Positive Airway Pressure at Extubation Minimizes Subglottic Secretion Leak In Vitro
Abstract
:1. Introduction
2. Materials and Methods
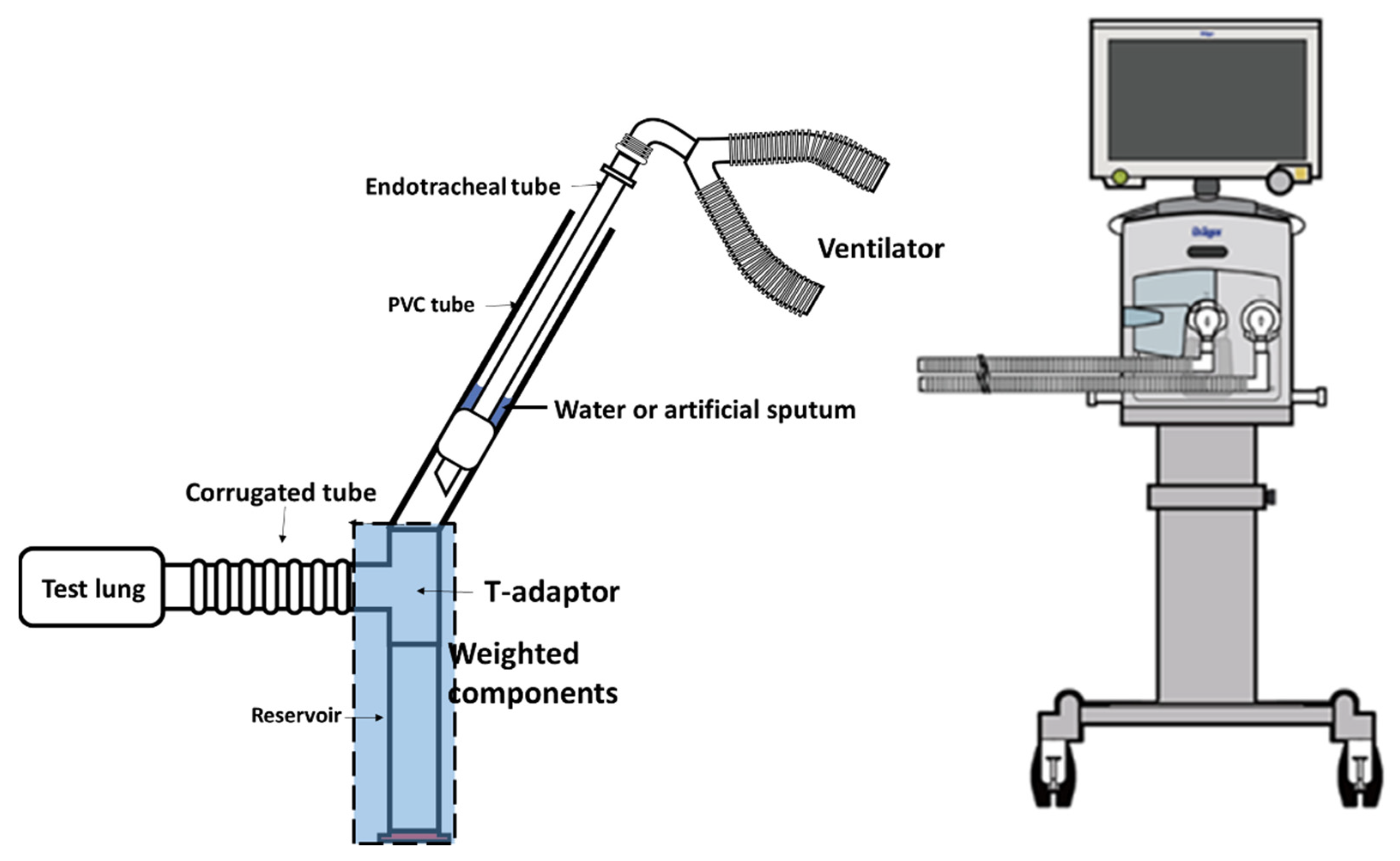
2.1. Tracheal Model
2.2. Preparation of Artificial Sputum
2.3. Extubation Techniques
2.4. Statistical Analysis
3. Results
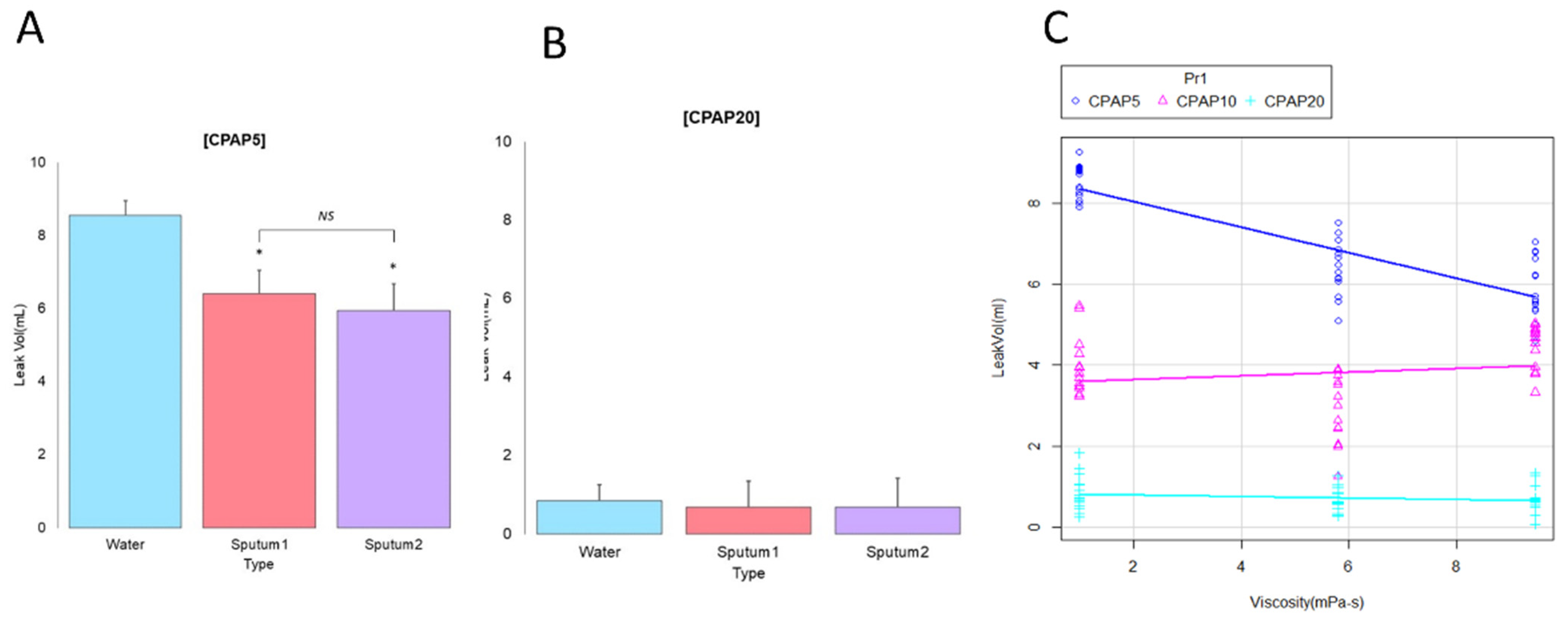
3.1. Influence of the Extubation Technique
3.2. Influence of Secretion Viscosity
3.3. Correlation between Secretion Viscosity and CPAP Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Neal, P.V.; Grap, M.J.; Munro, C.L.; Sessler, C.N.; Elswick, R.K., Jr.; Sinks, S.Z. Subglottic secretion volume and viscosity: Effect of systemic volume and oral hydration. Dynamics 2014, 25, 19–25. [Google Scholar]
- Nitta, K.; Okamoto, K.; Imamura, H.; Mochizuki, K.; Takayama, H.; Kamijo, H.; Okada, M.; Takeshige, K.; Kashima, Y.; Satou, T. A comprehensive protocol for ventilator weaning and extubation: A prospective observational study. J. Intensive Care 2019, 7, 50. [Google Scholar] [CrossRef] [PubMed]
- Hodd, J.; Doyle, A.; Carter, J.; Albarran, J.; Young, P. Increasing PEEP at extubation reduces subglottic secretion aspiration in a bench-top model. Nurs. Crit. Care 2010, 15, 257–261. [Google Scholar] [CrossRef]
- Andreu, M.F.; Bezzi, M.; Pedace, P.; Fredes, M.; Salvati, I.; Leoz, A.; Aguirre, M. Survey on the extubation procedure in intensive care units in Buenos Aires, Argentina. Rev. Bras Ter. Intensiva 2019, 31, 180–185. [Google Scholar] [CrossRef]
- Andreu, M.F.; Salvati, I.G.; Donnianni, M.C.; Ibanez, B.; Cotignola, M.; Bezzi, M. Effect of applying positive pressure with or without endotracheal suctioning during extubation: A laboratory study. Respir. Care 2014, 59, 1905–1911. [Google Scholar] [CrossRef] [Green Version]
- Rassam, S.; Sandbythomas, M.; Vaughan, R.S.; Hall, J.E. Airway management before, during and after extubation: A survey of practice in the United Kingdom and Ireland. Anaesthesia 2005, 60, 995–1001. [Google Scholar] [CrossRef]
- Gentile, M.A.; Siobal, M.S. Are specialized endotracheal tubes and heat-and-moisture exchangers cost-effective in preventing ventilator associated pneumonia? Respir. Care 2010, 55, 184–196. [Google Scholar] [PubMed]
- Hodd, J.; Doyle, A.; Carter, J.; Albarran, J.; Young, P. Extubation in intensive care units in the UK: An online survey. Nurs. Crit. Care 2010, 15, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Puchelle, E.; Bajolet, O.; Abély, M. Airway mucus in cystic fibrosis. Paediatr. Respir. Rev. 2002, 3, 115–119. [Google Scholar] [CrossRef]
- Lin, V.Y.; Kaza, N.; Birket, S.E.; Kim, H.; Edwards, L.J.; LaFontaine, J.; Liu, L.; Mazur, M.; Byzek, S.A.; Hanes, J.; et al. Excess mucus viscosity and airway dehydration impact COPD airway clearance. Eur. Respir. J. 2020, 55. [Google Scholar] [CrossRef]
- Brooks, M.L.; Brooks, D.L. Exploring Medical Language: A Student Directed Approach, 10th ed.; Mosby Elsevier: St. Louis, MI, USA, 2008; p. 68. [Google Scholar]
- Yousefshahi, F.; Barkhordari, K.; Movafegh, A.; Tavakoli, V.; Paknejad, O.; Bina, P.; Yousefshahi, H.; Fathollahi, M.S. A New Method for Extubation: Comparison between Conventional and New Method. J. Tehran Univ. Heart Cent. 2012, 7, 121–127. [Google Scholar]
- Andreu, M.F.; Dotta, M.E.; Bezzi, M.G.; Borello, S.; Cardoso, G.P.; Dib, P.C.; Garcia Schustereder, S.L.; Galloli, A.M.; Castro, D.R.; Di Giorgio, V.L.; et al. Safety of Positive Pressure Extubation Technique. Respir. Care 2019, 64, 899–907. [Google Scholar] [CrossRef]
- L’Hermite, J.; Wira, O.; Castelli, C.; de La Coussaye, J.E.; Ripart, J.; Cuvillon, P. Tracheal extubation with suction vs. positive pressure during emergence from general anaesthesia in adults: A randomised controlled trial. Anaesth. Crit. Care Pain Med. 2018, 37, 147–153. [Google Scholar] [CrossRef]
- Langeron, O.; Bourgain, J.L.; Francon, D.; Amour, J.; Baillard, C.; Bouroche, G.; Chollet Rivier, M.; Lenfant, F.; Plaud, B.; Schoettker, P.; et al. Difficult intubation and extubation in adult anaesthesia. Anaesth. Crit. Care Pain Med. 2018, 37, 639–651. [Google Scholar] [CrossRef]
- Cook, T.M.; MacDougall-Davis, S.R. Complications and failure of airway management. Br. J. Anaesth. 2012, 109 (Suppl. 1), i68–i85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warner, M.A.; Warner, M.E.; Weber, J.G. Clinical significance of pulmonary aspiration during the perioperative period. J. Am. Soc. Anesthesiol. 1993, 78, 56–62. [Google Scholar] [CrossRef]
- Young, P.J.; Rollinson, M.; Downward, G.; Henderson, S. Leakage of fluid past the tracheal tube cuff in a benchtop model. Br. J. Anaesth. 1997, 78, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Luecke, T.; Pelosi, P. Clinical review: Positive end-expiratory pressure and cardiac output. Crit. Care 2005, 9, 607–621. [Google Scholar] [CrossRef] [Green Version]
- Volpe, M.S.; Adams, A.B.; Amato, M.B.; Marini, J.J. Ventilation patterns influence airway secretion movement. Respir. Care 2008, 53, 1287–1294. [Google Scholar]
- Mohammadi, M.; Khafaee Pour Khamseh, A.; Varpaei, H.A. Invasive Airway “Intubation” in COVID-19 Patients; Statistics, Causes, and Recommendations: A Review Article. Anesthesiol. Pain Med. 2021, 11, e115868. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Gregson, F.K.A.; Shrimpton, A.; Cook, T.M.; Bzdek, B.R.; Reid, J.P.; Pickering, A.E. A quantitative evaluation of aerosol generation during tracheal intubation and extubation. Anaesthesia 2021, 76, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Priebe, H.J. Could “safe practice” be compromising safe practice? Should anesthetists have to deflate the cuff of the endotracheal tube before extubation? Minerva Anestesiol. 2016, 82, 236–239. [Google Scholar] [PubMed]
- Lacherade, J.C.; De Jonghe, B.; Guezennec, P.; Debbat, K.; Hayon, J.; Monsel, A.; Fangio, P.; Appere de Vecchi, C.; Ramaut, C.; Outin, H.; et al. Intermittent subglottic secretion drainage and ventilator-associated pneumonia: A multicenter trial. Am. J. Respir. Crit. Care Med. 2010, 182, 910–917. [Google Scholar] [CrossRef] [PubMed]

| Method | Description of Procedures |
|---|---|
| CPAP 5 | Ventilator was connected to the ETT, and the ventilator was set at CPAP mode of 5 cm H2O. The cuff was deflated after 3 spontaneous breaths, and then the ETT was removed immediately. |
| CPAP 10 | Ventilator was connected to ETT and the ventilator was set at CPAP mode of 10 cm H2O. The cuff was deflated after 3 spontaneous breaths, and then the ETT was removed immediately. |
| CPAP 20 | Ventilator was connected to the ETT, and the ventilator was set at CPAP mode of 20 cm H2O. The cuff was deflated after 3 spontaneous breaths, and then the ETT was removed immediately. |
| Resuscitator | A resuscitator was attached to the ETT and then squeezed 3 breaths every 3 s after achieving a pressure of 20 cm H2O. The ETT cuff was deflated while squeezing the resuscitator, and then the ETT was removed immediately. |
| Suction | A 14-Fr suction catheter was inserted into the ETT up to 2 cm above the ETT tip. A wall suction regulator at a pressure of 150 cm H2O was used for continuous suction. The ETT and suction catheter were removed together immediately after the cuff was deflated. |
| Water | Sputum 1 | Sputum 2 | p | |
|---|---|---|---|---|
| Suction | 8.85 ± 0.31 | 7.34 ± 0.54 | 7.8 6 ± 0.45 | <0.001 |
| Resuscitator | 8.96 ± 0.34 | 7.98 ± 0.34 | 8.00 ± 0.49 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, T.-P.; Li, H.-H.; Lin, H.-L. Positive Airway Pressure at Extubation Minimizes Subglottic Secretion Leak In Vitro. J. Clin. Med. 2022, 11, 307. https://doi.org/10.3390/jcm11020307
Wang T-P, Li H-H, Lin H-L. Positive Airway Pressure at Extubation Minimizes Subglottic Secretion Leak In Vitro. Journal of Clinical Medicine. 2022; 11(2):307. https://doi.org/10.3390/jcm11020307
Chicago/Turabian StyleWang, Tzu-Pei, Hsin-Hsien Li, and Hui-Ling Lin. 2022. "Positive Airway Pressure at Extubation Minimizes Subglottic Secretion Leak In Vitro" Journal of Clinical Medicine 11, no. 2: 307. https://doi.org/10.3390/jcm11020307
APA StyleWang, T.-P., Li, H.-H., & Lin, H.-L. (2022). Positive Airway Pressure at Extubation Minimizes Subglottic Secretion Leak In Vitro. Journal of Clinical Medicine, 11(2), 307. https://doi.org/10.3390/jcm11020307






