A Study on the Reference Values and Cutoff Criteria of Masking Level Difference for Children Aged 7–12 Years
Abstract
:1. Introduction
2. Materials and Methods
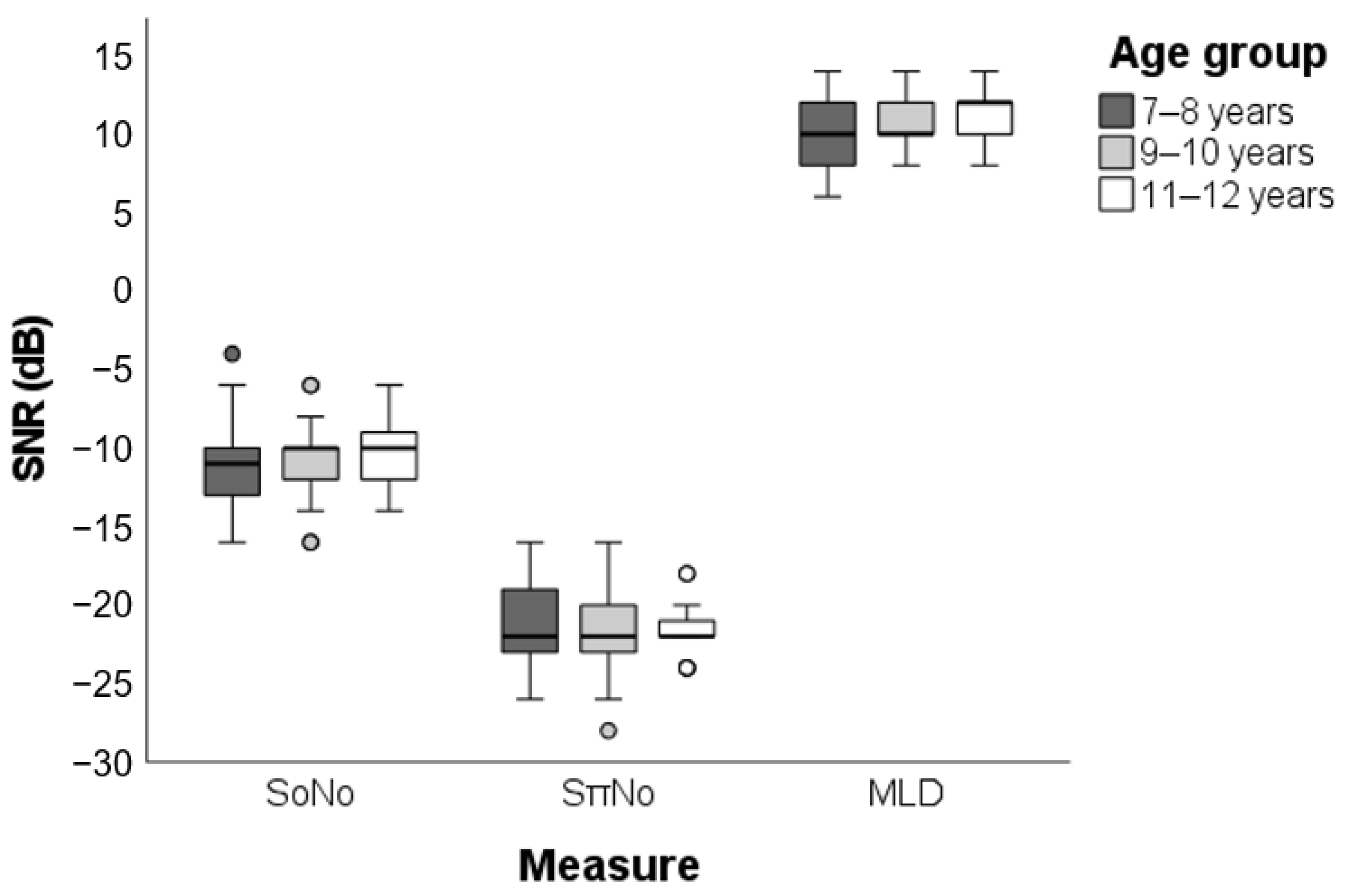
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- ASHA (American Speech-Language-Hearing Association). Central Auditory Processing Disorder (Practice Portal). Available online: www.asha.org/Practice-Portal/Clinical-Topics/Central-Auditory-Processing-Disorder/ (accessed on 12 March 2021).
- AAA (American Academy of Audiology). Clinical Practice Guidelines: Diagnosis, Treatment and Management of Children and Adults with Central Auditory Processing Disorder. Available online: https://audiology-web.s3.amazonaws.com/migrated/CAPD Guidelines 8-2010.pdf_539952af956c79.73897613.pdf (accessed on 26 March 2020).
- BSA (British Society of Audiology). Practice Guidance—An Overview of Current Management of Auditory Processing Disorder (APD). Available online: http://www.thebsa.org.uk/wp-content/uploads/2014/04/BSA_APD_Management_1Aug11_FINAL_amended17Oct11.pdf (accessed on 12 March 2021).
- BSA (British Society of Audiology). Position Statement and Practice Guidance—Auditory Processing Disorder (APD). Available online: www.thebsa.org (accessed on 12 March 2021).
- Baran, J.A. Test Battery Principles and Considerations. In Handbook of Central Auditory Processing Disorder: Auditory Neuroscience and Diagnosis; Musiek, F.E., Chermak, G.D., Eds.; Plural Publishing: San Diego, CA, USA, 2013; pp. 291–323. [Google Scholar]
- Sutojo, S.; Par, S.; Schoenmaker, E. Contribution of Binaural Masking Release to Improved Speech Intelligibility for Different Masker Types. Eur. J. Neurosci. 2020, 51, 1339–1352. [Google Scholar] [CrossRef] [PubMed]
- Hirsh, I.J. The Influence of Interaural Phase on Interaural Summation and Inhibition. J. Acoust. Soc. Am. 1948, 20, 536–544. [Google Scholar] [CrossRef]
- Licklider, J.C.R. The Influence of Interaural Phase Relations upon the Masking of Speech by White Noise. J. Acoust. Soc. Am. 1948, 20, 150–159. [Google Scholar] [CrossRef]
- Olsen, W.O.; Noffsinger, D.; Carhart, R. Masking Level Differences Encountered in Clinical Populations. Int. J. Audiol. 1976, 15, 287–301. [Google Scholar] [CrossRef] [PubMed]
- Burnham, M.N. Normal Masking Level Difference Parameters for Use in the Clinical Evaluation of Auditory Processing Disorders. Master’s Thesis, Brigham Young University, Provo, UT, USA, 2010. [Google Scholar]
- Wilson, J.R.; Krishnan, A. Human Frequency-Following Responses to Binaural Masking Level Difference Stimuli. J. Am. Acad. Audiol. 2005, 16, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Santiago, J.M.; Luiz, C.B.L.; Garcia, M.; Gil, D. Masking Level Difference and Electrophysiological Evaluation in Adults with Normal Hearing. Int. Arch. Otorhinolaryngol. 2020, 24, e399–e406. [Google Scholar] [CrossRef]
- Nickisch, A.; Kiese-Himmel, C.; Wiesner, T.; Schönweiler, R. Guideline: Auditory Processing and Perception Disorders: Differential Diagnosis: S1 Guideline of the German Society of Phoniatrics and Pediatric Audiology. HNO 2019, 67, 576–583. [Google Scholar] [CrossRef]
- Iliadou, V.; Ptok, M.; Grech, H.; Pedersen, E.R.; Brechmann, A.; Deggouj, N.; Kiese-Himmel, C.; Śliwińska-Kowalska, M.; Nickisch, A.; Demanez, L.; et al. A European Perspective on Auditory Processing Disorder-Current Knowledge and Future Research Focus. Front. Neurol. 2017, 8, 622. [Google Scholar] [CrossRef]
- Keith, W.J.; Purdy, S.C.; Baily, M.R.; Kay, F.M. New Zealand Guidelines on Auditory Processing Disorder. Available online: https://www.audiology.org.nz/ (accessed on 12 March 2021).
- Wilson, R.H.; Moncrieff, D.W.; Townsend, E.A.; Pillion, A.L. Development of a 500-Hz Masking-Level Difference Protocol for Clinic Use. J. Am. Acad. Audiol. 2003, 14, 1–8. [Google Scholar] [CrossRef]
- Sweetow, R.W.; Reddell, R.C. The Use of Masking Level Differences in the Identification of Children with Perceptual Problems. J. Am. Aud. Soc. 1978, 4, 52–56. [Google Scholar]
- Frota, S.M.M.C.; Leite Filho, C.A.; Bruno, C.S.; Carvalho, L.B.; Riegel, N.A.; da Silva Rodrigues de Souza, S.A.; Branco-Barreiro, F.C.A. Masking Level Difference: Test-Retest Reliability Assessment in Normal Hearing Female University Students. CoDAS 2022, 34, e20200207. [Google Scholar] [CrossRef] [PubMed]
- Martins, Q.P.; Faccin, V.A.; Brückmann, M.; Gil, D.; Garcia, M.V. Masking Level Difference in Schoolchildren: Environmental Analysis. CoDAS 2018, 30, e20170048. [Google Scholar] [CrossRef] [PubMed]
- Tomlin, D.; Dillon, H.; Sharma, M.; Rance, G. The Impact of Auditory Processing and Cognitive Abilities in Children. Ear Hear. 2015, 36, 527–542. [Google Scholar] [CrossRef] [PubMed]
- Loo, J.H.Y.; Bamiou, D.; Rosen, S. The Impacts of Language Background and Language-Related Disorders in Auditory Processing Assessment. J. Speech Lang. Hear. Res. 2013, 56, 1–12. [Google Scholar] [CrossRef]
- de Carvalho, N.G.; do Amaral, M.I.R.; de Barros, V.Z.; dos Santos, M.F.C. Masking Level Difference: Performance of School Children Aged 7–12 Years. J. Audiol. Otol. 2021, 25, 65–71. [Google Scholar] [CrossRef]
- Moore, D.R.; Cowan, J.A.; Riley, A.; Edmondson-Jones, A.M.; Ferguson, M.A. Development of Auditory Processing in 6- to 11-Yr-Old Children. Ear Hear. 2011, 32, 269–285. [Google Scholar] [CrossRef]
- Gicov, R.A.; Tordin, G.C.; Santos, T.M.M.; Branco-Barreiro, F.C.A. Masking Level Difference in Seven-to-Eight-Year-Old Children. Rev. Equilíb. Corpor. Saúde 2015, 7, 17–20. [Google Scholar]
- Bartz, D.W.; Laux, C.N.; Peruch, C.V.; da Costa Ferreira, M.I.D.; Machado, M.S.; Ribas, L.P. Relationship between Masking Level Difference Test and Acoustic Reflex Findings in Children with Phonological Disorder. Rev. CEFAC 2015, 17, 1499–1508. [Google Scholar] [CrossRef]
- Aithal, V.; Yonovitz, A.; Aithal, S.; Dold, N. Tonal Masking Level Difference in Children. Aust. N. Z. J. Audiol. 2006, 28, 11–17. [Google Scholar] [CrossRef]
- Litovsky, R. Development of the Auditory System. Handb. Clin. Neurol. 2015, 129, 55–72. [Google Scholar] [CrossRef]
- Hall, J.W.; Buss, E.; Grose, J.H.; Dev, M.B. Developmental Effects in the Masking-Level Difference. J. Speech Lang. Hear. Res. 2004, 47, 13–20. [Google Scholar] [CrossRef]
- Hogan, S.C.M.; Moore, D.R. Impaired Binaural Hearing in Children Produced by a Threshold Level of Middle Ear Disease. J. Assoc. Res. Otolaryngol. 2003, 4, 123–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Porter, H.L.; Grantham, D.W.; Ashmead, D.H.; Tharpe, A.M. Binaural Masking Release in Children With Down Syndrome. Ear Hear. 2014, 35, e134–e142. [Google Scholar] [CrossRef] [PubMed]
- Skoe, E.; Krizman, J.; Anderson, S.; Kraus, N. Stability and Plasticity of Auditory Brainstem Function across the Lifespan. Cereb. Cortex 2015, 25, 1415–1426. [Google Scholar] [CrossRef] [PubMed]
- Mattsson, T.S.; Follestad, T.; Andersson, S.; Lind, O.; Øygarden, J.; Nordgård, S. Normative Data for Diagnosing Auditory Processing Disorder in Norwegian Children Aged 7–12 Years. Int. J. Audiol. 2018, 57, 10–20. [Google Scholar] [CrossRef]
- Musiek, F.E. Frequency (Pitch) and Duration Pattern Tests. J. Am. Acad. Audiol. 1994, 5, 265–268. [Google Scholar]
- Filippini, R.; Leite Filho, C.A.; Barros, G.M.S.B.; Musiek, F.E.; Schochat, E. Evidence of Validity and Normative Values of a New Auditory Backward Masking Test. J. Clin. Med. 2022, 11, 4933. [Google Scholar] [CrossRef]
- Ahmmed, A.U.; Ahmmed, A.A. Setting Appropriate Pass or Fail Cut-off Criteria for Tests to Reflect Real Life Listening Difficulties in Children with Suspected Auditory Processing Disorder. Int. J. Pediatr. Otorhinolaryngol. 2016, 84, 166–173. [Google Scholar] [CrossRef]
- Musiek, F.E.; Gollegly, K.M.; Kibbe, K.S.; Verkest-Lenz, S.B. Proposed Screening Test for Central Auditory Disorders: Follow-up on the Dichotic Digits Test. Am. J. Otol. 1991, 12, 109–113. [Google Scholar]
- de Oliveira Bresola, J.; Padilha, F.Y.O.M.M.; de Braga Junior, J.; Pinheiro, M.M.C. The Use of the Dichotic Digit Test as a Screening Method. Codas 2021, 33, e20200314. [Google Scholar] [CrossRef]
- de Oliveira Matos, M.M.; Frota, S. The Influence of Sensoryneural Hearing Loss on Temporal Ordering. Rev. CEFAC 2013, 15, 1435–1440. [Google Scholar] [CrossRef]
- Pereira, L.D.; Schochat, E. Testes Auditivos Comportamentais Para Avaliação Do Processamento Auditivo Central; Pró-Fono: Barueri, Brazil, 2011. [Google Scholar]
- Auditec. Masking Level Difference. Evaluation Manual; Auditec: St. Louis, MO, USA, 2002. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Leite Filho, C.A. Considerations on Linear Correlation Analysis. Audiol. Commun. Res. 2019, 24, e2143. [Google Scholar] [CrossRef]
- Nozza, R.J.; Wagner, E.F.; Crandell, M.A. Binaural Release from Masking for a Speech Sound in Infants, Preschoolers, and Adults. J. Speech Lang. Hear. Res. 1988, 31, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Van Deun, L.; van Wieringen, A.; Van den Bogaert, T.; Scherf, F.; Offeciers, F.E.; Van de Heyning, P.H.; Desloovere, C.; Dhooge, I.J.; Deggouj, N.; De Raeve, L.; et al. Sound Localization, Sound Lateralization, and Binaural Masking Level Differences in Young Children with Normal Hearing. Ear Hear. 2009, 30, 178–190. [Google Scholar] [CrossRef]
- do Couto Mendes, S.; Branco-Barreiro, F.C.A.; Frota, S. Masking Level Difference: Reference Values in Adults. Audiol. Commun. Res. 2017, 22, 1746. [Google Scholar] [CrossRef]
- Paula, P.; Frota, S.; Felipe, L. Masking Threshold Differential (MLD): Pilot Study. Int. Arch. Otorhinolaryngol. 2012, 16, 102. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the Sample Mean and Standard Deviation from the Sample Size, Median, Range and/or Interquartile Range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Zhang, F.; Roland, C.; Rasul, D.; Cahn, S.; Liang, C.; Valencia, G. Comparing Musicians and Non-Musicians in Signal-in-Noise Perception. Int. J. Audiol. 2019, 58, 717–723. [Google Scholar] [CrossRef]
- Ziliotto, K.N.; dos Santos, M.F.C.; Monteiro, V.G.; Pradella-Hallinan, M.; Moreira, G.A.; Pereira, L.D.; Weckx, L.L.M.; Fujita, R.R.; Pizarro, G.U. Auditory Processing Assessment in Children with Obstructive Sleep Apnea Syndrome. Rev. Bras. Otorrinolaringol. 2006, 72, 321–327. [Google Scholar] [CrossRef]
- Leite Filho, C.A.; da Silva, F.F.; Pradella-Hallinan, M.; Xavier, S.D.; Miranda, M.C.; Pereira, L.D. Auditory Behavior and Auditory Temporal Resolution in Children with Sleep-Disordered Breathing. Sleep Med. 2017, 34, 90–95. [Google Scholar] [CrossRef]
- Musiek, F.E.; Chermak, G.D.; Weihing, J.; Zappulla, M.; Nagle, S. Diagnostic Accuracy of Established Central Auditory Processing Test Batteries in Patients with Documented Brain Lesions. J. Am. Acad. Audiol. 2011, 22, 342–358. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, M.A.; Fox-Thomas, L.; Tucker, D. Impact of Different Cutoff Criteria on Rate of (Central) Auditory Processing Disorders Diagnosis Using the Central Test Battery. Audiol. Res. 2016, 6, 40–43. [Google Scholar] [CrossRef]
- Wilson, W.J.; Arnott, W. Using Different Criteria to Diagnose (Central) Auditory Processing Disorder: How Big a Difference Does It Make? J. Speech Lang. Hear. Res. 2013, 56, 63–70. [Google Scholar] [CrossRef]
- Filippini, R.; Weihing, J.; Chermak, G.D.; Musiek, F.E. Current Issues in the Diagnosis and Treatment of CAPD in Children. In Auditory Processing Disorder: Assessment, Management, and Treatment; Geffner, D., Ross-Swain, D., Eds.; Plural Publishing: San Diego, CA, USA, 2019; pp. 3–36. [Google Scholar]

| Parameters | Mode | Percentile | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2.5 | 5 | 10 | 25 | 50 | 75 | 90 | 95 | 97.5 | ||
| SNR-S0N0 (dB) | −10 | −16 | −16 | −14 | −12 | −10 | −10 | −8 | −6 | −5 |
| SNR-SπN0 (dB) | −22 | −27 | −26 | −24 | −22 | −22 | −20 | −18 | −16 | −15 |
| MLD (dB) | 10 | 7 | 8 | 8 | 10 | 10 | 12 | 12 | 14 | 14 |
| Measure | Mean [BCa 95% CI] | SD | Cutoff Point (SD) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| −3 | −2 | −1.5 | −1 | +1 | +1.5 | +2 | +3 | |||
| SNR-S0N0 (dB) | −10.88 [−11.49, −10.26] | 2.66 | -- | -- | -- | -- | −8.22 | −6.89 | −5.56 | −2.90 |
| SNR-SπN0 (dB) | −21.39 [−22.03, −20.75] | 2.71 | -- | -- | -- | -- | −18.68 | −17.32 | −15.97 | −13.26 |
| MLD (dB) | 10.51 [10.04, 10.95] | 1.84 | 4.99 | 6.83 | 7.75 | 8.67 | -- | -- | -- | -- |
| Study (Data Source) | Age Group | n | Mean | SD | 95% CI b | Mean—2 SD b | |
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Leite Filho et al. (Present study) | 7–12 years | 59 | 10.51 | 1.84 | 10.04 | 10.95 | 6.83 |
| Aithal et al. [26] | 6–13 years | 62 | 11.21 | 1.67 | 10.79 | 11.63 | 7.87 |
| Moore et al. [23] | 6–11 years | 45 | 13.88 a | 4.61 a | 12.49 | 15.27 | 4.66 |
| Porter et al. [30] | 3–12 years | 46 | 13.70 | 4.90 | 12.28 | 15.12 | 3.90 |
| Gicov et al. [24] | 7–8 years | 21 | 6.95 | 2.33 | 5.95 | 7.95 | 2.29 |
| Martins et al. [19] | 7–10 years | 31 | 7.65 | 2.51 | 6.77 | 8.53 | 2.63 |
| Mattsson et al. [32] | 7–12 years | 266 | 14.60 | 2.80 | 14.26 | 14.94 | 9.00 |
| de Carvalho et al. [22] | 7–12 years | 47 | 13.66 | 2.18 | 13.04 | 14.28 | 9.30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leite Filho, C.A.; de Oliveira Viana, M.; Branco-Barreiro, F.C.A.; Frota, S.M.M.C. A Study on the Reference Values and Cutoff Criteria of Masking Level Difference for Children Aged 7–12 Years. J. Clin. Med. 2022, 11, 5282. https://doi.org/10.3390/jcm11185282
Leite Filho CA, de Oliveira Viana M, Branco-Barreiro FCA, Frota SMMC. A Study on the Reference Values and Cutoff Criteria of Masking Level Difference for Children Aged 7–12 Years. Journal of Clinical Medicine. 2022; 11(18):5282. https://doi.org/10.3390/jcm11185282
Chicago/Turabian StyleLeite Filho, Carlos Alberto, Mônica de Oliveira Viana, Fátima Cristina Alves Branco-Barreiro, and Silvana Maria Monte Coelho Frota. 2022. "A Study on the Reference Values and Cutoff Criteria of Masking Level Difference for Children Aged 7–12 Years" Journal of Clinical Medicine 11, no. 18: 5282. https://doi.org/10.3390/jcm11185282
APA StyleLeite Filho, C. A., de Oliveira Viana, M., Branco-Barreiro, F. C. A., & Frota, S. M. M. C. (2022). A Study on the Reference Values and Cutoff Criteria of Masking Level Difference for Children Aged 7–12 Years. Journal of Clinical Medicine, 11(18), 5282. https://doi.org/10.3390/jcm11185282





