What Are the Factors Associated with the Structural Damage Differences in Open-Angle Glaucoma? RNFL- and GCIPL-Dominant Progression
Abstract
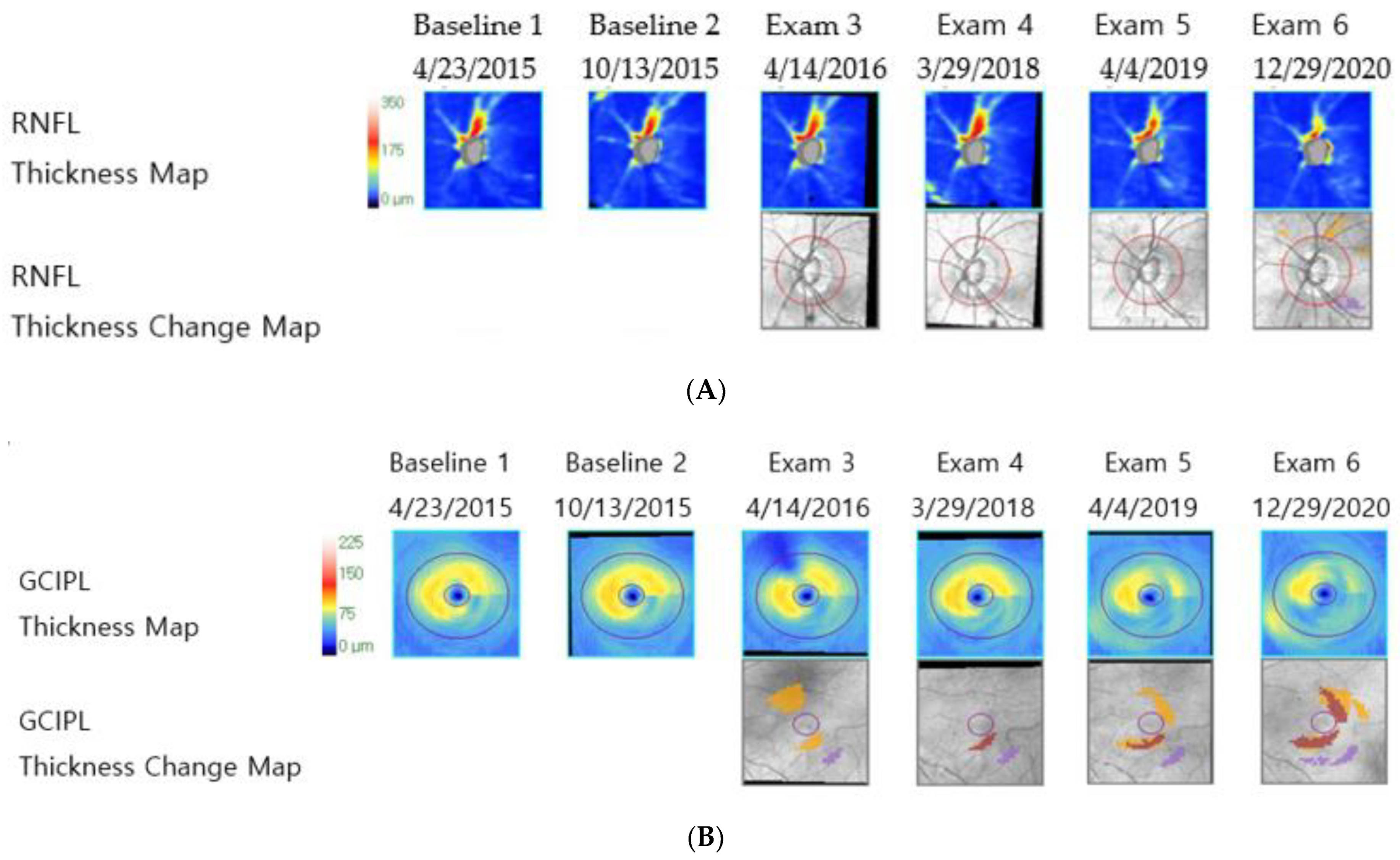
:1. Introduction
2. Materials and Methods
2.1. Patient Enrollment
2.2. Study Design
2.3. Intraocular Pressure Measurements
2.4. Enhanced Depth Imaging Optical Coherence Tomography of the Optic Disc
2.5. Definition and Measurement of the Lamina Cribrosa Curvature Index
2.6. Peripapillary Retinal Nerve Fiber Layer and Ganglion Cell–Inner Plexiform Layer Thickness
2.7. Definition of Peripapillary Choroid Microvascular Dropout and Choroidal Thickness
2.8. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Factors Associated with the Retinal Nerve Fiber Layer-Dominant Progression Group
3.3. Factors Associated with the Ganglion Cell–Inner Plexiform Layer Dominant Progression Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, J.A.; Kim, T.W.; Lee, E.J.; Kim, J.M.; Girard, M.J.A.; Mari, J.M. Intereye comparison of lamina cribrosa curvature in normal tension glaucoma patients with unilateral damage. Investig. Ophthalmol. Vis. Sci. 2019, 60, 2423–2430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bussel, I.I.; Wollstein, G.; Schuman, J.S. Oct for glaucoma diagnosis, screening and detection of glaucoma progression. Br. J. Ophthalmol. 2014, 98 (Suppl. 2), ii15–ii19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.W.; Jeoung, J.W.; Girard, M.J.; Mari, J.M.; Park, K.H. Positional and curvature difference of lamina cribrosa according to the baseline intraocular pressure in primary open-angle glaucoma: A swept-source optical coherence tomography (ss-oct) study. PLoS ONE 2016, 11, e0162182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.H.; Kim, T.W.; Lee, E.J.; Girard, M.J.; Mari, J.M. Diagnostic power of lamina cribrosa depth and curvature in glaucoma. Invest. Ophthalmol. Vis. Sci. 2017, 58, 755–762. [Google Scholar] [CrossRef] [Green Version]
- Lee, E.J.; Lee, K.M.; Lee, S.H.; Kim, T.W. Parapapillary choroidal microvasculature dropout in glaucoma: A comparison between optical coherence tomography angiography and indocyanine green angiography. Ophthalmology 2017, 124, 1209–1217. [Google Scholar] [CrossRef]
- Anctil, J.L.; Anderson, D.R. Early foveal involvement and generalized depression of the visual field in glaucoma. Arch. Ophthalmol. 1984, 102, 363–370. [Google Scholar] [CrossRef]
- Heijl, A.; Lundqvist, L. The frequency distribution of earliest glaucomatous visual field defects documented by automatic perimetry. Acta Ophthalmol. 1984, 62, 658–664. [Google Scholar] [CrossRef]
- Flammer, J.; Orgul, S.; Costa, V.P.; Orzalesi, N.; Krieglstein, G.K.; Serra, L.M.; Renard, J.P.; Stefansson, E. The impact of ocular blood flow in glaucoma. Prog. Retin. Eye Res. 2002, 21, 359–393. [Google Scholar] [CrossRef]
- Chiotoroiu, S.M.; Stefaniu, O.; Noaghi, M.; Teodorescu, A.; Taina, L. The role of systemic blood pressure in glaucoma progression. Rom. J. Ophthalmol. 2015, 59, 141–147. [Google Scholar]
- Kaiser, H.J.; Flammer, J.; Graf, T.; Stumpfig, D. Systemic blood pressure in glaucoma patients. Graefe’s Arch. Clin. Exp. Ophthalmol. 1993, 231, 677–680. [Google Scholar] [CrossRef]
- Agis Investigators. The advanced glaucoma intervention study (agis): 7. The relationship between control of intraocular pressure and visual field deterioration. Am. J. Ophthalmol. 2000, 130, 429–440. [Google Scholar] [CrossRef]
- Heijl, A.; Leske, M.C.; Bengtsson, B.; Hyman, L.; Bengtsson, B.; Hussein, M.; Early Manifest Glaucoma Trial, G. Reduction of intraocular pressure and glaucoma progression: Results from the early manifest glaucoma trial. Arch. Ophthalmol. 2002, 120, 1268–1279. [Google Scholar] [CrossRef]
- Musch, D.C.; Gillespie, B.W.; Niziol, L.M.; Lichter, P.R.; Varma, R.; Group, C.S. Intraocular pressure control and long-term visual field loss in the collaborative initial glaucoma treatment study. Ophthalmology 2011, 118, 1766–1773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellezza, A.J.; Rintalan, C.J.; Thompson, H.W.; Downs, J.C.; Hart, R.T.; Burgoyne, C.F. Deformation of the lamina cribrosa and anterior scleral canal wall in early experimental glaucoma. Investig. Ophthalmol. Vis. Sci. 2003, 44, 623–637. [Google Scholar] [CrossRef]
- Burgoyne, C.F.; Downs, J.C.; Bellezza, A.J.; Hart, R.T. Three-dimensional reconstruction of normal and early glaucoma monkey optic nerve head connective tissues. Investig. Ophthalmol. Vis. Sci. 2004, 45, 4388–4399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quigley, H.A.; Addicks, E.M.; Green, W.R.; Maumenee, A.E. Optic nerve damage in human glaucoma: II. The site of injury and susceptibility to damage. Arch. Ophthalmol. 1981, 99, 635–649. [Google Scholar] [CrossRef] [PubMed]
- Howell, G.R.; Libby, R.T.; Jakobs, T.C.; Smith, R.S.; Phalan, F.C.; Barter, J.W.; Barbay, J.M.; Marchant, J.K.; Mahesh, N.; Porciatti, V.; et al. Axons of retinal ganglion cells are insulted in the optic nerve early in dba/2j glaucoma. J. Cell Biol. 2007, 179, 1523–1537. [Google Scholar] [CrossRef] [Green Version]
- Lockwood, H.; Reynaud, J.; Gardiner, S.; Grimm, J.; Libertiaux, V.; Downs, J.C.; Yang, H.; Burgoyne, C.F. Lamina cribrosa microarchitecture in normal monkey eyes part 1: Methods and initial results. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1618–1637. [Google Scholar] [CrossRef] [Green Version]
- Yan, D.B.; Coloma, F.M.; Metheetrairut, A.; Trope, G.E.; Heathcote, J.G.; Ethier, C.R. Deformation of the lamina cribrosa by elevated intraocular pressure. Br. J. Ophthalmol. 1994, 78, 643–648. [Google Scholar] [CrossRef] [Green Version]
- Anderson, D.R.; Hendrickson, A. Effect of intraocular pressure on rapid axoplasmic transport in monkey optic nerve. Investig. Ophthalmol. 1974, 13, 771–783. [Google Scholar]
- Minckler, D.S.; Bunt, A.H.; Johanson, G.W. Orthograde and retrograde axoplasmic transport during acute ocular hypertension in the monkey. Investig. Ophthalmol. Vis. Sci. 1977, 16, 426–441. [Google Scholar]
- Hernandez, M.R. The optic nerve head in glaucoma: Role of astrocytes in tissue remodeling. Prog. Retin. Eye Res. 2000, 19, 297–321. [Google Scholar] [CrossRef]
- Kim, J.A.; Kim, T.W.; Lee, E.J.; Girard, M.J.A.; Mari, J.M. Comparison of lamina cribrosa morphology in eyes with ocular hypertension and normal-tension glaucoma. Investig. Ophthalmol. Vis. Sci. 2020, 61, 4. [Google Scholar] [CrossRef] [PubMed]


| RNFL-Dominant Progression Group (22 Eyes, 12 Patients) | GCIPL-Dominant Progression Group (36 Eyes, 21 Patients) | p-Value | |
|---|---|---|---|
| Age [years] | 54.95 ± 15.63 | 62.97 ± 13.58 | 0.044 |
| Female gender (%) | 6 (50) | 10 (47.62) | 0.896 |
| Hypertension [patients] | 3 | 13 | 0.063 |
| Diabetes mellitus [patients] | 0 | 8 | 0.019 |
| Diagnosis [eyes] | 0.005 | ||
| POAG | 20 (90.91) | 20 (55.56) | |
| NTG | 2 (9.09) | 16 (44.44) | |
| Pre-treatment IOP [mmHg] | 19.31 ± 4.45 | 15.69 ± 3.47 | 0.004 |
| Mean IOP [mmHg] | 14.81 ± 1.30 | 13.46 ± 2.13 | 0.006 |
| Axial length [mm] | 25.35 ± 2.21 | 24.90 ± 1.81 | 0.486 |
| Visual field MD [dB] | −6.71 ± 6.27 | −5.83 ± 5.17 | 0.566 |
| Glaucoma severity [eyes] | 0.350 | ||
| Early | 12 (54.56) | 20 (55.56) | |
| Moderate | 4 (18.18) | 11 (30.56) | |
| Severe | 6 (27.27) | 5 (13.89) | |
| Presence of pcMvD [eyes] | 1 (16.67) | 9 (64.29) | 0.141 |
| Choroidal thickness [µm] | 233.64 ± 78.86 | 217.92 ± 100.27 | 0.534 |
| LCCI | 27.54 ± 8.06 | 22.11 ± 9.62 | 0.031 |
| Mean SBP | 118.8 ± 14.8 | 123.7 ± 11 | 0.151 |
| Mean DBP | 71.6 ± 11.8 | 72.3 ± 7.3 | 0.806 |
| Presence of disc hemorrhage [eyes] | 3 | 10 | 0.332 |
| Univariate | Multivariate Analysis 1 | Multivariate Analysis 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Axial length | 1.126 | 0.657–1.580 | 0.4427 | ||||||
| Age, per 1 year older | 0.962 | 0.925–1 | 0.0493 | 0.977 | 0.929–1.028 | 0.3738 | 0.99 | 0.943–1.04 | 0.6992 |
| LCCI | 1.070 | 1.004–1.140 | 0.0368 | 1.043 | 0.953–1.141 | 0.3645 | 1.094 | 1.007–1.188 | 0.0345 |
| Pre-treatment IOP | 1.292 | 1.057–1.580 | 0.0124 | 1.325 | 1.058–1.661 | 0.0143 | |||
| Mean IOP | 1.522 | 1.066–2.053 | 0.019 | 1.655 | 1.139–2.405 | 0.0083 | |||
| Choroidal thickness | 1.002 | 0.996–1.008 | 0.5272 | ||||||
| Visual field test MD | 0.972 | 0.883–1.070 | 0.5591 | ||||||
| Mean SBP | 0.967 | 0.923–1.013 | 0.155 | ||||||
| Mean DBP | 0.992 | 0.935–1.052 | 0.7784 | ||||||
| Hypertension | 0.279 | 0.069–1.127 | 0.0731 | ||||||
| Diabetes mellitus | 0.074 | 0.003–1.616 | 0.098 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.E.; Lee, J.S.; Kim, M.; Kim, C.Y.; Bae, H.W. What Are the Factors Associated with the Structural Damage Differences in Open-Angle Glaucoma? RNFL- and GCIPL-Dominant Progression. J. Clin. Med. 2022, 11, 6728. https://doi.org/10.3390/jcm11226728
Park SE, Lee JS, Kim M, Kim CY, Bae HW. What Are the Factors Associated with the Structural Damage Differences in Open-Angle Glaucoma? RNFL- and GCIPL-Dominant Progression. Journal of Clinical Medicine. 2022; 11(22):6728. https://doi.org/10.3390/jcm11226728
Chicago/Turabian StylePark, Sung Eun, Jihei Sara Lee, Mijung Kim, Chan Yun Kim, and Hyoung Won Bae. 2022. "What Are the Factors Associated with the Structural Damage Differences in Open-Angle Glaucoma? RNFL- and GCIPL-Dominant Progression" Journal of Clinical Medicine 11, no. 22: 6728. https://doi.org/10.3390/jcm11226728





