Interventional Radiological Management and Prevention of Complications after Pancreatic Surgery: Drainage, Embolization and Islet Auto-Transplantation
Abstract
:1. Introduction
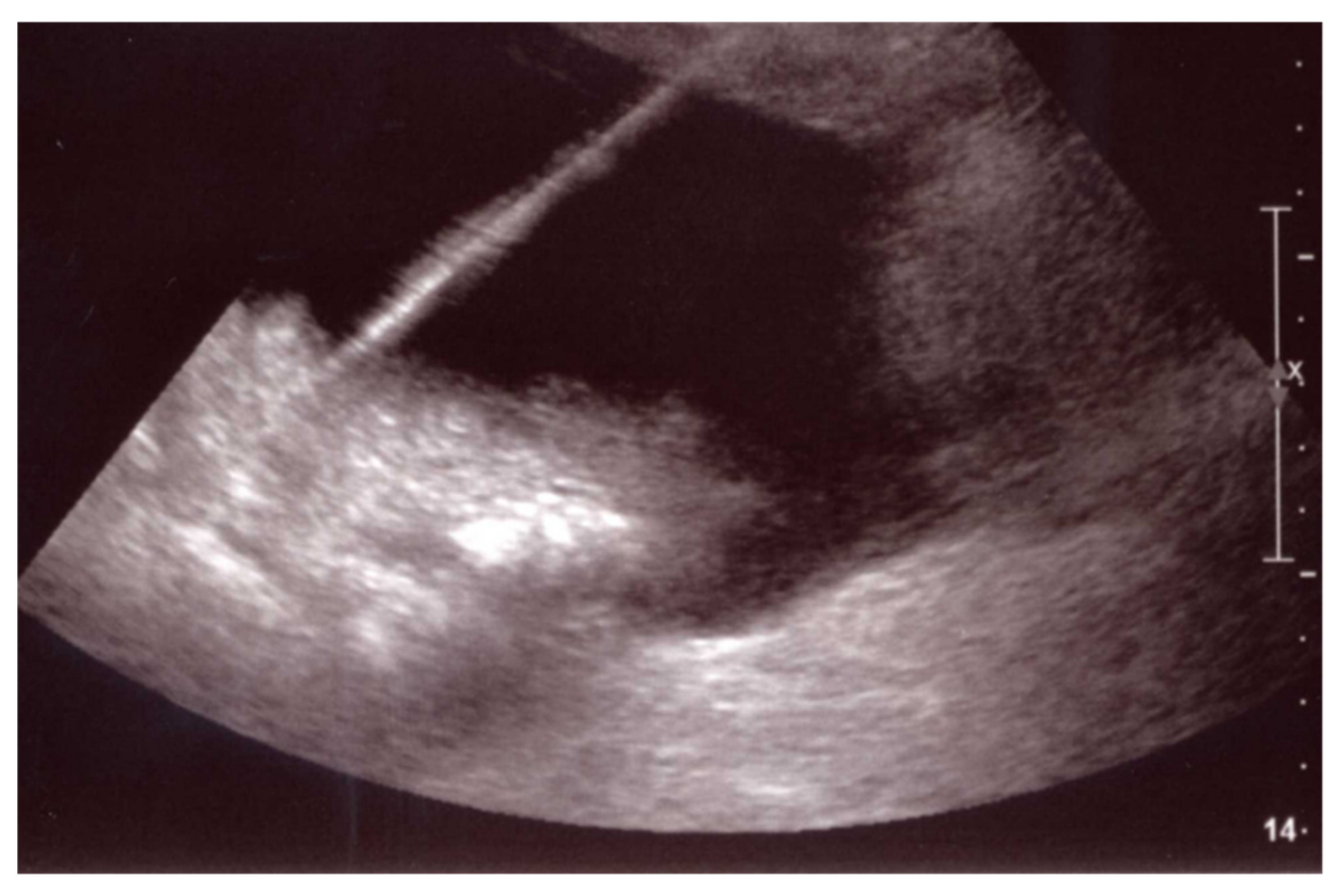
2. Percutaneous Fluid Collection Drainage
3. Percutaneous Transhepatic Biliary Drainage
4. Transcatheter Embolization (Stent–Graft)
5. Intra-Portal Islet Auto-Transplantation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ryan, D.P.; Hong, T.S.; Bardeesy, N. Pancreatic adenocarcinoma. N. Engl. J. Med. 2014, 371, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Uysal, A.; Una, E.; Karaosmanoglu, A.D.; Arellano, R.; Ciftci, T.T.; Akinci, D.; Akhan, O. The role of interventional radiology in the treatment of patients with pancreatic cancer. Br. J. Radiol. 2021, 94, 20200702. [Google Scholar] [CrossRef] [PubMed]
- Squadroni, M.; Fazio, N. Chemotherapy in pancreatic adenocarcinoma. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 386–394. [Google Scholar] [PubMed]
- Busch, E.; Werft, W.; Bougatf, N.; Hackert, T.; Jäger, D.; Springfeld, C.; Berger, A.K. Metastatic acinar cell carcinoma of the pancreas: A retrospective cohort study on systemic chemotherapy and review of the literature. Pancreas 2021, 50, 300–305. [Google Scholar] [CrossRef]
- Sarantis, P.; Koustas, E.; Papadimitropoulou, A.; Papavassiliou, A.G.; Karamouzis, M.V. Pancreatic ductal adenocarcinoma: Treatment hurdles, tumor microenvironment and immunotherapy. World J. Gastrointest. Oncol. 2020, 12, 173–181. [Google Scholar] [CrossRef]
- Brind’Amour, A.; Webb, M.; Parapini, M.; Sidéris, L.; Segedi, M.; Chung, S.W.; Chartier-Plante, S.; Dubé, P.; Scudamore, C.H.; Kim, P.T.W. The role of intraperitoneal chemotherapy in the surgical management of pancreatic ductal adenocarcinoma: A systematic review. Clin. Exp. Metastasis 2021, 38, 187–196. [Google Scholar] [CrossRef]
- Palmieri, L.S.; Barré, A.; Dhooge, M.; Brezault, C.; Cottereau, A.S.; Coriat, R. Medical treatment of advanced pancreatic neuroendocrine neoplasms. J. Clin. Med. 2020, 9, 1860. [Google Scholar] [CrossRef]
- Touloupas, C.; Faron, M.; Hadoux, J.; Deschamps, F.; Roux, C.; Ronot, M.; Yevich, S.; Joskin, J.; Gelli, M.; Barbé, R.; et al. Long term efficacy and assessment of tumor response of transarterial chemoembolization in neuroendocrine liver metastases: A 15-year monocentric experience. Cancers 2021, 13, 5366. [Google Scholar] [CrossRef]
- Aldrighetti, L.; Arru, M.; Angeli, E.; Venturini, M.; Salvioni, M.; Ronzoni, M.; Caterini, R.; Ferla, G. Percutaneous vs. surgical placement of hepatic artery indwelling catheters for regional chemotherapy. Hepatogastroenterology 2002, 49, 513–517. [Google Scholar]
- Simon, R. Complications After Pancreaticoduodenectomy. Surg. Clin. N. Am. 2021, 101, 865–874. [Google Scholar] [CrossRef]
- Narayanan, S.; Martin, A.N.; Turrentine, F.E.; Bauer, T.W.; Adams, R.B.; Zaydfudim, V.M. Mortality after pancreaticoduodenectomy: Assessing early and late causes of patient death. J. Surg. Res. 2018, 231, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Shaib, W.L.; Zakka, K.; Hoodbhoy, F.N.; Belalcazar, A.; Kim, S.; Cardona, K.; Russell, M.C.; Maithel, S.K.; Sarmiento, J.M.; Wu, C.; et al. In-hospital 30-day mortality for older patients with pancreatic cancer undergoing pancreaticoduodenectomy. J. Geriatr. Oncol. 2020, 11, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Standop, J.; Glowka, T.; Schmitz, V.; Schäfer, N.; Overhaus, M.; Hirner, A.; Kalff, J.C. Operative re-intervention following pancreatic head resection: Indications and outcome. J. Gastrointest. Surg. 2009, 13, 1503–1509. [Google Scholar] [CrossRef] [PubMed]
- Buchler, M.W.; Wagner, M.; Schmied, B.M.; Uhl, W.; Friess, H.; Z’Graggen, K. Changes in morbidity after pancreatic resection: Toward the end of completion pancreatectomy. Arch. Surg. 2003, 138, 1310–1314. [Google Scholar] [CrossRef]
- Mauri, G.; Mattiuz, C.; Sconfienza, L.M.; Pedicini, V.; Poretti, D.; Melchiorre, F.; Rossi, U.; Lutman, F.R.; Montorsi, M. Role of interventional radiology in the management of complications after pancreatic surgery: A pictorial review. Insights Imaging 2015, 6, 231–239. [Google Scholar] [CrossRef] [Green Version]
- Casadei, R.; Ricci, C.; Giampalma, E.; D’Ambra, M.; Taffurelli, G.; Mosconi, C.; Golfieri, R.; Minni, F. Interventional radiology procedures after pancreatic resections for pancreatic and periampullary diseases. JOP 2014, 15, 378–382. [Google Scholar] [CrossRef]
- Putzer, D.; Schullian, P.; Stättner, S.; Primavesi, F.; Braunwarth, E.; Fodor, M.; Cardini, B.; Resch, T.; Oberhuber, R.; Maglione, M.; et al. Interventional management after complicated pancreatic surgery. Eur. Surg. 2019, 51, 105–113. [Google Scholar] [CrossRef] [Green Version]
- Balzano, G.; Maffi, P.; Nano, R.; Zerbi, A.; Venturini, M.; Melzi, R.; Mercalli, A.; Magistretti, P.; Scavini, M.; Castoldi, R.; et al. Extending indications for islet autotransplantation in pancreatic surgery. Ann. Surg. 2013, 258, 210–218. [Google Scholar] [CrossRef]
- Balzano, G.; Maffi, P.; Nano, R.; Mercalli, A.; Melzi, R.; Aleotti, F.; Cobelli, F.D.; Magistretti, P.; Scavini, M.; Secchi, A.; et al. Diabetes-free survival after extended distal pancreatectomy and islet auto transplantation for benign or borderline/malignant lesions of the pancreas. Am. J. Transplant 2019, 19, 920–928. [Google Scholar] [CrossRef]
- Venturini, M.; Sallemi, C.; Colantoni, C.; Agostini, G.; Balzano, G.; Esposito, A.; Secchi, A.; Cobelli, F.D.; Falconi, M.; Piemonti, L.; et al. Single-centre experience of extending indications for percutaneous intraportal islet autotransplantation (PIPIAT) after pancreatic surgery to prevent diabetes: Feasibility, radiological aspects, complications and clinical outcome. Br. J. Radiol. 2016, 89, 20160246. [Google Scholar] [CrossRef]
- Kumar, R.; Chung, W.; Dennison, A.R.; Garcea, G. Current principles and practice in autologous intraportal islet transplantation: A meta-analysis of the technical considerations. Clin. Transplant 2016, 30, 344–356. [Google Scholar] [CrossRef] [PubMed]
- Dunn, T.B.; Wilhelm, J.J.; Bellin, M.D.; Pruett, T.L. Autologous islet transplantation: Challenges and lessons. Curr. Opin. Organ. Transplant 2017, 22, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Sohn, T.A.; Yeo, C.J.; Cameron, J.L.; Koniaris, L.; Kaushal, S.; Abrams, R.A.; Sauter, P.K.; Coleman, J.; Hruban, R.H.; Lillemoe, K.D. Resected adenocarcinoma of the pancreas-616 patients: Results, outcomes, and prognostic indicators. J. Gastrointest. Surg. 2000, 4, 567–579. [Google Scholar] [CrossRef]
- Gervais, D.A.; Castillo, C.F.-D.; O’Neill, M.J.; Hahn, P.F.; Mueller, P.R. Complications after pancreatoduodenectomy: Imaging and imaging-guided interventional procedures. Radiographics 2001, 21, 673–690. [Google Scholar] [CrossRef] [PubMed]
- Bassi, C.; Dervenis, C.; Butturini, G.; Fingerhut, A.; Yeo, C.; Izbicki, J.; Neoptolemos, J.; Sarr, M.; Traverso, W.; Buchler, M.; et al. Postoperative pancreatic fistula: An international study group (ISGPF) definition. Surgery 2005, 138, 8–13. [Google Scholar] [CrossRef]
- Li, X.; Paz-Fumagalli, R.; Wang, W.; Toskich, B.B.; Stauffer, J.A.; Frey, G.T.; McKinney, J.M.; Nguyen, J.H. Percutaneous direct pancreatic duct intervention in management of pancreatic fistulas: A primary treatment or temporizing therapy to prepare for elective surgery. BMC Gastroenterol. 2021, 21, 44. [Google Scholar] [CrossRef]
- Mercado, M.A.; Domínguez, I. Classification and management of bile duct injuries. World J. Gastrointest. Surg. 2011, 3, 43–48. [Google Scholar] [CrossRef]
- Iacono, C.; Verlato, G.; Ruzzenente, A.; Campagnaro, T.; Bacchelli, C.; Valdegamberi, A.; Bortolasi, L.; Guglielmi, A. Systematic review of central pancreatectomy and meta-analysis of central versus distal pancreatectomy. Br. J. Surg. 2013, 100, 873–885. [Google Scholar] [CrossRef]
- Larsen, M.; Kozarek, R. Management of pancreatic ductal leaks and fistulae. J. Gastroenterol. Hepatol. 2014, 29, 1360–1370. [Google Scholar] [CrossRef]
- Zink, S.I.; Soloff, E.V.; White, R.R.; Clary, B.M.; Tyler, D.S.; Pappas, T.N.; Paulson, E.K. Pancreaticoduodenectomy: Frequency and outcome of post-operative imaging-guided percutaneous drainage. Abdom. Imaging 2009, 34, 767–771. [Google Scholar] [CrossRef] [PubMed]
- Hoyt, A.C.; D’Agostino, H.B.; Carrillo, A.J.; Vasconcellos-Viera, M.; Kim, S.; O’Laoide, R.; vanSonnenberg, E. Drainage efficiency of double-lumen sump catheters and single-lumen catheters: An in vitro comparison. J. Vasc. Interv. Radiol. 1997, 8, 267–270. [Google Scholar] [CrossRef]
- Roberts, D.G.; Goudie, M.J.; Kim, A.J.; Kim, H.; Khademhosseini, A.; McWilliams, J.P. Novel dual-lumen drainage catheter to enhance the active evacuation of complex fluid collections. J. Vasc. Interv. Radiol. 2021, 32, 882–889. [Google Scholar] [CrossRef]
- Hirota, M.; Kanemitsu, K.; Takamori, H.; Chikamoto, A.; Hayashi, N.; Horino, K.; Baba, H. Percutaneous transfistulous pancreatic duct drainage and interventional pancreatojejunostomy as a treatment option for intractable pancreatic fistula. Am. J. Surg. 2008, 196, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Codina, J.; Gelabert, A.; Casellas, M.; Borreguero, D.P.; Huertas, C.; Falgueras, L.; Pedraza, S. Percutaneous Plastic Stent Insertion for Treatment of Disconnected Pancreatic Duct. J. Vasc. Interv. Radiol. 2017, 28, 1203–1205. [Google Scholar] [CrossRef] [PubMed]
- Hirota, M. Percutaneous transfistulous interventions for intractable pancreatic fistula. Radiol. Res. Pract. 2011, 2011, 109259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keane, M.G.; Sze, S.F.; Cieplik, N.; Murray, S.; Johnson, G.J.; Webster, G.J.; Thorburn, D.; Pereira, S.P. Endoscopic versus percutaneous drainage of symptomatic pancreatic fuid collections: A 14-year experience from a tertiary hepatobiliary centre. Surg. Endosc. 2016, 30, 3730–3740. [Google Scholar] [CrossRef] [Green Version]
- Lau, S.T.; Simchuk, E.J.; Kozarek, R.A.; Traverso, L.W. A pancreatic ductal leak should be sought to direct treatment in patients with acute pancreatitis. Am. J. Surg. 2001, 181, 411–415. [Google Scholar] [CrossRef]
- Kozarek, R.A. Pancreatic endoscopy. Endoscopy 2008, 40, 55–60. [Google Scholar] [CrossRef]
- Pearson, E.G.; Scaife, C.L.; Mulvihill, S.J.; Glasgow, R.E. Roux-en-Y drainage of a pancreatic fistula for disconnected pancreatic duct syndrome after acute necrotizing pancreatitis. HPB 2012, 14, 26–31. [Google Scholar] [CrossRef] [Green Version]
- Howard, T.J.; Stonerock, C.E.; Sarkar, J.; Lehman, G.A.; Sherman, S.; Wiebke, E.A.; Madura, J.A.; Broadie, T.A. Contemporary treatment strategies for external pancreatic fistulas. Surgery 1998, 124, 627–633. [Google Scholar] [CrossRef]
- Irani, S.; Gluck, M.; Ross, A.; Gan, S.I.; Crane, R.; Brandabur, J.J.; Hauptmann, E.; Fotoohi, M.; Kozarek, R.A. Resolving external pancreatic fistulas in patients with disconnected pancreatic duct syndrome: Using rendezvous techniques to avoid surgery (with video). Gastrointest. Endosc. 2012, 76, 586–593.e933. [Google Scholar] [CrossRef] [PubMed]
- Azeem, N.; Baron, T.H.; Topazian, M.D.; Zhong, N.; Fleming, C.J.; Kendrick, M.L. Outcomes of endoscopic and percutaneous drainage of pancreatic fluid collections arising after pancreatic tail resection. J. Am. Coll. Surg. 2012, 215, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Mosconi, C.; Calandri, M.; Mirarchi, M.; Vara, G.; Breatta, A.D.; Cappelli, A.; Brandi, N.; Paccapelo, A.; Benedittis, C.D.; Ricci, C.; et al. Percutaneous management of postoperative Bile leak after hepato-pancreato-biliary surgery: A multi-center experience. HPB 2021, 23, 1518–1524. [Google Scholar] [CrossRef] [PubMed]
- Henry, A.C.; Smits, F.J.; van Lienden, K.; van den Heuvel, D.A.F.; Hofman, L.; Busch, O.R.; van Delden, O.M.; Zijlstra, I.A.; Schreuder, S.M.; Lamers, A.B.; et al. Biliopancreatic and biliary leak after pancreatoduodenectomy treated by percutaneous transhepatic biliary drainage. HPB 2022, 24, 489–497. [Google Scholar] [CrossRef]
- Pedicini, V.; Poretti, D.; Mauri, G.; Trimboli, M.; Brambilla, G.; Sconfienza, L.M.; Cornalba, G.; Sardanelli, F. Management of post-surgical biliary leakage with percutaneous transhepatic biliary drainage (PTBD) and occlusion balloon (OB) in patients without dilatation of the biliary tree: Preliminary results. Eur. Radiol. 2010, 20, 1061–1068. [Google Scholar] [CrossRef]
- Mansueto, G.; Gatti, F.L.; Boninsegna, E.; Conci, S.; Guglielmi, A.; Contro, A. Biliary leakage after hepatobiliary and pancreatic surgery: A classification system to guide the proper percutaneous treatment. Cardiovasc. Interv. Radiol. 2020, 43, 302–310. [Google Scholar] [CrossRef]
- Koch, M.; Garden, O.J.; Padbury, R.; Rahbari, N.N.; Adam, R.; Capussotti, L.; Fan, S.T.; Yokoyama, Y.; Crawford, M.; Makuuchi, M.; et al. Bile leakage after hepatobiliary and pancreatic surgery: A definition and grading of severity by the International Study Group of Liver Surgery. Surgery 2011, 149, 680–688. [Google Scholar] [CrossRef]
- Jin, S.; Fu, Q.; Wuyun, G.; Wuyun, T. Management of post-hepatectomy complications. World J. Gastroenterol. 2013, 19, 7983–7991. [Google Scholar] [CrossRef]
- Sakamoto, K.; Tamesa, T.; Yukio, T.; Tokuhisa, Y.; Maeda, Y.; Oka, M. Risk Factors and Managements of Bile Leakage After Hepatectomy. World J. Surg. 2016, 40, 182–189. [Google Scholar] [CrossRef] [Green Version]
- Houghton, E.J.; Zeledón, M.; Acquafresca, P.; Finger, C.; Palermo, M.; Giménez, M.E. Prospective comparison of bleeding complications between right and left approaches in percutaneous biliary drainage. Surg. Laparosc. Endosc. Percutan Tech. 2019, 29, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Giurazza, F.; Corvino, F.; Contegiacomo, A.; Marra, P.; Lucarelli, N.M.; Calandri, M.; Silvestre, M.; Corvino, A.; Lucatelli, P.; Cobelli, F.D.; et al. Safety and effectiveness of ultrasound-guided percutaneous transhepatic biliary drainage: A multicenter experience. J. Ultrasound 2019, 22, 437–445. [Google Scholar] [CrossRef]
- Duan, F.; Cui, L.; Bai, Y.; Li, X.; Yan, J.; Liu, X. Comparison of efficacy and complications of endoscopic and percutaneous biliary drainage in malignant obstructive jaundice: A systematic review and meta-analysis. Cancer Imaging 2017, 17, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.H.; Oh, J.H.; Yoon, Y.; Hong, S.H.; Park, S.J. Acetic acid sclerotherapy for treatment of a biliary leak from an isolated bile duct after hepatic surgery. J. Vasc. Interv. Radiol. 2005, 16, 885–888. [Google Scholar] [CrossRef] [PubMed]
- Gwon, D.I.; Ko, G.Y.; Sung, K.B.; Kim, J.H.; Yoon, H.K. Percutaneous transhepatic treatment of postoperative bile leaks: Prospective evaluation of retrievable covered stent. J. Vasc. Interv. Radiol. 2011, 22, 75–83. [Google Scholar] [CrossRef]
- Bottari, A.; Silipigni, S.; Stagno, A.; Caloggero, S. Bilio-cutaneous fistula obliteration with NBCA. Indian J. Radiol. Imaging 2019, 29, 310–312. [Google Scholar] [CrossRef]
- Alberto, S.; Salvatore, S.; Marco, T.; Socrate, P.; Antonella, C.; Francesca, C.; Simona, C.; Antonio, B. Embolization of extrahepatic biliary leakage using NBCA. Radiol. Case Rep. 2021, 16, 1315–1319. [Google Scholar] [CrossRef]
- Nunes, T.F.; Tibana, T.K.; Pereira, M.E.S.; Marchiori, E. Treatment of extrahepatic biliary fistulas using n-butyl cyanoacrylate. Radiol. Bras. 2019, 52, 174–175. [Google Scholar] [CrossRef]
- Huo, Y.; Chi, J.; Zhang, J.; Liu, W.; Liu, D.; Li, J.; Yang, J.; Hua, R.; Sun, Y. Endovascular intervention for delayed post-pancreaticoduodenectomy hemorrhage: Clinical features and outcomes of transcatheter arterial embolization and covered stent placement. Int. J. Clin. Exp. Med. 2015, 8, 7457–7466. [Google Scholar]
- Pottier, E.; Ronot, M.; Gaujoux, S.; Cesaretti, M.; Barbier, L.; Sauvanet, A.; Vilgrain, V. Endovascular management of delayed post-pancreatectomy haemorrhage. Eur. Radiol. 2016, 26, 3456–3465. [Google Scholar] [CrossRef]
- Biondetti, P.; Fumarola, E.M.; Ierardi, A.M.; Carrafiello, G. Bleeding complications after pancreatic surgery: Interventional radiology management. Gland. Surg. 2019, 8, 150–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venturini, M.; Marra, P.; Colombo, M.; Alparone, M.; Agostini, G.; Bertoglio, L.; Sallemi, C.; Salvioni, M.; Gusmini, S.; Balzano, G.; et al. Endovascular treatment of visceral artery aneurysms and pseudoaneurysms in 100 patients: Covered stenting vs transcatheter embolization. J. Endovasc. Ther. 2017, 24, 709–717. [Google Scholar] [CrossRef]
- Kasumova, G.G.; Eskander, M.F.; Kent, T.S.; Ng, S.C.; Moser, A.J.; Ahmed, M.; Pleskow, D.K.; Callery, M.P.; Tseng, J.F. Hemorrhage after pancreaticoduodenectomy: Does timing matter? HPB 2016, 18, 861–869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grützmann, R.; Rückert, F.; Hippe-Davies, N.; Distler, M.; Saeger, H.D. Evaluation of the International Study Group of Pancreatic Surgery definition of post-pancreatectomy hemorrhage in a high-volume center. Surgery 2012, 151, 612–620. [Google Scholar] [CrossRef]
- Jilesen, A.P.; Tol, J.A.; Busch, O.R.; van Delden, O.M.; van Gulik, T.M.; van Dijkum, E.J.N.; Gouma, D.J. Emergency management in patients with late hemorrhage after pancreatoduodenectomy for a periampullary tumor. World J. Surg. 2014, 38, 2438–2447. [Google Scholar] [CrossRef] [PubMed]
- Wente, M.N.; Veit, J.A.; Bassi, C.; Dervenis, C.; Fingerhut, A.; Gouma, D.J.; Izbicki, J.R.; Neoptolemos, J.P.; Padbury, R.T.; Sarr, M.G.; et al. Postpancreatectomy hemorrhage (PPH): An International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007, 142, 20–25. [Google Scholar] [CrossRef]
- Devant, E.; Girard, E.; Abba, J.; Ghelfi, J.; Sage, P.Y.; Sengel, C.; Risse, O.; Bricault, I.; Trilling, B.; Chirica, M. Delayed Postoperative Hemorrhage Complicating Major Supramesocolic Surgery Management and Outcomes. World J. Surg. 2021, 45, 2432–2438. [Google Scholar] [CrossRef]
- Rajarathinam, G.; Kannan, D.G.; Vimalraj, V.; Amudhan, A.; Rajendran, S.; Jyotibasu, D.; Balachandar, T.G.; Jeswanth, S.; Ravichandran, P.; Surendran, R. Post pancreaticoduodenectomy haemorrhage: Outcome prediction based on new ISGPS clinical severity grading. HPB 2008, 10, 363–370. [Google Scholar] [CrossRef] [Green Version]
- Limongelli, P.; Khorsandi, S.E.; Pai, M.; Jackson, J.E.; Tait, P.; Tierris, J.; Habib, N.A.; Williamson, R.C.; Jiao, L.R. Management of delayed postoperative hemorrhage after pancreaticoduodenectomy: A meta-analysis. Arch. Surg. 2008, 143, 1001–1007. [Google Scholar] [CrossRef] [Green Version]
- de Castro, S.M.; Kuhlmann, K.F.; Busch, O.R.; van Delden, O.M.; Laméris, J.S.; van Gulik, T.M.; Obertop, H.; Gouma, D.J. Delayed massive hemorrhage after pancreatic and biliary surgery: Embolization or surgery? Ann. Surg. 2005, 241, 85–91. [Google Scholar] [CrossRef]
- Yamashita, Y.; Taketomi, A.; Fukuzawa, K.; Tsujita, E.; Harimoto, N.; Kitagawa, D.; Kuroda, Y.; Kayashima, H.; Wakasugi, K.; Maehara, Y. Risk factors for and management of delayed intraperitoneal hemorrhage after pancreatic and biliary surgery. Am. J. Surg. 2007, 193, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Hur, S.; Yoon, C.J.; Kang, S.G.; Dixon, R.; Han, H.S.; Yoon, Y.S.; Cho, J.Y. Transcatheter arterial embolization of gastroduodenal artery stump pseudoaneurysms after pancreaticoduodenectomy: Safety and efficacy of two embolization techniques. J. Vasc. Interv. Radiol. 2011, 22, 294–301. [Google Scholar] [CrossRef]
- Puppala, S.; Patel, J.; McPherson, S.; Nicholson, A.; Kessel, D. Hemorrhagic complications after Whipple surgery: Imaging and radiologic intervention. AJR Am. J. Roentgenol. 2011, 196, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Mañas-Gómez, M.J.; Rodríguez-Revuelto, R.; Balsells-Valls, J.; Olsina-Kissler, J.J.; Caralt-Barba, M.; Pérez-Lafuente, M.; Charco-Torra, R. Post-pancreaticoduodenectomy hemorrhage. Incidence, diagnosis, and treatment. World J. Surg. 2011, 35, 2543–2548. [Google Scholar] [CrossRef]
- Blanc, T.; Cortes, A.; Goere, D.; Sibert, A.; Pessaux, P.; Belghiti, J.; Sauvanet, A. Hemorrhage after pancreaticoduodenectomy: When is surgery still indicated? Am. J. Surg. 2007, 194, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Rossi, U.G.; Seitun, S.; Ferro, C. Endovascular embolization of a third jejunal artery aneurysm: Isolation technique using the Amplatzer Vascular Plug 4. Catheter. Cardiovasc. Interv. 2013, 81, 1049–1052. [Google Scholar] [CrossRef]
- Venturini, M.; Marra, P.; Augello, L.; Colarieti, A.; Guazzarotti, G.; Palumbo, D.; Lanza, C.; Melissano, G.; Chiesa, R.; Cobelli, F.D. Elective Embolization of Splenic Artery Aneurysms with an Ethylene Vinyl Alcohol Copolymer Agent (Squid) and Detachable Coils. J. Vasc. Interv. Radiol. 2020, 31, 1110–1117. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, J.; Jiang, J.; Shen, J. The Role of Interventional Radiology in the Management of Late Postpancreaticoduodenectomy Hemorrhage. Biomed. Res. Int. 2020, 2020, 8851950. [Google Scholar] [CrossRef]
- Hasegawa, T.; Ota, H.; Matsuura, T.; Seiji, K.; Mugikura, S.; Motoi, F.; Unno, M.; Takase, K. Endovascular Treatment of Hepatic Artery Pseudoaneurysm after Pancreaticoduodenectomy: Risk Factors Associated with Mortality and Complications. J. Vasc. Interv. Radiol. 2017, 28, 50–59.e5. [Google Scholar] [CrossRef]
- Ansari, D.; Tingstedt, B.; Lindell, G.; Keussen, I.; Ansari, D.; Andersson, R. Hemorrhage after Major Pancreatic Resection: Incidence, Risk Factors, Management, and Outcome. Scand. J. Surg. 2017, 106, 47–53. [Google Scholar] [CrossRef] [Green Version]
- Gaudon, C.; Soussan, J.; Louis, G.; Moutardier, V.; Gregoire, E.; Vidal, V. Late postpancreatectomy hemorrhage: Predictive factors of morbidity and mortality after percutaneous endovascular treatment. Diagn. Interv. Imaging 2016, 97, 1071–1077. [Google Scholar] [CrossRef] [PubMed]
- Hassold, N.; Wolfschmidt, F.; Dierks, A.; Klein, I.; Bley, T.; Kickuth, R. Effectiveness and outcome of endovascular therapy for late-onset postpancreatectomy hemorrhage using covered stents and embolization. J. Vasc. Surg. 2016, 64, 1373–1383. [Google Scholar] [CrossRef] [PubMed]
- Ching, K.C.; Santos, E.; McCluskey, K.M.; Orons, P.D.; Bandi, R.; Friend, C.J.; Xing, M.; Zureikat, A.H.; Zeh, H.J. Covered Stents and Coil Embolization for Treatment of Postpancreatectomy Arterial Hemorrhage. J. Vasc. Interv. Radiol. 2016, 27, 73–79. [Google Scholar] [CrossRef]
- Asari, S.; Matsumoto, I.; Toyama, H.; Yamaguchi, M.; Okada, T.; Shinzeki, M.; Goto, T.; Ajiki, T.; Fukumoto, T.; Ku, Y. Recommendation of treatment strategy for postpancreatectomy hemorrhage: Lessons from a single-center experience in 35 patients. Pancreatology 2016, 16, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Zhu, J.; Zhu, M.; Li, C.; Jian, W.; Jiang, J.; Wang, Z.; Hu, S.; Jiang, X. Therapeutic management of hemorrhage from visceral artery pseudoaneurysms after pancreatic surgery. J. Gastrointest. Surg. 2011, 15, 1417–1425. [Google Scholar] [CrossRef]
- Bellemann, N.; Sommer, C.M.; Mokry, T.; Kortes, N.; Gnutzmann, D.; Gockner, T.; Schmitz, A.; Weitz, J.; Kauczor, H.U.; Radeleff, B.; et al. Hepatic artery stent-grafts for the emergency treatment of acute bleeding. Eur. J. Radiol. 2014, 83, 1799–1803. [Google Scholar] [CrossRef]
- Yekebas, E.F.; Wolfram, L.; Cataldegirmen, G.; Habermann, C.R.; Bogoevski, D.; Koenig, A.M.; Kaifi, J.; Schurr, P.G.; Bubenheim, M.; Nolte-Ernsting, C.; et al. Postpancreatectomy hemorrhage: Diagnosis and treatment: An analysis in 1669 consecutive pancreatic resections. Ann. Surg. 2007, 246, 269–280. [Google Scholar] [CrossRef]
- You, Y.; Choi, S.H.; Choi, D.W.; Heo, J.S.; Han, I.W.; Han, S.; Shin, S.W.; Park, K.B.; Park, H.S.; Cho, S.K.; et al. Long-term clinical outcomes after endovascular management of ruptured pseudoaneurysm in patients undergoing pancreaticoduodenectomy. Ann. Surg. Treat. Res. 2019, 96, 237–249. [Google Scholar] [CrossRef]
- Wang, M.Q.; Liu, F.Y.; Duan, F.; Wang, Z.J.; Song, P.; Fan, Q.S. Stent-grafts placement for treatment of massive hemorrhage from ruptured hepatic artery after pancreaticoduodenectomy. World J. Gastroenterol. 2010, 16, 3716–3722. [Google Scholar] [CrossRef]
- Wallace, M.J.; Choi, E.; McRae, S.; Madoff, D.C.; Ahrar, K.; Pisters, P. Superior mesenteric artery pseudoaneurysm following pancreaticoduodenectomy: Management by endovascular stent-graft placement and transluminal thrombin injection. Cardiovasc. Interv. Radiol. 2007, 30, 518–522. [Google Scholar] [CrossRef]
- Herzog, T.; Suelberg, D.; Belyaev, O.; Uhl, W.; Seemann, M.; Seelig, M.H. Treatment of acute delayed visceral hemorrhage after pancreatic surgery from hepatic arteries with covered stents. J. Gastrointest. Surg. 2011, 15, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Kolokotronis, T.; Hosch, W.; Schmidt, J.; Radeleff, B.; Werner, J.; Weitz, J.; Büchler, M. Covered stents used for late, postpancreatectomy hemorrhage in the common hepatic artery. Am. Surg. 2011, 77, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Venturini, M.; Marra, P.; Colombo, M.; Panzeri, M.; Gusmini, S.; Sallemi, C.; Salvioni, M.; Lanza, C.; Agostini, G.; Balzano, G.; et al. Endovascular repair of 40 visceral artery aneurysms and pseudoaneurysms with the Viabahn stent-graft: Technical aspects, clinical outcome and mid-term patency. Cardiovasc. Interv. Radiol. 2018, 41, 385–397. [Google Scholar] [CrossRef] [PubMed]
- Stoupis, C.; Ludwig, K.; Inderbitzin, D.; Do, D.D.; Triller, J. Stent grafting of acute hepatic artery bleeding following pancreatic head resection. Eur. Radiol. 2007, 17, 401–408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanjay, P.; Kellner, M.; Tait, I.S. The role of interventional radiology in the management of surgical complications after pancreatoduodenectomy. HPB 2012, 14, 812–817. [Google Scholar] [CrossRef] [Green Version]
- Sato, A.; Yamada, T.; Takase, K.; Matsuhashi, T.; Higano, S.; Kaneda, T.; Egawa, S.; Takeda, K.; Ishibashi, T.; Takahashi, S. The fatal risk in hepatic artery embolization for hemostasis after pancreatic and hepatic surgery: Importance of collateral arterial pathways. J. Vasc. Interv. Radiol. 2011, 22, 287–293. [Google Scholar] [CrossRef]
- Lee, J.H.; Yoon, C.J.; Choi, W.S. Transhepatic stent placement for portal vein obstruction after hepatobiliary and pancreatic surgery: Long-term efficacy and risk factor for stent failure. Eur. Radiol. 2021, 31, 1300–1307. [Google Scholar] [CrossRef]
- Ruiz-Tovar, J.; Priego, P. Portal Vein Thrombosis After Splenic and Pancreatic Surgery. Adv. Exp. Med. Biol. 2017, 906, 241–251. [Google Scholar] [CrossRef]
- Fiorina, P.; Shapiro, A.M.; Ricordi, C.; Secchi, A. The clinical impact of islet transplantation. Am. J. Transplant 2008, 8, 1990–1997. [Google Scholar] [CrossRef]
- Ricordi, C.; Lacy, P.E.; Scharp, D.W. Automated islet isolation from human pancreas. Diabetes 1989, 38, 140–142. [Google Scholar] [CrossRef]
- Secchi, A.; Socci, C.; Maffi, P.; Taglietti, M.V.; Falqui, L.; Bertuzzi, F.; Nittis, P.D.; Piemonti, L.; Scopsi, L.; Carlo, V.D.; et al. Islet transplantation in IDDM patients. Diabetologia 1997, 40, 225–231. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, A.M.; Lakey, J.R.; Ryan, E.A.; Korbutt, G.S.; Toth, E.; Warnock, G.L.; Kneteman, N.M.; Rajotte, R.V. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N. Engl. J. Med. 2000, 343, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Fiorina, P.; Folli, F.; Maffi, P.; Placidi, C.; Venturini, M.; Finzi, G.; Bertuzzi, F.; Davalli, A.; D’Angelo, A.; Socci, C.; et al. Islet transplantation improves vascular diabetic complications in patients with diabetes who underwent kidney transplantation: A comparison between kidney-pancreas and kidney-alone transplantation. Transplantation 2003, 75, 1296–1301. [Google Scholar] [CrossRef]
- Fiorina, P.; Folli, F.; Bertuzzi, F.; Maffi, P.; Finzi, G.; Venturini, M.; Socci, C.; Davalli, A.; Orsenigo, E.; Monti, L.; et al. Long-term beneficial effect of islet transplantation on diabetic macro-/microangiopathy in type 1 diabetic kidney-transplanted patients. Diabetes Care 2003, 26, 1129–1136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venturini, M.; Fiorina, P.; Maffi, P.; Losio, C.; Vergani, A.; Secchi, A.; Maschio, A.D. Early increase of retinal arterial and venous blood flow velocities at color Doppler imaging in brittle type 1 diabetes after islet transplant alone. Transplantation 2006, 81, 1247–1274. [Google Scholar] [CrossRef] [PubMed]
- Carro, U.D.; Fiorina, P.; Amadio, S.; Franceschini, L.D.T.; Petrelli, A.; Menini, S.; Boneschi, F.M.; Ferrari, S.; Pugliese, G.; Maffi, P.; et al. Evaluation of polyneuropathy markers in type 1 diabetic kidney transplant patients and effects of islet transplantation: Neurophysiological and skin biopsy longitudinal analysis. Diabetes Care 2007, 30, 3063–3069. [Google Scholar] [CrossRef] [Green Version]
- Petrelli, A.; Maestroni, A.; Fadini, G.P.; Belloni, D.; Venturini, M.; Albiero, M.; Kleffel, S.; Mfarrej, B.G.; Maschio, A.D.; Maffi, P.; et al. Improved function of circulating angiogenic cells is evident in type 1 diabetic islet-transplanted patients. Am. J. Transplant 2010, 10, 2690–2700. [Google Scholar] [CrossRef]
- Sutherland, D.E.; Gruessner, A.C.; Carlson, A.M.; Blondet, J.J.; Balamurugan, A.N.; Reigstad, K.F.; Beilman, G.J.; Bellin, M.D.; Hering, B.J. Islet autotransplant outcomes after total pancreatectomy: A contrast to islet allograft outcomes. Transplantation 2008, 86, 1799–1802. [Google Scholar] [CrossRef]
- Helling, T.S. Surgical management of chronic pancreatitis and the role of islet cell autotransplantation. Curr. Surg. 2003, 60, 463–469. [Google Scholar] [CrossRef]
- Bellin, M.D. A Role for Total Pancreatectomy and islet autotransplant in the treatment of chronic pancreatitis. Am. J. Gastroenterol. 2018, 113, 324–326. [Google Scholar] [CrossRef]
- Balzano, G.; Piemonti, L. Autologous islet transplantation in patients requiring pancreatectomy for neoplasm. Curr. Diab. Rep. 2014, 14, 512. [Google Scholar] [CrossRef] [PubMed]
- Aleotti, F.; Nano, R.; Piemonti, L.; Falconi, M.; Balzano, G. Total pancreatectomy sequelae and quality of life: Results of islet autotransplantation as a possible mitigation strategy. Updates Surg. 2021, 73, 1237–1246. [Google Scholar] [CrossRef] [PubMed]
- King, J.; Kazanjian, K.; Matsumoto, J.; Reber, H.A.; Yeh, M.W.; Hines, O.J.; Eibl, G. Distal pancreatectomy: Incidence of postoperative diabetes. J. Gastrointest. Surg. 2008, 12, 1548–1553. [Google Scholar] [CrossRef] [PubMed]
- Parsaik, A.K.; Murad, M.H.; Sathananthan, A.; Moorthy, V.; Erwin, P.J.; Chari, S.; Carter, R.E.; Farnell, M.B.; Vege, S.S.; Sarr, M.G.; et al. Metabolic and target organ outcomes after total pancreatectomy: Mayo Clinic experience and meta-analysis of the literature. Clin. Endocrinol. 2010, 73, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Dixon, S.; Tapping, C.R.; Walker, J.N.; Bratby, M.; Anthony, S.; Boardman, P.; Phillips-Hughes, J.; Uberoi, R. The role of interventional radiology and imaging in pancreatic islet cell transplantation. Clin. Radiol. 2012, 67, 923–931. [Google Scholar] [CrossRef]
- Venturini, M.; Sallemi, C.; Marra, P.; Palmisano, A.; Agostini, G.; Lanza, C.; Balzano, G.; Falconi, M.; Secchi, A.; Fiorina, P.; et al. Allo- and auto-percutaneous intra-portal pancreatic islet transplantation (PIPIT) for diabetes cure and prevention: The role of imaging and interventional radiology. Gland. Surg. 2018, 7, 117–131. [Google Scholar] [CrossRef] [Green Version]
- Cahill, D.; Zamboni, F.; Collins, M.N. Radiological advances in pancreatic islet transplantation. Acad. Radiol. 2019, 26, 1536–1543. [Google Scholar] [CrossRef]
- Venturini, M.; Angeli, E.; Maffi, P.; Fiorina, P.; Bertuzzi, F.; Salvioni, M.; Cobelli, F.D.; Socci, C.; Aldrighetti, L.; Losio, C.; et al. Technique, complications, and therapeutic efficacy of percutaneous transplantation of human pancreatic islet cells in type 1 diabetes: The role of US. Radiology 2005, 234, 617–624. [Google Scholar] [CrossRef]







| Study | Patients (n) | Timing of Hemorrhage | Type of Procedure | Technical Success (%) | Complications (%) | Recurrent Bleeding (%) | Mortality (%) |
|---|---|---|---|---|---|---|---|
| Zhang et al., 2020 [78] | 15 | DPH | E | 89 | 15 | 23 | 30 |
| Hasegawa et al., 2017 [79] | 28 | EPH + DPH | E + S | 100 | 32 | - | 29 |
| Ansari et al., 2017 [80] | 10 | EPH + DPH | E + S | 80 | - | - | - |
| Gaudon et al., 2016 [81] | 42 | DPH | E + S | 69 | 12 | 28 | 13 |
| Hassold et al., 2016 [82] | 27 | DPH | E + S | 100 | 22 | 7 | 23 |
| Ching et al., 2016 [83] | 28 | DPH | E + S | 97 | 0 | 26 | 7 |
| Asari et al., 2016 [84] | 19 | EPH + DPH | E | 79 | - | - | 20 |
| Ding et al., 2011 [85] | 23 | DPH | E + S | 87 | 4 | 4 | 9 |
| Bellemann et al., 2014 [86] | 24 | DPH | S | 88 | 12 | 8 | 21 |
| Yekebas et al., 2007 [87] | 43 | EPH + DPH | E | 58 | - | - | 27 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mosconi, C.; Cocozza, M.A.; Piacentino, F.; Fontana, F.; Cappelli, A.; Modestino, F.; Coppola, A.; Palumbo, D.; Marra, P.; Maffi, P.; et al. Interventional Radiological Management and Prevention of Complications after Pancreatic Surgery: Drainage, Embolization and Islet Auto-Transplantation. J. Clin. Med. 2022, 11, 6005. https://doi.org/10.3390/jcm11206005
Mosconi C, Cocozza MA, Piacentino F, Fontana F, Cappelli A, Modestino F, Coppola A, Palumbo D, Marra P, Maffi P, et al. Interventional Radiological Management and Prevention of Complications after Pancreatic Surgery: Drainage, Embolization and Islet Auto-Transplantation. Journal of Clinical Medicine. 2022; 11(20):6005. https://doi.org/10.3390/jcm11206005
Chicago/Turabian StyleMosconi, Cristina, Maria Adriana Cocozza, Filippo Piacentino, Federico Fontana, Alberta Cappelli, Francesco Modestino, Andrea Coppola, Diego Palumbo, Paolo Marra, Paola Maffi, and et al. 2022. "Interventional Radiological Management and Prevention of Complications after Pancreatic Surgery: Drainage, Embolization and Islet Auto-Transplantation" Journal of Clinical Medicine 11, no. 20: 6005. https://doi.org/10.3390/jcm11206005
APA StyleMosconi, C., Cocozza, M. A., Piacentino, F., Fontana, F., Cappelli, A., Modestino, F., Coppola, A., Palumbo, D., Marra, P., Maffi, P., Piemonti, L., Secchi, A., Ricci, C., Casadei, R., Balzano, G., Falconi, M., Carcano, G., Basile, A., Ierardi, A. M., ... Venturini, M. (2022). Interventional Radiological Management and Prevention of Complications after Pancreatic Surgery: Drainage, Embolization and Islet Auto-Transplantation. Journal of Clinical Medicine, 11(20), 6005. https://doi.org/10.3390/jcm11206005









