FGFR-2 and Epithelial–Mesenchymal Transition in Endometrial Cancer
Abstract
:1. Introduction
2. Materials and Methods
2.1. Molecular Analysis
2.2. Ethical Statement
2.3. Statistical Analysis
3. Results
3.1. Epithelial–Mesenchymal Transition Analysis
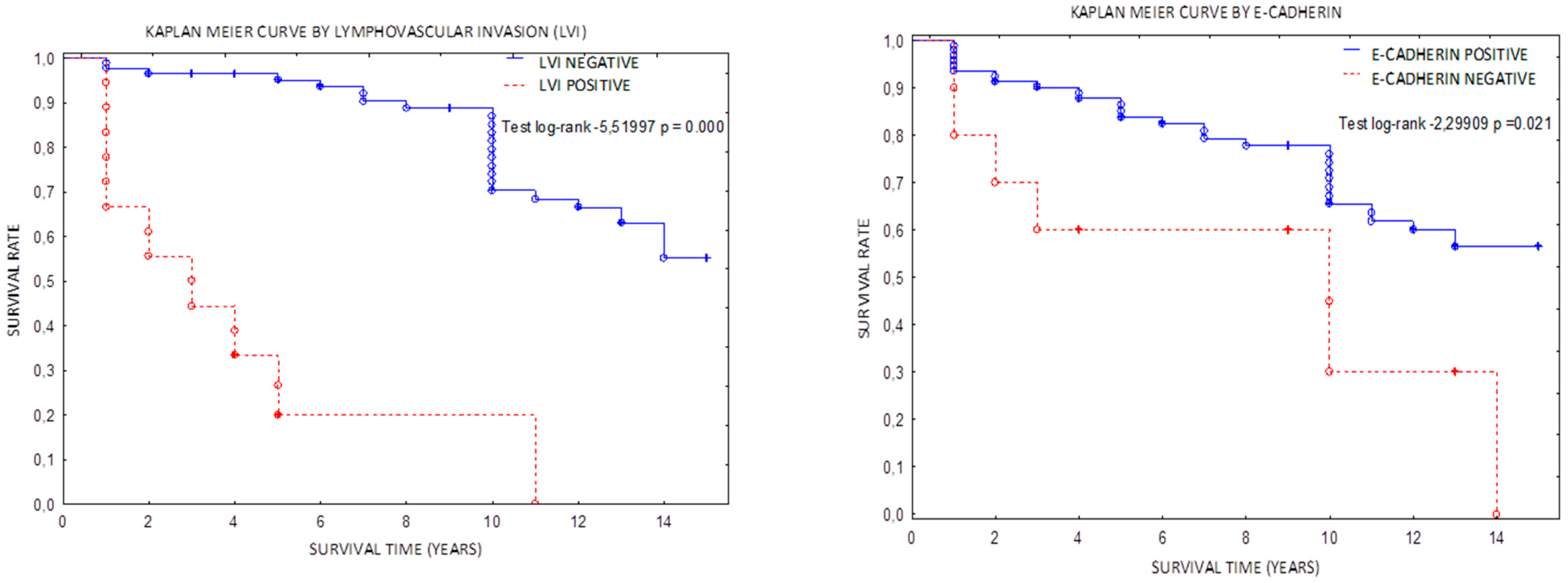
3.2. Epithelial–Mesenchymal Transition and FGFR-2 Mutation Impact on Survive
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.; Naishadham, D.; Jemal, A. Cancer statistics. Cancer J. Clin. 2013, 63, 11–30. [Google Scholar] [CrossRef]
- WHO. Female Genital Tumours: WHO Classification of Tumours, 5th ed.; WHO: Geneva, Switzerland, 2020; Volume 4. [Google Scholar]
- Vermij, L.; Smit, V.; Nout, R.; Bosse, T. Incorporation of molecular characteristics into endometrial cancer management. Histopathology 2019, 76, 52–63. [Google Scholar] [CrossRef] [PubMed]
- Mayakonda, A.; Lin, D.-C.; Assenov, Y.; Plass, C.; Koeffler, H.P. Maftools: Efficient and comprehensive analysis of somatic variants in cancer. Genome Res. 2018, 28, 1747–1756. [Google Scholar] [CrossRef] [PubMed]
- Ijichi, N.; Ikeda, K.; Horie-Inoue, K.; Inoue, S. FOXP1 and Estrogen Signaling in Breast Cancer. Vitam. Horm. 2013, 93, 203–212. [Google Scholar] [CrossRef]
- Cruz, R.; Madden, S.; Richards, C.; Vellanki, S.; Jahns, H.; Hudson, L.; Fay, J.; O’Farrell, N.; Sheehan, K.; Jirström, K.; et al. Human Epidermal Growth Factor Receptor-3 Expression Is Regulated at Transcriptional Level in Breast Cancer Settings by Junctional Adhesion Molecule-A via a Pathway Involving Beta-Catenin and FOXA1. Cancers 2021, 13, 871. [Google Scholar] [CrossRef]
- Colas, E.; Pedrola, N.; Devis-Jauregui, L.; Ertekin, T.; Campoy, I.; Martínez, E.; Llauradó, M.; Rigau, M.; Olivan, M.; Garcia, M.; et al. The EMT signaling pathways in endometrial carcinoma. Clin. Transl. Oncol. 2012, 14, 715–720. [Google Scholar] [CrossRef]
- Opławski, M.; Nowakowski, R.; Średnicka, A.; Ochnik, D.; Grabarek, B.; Boroń, D. Molecular Landscape of the Epithelial–Mesenchymal Transition in Endometrioid Endometrial Cancer. J. Clin. Med. 2021, 10, 1520. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Bueno, G.; Portillo, F.; Cano, A. Transcriptional regulation of cell polarity in EMT and cancer. Oncogene 2008, 27, 6958–6969. [Google Scholar] [CrossRef]
- Sobočan, M.; Smolle, M.A.; Schatz, C.; Haybaeck, J. The Interplay of Tumor Stroma and Translational Factors in Endometrial Cancer. Cancers 2020, 12, 2074. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, W.; Sun, X.; Lin, Y.; Chen, W. Cancer-associated fibroblasts induce epithelial-mesenchymal transition through secreted cytokines in endometrial cancer cells. Oncol. Lett. 2018, 15, 5694–5702. [Google Scholar] [CrossRef] [Green Version]
- Byron, S.A.; Gartside, M.; Powell, M.A.; Wellens, C.L.; Gao, F.; Mutch, D.G.; Goodfellow, P.J.; Pollock, P.M. FGFR2 point mutations in 466 endometrioid endometrial tumors: Relationship with MSI, KRAS, PIK3CA, CTNNB1 mutations and clinicopathological features. PLoS ONE 2012, 7, e30801. [Google Scholar] [CrossRef]
- Jeske, Y.W.; Ali, S.; Byron, S.A.; Gao, F.; Mannel, R.S.; Ghebre, R.G.; DiSilvestro, P.A.; Lele, S.B.; Pearl, M.L.; Schmidt, A.P.; et al. FGFR2 mutations are associated with poor outcomes in endometrioid endometrial cancer: An NRG Oncology/Gynecologic Oncology Group study. Gynecol. Oncol. 2017, 145, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Xin, X.-Y.; Jin, Z.-S.; Hua, T.; Wang, H.-B.; Wang, H.-B. Transcriptomic analysis of stromal cells from patients with endometrial carcinoma. Int. J. Clin. Exp. Pathol. 2017, 10, 9853–9857. [Google Scholar]
- Sahoo, S.S.; Zhang, X.D.; Hondermarck, H.; Tanwar, P.S. The Emerging Role of the Microenvironment in Endometrial Cancer. Cancers 2018, 10, 408. [Google Scholar] [CrossRef]
- Brierley, J.D.; Gospodarowicz, M.K.; Wittekind, C. TNM Classification of Malignant Tumours, 8th ed.; John Wiley & Sons: Hoboken, NJ, USA, 2017; ISBN 978-1-119-26357-9. [Google Scholar]
- Oaknin, A.; Bosse, T.; Creutzber, C.; Giornelli, G.; Harter, P.; Joly, F.; Lorusso, D.; Marth, C.; Makker, V.; Mirza, M.; et al. Endometrial cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2022. [Google Scholar] [CrossRef]
- Adamczyk-Gruszka, O.; Horecka-Lewitowicz, A.; Strzelecka, A.; Wawszczak-Kasza, M.; Gruszka, J.; Lewitowicz, P. The Roles of TP53 and FGFR2 in Progress Made Treating Endometrial Cancer. Diagnostics 2022, 12, 1737. [Google Scholar] [CrossRef]
- Ueno, H.; Murphy, J.; Jass, J.R.; Mochizuki, H.; Talbot, I.C. Tumour ‘budding’ as an index to estimate the potential of aggressiveness in rectal cancer. Histopathology 2002, 40, 127–132. [Google Scholar] [CrossRef]
- Lugli, A.; Kirsch, R.; Ajioka, Y.; Bosman, F.; Cathomas, G.; Dawson, H.; El Zimaity, H.; Fléjou, J.-F.; Hansen, T.P.; Hartmann, A.; et al. Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016. Mod. Pathol. 2017, 30, 1299–1311. [Google Scholar] [CrossRef] [PubMed]
- Guasti, L.; Sze, W.C.; McKay, T.; Grose, R.; King, P.J. FGF signalling through Fgfr2 isoform IIIb regulates adrenal cortex development. Mol. Cell. Endocrinol. 2013, 371, 182–188. [Google Scholar] [CrossRef]
- Zheng, Z.; Kang, H.-Y.; Lee, S.; Kang, S.-W.; Goo, B.; Bin Cho, S. Up-regulation of fibroblast growth factor (FGF) 9 expression and FGF-WNT/β-catenin signaling in laser-induced wound healing. Wound Repair Regen. 2014, 22, 660–665. [Google Scholar] [CrossRef]
- Haase, M.; Thiel, A.; Scholl, U.I.; Ashmawy, H.; Schott, M.; Ehlers, M. Subcellular localization of fibroblast growth factor receptor type 2 and correlation with CTNNB1 genotype in adrenocortical carcinoma. BMC Res. Notes 2020, 13, 282. [Google Scholar] [CrossRef] [PubMed]
- Ishiwata, T. Role of fibroblast growth factor receptor-2 splicing in normal and cancer cells. Front. Biosci. 2018, 23, 626–639. [Google Scholar] [CrossRef] [PubMed]
- Fatima, I.; Barman, S.; Rai, R.; Thiel, K.W.; Chandra, V. Targeting Wnt Signaling in Endometrial Cancer. Cancers 2021, 13, 2351. [Google Scholar] [CrossRef]
- Chioni, A.-M.; Grose, R.P. Biological Significance and Targeting of the FGFR Axis in Cancer. Cancers 2021, 13, 5681. [Google Scholar] [CrossRef]
- Ferguson, H.; Smith, M.; Francavilla, C. Fibroblast Growth Factor Receptors (FGFRs) and Noncanonical Partners in Cancer Signaling. Cells 2021, 10, 1201. [Google Scholar] [CrossRef]
- Yu, W.N.; Yang, L.; Li, T.; Zhang, Y. Cadherin Signaling in Cancer: Its Functions and Role as a Therapeutic Target. Front. Oncol. 2019, 9, 989. [Google Scholar] [CrossRef] [PubMed]
- El-Hariry, I.; Pignatelli, M.; Lemoine, N.R. FGF-1 and FGF-2 regulate the expression of E-cadherin and catenins in pancreatic adenocarcinoma. Int. J. Cancer 2001, 94, 652–661. [Google Scholar] [CrossRef] [PubMed]
- Adamczyk-Gruszka, O.; Horecka-Lewitowicz, A.; Gruszka, J.; Wawszczak-Kasza, M.; Strzelecka, A.; Lewitowicz, P. Endometrial Cancer in Aspect of Forkhead Box Protein Contribution. Int. J. Environ. Res. Public Health 2022, 19, 10403. [Google Scholar] [CrossRef]
- Chen, H.Y.; Chiang, Y.F.; Huang, J.S.; Huang, T.C.; Shih, Y.H.; Wang, K.L.; Ali, M.; Hong, Y.H.; Shieh, T.M.; Hsia, S.M. Isoliquiritigenin Reverses Epithelial–mesenchymal Transition through Modulation of the TGF-β/Smad Signaling Pathway in Endometrial Cancer. Cancers 2021, 13, 1236. [Google Scholar] [CrossRef]


| Clone | Dilution | Manufacturer | Positive Expression | |
|---|---|---|---|---|
| Β-catenin | 14—monoclonal; mouse | 1.64 µg/mL; ready to use | Cell Marque | Nuclear/Cytoplasmic |
| Vimentin | Vim 3B4 | ready to use | Ventana | Cytoplasmic |
| ER | SP1 monoclonal, rabbit | 1 µg/mL; ready to use | Ventana | Nuclear |
| E-cadherin | 36 monoclonal; mouse | 0.314 µg/mL; ready to use | Ventana | Membranous |
| N = 103 | G(N) | TNM/FIGO | Stage Progress | Grade Progress | FGFR2 Mutation (N) | FGFR2 Wild Type (N) | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G1 | G2 | G3 | IA | IB | II | III | IV | ||||||
| Histopathological type | n/a | n/a | p < 0.001 | ||||||||||
| 14 | 15 | 10 | 93 | |||||||||
| 49 | 39 | 7 | 25 | 21 | 20 | 4 | 5 | 0 | 0 | |||
| ESMO | n/a | n/a | p = 0.021 | ||||||||||
| 49 | 17 | 0 | 49 | 20 | 18 | 0 | 0 | 3 | 100 | |||
| 0 | 22 | 7 | 0 | 1 | 2 | 10 | 14 | 7 | 3 | |||
| Substantial lymphovascular invasion (LVI) | 0 | 20 | 7 | 0 | 2 | 4 | 7 | 11 | p = 0.038 | p < 0.001 | 3 | 24 | p > 0.05 |
| Vimentin+ | 0 | 14 | 22 | 0 | 0 | 1 | 16 | 20 | p < 0.001 | p < 0.009 | 10 | 2 | p < 0.001 |
| EMT (tumor budding plus vimentin+, E-cadherin negative) | 0 | 6 | 14 | 0 | 4 | 5 | 6 | 17 | p < 0.01 | p < 0.001 | 10 | 1 | p < 0.001 |
| Β-catenin | 5 | 9 | 1 | 7 | 3 | 5 | 0 | 0 | p = 0.044 | p = 0.032 | 6 | 9 | p > 0.05 |
| E-cadherin lack | 0 | 1 | 4 | 0 | 0 | 3 | 6 | 10 | p = 0.002 | p < 0.00 | 9 | 1 | p < 0.001 |
| ER (77%) | 42 | 33 | 5 | 54 | 10 | 12 | 2 | 1 | p > 0.5 | p > 0.5 | 4 | 76 | p < 0.001 |
| FGFR-2 Mutated | FGFR-2 Wild Type | p | |
|---|---|---|---|
| Age (median) | 72 | 70 | p = 0.1632 |
| BMI (median) | 32.2 | 34 | p > 0.05 |
| FIGO G1 | 2 | 47 | p = 0.016 |
| FIGO G2 | 3 | 36 | p > 0.05 |
| FIGO G3 | 6 | 1 | p > 0.05 |
| FIGO stage I/II | 3 | 72 | p > 0.05 |
| FIGO stage III/IV | 7 | 21 | p = 0.034 |
| OS (median) (years) | 7.7 | 8 | p > 0.05 |
| RFS (median) (years) | 4 | 6.2 | p = 0.032 |
| ECSS (endometrial cancer specific survival; median) | 5.2 | 7.4 | p = 0.047 |
| Univariate Cox Model | Multivariate Cox Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Chi Square | HR | CI 95% | p | Chi Square | HR | p | CI 95% | |
| LVI+ | 42.84 | 0.0779 | −1.65 to −0.89 | 0.000 | 43.58 | 0.061 | 0.000 | −3.61 to −1.96 |
| Tumor budding | 3.997 | 0.4821 | −1.44 to −0.01 | 0.0455 | 0.080 | 0.8338 | 0.776 | −1.43 to 1.07 |
| Vimentin+ | 3.377 | 0.4934 | −0.72 to −0.02 | 0.066 | 0.047 | 0.877 | 0.827 | −1.30 to 1.043 |
| E−cadherin | 5.238 | 0.38 | −1.79 to −0.13 | 0.022 | 0.524 | 0.628 | 0.469 | −1.72 to 0.79 |
| FGFR2 mutation | 3.203 | 0.42 | −0.89 to 0.12 | 0.043 | 0.2850 | 1.635 | 0.59 | −1.54 to 0.66 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adamczyk-Gruszka, O.; Horecka-Lewitowicz, A.; Gruszka, J.; Wawszczak-Kasza, M.; Strzelecka, A.; Lewitowicz, P. FGFR-2 and Epithelial–Mesenchymal Transition in Endometrial Cancer. J. Clin. Med. 2022, 11, 5416. https://doi.org/10.3390/jcm11185416
Adamczyk-Gruszka O, Horecka-Lewitowicz A, Gruszka J, Wawszczak-Kasza M, Strzelecka A, Lewitowicz P. FGFR-2 and Epithelial–Mesenchymal Transition in Endometrial Cancer. Journal of Clinical Medicine. 2022; 11(18):5416. https://doi.org/10.3390/jcm11185416
Chicago/Turabian StyleAdamczyk-Gruszka, Olga, Agata Horecka-Lewitowicz, Jakub Gruszka, Monika Wawszczak-Kasza, Agnieszka Strzelecka, and Piotr Lewitowicz. 2022. "FGFR-2 and Epithelial–Mesenchymal Transition in Endometrial Cancer" Journal of Clinical Medicine 11, no. 18: 5416. https://doi.org/10.3390/jcm11185416





