Cardiovascular Complications of COVID-19 among Pregnant Women and Their Fetuses: A Systematic Review
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Study Selection
3.2. Demographic Characteristics and Cardiovascular Comorbidities
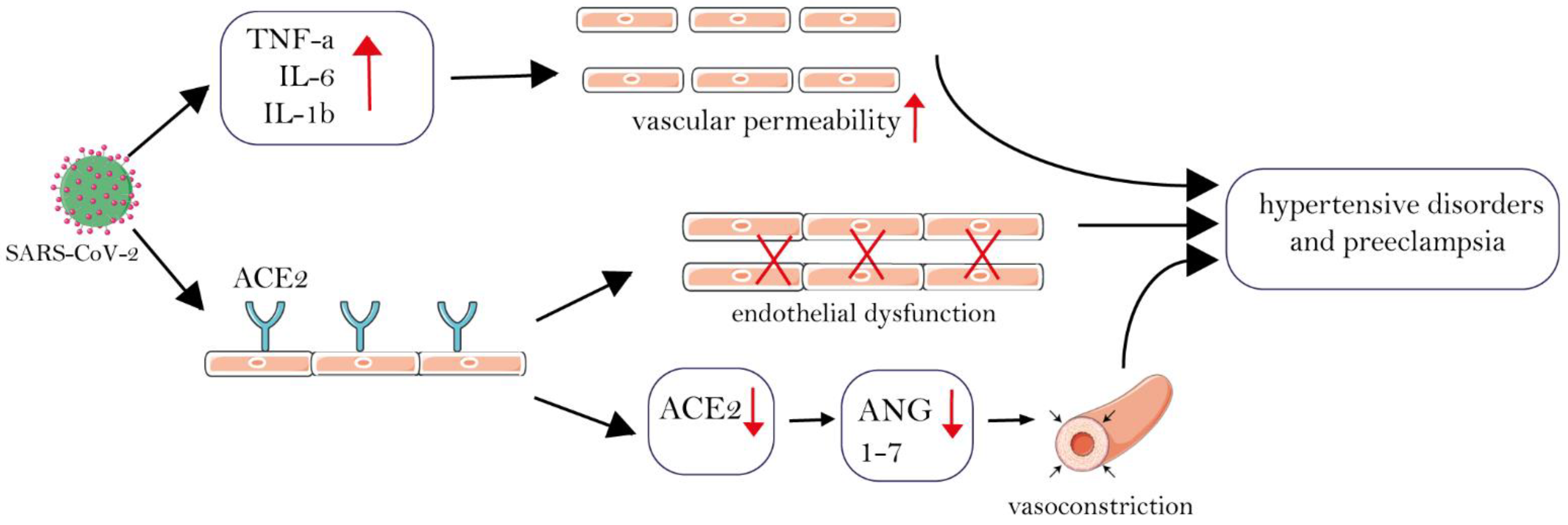
3.3. Pre-Eclampsia and Hypertensive Disorders
3.4. Cardiomyopathy, Myocardial Infarction, Heart Failure, and ECG Changes
3.5. Thrombotic Events in COVID-19 Patients during Pregnancy
3.6. Heart Rate Disorders
3.7. Doppler Findings and Fetal Complications
| First Author | Year | Study Design | Country | Number of Cases | Number of Controls | Pregnancy Phase | Mean Age of Cases | Mean Age of Controls | Cardiovascular Comorbidities Among Cases (Percentage) | Maternal Cardiovascular Complications Among Cases (Percentage) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hypertension | Others | Pre-eclampsia/Eclampsia/Gestational Hypertensive Disorders | Arrhythmia (Type) | Thrombotic Events | Doppler Findings | Others | |||||||||
| Kalahroudi et al. [28] | 2021 | Cohort | Iran | 56 | 94 | 31.9 ± 8.22 weeks | 31.6 ± 6.1 years | 6 (10.7%) | 10 (19.8%) | Pre-term labor (34.5%), caesarean delivery (67.3%) | |||||
| Antoun et al. [30] | 2020 | Cohort | UK | 23 | 6756 | Third trimester n = 19 Second trimester n = 4 | 29.0 | 2/23 (8.7%) | Pre-term labor 7/19 (36.4%), caesarean delivery 16/19 (68.4%) | ||||||
| Arslan et al. [38] | 2021 | Cohort | Turkey | 110 | 6508 | Third trimester n = 106 (96.4%) Second trimester n = 4 (3.6%) | 31.0 ± 6.0 years | 11 (10%) | Pre-term labor n = 37 (33.6%) | ||||||
| Melguizo et al. [20] | 2021 | Cohort | Spain | 1347 | 1607 | 33.0 | 33.0 | 19/1304 (1.5%) | Baseline heart disease 15/1316 (1.1%) | 69 (5.1%) (Severe pre-eclampsia n = 28/69 (40.6%)) | Venous thrombotic events (1.5%), DVT n = 10 (0.7%), pulmonary embolism n = 4 (0.3%) | Positive ultrasound prematurity screening n = 16 (1.4%) | Pre-term delivery (11.1%), premature rupture of membranes (15.5%), maternal mortality n = 2 (0.1%) | ||
| Daclin et al. [42] | 2021 | Case-control | France | 86 | 86 | 39.29 ± 2.65 weeks | 32.1 | 31.9 | 58/3235 (1.7%) | Pre-term delivery 6.2%, stillbirth n = 14/3235 (0.4%) | |||||
| Epelboin et al. [31] | 2021 | Cohort | France | 874 | 243,771 | Third trimester | 31.1 ± 5.9 | 30.5 ± 5.4 | 17/874 (1.9%) | 42/874 (4.8%) | Pre-term birth n = 146/874 (16.7%), caesarean delivery n = 288/847 (32.9%), mortality n = 2/874 (0.2%), gestational hypertension n = 20/874 (2.3%) | ||||
| Ferrera et al. [43] | 2022 | Cohort | USA | 1332 | 42,554 | 28.8 ± 5.5 | 30.8 ± 5.2 | 301/1332 (22.6%) | 20/1332 (1.5%) | Venous thromboembolism n = 4/1332 (0.3%) | Pre-term birth n = 143/1332 (10.7%), gestational hypertension n = 34/1332 (2.6%), caesarean delivery n = 357/1332 (26.8%), stillbirth n = 9/1332 (0.7%) | ||||
| Guida et al. [19] | 2022 | Case-control | Brazil | 21 (COVID-19 with pre-eclampsia) 10.3% | 182 (COVID-19 without pre-eclampsia) 89.7% | Third trimester 131 Second trimester 49 First trimester 23 | >35: n = 7/21 =<35: n = 14/21 | 7/21 (33.4%) | Eclampsia n = 1/21 (0.5%), imminent eclampsia n = 5/21 (2.5%) | Maternal death n = 2/21 (9.5%), pre-term birth n = 10/21 (47.6%/), caesarean delivery n = 19/21 (90.5%) | |||||
| Gurol et al. [32] | 2021 | Cohort | England | 3527 | 338,553 | =<19: n = 94/3527 20–24: n = 581/3527 25–29: n = 1040/3527 30–34: n = 1079/3527 35–39: n = 587/3527 +40: n = 146/3527 | 139/3527 (3.9%) | Pre-term birth n = 369/3047 (12.1%), fetal death n = 30/3527 (0.85%), emergency caesarean delivery n = 975/3527, (27.6%) | |||||||
| Hill et al. [21] | 2021 | Cohort | USA | 218 | 413 | Third trimester | 29.7 | 30.1 | 3/218 (1.4%) | 9/218 (4.2%) | Gestational hypertension n = 7/218 (3.3%), pre-term delivery n = 50/218 (22.93%) | ||||
| Jayaram et al. [27] | 2021 | Cohort | USA | 75 | 334 | Third trimester | 27.0 | 28.0 | 12/75 (16.0%) | 18/75 (24.0%) | Gestational HTN n = 8/75 (10.6%) | ||||
| Ahlberg et al. [77] | 2020 | Cohort | Sweden | 155 | 604 | 32.0 | 32.1 | 12/155 (7.7%) | Pre-term birth n = 14/155 (9%) | ||||||
| Mahajan [33] | 2020 | Retrospective study (historic cohort) | India | 879 | 63 | 38 and 34.5 weeks | 27.0 | Pre-eclampsia n = 50 (5.68%)/, eclampsia n = 4 (0.45%) | Dyspnea n = 38 (4.32%) | ||||||
| Melguizo [20] | 2020 | Cohort | Spain | 1347 | 1607 | 39 weeks and 2 days | 33.0 | 33.0 | 19 (1.5%) | Congenital heart disease n = 15 (1.1%) | Pre-eclampsia n = 69 (5.1%) | Thrombotic events: n = 7 (0.5%), deep vein thrombosis n = 10 (0.7%), pulmonary embolism n = 4 (0.3%) | |||
| Mendoza [39] | 2020 | Cohort | Spain | 8 | 34 | Third trimester, 31.6 weeks | 39.4 | 30.9 | Pre-eclampsia n = 5 (62.5%) | UtAPI n = 1 (12.5% of cases and 2.3% of total) | |||||
| Mercedes et al. [54] | 2020 | Cohort | Dominican Republic | 15 | 139 | 32.31 weeks | 29.8 | 29.8 | Palpitation n = 2 (13.3% of cases), atrial fibrillation and torsades de pointes and ventricular tachycardia n = 2 (13.3%), sinus tachycardia n = 4 (26.6%) | Elevated BNP and troponin in all cases group n = 15 (100%), BBB n = 5 (33.3%), ST depression and T-invert n = 6 (40%) | |||||
| Molteni [78] | 2020 | Replication cohort | USA, UK and Sweden | 16,718 | 1,328,248 | 14% in the first trimester, 43% in the second trimester, and 43% in the third trimester | 31.0 | 31.0 | Dyspnea n = 20/29 (73.6%), chest pain: 17 of 29 (62.3%) | ||||||
| Mullins et al. [45] | 2020–2021 | Prospective web-based registry—an observational cohort study | UK, Italy, China, Greece, Indonesia, India, Argentina, China, Czech Republic, Albania, Austria, Egypt and Chile | 5824 | 1923 | 34.0 | 34.0 | Pre-eclampsia n = 389/8189 (4.8%), eclampsia n = 41/8192 (0.5 %) | |||||||
| Chavan et al. [79] | April 2020–June 2021 | Prospective observational (cohort/cross sectional) | India | 17 | Not mentioned (but the whole numbers of data were 460) | Not mentioned | 26 | 26 | Pre-eclampsia n = 6/17 (35.2 %) | ||||||
| Osaikhuwuomwan et al. [40] | 2020 | Cross-sectional | Nigeria | 19 | 69 | 30.4 weeks | 31.4 | 31.4 | Pre-eclampsia/eclampsia n = 5/19 (26.3%) | ||||||
| Palomo et al. [80] | 2020 | Cohort | Spain | 17 | 10 | 39.1 | 35.6 | 36.9 | Hypertension n = 2 (11.7% of cases) | ||||||
| Papageorghiou et al. [34] | 2021 | Cohort | Argentina, Brazil, Egypt, France, Ghana, India, Indonesia, Italy, Japan, Mexico, Nigeria, North Macedonia, Pakistan, Russia, Spain, Switzerland, the United Kingdom, and the United States | 725 | 1459 | 29.95 | 30.31 | n = 26/725 (3.58%) | Pre-eclampsia n = 59/725 (8.13%) | ||||||
| Pierce-Williams et al. [46] | 2020 | Cohort | USA | 44 | 20 | 32 weeks | 33 | 33 | Chronic hypertension and cardiomyopathy n =11 (17%) | Pre-eclampsia n = 2 (3%) | Cardiac arrest n = 1 (3%) | ||||
| Pirjani et al. [35] | 2020 | Cohort | Iran | 66 | 133 | 32.64 weeks | 30.97 | 28.79 | - | - | Tachycardia n = 5 (7.57 %) | - | Dyspnea n = 27 (40.9%) | ||
| Serrano et al [36] | 2021 | Observational retrospective study (cross-sectional)/ historic cohort | Spain | 231 | 13,033 | First trimester (0–12 weeks) | 31.8 | 32.6 | Chronic hypertension n = 6/218 (2.8%), history of pre-eclampsia n = 9/218 (4.1 %) | High risk for pre-eclampsia n = 44/23 (19%) | |||||
| Trilla et al. [44] | 2020 | Prospective population-based study (cohort) | Spain | 124 | 639 | First, second and third trimester | 33.1 | 33.9 | Chronic hypertension n = 4/124 (3.2%) | pre-eclampsia n = 8/113 (7.3%) | |||||
| Yousefzadeh et al. [53] | 2020 | Cross-sectional | Iran | 89 | 111 | Mean = 29.59 weeks third trimester | 31 | 31 | - | - | Bradycardia n = 4 (4.5%), tachycardia n = 18 (20.5%) | ECG findings: atrioventricular (AV) block n = 3 (3.4%), first-degree AV block type (PR interval >200 ms) n = 3 (3.4%), mean QTC interval = 428.6 ± 37.4 ms, long QTC intervals (QTC ≥ 460 ms) n = 15 (17%), bundle branch block (QRS > 100 msec) (4.4%) of which three patients were RBBB and one was LBBB | |||
| Adhikari et al. [26] | 2020 | Cohort | USA | 245 | 3035 | First, second and third trimester | 27 | 27 | 26 (11%) | ||||||
| Anuk et al. [71] | 2021 | Case-control | Turkey | 30 | 40 | Median = 31.5 | Median = 30 | Median = 29 | Increased PI and RI of uterine artery, mean uterine artery PI = 1 (sd = 1), mean uterine artery RI = 0.6 (sd = 0.2), pre-term delivery n = 6 (20%) | ||||||
| Wu et al. [23] | 2020 | Cohort | China | 29 | - | 29 | 2 (6.90%) | ||||||||
| Pachtman et al. [17] | 2021 | Cohort | USA | 20 | - | 5 (25%) | Bradycardia (defined as <60 bpm), and maternal heart rate (HR) nadir n = 10/31 (32%) | Elevated cardiac troponins (I, T, or high sensitivity) n = 4/18 (22%), elevated BNP n = 3/10 (30%) | |||||||
| Berengueet et al. [18] | 2020 | Cohort | Spain | 4035 | 2052/4010 (51.2%) | Chronic heart disease n = 932/3994 (23.3%) | |||||||||
| Brandt et al. [81] | 2021 | Case-control | USA | 61 | 122 | 2 (3.3%) | |||||||||
| Jering et al. [37] | 2021 | Cohort | USA | 6380 | 400066 | 288 (4.5%) | Pre-eclampsia n = 564 (8.8%), eclampsia n = 8 (0.1%) | VTE n = 15 (0.2%), thrombotic event n = 22 (0.3%) | Myocardial infarction n = 8 (0.1%) | ||||||
| Soto-Torres et al. [10] | 2021 | Case-control | USA | 106 | 103 | Pre-eclampsia n = 21 (19.8%), other hypertensive disorders n = 17 (16%) | |||||||||
| Rosenbloom et al. [41] | 2021 | Cohort | Israel | 83 | 166 | 39 w | 26 | 28 | 10 (12.1%) | Gestational hypertension n = 10 (12.1%), pre-eclampsia n = 14(16.9%), other hypertensive disorders n = 24 (28.9) | |||||
| First Author | Year | Study Design | Country | Number of Cases | Number of Controls | Pregnancy Phase | Mean Age of Cases | Mean Age of Controls | Cardiovascular Comorbidities among Cases (%) | Fetal Cardiovascular Complications among Cases (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hypertension | Others | Arrhythmia (Type) | Thrombotic Events | Cardiomyopathy/Heart Failure | Doppler Findings | |||||||||
| Ayhan et al. [82] | 2022 | Case-control | Turkey | 45 | 45 | 32 ± 4 weeks | 33 ± 1 weeks | Aortic peak velocity = 79.4 cm/s, pulmonary peak velocity = 67.4 cm/s, left myocardial performance index = 0.57 ± 0.14, tricuspid annular plane systolic excursion (TAPSE) = 6.87 mm, mitral annular plane systolic excursion (MAPASE) = 6.69 mm | ||||||
| Mercedes et al. [54] | 2020 | Cohort | Dominican Republic | 15 | 139 | 32.31 week | 29.87 | 29.87 | - | Fetal bradycardia n =3 (20% of patients) | ||||
| Sinaci et al. [65] | 2020 | Cohort | Turkey | 224 | Over 150,000 | 37 weeks | 28 | Not mentioned | - | Tachycardia n = 12 (5.4%), bradycardia n = 3 (1.3%) | ||||
| Adhikari et al. [26] | 2020 | Cohort | USA | 245 | 3035 | 27 | 27 | 26 (11%) | Abnormal fetal heart rate n = 7 (3%) | |||||
| Anuk et al. [71] | 2021 | Case-control | Turkey | 30 | 40 | Median = 31.5 | 30 | 29 | Increased PI and RI of umbilical arteries, mean umbilical artery PI = 1 (IQR = 0.2), mean umbilical artery RI = 0.6 (IQR = 0.1), mean uterine artery PI = 1 (IQR = 1), mean uterine artery PI = 0.6 (IQR = 0.2) | |||||
| Soto-Torres et al. [10] | 2021 | Case-control | USA | 106 | 103 | Fetal tachycardia n = 1 (1%), premature atrial contractions n = 1 (1%) | Abnormal Doppler findings n = 8 (7%), mean PI of umbilical artery = 0.67 (No significant difference between patients and controls) | |||||||
| Sule et al. [70] | 2021 | Cohort | USA | 55 | 93 | Higher AT of pulmonary artery in patients, no significant difference in ET and PATET of pulmonary artery between patients and controls | ||||||||
| First Author | Year | Study Design | Country | Number of Cases | Pregnancy Phase | Mean Age | Cardiovascular Comorbidities | Maternal Cardiovascular Complications | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hypertension | Others | Pre-eclampsia/Eclampsia | Arrhythmia (Type) | Thrombotic Events | Cardiomyopathy/Heart Failure | Doppler Findings | Others | |||||||
| Ahmed et al. [49] | 2020 | Case report | UK | 1 | 37 weeks | 26 | 173/111 mmHg | Pre-eclampsia | HELLP syndrome | |||||
| Askary et al. [48] | 2020 | Case series | Iran | 16 | Third trimester 10, second trimester 5, first trimester 1 | 30.06 | 7/16 | Pulmonary thromboembolism n = 1 | Massive myocardial infarction n = 1 | Pre-term labor n = 6/16, caesarean delivery n = 9/12, premature labor pain (PLP) n = 2, placenta accreta n = 2 | ||||
| Azarkish et al. [50] | 2021 | Case report | Iran | 1 | 38 weeks | 19 | 140/90 mmHg | Sinus tachycardia | Elevated PTT | Cardiorespiratory arrest and death | ||||
| Breslin et al. [66] | 2020 | Case series | USA | 7 | 33.2 weeks | 33.85 | Bronchospasm, tachycardia | Hypertension | ||||||
| Seresht et al. [55] | 2022 | Case series | Iran | 4 | 25 weeks | 29.25 | Large atrial septal defect | Tachycardia 4/4 | (1) Minimal pericardial effusion, EF 25%, heart failure (2) Severe acute cardiac failure, acute left ventricular failure, EF 20% (3) EF 30%, pulmonary edema (4) Heart failure, EF 35% | Severe mitral valve regurgitation | Intrauterine fetal demise with oligohydramnios, expired n = 2/4 | |||
| Donovan et al. [67] | 2022 | Case report | USA | 1 | 35 weeks and 5 days | 36 | Tachycardia 110 beats/min | |||||||
| Franca et al. [59] | 2022 | Case report | Brazil | 1 | 28 weeks | 26 | Mitral valve replacement in 2011 due to mitral valve stenosis | Tachycardia >145 beats/minute, ventricular tachyarrhythmia, mitral murmur | High blood pressure (147/95 mmHg), death | |||||
| Goudarzi et al. [64] | 2022 | Case report | Iran | 1 | Third trimester | 22 | Massive pulmonary embolism | Right and left-sided heart failure | First echocardiography showed a very dilated right atria and ventricle fetal death. Second echocardiography showed right ventricle enlargement, severe dysfunction, McConnell’s sign, moderate tricuspid regurgitation, dilated pulmonary artery, mild pulmonary insufficiency, dilated inferior vena cava, respiratory cardiovascular arrest and death | |||||
| Gulersen et al. [60] | 2021 | Case report | USA | 1 | 28 weeks and 4 days | 31 | Yes | Tachycardia (heart rate 122 beats per minute), sinus tachycardia | Multiple risk factors for venous thromboembolism | Pericardial effusion biventricular dysfunction | Caesarean birth | |||
| Hansen et al. [51] | 2020 | Case report | USA | 1 | 34 weeks | 31 | 162/86 mm Hg | Presumed pre-eclampsia | Caesarean birth | |||||
| Khodamoradi et al. [62] | 2020 | Case report | Iran | 1 | 37 weeks and 2 days | 36 | Pulmonary embolism, hypercoagulable state | Had elective scheduled caesarean section | ||||||
| Leal et al. [25] | 2020 | Case series | Brazil | 5469 | First trimester: n = 378 6.9 %, second trimester: n = 985 18%, third trimester: n = 2475 45.25%, postpartum and postabortion: n = 1393 25.4% | 30 | n = 562 (10.2%) | Chest pain: n = 107 (2%) | ||||||
| Naeh et al. [52] | 2021 | Case report | Canada | 1 | 28 week (third trimester) | 39 | 152/132 mm Hg | Sinus tachycardia PR = 141 | Dyspnea | |||||
| Nejadrahim et al. [57] | 2020 | Case report | Iran | 1 | Postpartum | 38 | Severe pre-eclampsia | Tachycardia PR = 115 | Postpartum cardiomyopathy/heart failure with LVEF of 30%, global hypokinesis, LV enlargement (LV end diastolic size 5.8 cm) | Dyspnea/ pulmonary edema | ||||
| Pelayo et al. | 2020 | Case report | USA | 1 | 36 week and 2 days | 35 | Tachycardia | Cardiomyopathy as evidenced with 45% ejection fraction on echocardiography | Pulmonary embolism | |||||
| Radoi et al. [83] | 2021 | Case report | Romania | 1 | 26 weeks | 19 | Pre-eclampsia BP = 178,110 | Tachycardia | Heart failure with ejection fraction less than 30% | Dyspnea, cyanosis, pulmonary edema, chest pain, pulmonary hypertension, VSD and Mirror and Eisenmenger Syndrome, increased jugular venous pressure | ||||
| Soofi et al. [58] | 2020 | Case report | Saudi Arabia | 1 | 34 weeks | 25 | Sinus tachycardia and occasional PVCs | DVT in the right superficial femoral Vein | Acute heart failure on echocardiography exhibited features of severe left ventricle systolic dysfunction. Cardiac MRI displayed severe global LV and RV systolic dysfunction, | Pleuritic chest pain with dyspnea | ||||
| Stout et al. [61] | 2020 | Case report | UK | 1 | 36 weeks and 4 days | 28 | Tachycardia PR = 120, ventricular fibrillation, ventricular escape rhythm | - | - | - | Cardiac arrest | |||
| Vaezi et al. [24] | 2020 | Case series | Iran | 24 | Third trimester (15 cases, 62.5%), 6 cases were in their second trimester (25%), and only 3 cases (12.5%) were under 14 weeks | 26.5 | n = 1 (4.16%) | HELLP n = 1 (4.16%) | Severe pre-eclampsia n = 3 (12.5%) | Tachycardia n = 3 (12.5%) | Dyspnea n = 10 (41.6 %) | |||
| Zarrintan et al. [63] | 2020 | Case report | Iran | 1 | 34 weeks | 39 | Sinus tachycardia | Pulmonary thromboembolism | Echocardiography showed an ejection fraction of 45–50%. Severe right ventricle enlargement was also evident, with moderate to severe dysfunction of the right ventricle. | Dyspnea, chest discomfort. ECG showed an S wave in the lead I, q wave in lead II and sinus tachycardia, suggestive of right ventricle straining. | ||||
| Agarwal et al. [84] | 2021 | Case report | India | 1 | Third trimester | 28 | Portal hypertension due to portal vein thrombosis (PVT) | |||||||
| Bhattacharyya et al. [56] | 2020 | Case report | India | 1 | 38 w | Takotsubo cardiomyopathy | ||||||||
| De Vita et al. [16] | 2020 | Case report | Italy | 1 | Third trimester | 35 | Thrombosis both in the apical left ventricle and in a branch of the pulmonary artery | Peripartum cardiomyopathy, congestive heart failure | ||||||
| Juusela et al. [47] | 2020 | Case series | USA | 2 | 39 w 2 d–33 w 6 d | Pre-eclampsia | Cardiomyopathy (cardiac dysfunction with moderately reduced left ventricular ejection fractions of 40% and 45% and hypokinesis) | |||||||
| First Author | Year | Study Design | Country | Number of Cases | Pregnancy Phase | Mean Age | Fetal Cardiovascular Complications | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Arrhythmia (Type) | Thrombotic Events | Cardiomyopathy/Heart Failure | Others | |||||||
| Cetera et al. [74] | 2021 | Case series | Italy | 3 | Fetal bradycardia 1 | Type 2 fetal cardiotocography n = 1 fetal demise n = 2 | ||||
| Perez et al. [72] | 2020 | Case series | Spain | 12 | 37.80 weeks | Gross fetal tachycardia (>210 bpm) n = 1/12, absence of accelerations n = 12/12, prolonged decelerations n = 10/12, zigzag pattern n = 4/12 (33%) | Absence of cycling n = 7/12 (58.3%) | |||
| Gubbari et al. [76] | 2022 | Case report | India | 1 | 34 weeks | 17 days | Persistent tachycardia | Right ventricular dilation | Echocardiography revealed pulmonary hypertension biventricular hypertrophy, severe mitral and tricuspid regurgitation with EF = 35% on day 2 | |
| Kato et al. [73] | 2022 | Case report | Japan | 1 | 21 weeks | Tachycardia (165 bpm) | Intrauterine fetal death The RT-PCR test result from a dead neonatal nasopharyngeal swab was positive | |||
| Mevada et al. [85] | 2020 | Case report | India | 1 | Third trimester (GA: 36.5 by date and 37 by scan) | 30 | Tachycardia (PR = 110) | PPCM or viral cardiomyopathy | Echocardiography: global left ventricular hypokinesia, EF 25–30% | |
| Radoi et al. [83] | 2021 | Case report | Romania | 1 | 26 weeks | 19 | Hydrops fetalis, Mirror syndrome | |||
| Vaezi [24] | 2020 | Case series | Iran | 24 | Third trimester (15 cases, 62.5%), 6 cases were in their second trimester (25%), and only 3 cases (12.5%) were under 14 weeks | 26.5 | Fetal bradycardia n = 1 (4.16%) | |||
| Mongula et al. [86] | 2020 | Case report | Netherlands | 1 | 31w4d | Fetal tachycardia | ||||
| Wang et al. [87] | 2022 | Case report | USA | 1 | 31w5d | Supraventricular tachycardia | ||||
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jiang, F.; Deng, L.; Zhang, L.; Cai, Y.; Cheung, C.W.; Xia, Z. Review of the Clinical Characteristics of Coronavirus Disease 2019 (COVID-19). J. Gen. Intern. Med. 2020, 35, 1545–1549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.Q.; Huang, T.; Wang, Y.Q.; Wang, Z.P.; Liang, Y.; Huang, T.B.; Zhang, H.Y.; Sun, W.; Wang, Y. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020, 92, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.Y.; Ma, Y.T.; Zhang, J.Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef] [Green Version]
- Sutton, D.; Fuchs, K.; D’Alton, M.; Goffman, D. Universal Screening for SARS-CoV-2 in Women Admitted for Delivery. N. Engl. J. Med. 2020, 382, 2163–2164. [Google Scholar] [CrossRef]
- Crovetto, F.; Crispi, F.; Llurba, E.; Pascal, R.; Larroya, M.; Trilla, C.; Camacho, M.; Medina, C.; Dobaño, C.; Gomez-Roig, M.D.; et al. Impact of SARS-CoV-2 Infection on Pregnancy Outcomes: A Population-Based Study. Clin. Infect. Dis. 2021, 73, 1768–1775. [Google Scholar] [CrossRef] [PubMed]
- Cosma, S.; Borella, F.; Carosso, A.; Sciarrone, A.; Cusato, J.; Corcione, S.; Mengozzi, G.; Preti, M.; Katsaros, D.; Di Perri, G.; et al. The “scar” of a pandemic: Cumulative incidence of COVID-19 during the first trimester of pregnancy. J. Med. Virol. 2021, 93, 537–540. [Google Scholar] [CrossRef] [PubMed]
- Pineles, B.L.; Alamo, I.C.; Farooq, N.; Green, J.; Blackwell, S.C.; Sibai, B.M.; Parchem, J.G. Racial-ethnic disparities and pregnancy outcomes in SARS-CoV-2 infection in a universally-tested cohort in Houston, Texas. Eur. J. Obs. Gynecol. Reprod. Biol. 2020, 254, 329–330. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Portilla, R.J.; Sotiriadis, A.; Chatzakis, C.; Torres-Torres, J.; Espino, Y.S.S.; Sandoval-Mandujano, K.; Castro-Bernabe, D.A.; Medina-Jimenez, V.; Monarrez-Martin, J.C.; Figueras, F.; et al. Pregnant women with SARS-CoV-2 infection are at higher risk of death and pneumonia: Propensity score matched analysis of a nationwide prospective cohort (COV19Mx). Ultrasound Obs. Gynecol. 2021, 57, 224–231. [Google Scholar] [CrossRef]
- Chen, Y.; Bai, J. Maternal and infant outcomes of full-term pregnancy combined with COVID-2019 in Wuhan, China: Retrospective case series. Arch. Gynecol. Obs. 2020, 302, 545–551. [Google Scholar] [CrossRef]
- Soto-Torres, E.; Hernandez-Andrade, E.; Huntley, E.; Mendez-Figueroa, H.; Blackwell, S.C. Ultrasound and Doppler findings in pregnant women with SARS-CoV-2 infection. Ultrasound Obstet. Gynecol. 2021, 58, 111–120. [Google Scholar] [CrossRef]
- Vigil-De Gracia, P.; Caballero, L.; Sánchez, J.; Espinosa, J.; Campana, S.; Quintero, A.; Luo, C.; Ng, J. Pregnancies recovered from SARS-CoV-2 infection in second or third trimester: Obstetric evolution. Ultrasound Obstet. Gynecol. 2020, 56, 777. [Google Scholar] [CrossRef] [PubMed]
- Phoswa, W.N.; Khaliq, O.P. Is pregnancy a risk factor of COVID-19? Eur. J. Obs. Gynecol. Reprod. Biol. 2020, 252, 605–609. [Google Scholar] [CrossRef]
- Zambrano, L.D.; Ellington, S.; Strid, P.; Galang, R.R.; Oduyebo, T.; Tong, V.T.; Woodworth, K.R.; Nahabedian, J.F., 3rd; Azziz-Baumgartner, E.; Gilboa, S.M.; et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status—United States, January 22–October 3, 2020. MMWR Morb. Mortal Wkly. Rep. 2020, 69, 1641–1647. [Google Scholar] [CrossRef] [PubMed]
- Turan, O.; Hakim, A.; Dashraath, P.; Jeslyn, W.J.L.; Wright, A.; Abdul-Kadir, R. Clinical characteristics, prognostic factors, and maternal and neonatal outcomes of SARS-CoV-2 infection among hospitalized pregnant women: A systematic review. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2020, 151, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Wang, L.; Fang, C.; Peng, S.; Zhang, L.; Chang, G.; Xia, S.; Zhou, W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 2020, 9, 51–60. [Google Scholar] [CrossRef]
- De Vita, S.; Ippolito, S.; Caracciolo, M.M.; Barosi, A. Peripartum cardiomyopathy in a COVID-19-infected woman: Differential diagnosis with acute myocarditis-A case report from a Hub Institution during the COVID-19 outbreak. Echocardiography 2020, 37, 1673–1677. [Google Scholar] [CrossRef]
- Pachtman Shetty, S.L.; Meirowitz, N.; Blitz, M.J.; Gadomski, T.; Weinberg, C.R. Myocardial injury associated with coronavirus disease 2019 in pregnancy. Am. J. Obstet. Gynecol. 2021, 224, 229–232. [Google Scholar] [CrossRef]
- Berenguer, J.; Ryan, P.; Rodríguez-Baño, J.; Jarrín, I.; Carratalà, J.; Pachón, J.; Yllescas, M.; Arriba, J.R.; Aznar Muñoz, E.; Gil Divasson, P.; et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain. Clin. Microbiol. Infect. 2020, 26, 1525–1536. [Google Scholar] [CrossRef]
- Guida, J.P.; Cecatti, J.G.; Souza, R.T.; Pacagnella, R.C.; Ribeiro-do-Valle, C.C.; Luz, A.G.; Lajos, G.J.; Surita, F.G.; Nobrega, G.M.; Griggio, T.B. Preeclampsia among women with COVID-19 during pregnancy and its impact on maternal and perinatal outcomes: Results from a national multicenter study on COVID in Brazil, the REBRACO initiative. Pregnancy Hypertens. 2022, 28, 168–173. [Google Scholar] [CrossRef]
- Melguizo, S.C.; Conty, M.L.D.; Payan, P.C.; Abascal-Saiz, A.; Recarte, P.P.; Rodriguez, L.G.; Marin, C.C.; Varea, A.M.; Cuesta, A.B.O.; Rodriguez, P.P.; et al. Pregnancy Outcomes and SARS-CoV-2 Infection: The Spanish Obstetric Emergency Group Study. Viruses 2021, 13, 853. [Google Scholar] [CrossRef]
- Hill, J.; Patrick, H.S.; Ananth, C.V.; O’Brien, D.; Spernal, S.; Horgan, R.; Brandt, J.S.; Schwebel, M.; Miller, R.C.; Straker, M.J. Obstetrical outcomes and follow-up for patients with asymptomatic COVID-19 at delivery: A multicenter prospective cohort study. Am. J. Obstet. Gynecol. MFM 2021, 3, 100454. [Google Scholar] [CrossRef] [PubMed]
- Moodley, J.; Soma-Pillay, P.; Buchmann, E.; Pattinson, R.C. Hypertensive disorders in pregnancy: 2019 National guideline. S. Afr. Med. J. 2019, 109. [Google Scholar]
- Wu, Y.-T.; Liu, J.; Xu, J.-J.; Chen, Y.-F.; Yang, W.; Chen, Y.; Li, C.; Wang, Y.; Liu, H.; Zhang, C. Neonatal outcome in 29 pregnant women with COVID-19: A retrospective study in Wuhan, China. PLoS Med. 2020, 17, e1003195. [Google Scholar] [CrossRef] [PubMed]
- Vaezi, M.; Mirghafourvand, M.; Hemmatzadeh, S. Characteristics, clinical and laboratory data and outcomes of pregnant women with confirmed SARS-CoV-2 infection admitted to Al-Zahra tertiary referral maternity center in Iran: A case series of 24 patients. BMC Pregnancy Childbirth 2021, 21, 378. [Google Scholar] [CrossRef] [PubMed]
- Leal, L.F.; Merckx, J.; Fell, D.B.; Kuchenbecker, R.; Miranda, A.E.; de Oliveira, W.K.; Platt, R.W.; Antunes, L.; Silveira, M.F.; Barbieri, N.B. Characteristics and outcomes of pregnant women with SARS-CoV-2 infection and other severe acute respiratory infections (SARI) in Brazil from January to November 2020. Braz. J. Infect. Dis. 2021, 25, 101620. [Google Scholar] [CrossRef]
- Adhikari, E.H.; Moreno, W.; Zofkie, A.C.; MacDonald, L.; McIntire, D.D.; Collins, R.R.J.; Spong, C.Y. Pregnancy Outcomes Among Women With and Without Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Netw. Open 2020, 3, e2029256. [Google Scholar] [CrossRef]
- Jayaram, A.; Buhimschi, I.A.; Aldasoqi, H.; Hartwig, J.; Owens, T.; Elam, G.L.; Buhimschi, C.S. Who said differentiating preeclampsia from COVID-19 infection was easy? Pregnancy Hypertens. 2021, 26, 8–10. [Google Scholar] [CrossRef]
- Abedzadeh-Kalahroudi, M.; Sehat, M.; Vahedpour, Z.; Talebian, P. Maternal and neonatal outcomes of pregnant patients with COVID-19: A prospective cohort study. Int. J. Gynecol. Obstet. 2021, 153, 449–456. [Google Scholar] [CrossRef]
- Ahlberg, M.; Neovius, M.; Saltvedt, S.; Söderling, J.; Pettersson, K.; Brandkvist, C.; Stephansson, O. Association of SARS-CoV-2 Test Status and Pregnancy Outcomes. JAMA 2020, 324, 1782–1785. [Google Scholar] [CrossRef]
- Antoun, L.; El Taweel, N.; Ahmed, I.; Patni, S.; Honest, H. Maternal COVID-19 infection, clinical characteristics, pregnancy, and neonatal outcome: A prospective cohort study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 559–562. [Google Scholar] [CrossRef]
- Epelboin, S.; Labrosse, J.; De Mouzon, J.; Fauque, P.; Gervoise-Boyer, M.-J.; Levy, R.; Sermondade, N.; Hesters, L.; Bergère, M.; Devienne, C. Obstetrical outcomes and maternal morbidities associated with COVID-19 in pregnant women in France: A national retrospective cohort study. PLoS Med. 2021, 18, e1003857. [Google Scholar] [CrossRef] [PubMed]
- Gurol-Urganci, I.; Jardine, J.E.; Carroll, F.; Draycott, T.; Dunn, G.; Fremeaux, A.; Harris, T.; Hawdon, J.; Morris, E.; Muller, P.; et al. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection at the time of birth in England: National cohort study. Am. J. Obs. Gynecol. 2021, 225, 522.e1–522.e11. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, N.N.; Ansari, M.; Gaikwad, C.; Jadhav, P.; Tirkey, D.; Pophalkar, M.P.; Bhurke, A.V.; Modi, D.N.; Mahale, S.D.; Gajbhiye, R.K. Impact of SARS-CoV-2 on multiple gestation pregnancy. Int. J. Gynaecol. Obs. 2021, 152, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Papageorghiou, A.T.; Deruelle, P.; Gunier, R.B.; Rauch, S.; García-May, P.K.; Mhatre, M.; Usman, M.A.; Abd-Elsalam, S.; Etuk, S.; Simmons, L.E.; et al. Preeclampsia and COVID-19: Results from the INTERCOVID prospective longitudinal study. Am. J. Obs. Gynecol. 2021, 225, 289.e1–289.e17. [Google Scholar] [CrossRef]
- Pirjani, R.; Hosseini, R.; Soori, T.; Rabiei, M.; Hosseini, L.; Abiri, A.; Moini, A.; Shizarpour, A.; Razani, G.; Sepidarkish, M. Maternal and neonatal outcomes in COVID-19 infected pregnancies: A prospective cohort study. J. Travel. Med. 2020, 27. [Google Scholar] [CrossRef]
- Serrano, B.; Mendoza, M.; Garcia-Aguilar, P.; Bonacina, E.; Garcia-Ruiz, I.; Garcia-Manau, P.; Gil, J.; Armengol-Alsina, M.; Fernandez-Hidalgo, N.; Sulleiro, E.; et al. Shared risk factors for COVID-19 and preeclampsia in the first trimester: An observational study. Acta Obs. Gynecol. Scand. 2022, 101, 803–808. [Google Scholar] [CrossRef]
- Jering, K.S.; Claggett, B.L.; Cunningham, J.W.; Rosenthal, N.; Vardeny, O.; Greene, M.F.; Solomon, S.D. Clinical Characteristics and Outcomes of Hospitalized Women Giving Birth With and Without COVID-19. JAMA Intern. Med. 2021, 181, 714–717. [Google Scholar] [CrossRef]
- Arslan, B.; Bicer, I.G.; Sahin, T.; Vay, M.; Dilek, O.; Destegul, E. Clinical characteristics and hematological parameters associated with disease severity in COVID-19 positive pregnant women undergoing cesarean section: A single-center experience. J. Obs. Gynaecol. Res. 2022, 48, 402–410. [Google Scholar] [CrossRef]
- Mendoza, M.; Garcia-Ruiz, I.; Maiz, N.; Rodo, C.; Garcia-Manau, P.; Serrano, B.; Lopez-Martinez, R.M.; Balcells, J.; Fernandez-Hidalgo, N.; Carreras, E.; et al. Pre-eclampsia-like syndrome induced by severe COVID-19: A prospective observational study. Bjog 2020, 127, 1374–1380. [Google Scholar] [CrossRef]
- Osaikhuwuomwan, J.; Ezeanochie, M.; Uwagboe, C.; Ndukwu, K.; Yusuf, S.; Ande, A. Clinical characteristics and outcomes for pregnant women diagnosed with COVID-19 disease at the University of Benin Teaching Hospital, Benin City, Nigeria. Pan. Afr. Med. J. 2021, 39, 134. [Google Scholar] [CrossRef]
- Rosenbloom, J.I.; Raghuraman, N.; Carter, E.B.; Kelly, J.C. Coronavirus disease 2019 infection and hypertensive disorders of pregnancy. Am. J. Obs. Gynecol. 2021, 224, 623–624. [Google Scholar] [CrossRef] [PubMed]
- Daclin, C.; Carbonnel, M.; Rossignol, M.; Abbou, H.; Trabelsi, H.; Cimmino, A.; Delmas, J.; Rifai, A.S.; Coiquaud, L.A.; Tiberon, A.; et al. Impact of COVID-19 infection in pregnancy and neonates: A case control study. J. Gynecol. Obs. Hum. Reprod. 2022, 51, 102366. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, A.; Hedderson, M.M.; Zhu, Y.; Avalos, L.A.; Kuzniewicz, M.W.; Myers, L.C.; Ngo, A.L.; Gunderson, E.P.; Ritchie, J.L.; Quesenberry, C.P.; et al. Perinatal Complications in Individuals in California With or Without SARS-CoV-2 Infection During Pregnancy. JAMA Intern. Med. 2022, 182, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Trilla, C.; Mora, J.; Crovetto, F.; Crispi, F.; Gratacos, E.; Llurba, E. First-Trimester SARS-CoV-2 Infection: Clinical Presentation, Inflammatory Markers, and Obstetric Outcomes. Fetal Diagn. 2022, 49, 67–76. [Google Scholar] [CrossRef]
- Mullins, E.; Perry, A.; Banerjee, J.; Townson, J.; Grozeva, D.; Milton, R.; Kirby, N.; Playle, R.; Bourne, T.; Lees, C. Pregnancy and neonatal outcomes of COVID-19: The PAN-COVID study. Eur. J. Obs. Gynecol. Reprod. Biol. 2022, 276, 161–167. [Google Scholar] [CrossRef]
- Pierce-Williams, R.A.M.; Burd, J.; Felder, L.; Khoury, R.; Bernstein, P.S.; Avila, K.; Penfield, C.A.; Roman, A.S.; DeBolt, C.A.; Stone, J.L.; et al. Clinical course of severe and critical coronavirus disease 2019 in hospitalized pregnancies: A United States cohort study. Am. J. Obs. Gynecol. MFM 2020, 2, 100134. [Google Scholar] [CrossRef]
- Juusela, A.; Nazir, M.; Gimovsky, M. Two cases of coronavirus 2019-related cardiomyopathy in pregnancy. Am. J. Obs. Gynecol. MFM 2020, 2, 100113. [Google Scholar] [CrossRef]
- Askary, E.; Poordast, T.; Shiravani, Z.; Ali, M.A.; Hashemi, A.; Naseri, R.; Moradialamdarloo, S.; Karimi, Z.; Izanloo, E.; Najib, F.S. Coronavirus disease 2019 (COVID-19) manifestations during pregnancy in all three trimesters: A case series. Int. J. Reprod. Biomed. 2021, 19, 191–204. [Google Scholar] [CrossRef]
- Ahmed, I.; Eltaweel, N.; Antoun, L.; Rehal, A. Severe pre-eclampsia complicated by acute fatty liver disease of pregnancy, HELLP syndrome and acute kidney injury following SARS-CoV-2 infection. BMJ Case Rep. 2020, 13, e237521. [Google Scholar] [CrossRef]
- Azarkish, F.; Sheikhi, F.; Mirkazehi, Z.; Kalkali, S.; Moghadam, P.B.; Zahirniya, M. Preeclampsia and the crucial postpartum period for COVID-19 infected mothers: A case report. Pregnancy Hypertens. 2021, 23, 136–139. [Google Scholar] [CrossRef]
- Hansen, J.N.; Hine, J.; Strout, T.D. COVID-19 and preeclampsia with severe features at 34-weeks gestation. Am. J. Emerg. Med. 2021, 39, 252.e3–252.e5. [Google Scholar] [CrossRef] [PubMed]
- Naeh, A.; Berezowsky, A.; Yudin, M.H.; Dhalla, I.A.; Berger, H. Preeclampsia-Like Syndrome in a Pregnant Patient With Coronavirus Disease 2019 (COVID-19). J. Obs. Gynaecol. Can. 2022, 44, 193–195. [Google Scholar] [CrossRef] [PubMed]
- Yousefzadeh, M.; Asgarian, A.; Ahangari, R.; Vahedian, M.; Mirzaie, M. Electrocardiographic changes in pregnant women with COVID-19. J. Pract. Cardiovasc. Sci. 2022, 8, 17–21. [Google Scholar] [CrossRef]
- Mercedes, B.R.; Serwat, A.; Naffaa, L.; Ramirez, N.; Khalid, F.; Steward, S.B.; Feliz, O.G.C.; Kassab, M.B.; Karout, L. New-onset myocardial injury in pregnant patients with coronavirus disease 2019: A case series of 15 patients. Am. J. Obstet. Gynecol. 2021, 224, 387.e1–387.e9. [Google Scholar] [CrossRef]
- Mousavi Seresht, L.; Dehghan, M.; Fakhrolmobasheri, M.; Kawakita, T.; Mazaheri Tehrani, S.; Rastegar, A. Peripartum cardiomyopathy and Coronavirus Disease 2019 (COVID-19) associated cardiomyopathy: Case series and review of literature. Authorea 2022. [Google Scholar] [CrossRef]
- Bhattacharyya, P.J.; Attri, P.K.; Farooqui, W. Takotsubo cardiomyopathy in early term pregnancy: A rare cardiac complication of SARS-CoV-2 infection. BMJ Case Rep. 2020, 13, e239104. [Google Scholar] [CrossRef]
- Nejadrahim, R.; Khademolhosseini, S.; Kavandi, H.; Hajizadeh, R. Severe acute respiratory syndrome coronavirus-2- or pregnancy-related cardiomyopathy, a differential to be considered in the current pandemic: A case report. J. Med. Case Rep. 2021, 15, 143. [Google Scholar] [CrossRef]
- Soofi, M.A.; Shah, M.A.; Mhish, O.H.; AlSamadi, F. COVID-19 Infection During Pregnancy With Acute Heart Failure, Venous Thrombosis And Pneumonia. J. Ayub Med. Coll. Abbottabad. 2022, 34, 369–374. [Google Scholar] [CrossRef]
- França, A.; Pereira, D.D.V.; Rodrigues, E.V.; Vieira, F.N.; Machado, K.S.; Nogueira, P.A.; Fonseca, R.R.S.; Machado, L.F.A. Severe COVID-19 in Cardiopath Young Pregnant Patient without Vertical Transmission. Viruses 2022, 14, 675. [Google Scholar] [CrossRef]
- Gulersen, M.; Staszewski, C.; Grayver, E.; Tam, H.T.; Gottesman, E.; Isseroff, D.; Rochelson, B.; Bonanno, C. Coronavirus Disease 2019 (COVID-19)–related multisystem inflammatory syndrome in a pregnant woman. Obstet. Gynecol. 2021, 137, 418. [Google Scholar] [CrossRef]
- Stout, A.; Crichton, R.; Tahmasebi, F. Maternal death secondary to COVID-19 infection: A case report and review of the literature. Obstet. Med. 2020, 14, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Khodamoradi, Z.; Boogar, S.S.; Shirazi, F.K.H.; Kouhi, P. COVID-19 and Acute Pulmonary Embolism in Postpartum Patient. Emerg. Infect. Dis. 2020, 26, 1937–1939. [Google Scholar] [CrossRef] [PubMed]
- Zarrintan, A.; Boeoofeh, B.; Rabieipour, M.; Mohammadi, A.; Khademvatani, K.; Pirnejad, H.; Mirza-Aghazadeh-Attari, M. Pulmonary Thromboembolism in a Pregnant Patient with Severe COVID19: A Novel Case Report and Review of Literature. Arch. Clin. Infect. Dis. 2020, 15. [Google Scholar] [CrossRef]
- Goudarzi, S.; Firouzabadi, F.D.; Mahmoudzadeh, F.; Aminimoghaddam, S. Pulmonary embolism in pregnancy with COVID-19 infection: A case report. Clin. Case Rep. 2021, 9, 1882–1886. [Google Scholar] [CrossRef]
- Sinaci, S.; Ocal, D.F.; Ozden Tokalioglu, E.; Halici Ozturk, F.; Aydin Senel, S.; Keskin, L.H.; Moraloglu Tekin, O.; Sahin, D. Cardiotocographic features in COVID-19 infected pregnant women. J. Perinat. Med. 2022, 50, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Breslin, N.; Baptiste, C.; Miller, R.; Fuchs, K.; Goffman, D.; Gyamfi-Bannerman, C.; D’Alton, M. Coronavirus disease 2019 in pregnancy: Early lessons. Am. J. Obstet. Gynecol. MFM 2020, 2, 100111. [Google Scholar] [CrossRef] [PubMed]
- Donovan, B.M.; Spiel, M. Peripartum Severe COVID-19 Pneumonia: Fetal and Neonatal Implications. NeoReviews 2022, 23, e345–e353. [Google Scholar] [CrossRef]
- Rizzo, G.; Mappa, I.; Pietrolucci, M.E.; Lu, J.L.A.; Makatsarya, A.; D’Antonio, F. Effect of SARS-CoV-2 infection on fetal umbilical vein flow and cardiac function: A prospective study. J. Perinat. Med. 2022, 50, 398–403. [Google Scholar] [CrossRef]
- Turgut, E.; Sakcak, B.; Uyan Hendem, D.; Oluklu, D.; Goncu Ayhan, S.; Sahin, D. Decreased fetal cardiac output in pregnant women with severe SARS-CoV-2 infection. Echocardiography 2022, 39, 803–810. [Google Scholar] [CrossRef]
- Sule, G.A.; Aysegul, A.; Selcan, S.; Atakan, T.; Eda, O.T.; Deniz, O.; Filiz, H.O.; Ozlem, M.T.; Dilek, S. Effects of SARS-CoV-2 infection on fetal pulmonary artery Doppler parameters. Echocardiography 2021, 38, 1314–1318. [Google Scholar] [CrossRef]
- Anuk, A.T.; Tanacan, A.; Yetiskin, F.D.Y.; Buyuk, G.N.; Senel, S.A.; Keskin, H.L.; Moraloglu, O.; Uygur, D. Doppler assessment of the fetus in pregnant women recovered from COVID-19. J. Obstet. Gynaecol. Res. 2021, 47, 1757–1762. [Google Scholar] [CrossRef] [PubMed]
- Gracia-Perez-Bonfils, A.; Martinez-Perez, O.; Llurba, E.; Chandraharan, E. Fetal heart rate changes on the cardiotocograph trace secondary to maternal COVID-19 infection. Eur. J. Obs. Gynecol. Reprod. Biol. 2020, 252, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Yamaguchi, K.; Maegawa, Y.; Komine-Aizawa, S.; Kondo, E.; Ikeda, T. Intrauterine fetal death during COVID-19 pregnancy: Typical fetal heart rate changes, coagulopathy, and placentitis. J. Obstet. Gynaecol. Res. 2022, 48, 1978–1982. [Google Scholar] [CrossRef] [PubMed]
- Cetera, G.E.; D’Ambrosi, F.; Iurlaro, E.; Cesano, N.; Carbone, I.F.; De Marinis, S.; Ferrazzi, E. COVID-19-associated coagulopathy and unfavorable obstetric outcomes in the third trimester of pregnancy. Int. J. Gynaecol. Obstet. 2022, 157, 206. [Google Scholar] [CrossRef] [PubMed]
- Pelayo, J.; Pugliese, G.; Salacup, G.; Quintero, E.; Khalifeh, A.; Jaspan, D.; Sharma, B. Severe COVID-19 in Third Trimester Pregnancy: Multidisciplinary Approach. Case Rep. Crit. Care 2020, 2020, 8889487. [Google Scholar] [CrossRef]
- Gubbari, C.; Govindarajan, V.; Reddy, C.; Raman, P.; Supriya, M. Newborn with Nonimmune Hydrops Secondary to Fetal COVID-19 Myocarditis. Indian J. Pediatr. 2022, 89, 99. [Google Scholar] [CrossRef]
- Patel, M.; Thornburg, N. Stubblefield WB, Talbot HK, Coughlin MM, Feldstein LR, Self WH. Change in Antibodies to SARS-CoV-2 Over 60 Days Among Health Care Personnel in Nashville, Tennessee. JAMA 2020, 324, 1781. [Google Scholar] [CrossRef]
- Molteni, E.; Astley, C.M.; Ma, W.J.; Sudre, C.H.; Magee, L.A.; Murray, B.; Fall, T.; Gomez, M.F.; Tsereteli, N.; Franks, P.W.; et al. Symptoms and syndromes associated with SARS-CoV-2 infection and severity in pregnant women from two community cohorts. Sci. Rep. 2021, 11, 6928. [Google Scholar] [CrossRef]
- Chavan, N.; Shikhanshi; Kapote, D.; Deshmukh, P.; Sakhalkar, A. Study of maternal deaths with COVID-19 infection in a tertiary care centre. Int. J. Reprod. Contracept. Obstet. Gynecol. 2021, 11, 75. [Google Scholar] [CrossRef]
- Palomo, M.; Youssef, L.; Ramos, A.; Torramade-Moix, S.; Moreno-Castaño, A.B.; Martinez-Sanchez, J.; Bonastre, L.; Pino, M.; Gomez-Ramirez, P.; Martin, L.; et al. Differences and similarities in endothelial and angiogenic profiles of preeclampsia and COVID-19 in pregnancy. Am. J. Obstet. Gynecol. 2022, 227, 277.e1–277.e6. [Google Scholar] [CrossRef]
- Brandt, J.S.; Hill, J.; Reddy, A.; Schuster, M.; Patrick, H.S.; Rosen, T.; Sauer, M.V.; Boyle, C.; Ananth, C.V. Epidemiology of coronavirus disease 2019 in pregnancy: Risk factors and associations with adverse maternal and neonatal outcomes. Am. J. Obstet. Gynecol. 2021, 224, 389.e1–389.e9. [Google Scholar] [CrossRef] [PubMed]
- Goncu Ayhan, S.; Turgut, E.; Ozden Tokalioglu, E.; Oluklu, D.; Sakcak, B.; Uyan Hendem, D.; Tanacan, A.; Moraloglu Tekin, O.; Sahin, D. Post-COVID-19 fetal cardiac evaluation in moderate infection group of pregnant women. J. Clin. Ultrasound 2022, 50, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Radoi, V.; Pop, L.G.; Bacalbasa, N.; Panaitescu, A.M.; Ciobanu, A.M.; Cretoiu, D.; Toader, O.D. Fatal Association of Mirror and Eisenmenger Syndrome during the COVID-19 Pandemic. Medicina 2021, 57, 1031. [Google Scholar] [CrossRef]
- Agarwal, M.; Singh, S.; Sinha, U.; Bhushan, D. Extrahepatic portal vein thrombosis in a pregnant patient with COVID-19: A rare thrombotic event survivor. BMJ Case Rep. 2021, 14, e243697. [Google Scholar] [CrossRef] [PubMed]
- Mevada, S.A.; Mehendale, M.A.; Nayak, A.H.; Gite, P.M.; Khan, N.S. Cardiomyopathy in Pregnancy with COVID-19: An Enigma. J. South Asian Fed. Obstet. Gynaecol. 2020, 12, 243–244. [Google Scholar] [CrossRef]
- Mongula, J.E.; Frenken, M.W.E.; van Lijnschoten, G.; Arents, N.L.A.; de Wit-Zuurendonk, L.D.; Schimmel-de Kok, A.P.A.; van Runnard Heimel, P.J.; Porath, M.M.; Goossens, S. COVID-19 during pregnancy: Non-reassuring fetal heart rate, placental pathology and coagulopathy. Ultrasound Obstet. Gynecol. 2020, 56, 773–776. [Google Scholar] [CrossRef]
- Wang, G.; Stapley, E.; Peterson, S.; Parrott, J.; Clark-Ganheart, C. Persistent Fetal SVT in a COVID-19 Positive Pregnancy. Case Rep. Obs. Gynecol. 2022, 2022, 9933520. [Google Scholar] [CrossRef] [PubMed]
- Soma-Pillay, P.; Nelson-Piercy, C.; Tolppanen, H.; Mebazaa, A. Physiological changes in pregnancy: Review articles. Cardiovasc. J. Afr. 2016, 27, 89–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clerkin, K.J.; Fried, J.A.; Raikhelkar, J.; Sayer, G.; Griffin, J.M.; Masoumi, A.; Jain, S.S.; Burkhoff, D.; Kumaraiah, D.; Rabbani, L. COVID-19 and cardiovascular disease. Circulation 2020, 141, 1648–1655. [Google Scholar] [CrossRef] [Green Version]
- ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: Part 2—Care pathways, treatment, and follow-up. Eur. Heart J. 2022, 43, 1059–1103. [CrossRef]
- Dehghan, H.; Soleimani, A. Pulmonary thromboembolism with multiple right heart mural thrombus in a patient with COVID-19. J. Echocardiogr. 2020, 20, 124–125. [Google Scholar] [CrossRef] [PubMed]
- Bansal, M. Cardiovascular disease and COVID-19. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Shafiabadi Hassani, N.; Talakoob, H.; Karim, H.; Mozafari Bazargany, M.H.; Rastad, H. Cardiac magnetic resonance imaging findings in 2954 COVID-19 adult survivors: A comprehensive systematic review. J. Magn. Reson. Imaging 2022, 55, 866–880. [Google Scholar] [CrossRef] [PubMed]
- Karamitsos, T.D.; Arvanitaki, A.; Karvounis, H.; Neubauer, S.; Ferreira, V.M. Myocardial tissue characterization and fibrosis by imaging. JACC Cardiovasc. Imaging 2020, 13, 1221–1234. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liang, X.; Wang, H.; Li, L.; Xiong, G.; Mi, L. A considerable asymptomatic proportion and thromboembolism risk of pregnant women with COVID-19 infection in Wuhan, China. J. Perinat. Med. 2021, 49, 237–240. [Google Scholar] [CrossRef] [PubMed]
- Mehta, L.S.; Warnes, C.A.; Bradley, E.; Burton, T.; Economy, K.; Mehran, R.; Safdar, B.; Sharma, G.; Wood, M.; Valente, A.M. Cardiovascular considerations in caring for pregnant patients: A scientific statement from the American Heart Association. Circulation 2020, 141, e884–e903. [Google Scholar] [CrossRef] [PubMed]
- Regitz-Zagrosek, V.; Roos-Hesselink, J.W.; Bauersachs, J.; Blomström-Lundqvist, C.; Cifkova, R.; De Bonis, M.; Iung, B.; Johnson, M.R.; Kintscher, U.; Kranke, P. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy: The task force for the management of cardiovascular diseases during pregnancy of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 3165–3241. [Google Scholar] [CrossRef]
- Taranikanti, M. Physiological changes in cardiovascular system during normal pregnancy: A review. Indian J. Cardiovasc. Dis. Women-WINCARS 2018, 3, 062–067. [Google Scholar] [CrossRef] [Green Version]
- Zaigham, M.; Andersson, O. Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020, 99, 823–829. [Google Scholar] [CrossRef] [Green Version]
- Mullins, E.; Evans, D.; Viner, R.; O’Brien, P.; Morris, E. Coronavirus in pregnancy and delivery: Rapid review. Ultrasound Obstet. Gynecol. 2020, 55, 586–592. [Google Scholar] [CrossRef] [Green Version]
- Di Mascio, D.; Khalil, A.; Saccone, G.; Rizzo, G.; Buca, D.; Liberati, M.; Vecchiet, J.; Nappi, L.; Scambia, G.; Berghella, V.; et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: A systematic review and meta-analysis. Am. J. Obs. Gynecol. MFM 2020, 2, 100107. [Google Scholar] [CrossRef] [PubMed]
- Lassi, Z.S.; Ana, A.; Das, J.K.; Salam, R.A.; Padhani, Z.A.; Irfan, O.; Bhutta, Z.A. A systematic review and meta-analysis of data on pregnant women with confirmed COVID-19: Clinical presentation, and pregnancy and perinatal outcomes based on COVID-19 severity. J. Glob. Health 2021, 11, 05018. [Google Scholar] [CrossRef] [PubMed]
- Gheblawi, M.; Wang, K.; Viveiros, A.; Nguyen, Q.; Zhong, J.-C.; Turner, A.J.; Raizada, M.K.; Grant, M.B.; Oudit, G.Y. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: Celebrating the 20th anniversary of the discovery of ACE2. Circ. Res. 2020, 126, 1456–1474. [Google Scholar] [CrossRef] [PubMed]
- Narang, K.; Enninga, E.A.L.; Gunaratne, M.D.; Ibirogba, E.R.; Trad, A.T.A.; Elrefaei, A.; Theiler, R.N.; Ruano, R.; Szymanski, L.M.; Chakraborty, R. SARS-CoV-2 infection and COVID-19 during pregnancy: A multidisciplinary review. Mayo Clin. Proc. 2020, 95, 1750–1765. [Google Scholar] [CrossRef]
- Ferrario, C.M.; Trask, A.J.; Jessup, J.A. Advances in biochemical and functional roles of angiotensin-converting enzyme 2 and angiotensin-(1-7) in regulation of cardiovascular function. Am. J. Physiol. Heart Circ. Physiol. 2005, 289, H2281–H2290. [Google Scholar] [CrossRef] [Green Version]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Garovic, V.D.; Hayman, S.R. Hypertension in pregnancy: An emerging risk factor for cardiovascular disease. Nat. Clin. Pract. Nephrol. 2007, 3, 613–622. [Google Scholar] [CrossRef]
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. 2020, 130, 2620–2629. [Google Scholar] [CrossRef] [Green Version]
- Chousterman, B.G.; Swirski, F.K.; Weber, G.F. Cytokine storm and sepsis disease pathogenesis. Semin. Immunopathol. 2017, 39, 517–528. [Google Scholar] [CrossRef]
- Ye, Q.; Wang, B.; Mao, J. The pathogenesis and treatment of theCytokine Storm’in COVID-19. J. Infect. 2020, 80, 607–613. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Di Renzo, G.C.; Giardina, I. Coronavirus disease 2019 in pregnancy: Consider thromboembolic disorders and thromboprophylaxis. Am. J. Obstet. Gynecol. 2020, 223, 135. [Google Scholar] [CrossRef] [PubMed]
- Inciardi, R.M.; Lupi, L.; Zaccone, G.; Italia, L.; Raffo, M.; Tomasoni, D.; Cani, D.S.; Cerini, M.; Farina, D.; Gavazzi, E.; et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 819–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, L.; Li, X.; Chen, M.; Feng, Y.; Xiong, C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc. Res. 2020, 116, 1097–1100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avila, W.S.; de Carvalho, R.C. COVID-19: A New Challenge in Pregnancy and Heart Disease. Arq. Bras. Cardiol. 2020, 115, 1–4. [Google Scholar] [CrossRef]
- Bauersachs, J.; König, T.; van der Meer, P.; Petrie, M.C.; Hilfiker-Kleiner, D.; Mbakwem, A.; Hamdan, R.; Jackson, A.M.; Forsyth, P.; de Boer, R.A. Pathophysiology, diagnosis and management of peripartum cardiomyopathy: A position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur. J. Heart Fail. 2019, 21, 827–843. [Google Scholar] [CrossRef]
- Lippi, G.; Lavie, C.J.; Sanchis-Gomar, F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog. Cardiovasc. Dis. 2020, 63, 390. [Google Scholar] [CrossRef]
- Hantoushzadeh, S.; Nabavian, S.M.; Soleimani, Z.; Soleimani, A. COVID-19 Disease During Pregnancy and Peripartum Period: A Cardiovascular Review. Curr. Probl. Cardiol. 2022, 47, 100888. [Google Scholar] [CrossRef]
- Avila, W.S.; Kirschbaum, M.; Devido, M.S.; Demarchi, L.M.M.F. COVID-19, congenital heart disease, and pregnancy: Dramatic conjunction—Case report. Eur. Heart J.-Case Rep. 2021, 5, ytab291. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Rabinovich, A.; Abdul-Kadir, R.; Thachil, J.; Iba, T.; Othman, M.; Erez, O. DIC in obstetrics: Diagnostic score, highlights in management, and international registry-communication from the DIC and Women’s Health SSCs of the International Society of Thrombosis and Haemostasis. J. Thromb. Haemost. 2019, 17, 1562–1566. [Google Scholar] [CrossRef] [PubMed]
- Servante, J.; Swallow, G.; Thornton, J.G.; Myers, B.; Munireddy, S.; Malinowski, A.K.; Othman, M.; Li, W.; O’Donoghue, K.; Walker, K.F. Haemostatic and thrombo-embolic complications in pregnant women with COVID-19: A systematic review and critical analysis. BMC Pregnancy Childbirth 2021, 21, 108. [Google Scholar] [CrossRef]
- Levi, M.; Sivapalaratnam, S. Disseminated intravascular coagulation: An update on pathogenesis and diagnosis. Expert Rev. Hematol. 2018, 11, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Ranucci, M.; Ballotta, A.; Di Dedda, U.; Baryshnikova, E.; Dei Poli, M.; Resta, M.; Falco, M.; Albano, G.; Menicanti, L. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J. Thromb. Haemost. 2020, 18, 1747–1751. [Google Scholar] [CrossRef] [PubMed]
- Hunt, B.J.; Jurd, K.M. Endothelial cell activation: A central pathophysiological process. Br. Med. J. 1998, 316, 1328. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Idell, S. Coagulation, fibrinolysis, and fibrin deposition in acute lung injury. Crit. Care Med. 2003, 31, S213–S220. [Google Scholar] [CrossRef]
- Obi, A.T.; Barnes, G.D.; Wakefield, T.W.; Brown, S.; Eliason, J.L.; Arndt, E.; Henke, P.K. Practical diagnosis and treatment of suspected venous thromboembolism during COVID-19 pandemic. J. Vasc. Surg. Venous Lymphat. Disord. 2020, 8, 526–534. [Google Scholar] [CrossRef]
- Bermejo-Martin, J.F.; Almansa, R.; Torres, A.; González-Rivera, M.; Kelvin, D.J. COVID-19 as a cardiovascular disease: The potential role of chronic endothelial dysfunction. Cardiovasc. Res. 2020, 116, e132–e133. [Google Scholar] [CrossRef]
- Jin, Y.; Ji, W.; Yang, H.; Chen, S.; Zhang, W.; Duan, G. Endothelial activation and dysfunction in COVID-19: From basic mechanisms to potential therapeutic approaches. Signal Transduct. Target. Ther. 2020, 5, 293. [Google Scholar] [CrossRef] [PubMed]
- Teuwen, L.-A.; Geldhof, V.; Pasut, A.; Carmeliet, P. COVID-19: The vasculature unleashed. Nat. Rev. Immunol. 2020, 20, 389–391. [Google Scholar] [CrossRef] [PubMed]
- Herrey, A.S.; Osman, A.; Soma-Pillay, P.; Sliwa, K.; Ntusi, N.A. COVID-19 and the cardiovascular system in pregnancy. SA Heart 2020, 17, 288–295. [Google Scholar] [CrossRef]
- Mohammadi, S.; Abouzaripour, M.; Hesam Shariati, N.; Hesam Shariati, M.B. Ovarian vein thrombosis after coronavirus disease (COVID-19) infection in a pregnant woman: Case report. J. Thromb. Thrombolysis 2020, 50, 604–607. [Google Scholar] [CrossRef]
- Martinelli, I.; Ferrazzi, E.; Ciavarella, A.; Erra, R.; Iurlaro, E.; Ossola, M.; Lombardi, A.; Blasi, F.; Mosca, F.; Peyvandi, F. Pulmonary embolism in a young pregnant woman with COVID-19. Thromb. Res. 2020, 191, 36–37. [Google Scholar] [CrossRef]
- Tang, N.; Bai, H.; Chen, X.; Gong, J.; Li, D.; Sun, Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020, 18, 1094–1099. [Google Scholar] [CrossRef] [Green Version]
- IoOaG, R. COVID-19 Infection Guidance for Maternity Services. Inst. Obstet. Gynaecol.-R. Coll. Physicians Irel. (RCPI) 2020, 21. [Google Scholar]
- D’Souza, R.; Malhamé, I.; Teshler, L.; Acharya, G.; Hunt, B.J.; McLintock, C. A critical review of the pathophysiology of thrombotic complications and clinical practice recommendations for thromboprophylaxis in pregnant patients with COVID-19. Acta Obstet. Gynecol. Scand. 2020, 99, 1110–1120. [Google Scholar] [CrossRef]
- Kwiatkowski, S.; Borowski, D.; Kajdy, A.; Poon, L.; Rokita, W.; Wielgos, M. Why we should not stop giving aspirin to pregnant women during the COVID-19 pandemic. Ultrasound Obstet. Gynecol. 2020, 55, 841. [Google Scholar] [CrossRef]
- Yuan, S.-M. Fetal arrhythmias: Surveillance and management. Hell. J. Cardiol. 2019, 60, 72–81. [Google Scholar] [CrossRef]
- Aldemir, O.; Karahanoğlu, E.; Esinler, D.; Yerebasmaz, N.; Fadıllıoğlu, E. Umbilical artery Doppler findings in patients with preterm premature rupture of membranes. Gynecol. Obstet. Reprod. Med. 2014, 20, 143–145. [Google Scholar]
- Khalil, A.; Von Dadelszen, P.; Draycott, T.; Ugwumadu, A.; O’Brien, P.; Magee, L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA 2020, 324, 705–706. [Google Scholar] [CrossRef] [PubMed]
- Ayhan, S.G.; Tanacan, A.; Atalay, A.; Sinaci, S.; Tokalioglu, E.O.; Sahin, D.; Tekin, O.M. Assessment of fetal Doppler parameters in pregnant women with COVID-19 infection: A prospective case-control study. J. Perinat. Med. 2021, 49, 697–701. [Google Scholar] [CrossRef] [PubMed]
- Fenizia, C.; Biasin, M.; Cetin, I.; Vergani, P.; Mileto, D.; Spinillo, A.; Gismondo, M.R.; Perotti, F.; Callegari, C.; Mancon, A. Analysis of SARS-CoV-2 vertical transmission during pregnancy. Nat. Commun. 2020, 11, 5128. [Google Scholar] [CrossRef] [PubMed]
- Carosso, A.; Cosma, S.; Serafini, P.; Benedetto, C.; Mahmood, T. How to reduce the potential risk of vertical transmission of SARS-CoV-2 during vaginal delivery? Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 250, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Gao, X.; Zheng, H.; Yan, M.; Liang, W.; Shao, Z.; Li, W.; Zhang, E.; Hu, Y.; Hai, R. Specific immunoglobulin g antibody detected in umbilical blood and amniotic fluid from a pregnant woman infected by the coronavirus associated with severe acute respiratory syndrome. Clin. Vaccine Immunol. 2004, 11, 1182–1184. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.; Guo, J.; Wang, C.; Luo, F.; Yu, X.; Zhang, W.; Li, J.; Zhao, D.; Xu, D.; Gong, Q. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet 2020, 395, 809–815. [Google Scholar] [CrossRef] [Green Version]
- Shek, C.C.; Ng, P.C.; Fung, G.P.; Cheng, F.W.; Chan, P.K.; Peiris, M.J.; Lee, K.H.; Wong, S.F.; Cheung, H.M.; Li, A.M. Infants born to mothers with severe acute respiratory syndrome. Pediatrics 2003, 112, e254. [Google Scholar] [CrossRef] [Green Version]
- Yang, P.; Wang, X.; Liu, P.; Wei, C.; He, B.; Zheng, J.; Zhao, D. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J. Clin. Virol. 2020, 127, 104356. [Google Scholar] [CrossRef]
- Büke, B.; Akkaya, H. A non-invasive method to rule out transient tachypnea of the newborn (TTN): Fetal pulmonary artery acceleration to ejection time ratio. J. Perinat. Med. 2018, 46, 219–224. [Google Scholar] [CrossRef]
- Azpurua, H.; Norwitz, E.R.; Campbell, K.H.; Funai, E.F.; Pettker, C.M.; Kleine, M.; Bahtiyar, M.O.; Malkus, H.; Copel, J.A.; Thung, S.F. Acceleration/ejection time ratio in the fetal pulmonary artery predicts fetal lung maturity. Am. J. Obstet. Gynecol. 2010, 203, 40.e1–40.e8. [Google Scholar] [CrossRef] [PubMed]
- Turgut, E.; Ayhan, S.G.; Oluklu, D.; Tokalioglu, E.O.; Tekin, O.M.; Sahin, D. Fetal pulmonary artery Doppler evaluation in pregnant women after recovery from COVID-19. Int. J. Gynecol. Obstet. 2021, 155, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Liu, J. Lung ultrasonography for the diagnosis of neonatal lung disease. J. Matern.-Fetal Neonatal Med. 2014, 27, 856–861. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.; Kalafat, E.; Blakeway, H.; Townsend, R.; O’Brien, P.; Morris, E.; Draycott, T.; Thangaratinam, S.; Le Doare, K.; Ladhani, S. Systematic review and meta-analysis of the effectiveness and perinatal outcomes of COVID-19 vaccination in pregnancy. Nat. Commun. 2022, 13, 2414. [Google Scholar] [CrossRef]
- Kirschbaum, M.; Devido, M.; Azeka, E.; Demarchi, L.; Santos, J.; Pinto, D.; Hajjar, L.; Tarasoutchi, F.; Park, M.; Avila, W. COVID-19 in pregnant women with heart diseases. Adverse maternal and fetal outcomes. Case series from InCor registry of Pregnancy and Heart Disease. Eur. Heart J. 2021, 42, ehab724.2890. [Google Scholar] [CrossRef]
- Şahin, D.; Tanaçan, A.; Webster, S.N.; Tekin, Ö.M. Pregnancy and COVID-19: Prevention, vaccination, therapy, and beyond. Turk. J. Med. Sci. 2021, 51, 3312–3326. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yaghoobpoor, S.; Fathi, M.; Vakili, K.; Tutunchian, Z.; Dehghani, M.; Bahrami, A.; Hajibeygi, R.; Eslami, S.; Yaghoobpour, T.; Hajiesmaeili, M. Cardiovascular Complications of COVID-19 among Pregnant Women and Their Fetuses: A Systematic Review. J. Clin. Med. 2022, 11, 6194. https://doi.org/10.3390/jcm11206194
Yaghoobpoor S, Fathi M, Vakili K, Tutunchian Z, Dehghani M, Bahrami A, Hajibeygi R, Eslami S, Yaghoobpour T, Hajiesmaeili M. Cardiovascular Complications of COVID-19 among Pregnant Women and Their Fetuses: A Systematic Review. Journal of Clinical Medicine. 2022; 11(20):6194. https://doi.org/10.3390/jcm11206194
Chicago/Turabian StyleYaghoobpoor, Shirin, Mobina Fathi, Kimia Vakili, Zohreh Tutunchian, Mina Dehghani, Ashkan Bahrami, Ramtin Hajibeygi, Samira Eslami, Tina Yaghoobpour, and Mohammadreza Hajiesmaeili. 2022. "Cardiovascular Complications of COVID-19 among Pregnant Women and Their Fetuses: A Systematic Review" Journal of Clinical Medicine 11, no. 20: 6194. https://doi.org/10.3390/jcm11206194
APA StyleYaghoobpoor, S., Fathi, M., Vakili, K., Tutunchian, Z., Dehghani, M., Bahrami, A., Hajibeygi, R., Eslami, S., Yaghoobpour, T., & Hajiesmaeili, M. (2022). Cardiovascular Complications of COVID-19 among Pregnant Women and Their Fetuses: A Systematic Review. Journal of Clinical Medicine, 11(20), 6194. https://doi.org/10.3390/jcm11206194








