analysis in patients undergoing hip replacement. J. Orthop. Surg. Res. 2022, 17, 64. [Google Scholar] [CrossRef]
- Benlidayi, I.C.; Coskun, N.C.; Basaran, S. Does Lumbosacral Transitional Vertebra Have Any Influence on Sacral Tilt? Spine 2015, 40, E1176–E1179. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.T.; Shen, Q.H.; Jeon, C.H.; Chung, N.S.; Jeong, S.; Lee, H.D. No linear correlation between pelvic incidence and acetabular orientation: Retrospective observational study. Medicine 2021, 100, e25445. [Google Scholar] [CrossRef] [PubMed]



| Castellvi Type | Description | Patients Example |
|---|---|---|
| I | Ia: Unilateral dysplastic transversal process > 19 mm Ib: Bilateral dysplastic transversal process > 19 mm | Ib |
| II | IIa: Unilateral pseudarthrosis between transversal process and sacral bone IIb: Bilateral pseudarthrosis between transversal process and sacral bone | IIa |
| III | IIIa: Unilateral bony union between transversal process and sacral bone IIIb: Bilateral bony union between transversal process and sacral bone | IIIb |
| IV | Unilateral bony union contralateral pseudarthrosis between transversal process and sacral bone | IV |
| Castellvi | I | II | III | IV |
|---|---|---|---|---|
| Patients (n) | 16 (32%) | 23 (46%) | 6 (12%) | 5 (10%) |
| Control Group | LSTV | |
|---|---|---|
| Age (years) mean (SD) | 51.9 (20.1) | 52.0 (17.6) |
| Sex | ||
| Female (n) | 23 | 23 |
| Male (n) | 27 | 27 |
| 5 Lumbar vertebrae (n) | 50 | 32 |
| 6 Lumbar vertebrae (n) | 0 | 11 |
| 4 Lumbar vertebrae (n) | 0 | 7 |
| Anatomical (±SD) | Functional (±SD) | p-Value | |
|---|---|---|---|
| Anteversion | 19.4 (7.5) | 19.4 (7.5) | 0.783 |
| Inclination | 49.6 (7.4) | 48.8 (6.8) | <0.001 |
| LSTV (n = 50) (±SD) | Control (n = 50) (±SD) | p-Value | |
|---|---|---|---|
| Pelvic tilt (°) | 2.2 (6.6) | 1.4 (7.8) | 0.553 |
| fAA (°) | 20.2 (7.0) | 18.5 (8.0) | 0.266 |
| aAA (°) | 20.2 (7.2) | 18.6 (7.7) | 0.282 |
| fAI (°) | 49.1 (6.7) | 48.6 (7.1) | 0.765 |
| aAI (°) | 49.9 (7.2) | 49.3 (7.7) | 0.748 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Becker, L.; Taheri, N.; Haffer, H.; Muellner, M.; Hipfl, C.; Ziegeler, K.; Diekhoff, T.; Pumberger, M. Lumbosacral Transitional Vertebrae Influence on Acetabular Orientation and Pelvic Tilt. J. Clin. Med. 2022, 11, 5153. https://doi.org/10.3390/jcm11175153
Becker L, Taheri N, Haffer H, Muellner M, Hipfl C, Ziegeler K, Diekhoff T, Pumberger M. Lumbosacral Transitional Vertebrae Influence on Acetabular Orientation and Pelvic Tilt. Journal of Clinical Medicine. 2022; 11(17):5153. https://doi.org/10.3390/jcm11175153
Chicago/Turabian StyleBecker, Luis, Nima Taheri, Henryk Haffer, Maximilian Muellner, Christian Hipfl, Katharina Ziegeler, Torsten Diekhoff, and Matthias Pumberger. 2022. "Lumbosacral Transitional Vertebrae Influence on Acetabular Orientation and Pelvic Tilt" Journal of Clinical Medicine 11, no. 17: 5153. https://doi.org/10.3390/jcm11175153





