Comparative Effectiveness Research: A Roadmap to Sail the Seas of IBD Therapies
Abstract
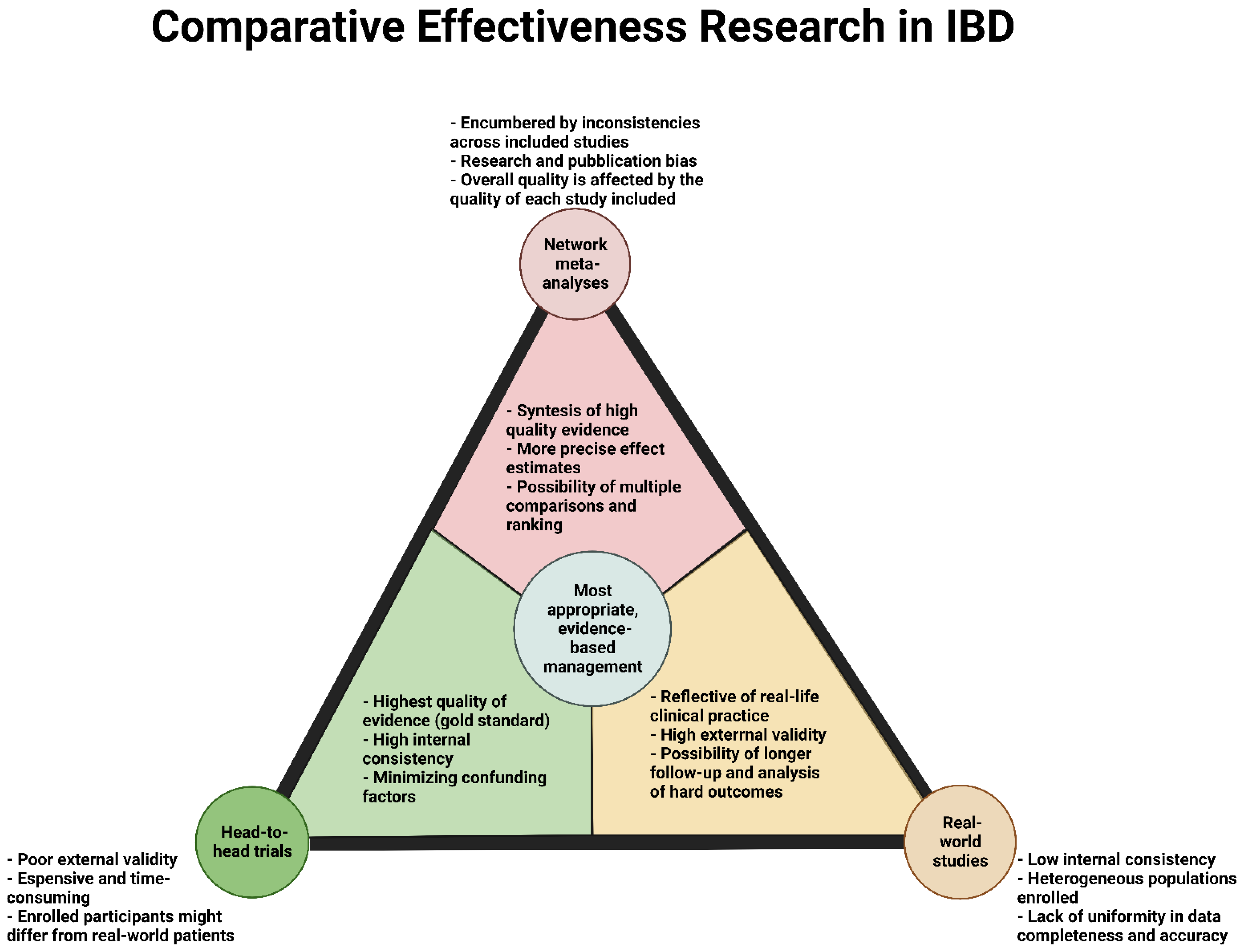
1. Introduction
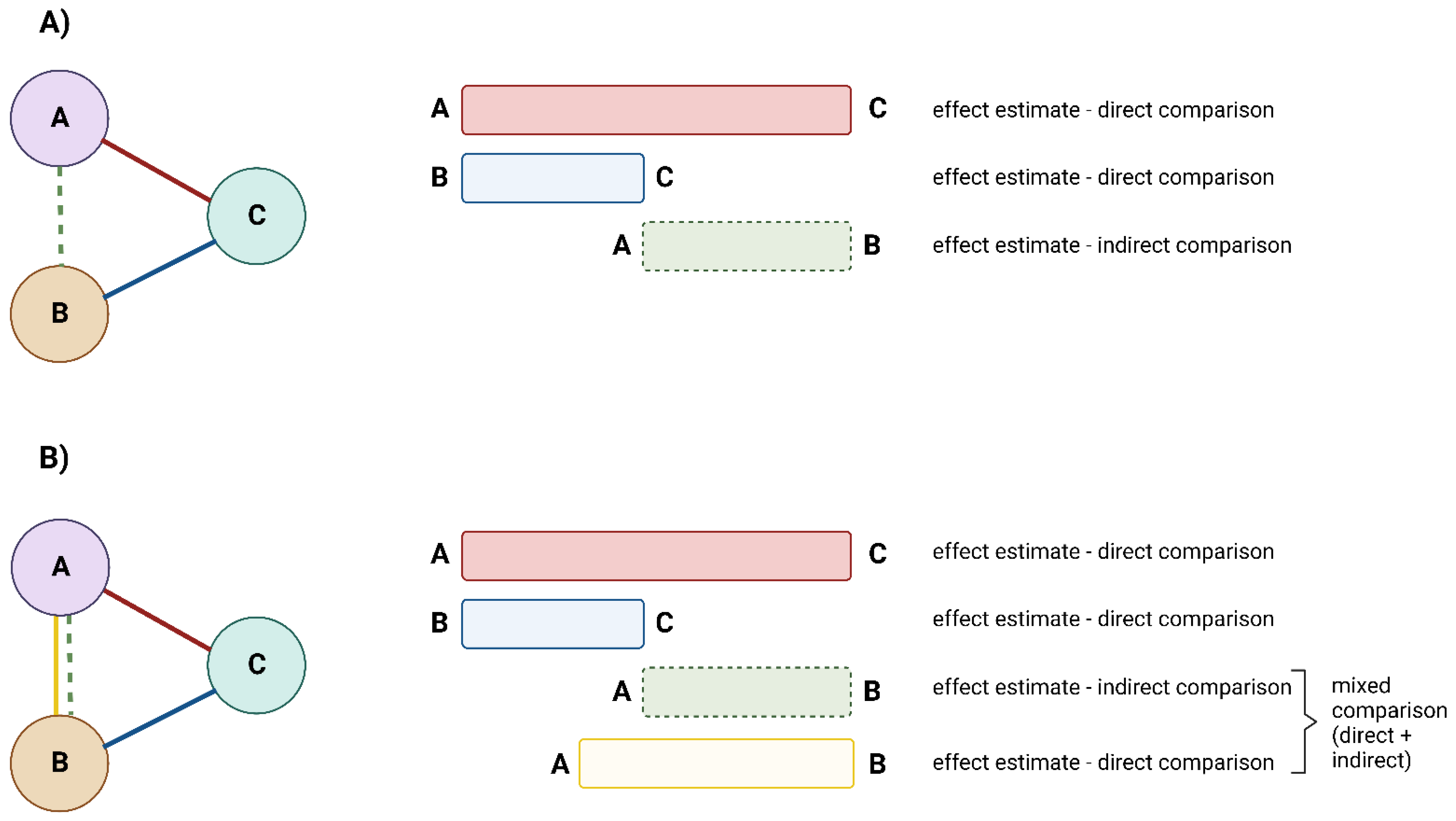
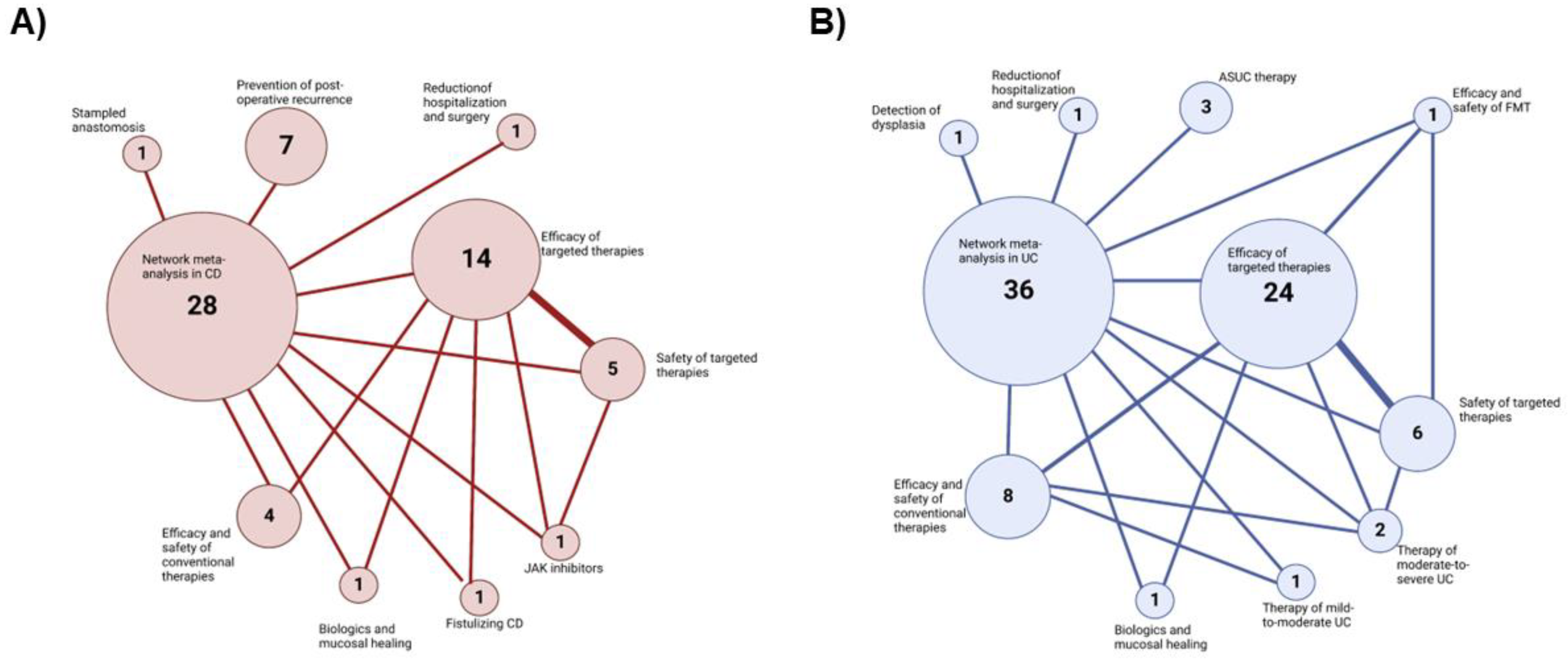
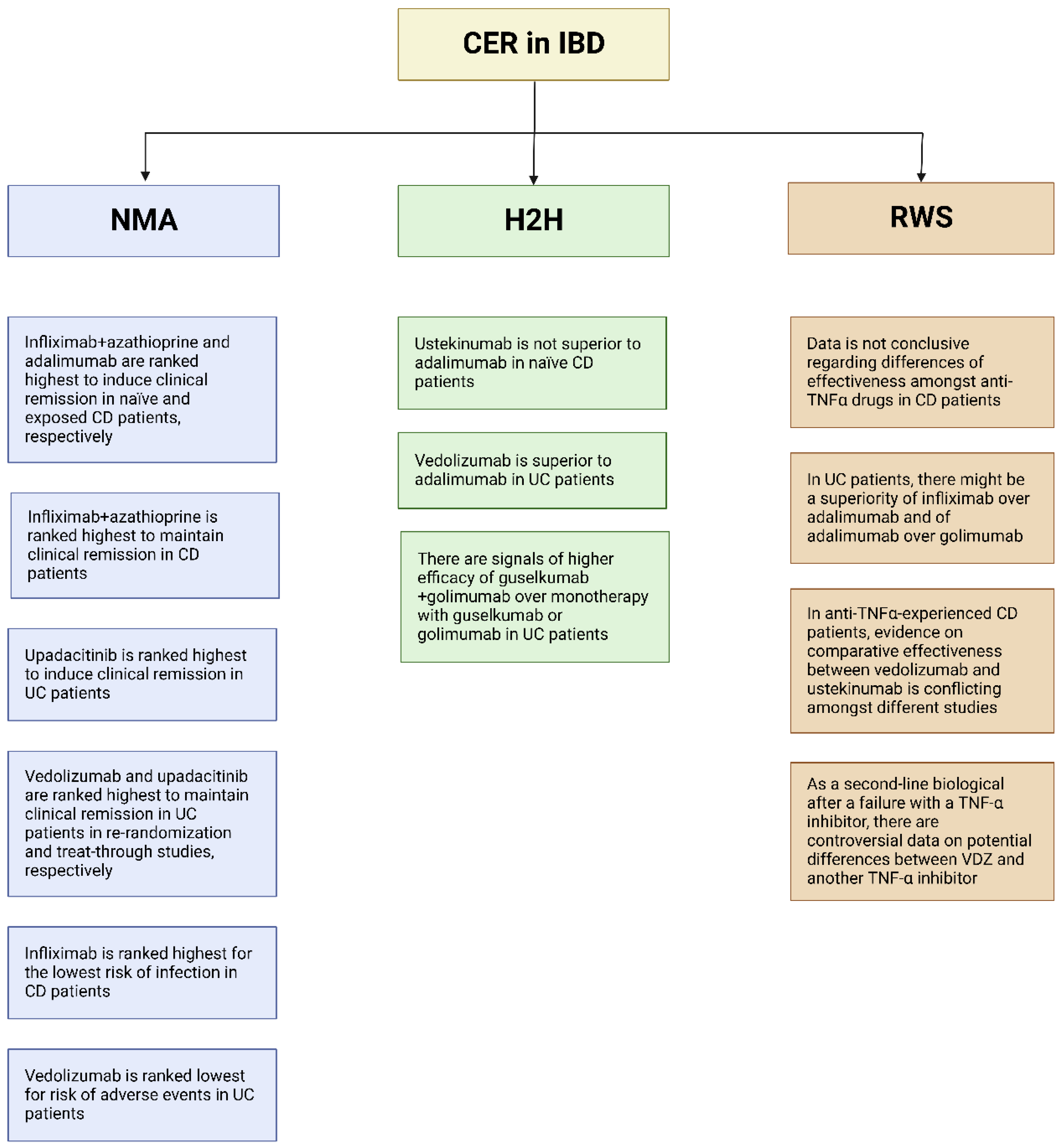
2. Network Meta-Analyses
Network Metanalysis in IBD
3. Head-to-Head Trials in IBD
3.1. Placebo-Controlled Trial with a Non-Powered Reference Arm
3.2. Non-Inferiority Trials
3.3. Superiority Trials
4. Real-Word Studies
4.1. Anti-TNF-α within the Class
4.2. Anti TNF-α outside the Class (vs. Vedolizumab)
4.3. Vedolizumab vs. Ustekinumab in Crohn’s Disease
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Privitera, G.; Pugliese, D.; Lopetuso, L.R.; Scaldaferri, F.; Neri, M.; Guidi, L.; Gasbarrini, A.; Armuzzi, A. Novel trends with biologics in inflammatory bowel disease: Sequential and combined approaches. Therap. Adv. Gastroenterol. 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed]
- Raine, T.; Bonovas, S.; Burisch, J.; Kucharzik, T.; Adamina, M.; Annese, V.; Bachmann, O.; Bettenworth, D.; Chaparro, M.; Czuber-Dochan, W.; et al. ECCO Guidelines on Therapeutics in Ulcerative Colitis: Medical Treatment. J. Crohns. Colitis 2022, 16, 2–17. [Google Scholar] [CrossRef]
- Feuerstein, J.D.; Isaacs, K.L.; Schneider, Y.; Siddique, S.M.; Falck-Ytter, Y.; Singh, S.; Chachu, K.; Day, L.; Lebwohl, B.; Muniraj, T.; et al. AGA Clinical Practice Guidelines on the Management of Moderate to Severe Ulcerative Colitis. Gastroenterology 2020, 158, 1450–1461. [Google Scholar] [CrossRef]
- Singh, S.; Murad, M.H.; Fumery, M.; Dulai, P.S.; Sandborn, W.J. First- and Second-line Pharmacotherapies for Patients with Moderate to Severely Active Ulcerative Colitis: An Updated Network Meta-Analysis. Clin. Gastroenterol. Hepatol. 2020, 18, 2179–2191.e6. [Google Scholar] [CrossRef]
- Macaluso, F.S.; Orlando, A.; Papi, C.; Festa, S.; Pugliese, D.; Bonovas, S.; Pansieri, C.; Piovani, D.; Fiorino, G.; Fantini, M.C.; et al. Use of biologics and small molecule drugs for the management of moderate to severe ulcerative colitis: IG-IBD clinical guidelines based on the GRADE methodology. Dig. Liver Dis. 2022, 54, 440–451. [Google Scholar] [CrossRef]
- IOM (Institute of Medicine). Initial National Priorities for Comparative Effectiveness Research; National Academies Press: Washington, DC, USA, 2009; ISBN 0309138361. [Google Scholar]
- Fritz, J.M.; Cleland, J. Effectiveness versus efficacy: More than a debate over language. J. Orthop. Sports Phys. Ther. 2003, 33, 163–165. [Google Scholar] [CrossRef]
- Gopalakrishnan, S.; Ganeshkumar, P. Systematic reviews and meta-analysis: Understanding the best evidence in primary healthcare. J. Fam. Med. Prim. Care 2013, 2, 9. [Google Scholar] [CrossRef]
- Dias, S.; Caldwell, D.M. Network meta-Analysis explained. Arch. Dis. Child. Fetal Neonatal Ed. 2019, 104, F8–F12. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Sandborn, W.J.; Colombel, J.F.; Feagan, B.G.; Panaccione, R.; Hanauer, S.; Schreiber, S.; Peyrin-Biroulet, L.; Vermeire, S.; Eichner, S.; et al. Interpreting Registrational Clinical Trials of Biological Therapies in Adults with Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2016, 22, 2711–2723. [Google Scholar] [CrossRef] [PubMed]
- Ha, C.; Ullman, T.A.; Siegel, C.A.; Kornbluth, A. Patients Enrolled in Randomized Controlled Trials Do Not Represent the Inflammatory Bowel Disease Patient Population. Clin. Gastroenterol. Hepatol. 2012, 10, 1002–1007. [Google Scholar] [CrossRef] [PubMed]
- Salanti, G.; Ades, A.E.; Ioannidis, J.P.A. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J. Clin. Epidemiol. 2011, 64, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Bafeta, A.; Trinquart, L.; Seror, R.; Ravaud, P. Reporting of results from network meta-analyses: Methodological systematic review. BMJ 2014, 348, g1741. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Murad, M.H.; Fumery, M.; Sedano, R.; Jairath, V.; Panaccione, R.; Sandborn, W.J.; Ma, C. Comparative efficacy and safety of biologic therapies for moderate-to-severe Crohn’s disease: A systematic review and network meta-analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 1002–1014. [Google Scholar] [CrossRef]
- Sands, B.E.; Irving, P.M.; Hoops, T.; Izanec, J.L.; Gao, L.L.; Gasink, C.; Greenspan, A.; Allez, M.; Danese, S.; Hanauer, S.B.; et al. Ustekinumab versus adalimumab for induction and maintenance therapy in biologic-naive patients with moderately to severely active Crohn’s disease: A multicentre, randomised, double-blind, parallel-group, phase 3b trial. Lancet 2022, 399, 2200–2211. [Google Scholar] [CrossRef]
- Colombel, J.F.; Sandborn, W.J.; Reinisch, W.; Mantzaris, G.J.; Kornbluth, A.; Rachmilewitz, D.; Lichtiger, S.; D’Haens, G.; Diamond, R.H.; Broussard, D.L.; et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N. Engl. J. Med. 2010, 362, 1383–1395. [Google Scholar] [CrossRef]
- Matsumoto, T.; Motoya, S.; Watanabe, K.; Hisamatsu, T.; Nakase, H.; Yoshimura, N.; Ishida, T.; Kato, S.; Nakagawa, T.; Esaki, M.; et al. Adalimumab monotherapy and a combination with azathioprine for Crohn’s disease: A prospective, randomized trial. J. Crohn’s Colitis 2016, 10, 1259–1266. [Google Scholar] [CrossRef]
- Rutgeerts, P.; Van Assche, G.; Sandborn, W.J.; Wolf, D.C.; Geboes, K.; Colombel, J.F.; Reinisch, W.; Kumar, A.; Lazar, A.; Camez, A.; et al. Adalimumab induces and maintains mucosal healing in patients with Crohn’s disease: Data from the EXTEND trial. Gastroenterology 2012, 142, 1102–1111.e2. [Google Scholar] [CrossRef]
- Sandborn, W.J.; Rutgeerts, P.; Enns, R.; Hanauer, S.B.; Colombel, J.F.; Panaccione, R.; D’Haens, G.; Li, J.; Rosenfeld, M.R.; Kent, J.D.; et al. Adalimumab induction therapy for Crohn disease previously treated with infliximab: A randomized trial. Ann. Intern. Med. 2007, 146, 829–838. [Google Scholar] [CrossRef]
- Lasa, J.S.; Olivera, P.A.; Danese, S.; Peyrin-Biroulet, L. Efficacy and safety of biologics and small molecule drugs for patients with moderate-to-severe ulcerative colitis: A systematic review and network meta-analysis. Lancet Gastroenterol. Hepatol. 2022, 7, 161–170. [Google Scholar] [CrossRef]
- Rubin, D.T.; Dotan, I.; DuVall, A.; Bouhnik, Y.; Radford-Smith, G.; Higgins, P.D.R.; Mishkin, D.S.; Arrisi, P.; Scalori, A.; Oh, Y.S.; et al. Etrolizumab versus adalimumab or placebo as induction therapy for moderately to severely active ulcerative colitis (HIBISCUS): Two phase 3 randomised, controlled trials. Lancet Gastroenterol. Hepatol. 2022, 7, 17–27. [Google Scholar] [CrossRef]
- Sands, B.E.; Peyrin-Biroulet, L.; Loftus, E.V.; Danese, S.; Colombel, J.-F.; Törüner, M.; Jonaitis, L.; Abhyankar, B.; Chen, J.; Rogers, R.; et al. Vedolizumab versus Adalimumab for Moderate-to-Severe Ulcerative Colitis. N. Engl. J. Med. 2019, 381, 1215–1226. [Google Scholar] [CrossRef] [PubMed]
- Danese, S.; Colombel, J.F.; Lukas, M.; Gisbert, J.P.; D’Haens, G.; Hayee, B.; Panaccione, R.; Kim, H.S.; Reinisch, W.; Tyrrell, H.; et al. Etrolizumab versus infliximab for the treatment of moderately to severely active ulcerative colitis (GARDENIA): A randomised, double-blind, double-dummy, phase 3 study. Lancet Gastroenterol. Hepatol. 2022, 7, 118–127. [Google Scholar] [CrossRef]
- Khanna, R.; Bressler, B.; Levesque, B.G.; Zou, G.; Stitt, L.W.; Greenberg, G.R.; Panaccione, R.; Bitton, A.; Paré, P.; Vermeire, S.; et al. Early combined immunosuppression for the management of Crohn’s disease (REACT): A cluster randomised controlled trial. Lancet 2015, 386, 1825–1834. [Google Scholar] [CrossRef]
- Armstrong, K. Methods in comparative effectiveness research. J. Clin. Oncol. 2012, 30, 4208–4214. [Google Scholar] [CrossRef] [PubMed]
- Pouillon, L.; Travis, S.; Bossuyt, P.; Danese, S.; Peyrin-Biroulet, L. Head-to-head trials in inflammatory bowel disease: Past, present and future. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 365–376. [Google Scholar] [CrossRef]
- Kamm, M.A.; Sandborn, W.J.; Gassull, M.; Schreiber, S.; Jackowski, L.; Butler, T.; Lyne, A.; Stephenson, D.; Palmen, M.; Joseph, R.E. Once-daily, high-concentration MMX mesalamine in active ulcerative colitis. Gastroenterology 2007, 132, 66–75. [Google Scholar] [CrossRef]
- Sandborn, W.J.; Travis, S.; Moro, L.; Jones, R.; Gautille, T.; Bagin, R.; Huang, M.; Yeung, P.; Ballard, E.D. Once-daily budesonide MMX® extended-release tablets induce remission in patients with mild to moderate ulcerative colitis: Results from the CORE I study. Gastroenterology 2012, 143, 1218–1226.e2. [Google Scholar] [CrossRef]
- Williams, J.G.; Alam, M.F.; Alrubaiy, L.; Arnott, I.; Clement, C.; Cohen, D.; Gordon, J.N.; Hawthorne, A.B.; Hilton, M.; Hutchings, H.A.; et al. Infliximab versus ciclosporin for steroid-resistant acute severe ulcerative colitis (CONSTRUCT): A mixed methods, open-label, pragmatic randomised trial. Lancet Gastroenterol. Hepatol. 2016, 1, 15–24. [Google Scholar] [CrossRef]
- Jørgensen, K.K.; Olsen, I.C.; Goll, G.L.; Lorentzen, M.; Bolstad, N.; Haavardsholm, E.A.; Lundin, K.E.A.; Mørk, C.; Jahnsen, J.; Kvien, T.K.; et al. Switching from originator infliximab to biosimilar CT-P13 compared with maintained treatment with originator infliximab (NOR-SWITCH): A 52-week, randomised, double-blind, non-inferiority trial. Lancet 2017, 389, 2304–2316. [Google Scholar] [CrossRef]
- Sands, B.E.; Feagan, B.G.; Sandborn, W.J.; Shipitofsky, N.; Marko, M.; Sheng, S.; Johanns, J.; Germinaro, M.; Vetter, M.; Panés, J. OP36 Efficacy and safety of combination induction therapy with guselkumab and golimumab in participants with moderately-to-severely active Ulcerative Colitis: Results through week 12 of a phase 2a randomized, double-blind, active-controlled, parallel-group, multicenter, proof-of-concept study. J. Crohn’s Colitis 2022, 16, i042–i043. [Google Scholar] [CrossRef]
- Olivera, P.; Sandborn, W.J.; Panés, J.; Baumann, C.; D’Haens, G.; Vermeire, S.; Danese, S.; Peyrin-Biroulet, L. Physicians’ perspective on the clinical meaningfulness of inflammatory bowel disease trial results: An International Organization for the Study of Inflammatory Bowel Disease (IOIBD) survey. Aliment. Pharmacol. Ther. 2018, 47, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Tsui, M.; Rehal, S.; Jairath, V.; Kahan, B.C. Most noninferiority trials were not designed to preserve active comparator treatment effects. J. Clin. Epidemiol. 2019, 110, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Oxford Centre for Evidence-Based Medicine: Levels of Evidence (March 2009)—Centre for Evidence-Based Medicine (CEBM), University of Oxford. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 (accessed on 2 August 2022).
- Axelrad, J.; Bernheim, O.; Colombel, J.F.; Malerba, S.; Ananthakrishnan, A.; Yajnik, V.; Hoffman, G.; Agrawal, M.; Lukin, D.; Desai, A.; et al. Risk of New or Recurrent Cancer in Patients With Inflammatory Bowel Disease and Previous Cancer Exposed to Immunosuppressive and Anti-Tumor Necrosis Factor Agents. Clin. Gastroenterol. Hepatol. 2016, 14, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Vegh, Z.; Burisch, J.; Pedersen, N.; Kaimakliotis, I.; Duricova, D.; Bortlik, M.; Kofod Vinding, K.; Avnstrøm, S.; Olsen, J.; Nielsen, K.R.; et al. Treatment Steps, Surgery, and Hospitalization Rates During the First Year of Follow-up in Patients with Inflammatory Bowel Diseases from the 2011 ECCO-Epicom Inception Cohort On behalf of the EpiCom Northern Italy centre based in Crema. J. Crohn’s Colitis 2015, 9, 747–753. [Google Scholar] [CrossRef]
- Pugliese, D.; Daperno, M.; Fiorino, G.; Savarino, E.; Mosso, E.; Biancone, L.; Testa, A.; Sarpi, L.; Cappello, M.; Bodini, G.; et al. Real-life effectiveness of ustekinumab in inflammatory bowel disease patients with concomitant psoriasis or psoriatic arthritis: An IG-IBD study. Dig. Liver Dis. 2019, 51, 972–977. [Google Scholar] [CrossRef]
- Pugliese, D.; Guidi, L.; Ferraro, P.M.; Marzo, M.; Felice, C.; Celleno, L.; Landi, R.; Andrisani, G.; Pizzolante, F.; De Vitis, I.; et al. Paradoxical psoriasis in a large cohort of patients with inflammatory bowel disease receiving treatment with anti-TNF alpha: 5-year follow-up study. Aliment. Pharmacol. Ther. 2015, 42, 880–888. [Google Scholar] [CrossRef]
- Odufalu, F.D.; Long, M.; Lin, K.; Mahadevan, U.; PIANO Investigators from the Crohn’s and Colitis Foundation (CCF) Clinical Research Alliance recruited patients for their respective centers for participant enrollment. Exposure to corticosteroids in pregnancy is associated with adverse perinatal outcomes among infants of mothers with inflammatory bowel disease: Results from the PIANO registry. Gut 2022, 71, 1766–1772. [Google Scholar] [CrossRef]
- Sebastian, S.; Black, C.; Pugliese, D.; Armuzzi, A.; Sahnan, K.; Elkady, S.M.; Katsanos, K.H.; Christodoulou, D.K.; Selinger, C.; Maconi, G.; et al. The role of multimodal treatment in Crohn’s disease patients with perianal fistula: A multicentre retrospective cohort study. Aliment. Pharmacol. Ther. 2018, 48, 941–950. [Google Scholar] [CrossRef]
- Vavricka, S.R.; Gubler, M.; Gantenbein, C.; Spoerri, M.; Froehlich, F.; Seibold, F.; Protic, M.; Michetti, P.; Straumann, A.; Fournier, N.; et al. Anti-TNF Treatment for Extraintestinal Manifestations of Inflammatory Bowel Disease in the Swiss IBD Cohort Study. Inflamm. Bowel Dis. 2017, 23, 1174–1181. [Google Scholar] [CrossRef]
- Pugliese, D.; Privitera, G.; Crispino, F.; Mezzina, N.; Castiglione, F.; Fiorino, G.; Laterza, L.; Viola, A.; Bertani, L.; Caprioli, F.; et al. Effectiveness and safety of vedolizumab in a matched cohort of elderly and nonelderly patients with inflammatory bowel disease: The IG-IBD LIVE study. Aliment. Pharmacol. Ther. 2022, 56, 95–109. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Andersen, N.N.; Andersson, M.; Loftus, E.V.; Jess, T. Comparison of infliximab with adalimumab in 827 biologic-naïve patients with Crohn’s disease: A population-based Danish cohort study. Aliment. Pharmacol. Ther. 2018, 47, 596–604. [Google Scholar] [CrossRef] [PubMed]
- Macaluso, F.S.; Fries, W.; Privitera, A.C.; Cappello, M.; Siringo, S.; Inserra, G.; Magnano, A.; Di Mitri, R.; Mocciaro, F.; Belluardo, N.; et al. A Propensity Score-matched Comparison of Infliximab and Adalimumab in Tumour Necrosis Factor-α Inhibitor-naïve and Non-naïve Patients With Crohn’s Disease: Real-Life Data From the Sicilian Network for Inflammatory Bowel Disease. J. Crohns. Colitis 2019, 13, 209–217. [Google Scholar] [CrossRef]
- Singh, S.; Andersen, N.N.; Andersson, M.; Loftus, E.V.; Jess, T. Comparison of Infliximab and Adalimumab in Biologic-Naive Patients With Ulcerative Colitis: A Nationwide Danish Cohort Study. Clin. Gastroenterol. Hepatol. 2017, 15, 1218–1225.e7. [Google Scholar] [CrossRef] [PubMed]
- Renna, S.; Mocciaro, F.; Ventimiglia, M.; Orlando, R.; Macaluso, F.S.; Cappello, M.; Fries, W.; Mendolaro, M.; Privitera, A.C.; Ferracane, C.; et al. A real life comparison of the effectiveness of adalimumab and golimumab in moderate-to-severe ulcerative colitis, supported by propensity score analysis. Dig. Liver Dis. 2018, 50, 1292–1298. [Google Scholar] [CrossRef]
- Bohm, M.; Xu, R.; Zhang, Y.; Varma, S.; Fischer, M.; Kochhar, G.; Boland, B.; Singh, S.; Hirten, R.; Ungaro, R.; et al. Comparative safety and effectiveness of vedolizumab to tumour necrosis factor antagonist therapy for Crohn’s disease. Aliment. Pharmacol. Ther. 2020, 52, 669–681. [Google Scholar] [CrossRef]
- Lukin, D.; Faleck, D.; Xu, R.; Zhang, Y.; Weiss, A.; Aniwan, S.; Kadire, S.; Tran, G.; Rahal, M.; Winters, A.; et al. Comparative Safety and Effectiveness of Vedolizumab to Tumor Necrosis Factor Antagonist Therapy for Ulcerative Colitis. Clin. Gastroenterol. Hepatol. 2020, 20, 126–135. [Google Scholar] [CrossRef]
- Alric, H.; Amiot, A.; Kirchgesner, J.; Tréton, X.; Allez, M.; Bouhnik, Y.; Beaugerie, L.; Carbonnel, F.; Meyer, A. The effectiveness of either ustekinumab or vedolizumab in 239 patients with Crohn’s disease refractory to anti-tumour necrosis factor. Aliment. Pharmacol. Ther. 2020, 51, 948–957. [Google Scholar] [CrossRef]
- Townsend, T.; Razanskaite, V.; Dodd, S.; Storey, D.; Michail, S.; Morgan, J.; Davies, M.; Penman, D.; Watters, C.; Swaminathan, M.; et al. Comparative effectiveness of ustekinumab or vedolizumab after one year in 130 patients with anti-TNF-refractory Crohn’s disease. Aliment. Pharmacol. Ther. 2020, 52, 1341–1352. [Google Scholar] [CrossRef]
- Biemans, V.B.C.; van der Woude, C.J.; Dijkstra, G.; van der Meulen-de Jong, A.E.; Löwenberg, M.; de Boer, N.K.; Oldenburg, B.; Srivastava, N.; Jansen, J.M.; Bodelier, A.G.L.; et al. Ustekinumab is associated with superior effectiveness outcomes compared to vedolizumab in Crohn’s disease patients with prior failure to anti-TNF treatment. Aliment. Pharmacol. Ther. 2020, 52, 123–134. [Google Scholar] [CrossRef]
- Onali, S.; Pugliese, D.; Caprioli, F.; Orlando, A.; Biancone, L.; Nardone, O.; Imperatore, N.; Fiorino, G.; Cappello, M.; Viola, A.; et al. Objective comparison of vedolizumab and ustekinumab effectiveness in Crohn’s disease patients failure to TNF-alpha inhibitors. Am. J. Gastroenterol. 2022, 117, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Lenti, M.V.; Dolby, V.; Clark, T.; Hall, V.; Tattersall, S.; Fairhurst, F.; Kenneth, C.; Walker, R.; Kemp, K.; Borg-Bartolo, S.; et al. A propensity score-matched, real-world comparison of ustekinumab vs vedolizumab as a second-line treatment for Crohn’s disease. The Cross Pennine study II. Aliment. Pharmacol. Ther. 2022, 55, 856–866. [Google Scholar] [CrossRef] [PubMed]
- Manlay, L.; Boschetti, G.; Pereira, B.; Flourié, B.; Dapoigny, M.; Reymond, M.; Sollelis, E.; Gay, C.; Boube, M.; Buisson, A.; et al. Comparison of short- and long-term effectiveness between ustekinumab and vedolizumab in patients with Crohn’s disease refractory to anti-tumour necrosis factor therapy. Aliment. Pharmacol. Ther. 2021, 53, 1289–1299. [Google Scholar] [CrossRef] [PubMed]
- Bonovas, S.; Nikolopoulos, G.K.; Lytras, T.; Fiorino, G.; Peyrin-Biroulet, L.; Danese, S. Comparative safety of systemic and low-bioavailability steroids in inflammatory bowel disease: Systematic review and network meta-analysis. Br. J. Clin. Pharmacol. 2018, 84, 239–251. [Google Scholar] [CrossRef]
- Rui, M.; Fei, Z.; Wang, Y.; Shi, F.; Meng, R.; Shang, Y.; Ma, A.; Li, H. Will the Inducing and Maintaining Remission of Non-biological Agents and Biological Agents Differ for Crohn’s Disease? The Evidence From the Network Meta-Analysis. Front. Med. 2021, 8, 679258. [Google Scholar] [CrossRef] [PubMed]
- Vuyyuru, S.K.; Kedia, S.; Kalaivani, M.; Sahu, P.; Kante, B.; Kumar, P.; Ranjan, M.K.; Makharia, G.; Ananthakrishnan, A.; Ahuja, V. Efficacy and safety of fecal transplantation versus targeted therapies in ulcerative colitis: Network meta-analysis. Future Microbiol. 2021, 16, 1215–1227. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.Y.; Guo, B.; Lufumpa, E.; Li, X.M.; Chen, L.H.; Meng, X.; Li, B.Z. Comparative of the Effectiveness and Safety of Biological Agents, Tofacitinib, and Fecal Microbiota Transplantation in Ulcerative Colitis: Systematic Review and Network Meta-Analysis. Immunol. Investig. 2021, 50, 323–337. [Google Scholar] [CrossRef] [PubMed]
| Induction of clinical remission—naïve patients |
Pairwise meta-analysis:
|
| Induction of clinical remission—exposed patients |
Pairwise meta-analysis:
|
| Maintenance of clinical remission—combined naïve and exposed patients |
Pairwise:
|
| Safety—only from maintenance trials |
|
| UC |
| Induction of clinical remission |
Pairwise meta-analysis:
|
| Maintenance of clinical remission–treat-through studies |
Pairwise meta-analysis:
|
| Maintenance of clinical remission–re-randomization studies |
Pairwise meta-analysis:
|
| Induction of endoscopic improvement |
Pairwise meta-analysis:
|
| Maintenance of endoscopic improvement–treat-through studies |
Pairwise meta-analysis:
|
| Maintenance of endoscopic improvement–re-randomization studies |
Pairwise meta-analysis:
|
| Induction of clinical response–naïve patients |
Pairwise meta-analysis:
|
| Induction of clinical response–exposed patients |
Pairwise meta-analysis:
|
| Induction of endoscopic improvement–naïve patients |
Pairwise meta-analysis:
|
| Induction of endoscopic improvement–exposed patients |
Pairwise meta-analysis:
|
| Safety |
|
| Author | Drugs | Disease/pts | Study Design | Primary End-Point | Main Finding |
|---|---|---|---|---|---|
| Placebo-controlled trial with a non-powered reference arm | |||||
| Kamm et al. [28] | MMX mesalazine vs. 5-ASA vs. placebo | 343 UC pts | Phase 3 double-blind, double dummy parallel group, randomized, placebo-controlled trial | Remission rate (defined as a reduction of UC Activity index (DAI) <1 and at least 1 point of reduction in sigmoidoscopy score from the baseline | MMX mesalamine was efficacious and well-tolerated for the induction of clinical and endoscopic remission. |
| Sandborn et al. (CORE I) [29] | MMX budesonide 6 mg/die vs. 9 mg/die vs. 5-ASA vs. PL | 509 UC pts | Phase 3, multicenter, randomized, double-blind, double-dummy, placebo-controlled trial | Remission rate (defined as a reduction of UC Activity index (DAI) <1 and at least 1 point of reduction in sigmoidoscopy score from the baseline | Budesonide MMX (9 mg) was safe and more effective than pl in inducing remission. |
| Non-inferiority trials | |||||
| Williams et al. (CONSTRUCT) [30] | Ciclosporin vs. infliximab | Acute severe ulcerative colitis refractory to IV CS | Single-blind | Quality- adjusted survival | No difference between ciclosporin and infliximab |
| Jørgensen et al. (Nor-switch) [31] | Infliximab originator vs. infliximab biosimilar (CT-P13) | 482 pts including CD-UC or other IMID, at least 6 months stable infliximab treatment | Double-blind, randomized trials | Disease worsening | Switching from originator to biosimilar infliximab non- inferior to continuation of infliximab originator |
| Superiority trials | |||||
| Sands et al. (VARSITY) [23] | Vedolizumab IV vs. adalimumab SC | 769 Moderate- to severe Active UC | Phase 3b, double-blind, double-dummy, randomized, active-controlled study | Achieving clinical remission | Vedolizumab superior to adalimumab |
| Sands et al. (SEAVUE) [16] | Adalimumab. vs. Ustekinumab | moderate-to-severely active CD | Phase 3b randomised, double-blind, parallel group, active-comparator | for clinical remission at week 5 | Ustekinumab not superior to adalimumab at week 52 |
| Danese S. (GARDENIA) [24] | Etrolizumab vs. infliximab | moderate-to-severely active UC patients naïve to TNF alpha inhibitor | Phase 3 randomised, double-blind, double-dummy, parallel-group, | Clinical response and Clinical remission | Primary end-point not reached |
| Sands et al. (VEGA) [32] | Golimumab + guselkumab vs. golimumab or guselkumab, | Moderately to Severely Active UC | Phase 2a Randomized, Double-Blind, Active-Controlled, Parallel- Group, Multicenter, Proof-of-Concept Study | Clinical responce | Combination significantly superior to golimumab monotherapy |
| Study Name or Number | Drugs | Disease | Phase | Design |
|---|---|---|---|---|
| INTREPID (NCT03759288) | Brazikumab vs. placebo and vs. adalimumab | Moderately to severely active CD | Phase 2 Phase 3 | Multicenter, randomized, double-blind, placebo- and active-controlled |
| VIVID-1 (LY3074828) | Mirikizumab vs. ustekinumab | Moderately to severely active CD | Phase 3 | Multicenter, randomized, double-blind, active-controlled |
| GALAXY (2–3) | Guselkumab vs. placebo and vs. ustekinumab | Moderately to severely active CD | Phase 2/3 | Multicenter, randomized, double-blind, placebo- and active-controlled |
| TRIDENT (NCT04524611) | JnJ-64304500 vs. placebo and vs. ustekinumab | Moderately to severely active CD | Phase 2b | Multicenter, randomized, double-blind, placebo-controlled, parallel group |
| SEQUENCE (NCT04524611) | Risankizumab vs. ustekinumab | Moderately to severely active CD who have failed anti-TNFα therapy | Phase 3 | Multicenter, randomized, efficacy assessor-blinded |
| NCT03558152 | UTTR1147A vs. placebo and vs. vedolizumab | Moderately to severely active UC | Phase 2 | Multicenter, randomized, parallel-group, double-blind, double-dummy, placebo-controlled |
| Author | Disease Drugs | Patients Followed | Main Outcomes | Results |
|---|---|---|---|---|
| Singh et al. [44] | CD ADA vs. IFX | 2908 naïve pts |
|
|
| Macaluso et al. [45] | CD ADA vs. IFX | 632 ptsNaïve ptsExperienced pts | Clinical benefit a at week 12 and 1 year |
|
| Singh et al. [46] | UC ADA vs. IFX | 1719 naïve pts |
|
|
| Renna et al. [47] | UC ADA vs. GOL | 118 pts (both naïve and experienced) |
|
|
| Bohm et al. [48] | CD VDZ vs. Anti-TNF-α | 1266 (both naïve and experienced) |
|
|
| Lukin et al. [49] | UC VDZ vs. Anti-TNF-α | 722 pts (both naïve and experienced) |
|
|
| Alric et al. [50] | CD UST vs. VDZ | 239 pts (107 vs. 132) |
|
|
| Townsend et al. [51] | CD UST vs. VDZ | 130 pts (45 vs. 85) |
|
|
| Biemans et al. [52] | CD UST vs. VDZ | 213 pts (85 vs. 128) |
|
|
| Onali et al. [53] | CD UST vs. VDZ | 470 pts (239 vs. 231) |
|
|
| Lenti et al. [54] | CD UST vs. VDZ | 393 pts (275 vs. 118) |
|
|
| Manlay et al. [55] | CD UST vs. VDZ | 312 pts (224 vs. 88) |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pugliese, D.; Onali, S.; Privitera, G.; Armuzzi, A.; Papi, C. Comparative Effectiveness Research: A Roadmap to Sail the Seas of IBD Therapies. J. Clin. Med. 2022, 11, 6717. https://doi.org/10.3390/jcm11226717
Pugliese D, Onali S, Privitera G, Armuzzi A, Papi C. Comparative Effectiveness Research: A Roadmap to Sail the Seas of IBD Therapies. Journal of Clinical Medicine. 2022; 11(22):6717. https://doi.org/10.3390/jcm11226717
Chicago/Turabian StylePugliese, Daniela, Sara Onali, Giuseppe Privitera, Alessandro Armuzzi, and Claudio Papi. 2022. "Comparative Effectiveness Research: A Roadmap to Sail the Seas of IBD Therapies" Journal of Clinical Medicine 11, no. 22: 6717. https://doi.org/10.3390/jcm11226717
APA StylePugliese, D., Onali, S., Privitera, G., Armuzzi, A., & Papi, C. (2022). Comparative Effectiveness Research: A Roadmap to Sail the Seas of IBD Therapies. Journal of Clinical Medicine, 11(22), 6717. https://doi.org/10.3390/jcm11226717







