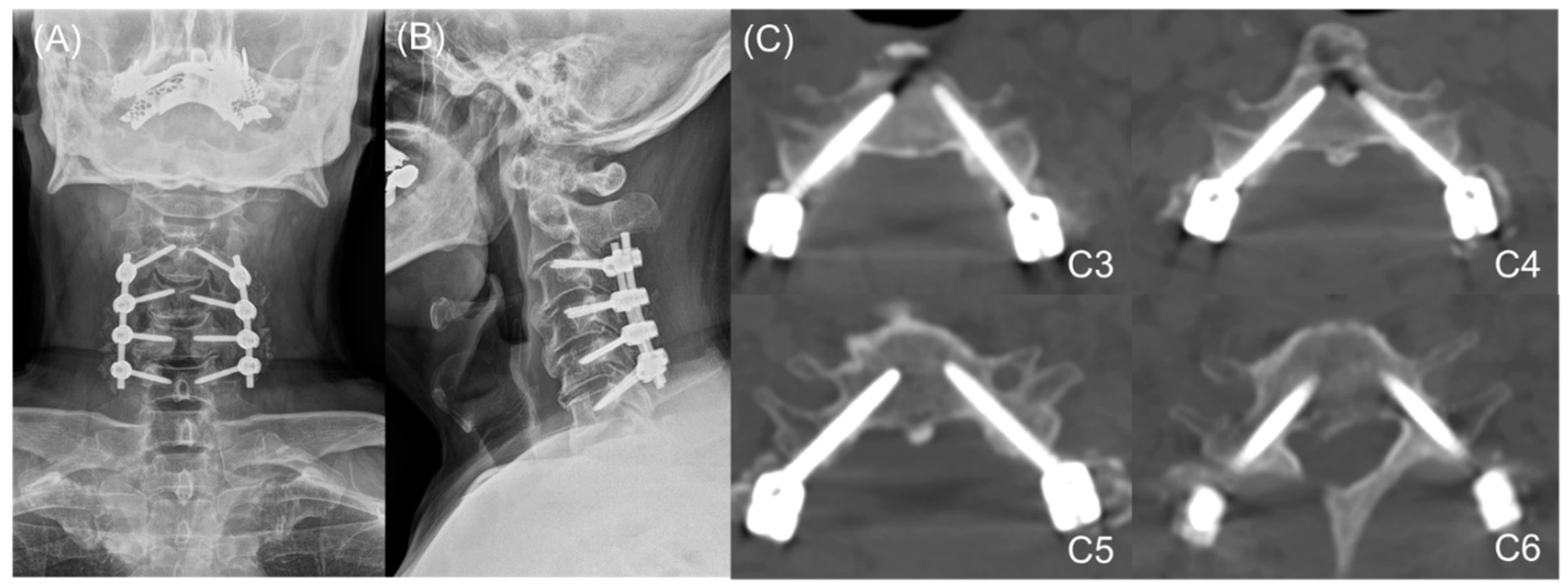
Medial Pedicle Pivot Point Using Preoperative Computed Tomography Morphometric Measurements for Cervical Pedicle Screw Insertion: A Novel Technique and Case Series
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographic and Operative Data
3.2. Perforation Grades and Directions
3.3. Risk Factors for Perforation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cheung, J.P.Y.; Cheung, P.W.H.; Chiu, C.K.; Chan, C.Y.W.; Kwan, M.K. Variations in practice among asia–pacific surgeons and recommendations for managing cervical myelopathy: The first asia–pacific spine society collaborative study. Asian Spine J. 2019, 13, 45. [Google Scholar] [CrossRef]
- Tracy, J.A.; Bartleson, J. Cervical spondylotic myelopathy. Neurologist 2010, 16, 176–187. [Google Scholar]
- Zhang, R.; Shen, C.; Zhang, J.; Zhang, X.; Dong, F.; Tao, H.; Song, P.; Ge, P.; Xu, P.; Zhang, H. Clinical features and surgical outcomes of cervical spondylotic myelopathy in patients of different ages: A retrospective study. Spinal Cord 2018, 56, 7–13. [Google Scholar] [PubMed] [Green Version]
- Choi, S.H.; Kang, C.N. Degenerative cervical myelopathy: Pathophysiology and current treatment strategies. Asian Spine J. 2020, 14, 710–720. [Google Scholar] [PubMed]
- Guzman, J.Z.; Feldman, Z.M.; McAnany, S.; Hecht, A.C.; Qureshi, S.A.; Cho, S.K. Osteoporosis in cervical spine surgery. Spine 2016, 41, 662–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghori, A.; Le, H.V.; Makanji, H.; Cha, T. Posterior fixation techniques in the subaxial cervical spine. Cureus 2015, 7, e338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwon, J.-W.; Bang, S.H.; Park, T.H.; Lee, S.-J.; Lee, H.-M.; Lee, S.-B.; Lee, B.H.; Moon, S.-H. Biomechanical comparison of cervical discectomy/fusion model using allograft spacers between anterior and posterior fixation methods (lateral mass and pedicle screw). Clin. Biomech. 2020, 73, 226–233. [Google Scholar]
- Ito, Z.; Higashino, K.; Kato, S.; Kim, S.S.; Wong, E.; Yoshioka, K.; Hutton, W.C. Pedicle screws can be 4 times stronger than lateral mass screws for insertion in the midcervical spine: A biomechanical study on strength of fixation. Clin. Spine Surg. 2014, 27, 80–85. [Google Scholar]
- Nakashima, H.; Yukawa, Y.; Imagama, S.; Kanemura, T.; Kamiya, M.; Yanase, M.; Ito, K.; Machino, M.; Yoshida, G.; Ishikawa, Y. Complications of cervical pedicle screw fixation for nontraumatic lesions: A multicenter study of 84 patients. J. Neurosurg. Spine 2012, 16, 238–247. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.-B.; Lee, H.-M.; Park, T.-H.; Lee, S.J.; Kwon, Y.-W.; Moon, S.-H.; Lee, B.H. Biomechanical comparison of posterior fixation combinations with an allograft spacer between the lateral mass and pedicle screws. Appl. Sci. 2020, 10, 7291. [Google Scholar]
- Oikonomidis, S.; Beyer, F.; Meyer, C.; Baltin, C.T.; Eysel, P.; Bredow, J. Insertion angle of pedicle screws in the subaxial cervical spine: The analysis of computed tomography-navigated insertion of pedicle screws. Asian Spine J. 2020, 14, 66. [Google Scholar] [CrossRef]
- Sundaram, P.P.M.; Oh, J.Y.; Tan, M.; Nolan, C.P.; Yu, C.S.; Ling, J.M. Accuracy of thoracolumbar pedicle screw insertion based on routine use of intraoperative imaging and navigation. Asian Spine J. 2021, 15, 491–497. [Google Scholar] [CrossRef]
- Luther, N.; Iorgulescu, J.B.; Geannette, C.; Gebhard, H.; Saleh, T.; Tsiouris, A.J.; Härtl, R. Comparison of navigated versus non-navigated pedicle screw placement in 260 patients and 1434 screws: Screw accuracy, screw size, and the complexity of surgery. J. Spinal Disord. Tech. 2015, 28, E298–E303. [Google Scholar] [CrossRef]
- Karaikovic, E.E.; Yingsakmongkol, W.; Gaines, R.W., Jr. Accuracy of cervical pedicle screw placement using the funnel technique. Spine (Phila Pa 1976) 2001, 26, 2456–2462. [Google Scholar] [CrossRef]
- Lee, J.H.; Choi, B.K.; Han, I.H.; Choi, W.G.; Nam, K.H.; Kim, H.S. Cervical pedicle screw placement using medial funnel technique. Korean J. Spine 2017, 14, 84–88. [Google Scholar]
- Abumi, K. Cervical spondylotic myelopathy: Posterior decompression and pedicle screw fixation. Eur. Spine J. 2015, 24, 186–196. [Google Scholar]
- Abumi, K.; Itoh, H.; Taneichi, H.; Kaneda, K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: Description of the techniques and preliminary report. J. Spinal Disord. 1994, 7, 19–28. [Google Scholar]
- Liu, B.; Liu, X.; Shen, X.; Wang, G.; Chen, Y. The “slide technique”-a novel free-hand method of subaxial cervical pedicle screw placement. BMC Musculoskelet. Disord. 2020, 21, 399. [Google Scholar]
- Jo, D.-J.; Seo, E.-M.; Kim, K.-T.; Kim, S.-M.; Lee, S.-H. Cervical pedicle screw insertion using the technique with direct exposure of the pedicle by laminoforaminotomy. J. Korean Neurosurg. Soc. 2012, 52, 459. [Google Scholar]
- Schroeder, G.D.; Canseco, J.A.; Patel, P.D.; Divi, S.N.; Karamian, B.A.; Kandziora, F.; Vialle, E.N.; Oner, F.C.; Schnake, K.J.; Dvorak, M.F.; et al. Establishing the injury severity of subaxial cervical spine trauma: Validating the hierarchical nature of the ao spine subaxial cervical spine injury classification system. Spine (Phila Pa 1976) 2021, 46, 649–657. [Google Scholar] [CrossRef]
- Canseco, J.A.; Schroeder, G.D.; Patel, P.D.; Grasso, G.; Chang, M.; Kandziora, F.; Vialle, E.N.; Oner, F.C.; Schnake, K.J.; Dvorak, M.F.; et al. Regional and experiential differences in surgeon preference for the treatment of cervical facet injuries: A case study survey with the ao spine cervical classification validation group. Eur. Spine J. 2021, 30, 517–523. [Google Scholar]
- Liu, Y.; Zhang, B.; Dai, M.; Xiong, H.-C.; Gao, S.; Li, B.-H.; Yao, H.-Q.; Cao, K.; Liu, Z.-L. Anatomic study of individualized and improved pedicle screw implantation in the lower cervical spine. Int. Surg. 2015, 100, 328–333. [Google Scholar] [CrossRef] [Green Version]
- Luo, J.; Wu, C.; Huang, Z.; Pan, Z.; Li, Z.; Zhong, J.; Chen, Y.; Han, Z.; Cao, K. The accuracy of the lateral vertebral notch-referred pedicle screw insertion technique in subaxial cervical spine: A human cadaver study. Arch. Orthop. Trauma Surg. 2017, 137, 517–522. [Google Scholar]
- Lee, K.H.; Yue, W.M.; Yeo, W.; Soeharno, H.; Tan, S.B. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur. Spine J. 2012, 21, 2265–2270. [Google Scholar] [CrossRef]
- Eldin, M.M.M. Cervical pedicle screw fixation: Anatomic feasibility of pedicle morphology and radiologic evaluation of the anatomical measurements. Asian Spine J. 2014, 8, 273. [Google Scholar] [CrossRef] [Green Version]
- Panjabi, M.M.; Duranceau, J.; Goel, V.; Oxland, T.; Takata, K. Cervical human vertebrae. Quantitative three-dimensional anatomy of the middle and lower regions. Spine (Phila Pa 1976) 1991, 16, 861–869. [Google Scholar]
- Jones, E.L.; Heller, J.G.; Silcox, D.H.; Hutton, W.C. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine (Phila Pa 1976) 1997, 22, 977–982. [Google Scholar] [CrossRef]
- Abumi, K.; Kaneda, K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1997, 22, 1853–1863. [Google Scholar] [CrossRef] [PubMed]
- Munusamy, T.; Thien, A.; Anthony, M.G.; Bakthavachalam, R.; Dinesh, S.K. Computed tomographic morphometric analysis of cervical pedicles in a multi-ethnic asian population and relevance to subaxial cervical pedicle screw fixation. Eur. Spine J. 2015, 24, 120–126. [Google Scholar]
- Pech, P.; Daniels, D.; Williams, A.; Haughton, V. The cervical neural foramina: Correlation of microtomy and ct anatomy. Radiology 1985, 155, 143–146. [Google Scholar] [CrossRef]
- Park, H.-J.; Kwon, K.-Y.; Yoon, W.-S. Ideal insertion point and angle of cervical pedicular screws in korean. J. Korean Soc. Spine Surg. 2013, 20, 169–177. [Google Scholar] [CrossRef] [Green Version]
- Park, J.H.; Jeon, S.R.; Roh, S.W.; Kim, J.H.; Rhim, S.C. The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: A series of 45 consecutive patients. Spine 2014, 39, 280–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tukkapuram, V.R.; Kuniyoshi, A.; Ito, M. A review of the historical evolution, biomechanical advantage, clinical applications, and safe insertion techniques of cervical pedicle screw fixation. Spine Surg. Relat. Res. 2018, 3, 126–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burcev, A.V.; Pavlova, O.M.; Diachkov, K.A.; Diachkova, G.V.; Ryabykh, S.O.; Gubin, A.V. Easy method to simplify “freehand” subaxial cervical pedicle screw insertion. J. Craniovertebral Junction Spine 2017, 8, 390. [Google Scholar]





| Pedicle Diameter (mm) | Pedicle Insertion Angle (Degrees) | Lateral Mass Depth (mm) | Facet-Pedicle Distance (mm) | Pedicle Total Length (mm) | |
|---|---|---|---|---|---|
| C3 | 4.22 ± 1.85 | 46.49 ± 5.44 | 8.45 ± 1.93 | 3.58 ± 1.94 | 30.30 ± 3.26 |
| C4 | 4.41 ± 1.62 | 47.28 ± 5.22 | 8.02 ± 1.50 | 3.14 ± 1.80 | 29.88 ± 3.52 |
| C5 | 4.38 ± 1.12 | 46.00 ± 5.80 | 8.32 ± 2.04 | 3.00 ± 1.39 | 31.20 ± 3.29 |
| C6 | 5.23 ± 4.79 | 42.36 ± 5.49 | 8.47 ± 1.79 | 3.66 ± 1.61 | 32.53 ± 4.45 |
| C7 | 5.49 ± 1.10 | 40.24 ± 7.57 | 6.79 ± 1.40 | 3.93 ± 3.20 | 31.16 ± 4.06 |
| Perforation Grade and Rate | Cervical Level | |||||
|---|---|---|---|---|---|---|
| C3 (n = 38) | C4 (n = 48) | C5 (n = 51) | C6 (n = 66) | C7 (n = 68) | Total (n = 271) | |
| Grade | ||||||
| 0 (No Perforation) | 30 | 33 | 41 | 50 | 63 | 217 (80.1%) |
| 1 | 6 | 14 | 6 | 13 | 5 | 44 (16.2%) |
| 2 | 2 | 1 | 4 | 3 | 0 | 10 (3.7%) |
| 3 | 0 | 0 | 0 | 0 | 0 | 0 (0.0%) |
| Perforation Rate (Grade 1 or Higher) | 8/38 (21.1%) | 15/48 (31%) | 10/51 (19.6%) | 16/66 (24.2%) | 5/68 (7.4%) | 54/271 (19.9%) |
| Direction of Perforation | Grade of Perforation | Total | ||
|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | ||
| Medial | 32 | 7 | 0 | 39 (72.2%) |
| Lateral | 12 | 3 | 0 | 15 (27.7%) |
| Cranial | 0 | 0 | 0 | 0 (0.0%) |
| Caudal | 0 | 0 | 0 | 0 (0.0%) |
| Total | 44 (81.5%) | 10 (18.5%) | 0 | 54 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, J.-W.; Arreza, E.O.; Suguitan, A.A.; Lee, S.-B.; Sung, S.; Park, Y.; Ha, J.-W.; Kim, T.H.; Moon, S.-H.; Lee, B.H. Medial Pedicle Pivot Point Using Preoperative Computed Tomography Morphometric Measurements for Cervical Pedicle Screw Insertion: A Novel Technique and Case Series. J. Clin. Med. 2022, 11, 396. https://doi.org/10.3390/jcm11020396
Kwon J-W, Arreza EO, Suguitan AA, Lee S-B, Sung S, Park Y, Ha J-W, Kim TH, Moon S-H, Lee BH. Medial Pedicle Pivot Point Using Preoperative Computed Tomography Morphometric Measurements for Cervical Pedicle Screw Insertion: A Novel Technique and Case Series. Journal of Clinical Medicine. 2022; 11(2):396. https://doi.org/10.3390/jcm11020396
Chicago/Turabian StyleKwon, Ji-Won, Edward O. Arreza, Anthony A. Suguitan, Soo-Bin Lee, Sahyun Sung, Yung Park, Joong-Won Ha, Tae Hyung Kim, Seong-Hwan Moon, and Byung Ho Lee. 2022. "Medial Pedicle Pivot Point Using Preoperative Computed Tomography Morphometric Measurements for Cervical Pedicle Screw Insertion: A Novel Technique and Case Series" Journal of Clinical Medicine 11, no. 2: 396. https://doi.org/10.3390/jcm11020396
APA StyleKwon, J.-W., Arreza, E. O., Suguitan, A. A., Lee, S.-B., Sung, S., Park, Y., Ha, J.-W., Kim, T. H., Moon, S.-H., & Lee, B. H. (2022). Medial Pedicle Pivot Point Using Preoperative Computed Tomography Morphometric Measurements for Cervical Pedicle Screw Insertion: A Novel Technique and Case Series. Journal of Clinical Medicine, 11(2), 396. https://doi.org/10.3390/jcm11020396






