Contemporary Management of Postoperative Crohn’s Disease after Ileocolonic Resection
Abstract
:1. Introduction
2. Diagnosing Recurrence in Postoperative Crohn’s Disease
2.1. Endoscopy
2.1.1. (Modified) Rutgeerts Score
2.1.2. REMIND Score
2.1.3. POCER Index
2.2. Fecal and Serum Biomarkers
2.2.1. Fecal Biomarkers
2.2.2. Serum Biomarkers
2.3. Cross-Sectional Imaging
2.3.1. Intestinal Ultrasound
2.3.2. Magnetic Resonance and Computed Tomography Enterography
2.4. Novel and Emerging Biomarkers
3. Treatment of Postoperative Crohn’s Disease
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Torres, J.; Mehandru, S.; Colombel, J.F.; Peyrin-Biroulet, L. Crohn’s disease. Lancet 2017, 389, 1741–1755. [Google Scholar] [CrossRef]
- Tsai, L.; Ma, C.; Dulai, P.S.; Prokop, L.J.; Eisenstein, S.; Ramamoorthy, S.L.; Feagan, B.G.; Jairath, V.; Sandborn, W.J.; Singh, S. Contemporary Risk of Surgery in Patients With Ulcerative Colitis and Crohn’s Disease: A Meta-Analysis of Population-Based Cohorts. Clin. Gastroenterol. Hepatol. 2020, 19, 2031–2204. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Moran, G.W.; Benchimol, E.I.; Targownik, L.E.; Heitman, S.J.; Hubbard, J.N.; Seow, C.H.; Novak, K.L.; Ghosh, S.; Panaccione, R.; et al. Surgical Rates for Crohn’s Disease are Decreasing: A Population-Based Time Trend Analysis and Validation Study. Am. J. Gastroenterol. 2017, 112, 1840–1848. [Google Scholar] [CrossRef] [Green Version]
- Frolkis, A.D.; Dykeman, J.; Negron, M.E.; Debruyn, J.; Jette, N.; Fiest, K.M.; Frolkis, T.; Barkema, H.W.; Rioux, K.P.; Panaccione, R.; et al. Risk of surgery for inflammatory bowel diseases has decreased over time: A systematic review and meta-analysis of population-based studies. Gastroenterology 2013, 145, 996–1006. [Google Scholar] [CrossRef]
- Frolkis, A.D.; Lipton, D.S.; Fiest, K.M.; Negron, M.E.; Dykeman, J.; deBruyn, J.; Jette, N.; Frolkis, T.; Rezaie, A.; Seow, C.H.; et al. Cumulative incidence of second intestinal resection in Crohn’s disease: A systematic review and meta-analysis of population-based studies. Am. J. Gastroenterol. 2014, 109, 1739–1748. [Google Scholar] [CrossRef] [PubMed]
- Gionchetti, P.; Dignass, A.; Danese, S.; Magro Dias, F.J.; Rogler, G.; Lakatos, P.L.; Adamina, M.; Ardizzone, S.; Buskens, C.J.; Sebastian, S.; et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 2: Surgical Management and Special Situations. J. Crohn’s Colitis 2017, 11, 135–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, G.C.; Loftus, E.V., Jr.; Hirano, I.; Falck-Ytter, Y.; Singh, S.; Sultan, S. American Gastroenterological Association Institute Guideline on the Management of Crohn’s Disease After Surgical Resection. Gastroenterology 2017, 152, 271–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lamb, C.A.; Kennedy, N.A.; Raine, T.; Hendy, P.A.; Smith, P.J.; Limdi, J.K.; Hayee, B.; Lomer, M.C.E.; Parkes, G.C.; Selinger, C.; et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019, 68, s1–s106. [Google Scholar] [CrossRef] [Green Version]
- De Cruz, P.; Kamm, M.A.; Hamilton, A.L.; Ritchie, K.J.; Krejany, E.O.; Gorelik, A.; Liew, D.; Prideaux, L.; Lawrance, I.C.; Andrews, J.M.; et al. Crohn’s disease management after intestinal resection: A randomised trial. Lancet 2015, 385, 1406–1417. [Google Scholar] [CrossRef]
- Rutgeerts, P.; Geboes, K.; Vantrappen, G.; Beyls, J.; Kerremans, R.; Hiele, M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology 1990, 99, 956–963. [Google Scholar] [CrossRef]
- Burr, N.E.; Hall, B.; Hamlin, P.J.; Selinger, C.P.; Ford, A.C.; O’Connor, A. Systematic Review and Network Meta-Analysis of Medical Therapies to Prevent Recurrence of Post-Operative Crohn’s Disease. J. Crohn’s Colitis 2019, 13, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Regueiro, M.; Feagan, B.G.; Zou, B.; Johanns, J.; Blank, M.A.; Chevrier, M.; Plevy, S.; Popp, J.; Cornillie, F.J.; Lukas, M.; et al. Infliximab Reduces Endoscopic, but Not Clinical, Recurrence of Crohn’s Disease After Ileocolonic Resection. Gastroenterology 2016, 150, 1568–1578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, C.; Gecse, K.B.; Duijvestein, M.; Sandborn, W.J.; Zou, G.; Shackelton, L.M.; Stitt, L.W.; Parker, C.E.; Bossuyt, P.; Lowenberg, M.; et al. Reliability of Endoscopic Evaluation of Postoperative Recurrent Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2020, 18, 2139–2141. [Google Scholar] [CrossRef] [PubMed]
- Domenech, E.; Manosa, M.; Bernal, I.; Garcia-Planella, E.; Cabre, E.; Pinol, M.; Lorenzo-Zuniga, V.; Boix, J.; Gassull, M.A. Impact of azathioprine on the prevention of postoperative Crohn’s disease recurrence: Results of a prospective, observational, long-term follow-up study. Inflamm. Bowel Dis. 2008, 14, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Hirten, R.P.; Mashiana, S.; Cohen, B.L.; Sands, B.E.; Colombel, J.F.; Harpaz, N. Ileocolic anastomotic inflammation after resection for Crohn’s disease indicates disease recurrence: A histopathologic study. Scand. J. Gastroenterol. 2020, 55, 795–799. [Google Scholar] [CrossRef]
- Ollech, J.E.; Aharoni-Golan, M.; Weisshof, R.; Normatov, I.; Sapp, A.R.; Kalakonda, A.; Israel, A.; Glick, L.R.; Karrison, T.; Dalal, S.R.; et al. Differential risk of disease progression between isolated anastomotic ulcers and mild ileal recurrence after ileocolonic resection in patients with Crohn’s disease. Gastrointest. Endosc. 2019, 90, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Riviere, P.; Vermeire, S.; Irles-Depe, M.; Van Assche, G.; Rutgeerts, P.; de Buck van Overstraeten, A.; Denost, Q.; Wolthuis, A.; D’Hoore, A.; Laharie, D.; et al. No Change in Determining Crohn’s Disease Recurrence or Need for Endoscopic or Surgical Intervention With Modification of the Rutgeerts’ Scoring System. Clin. Gastroenterol. Hepatol. 2019, 17, 1643–1645. [Google Scholar] [CrossRef]
- Hammoudi, N.; Auzolle, C.; Tran Minh, M.L.; Boschetti, G.; Bezault, M.; Buisson, A.; Pariente, B.; Treton, X.; Seksik, P.; Fumery, M.; et al. Postoperative Endoscopic Recurrence on the Neoterminal Ileum But Not on the Anastomosis Is Mainly Driving Long-Term Outcomes in Crohn’s Disease. Am. J. Gastroenterol. 2020, 115, 1084–1093. [Google Scholar] [CrossRef]
- Hirten, R.P.; Ungaro, R.C.; Castaneda, D.; Lopatin, S.; Sands, B.E.; Colombel, J.F.; Cohen, B.L. Anastomotic Ulcers After Ileocolic Resection for Crohn’s Disease Are Common and Predict Recurrence. Inflamm. Bowel Dis. 2020, 26, 1050–1058. [Google Scholar] [CrossRef]
- Bachour, S.P.; Shah, R.S.; Lyu, R.; Rieder, F.; Qazi, T.; Lashner, B.; Achkar, J.P.; Philpott, J.; Barnes, E.L.; Axelrad, J.; et al. Mild neoterminal ileal post-operative recurrence of Crohn’s disease conveys higher risk for severe endoscopic disease progression than isolated anastomotic lesions. Aliment. Pharmacol. Ther. 2022, 55, 1139–1150. [Google Scholar] [CrossRef]
- Riviere, P.; Pekow, J.; Hammoudi, N.; Wils, P.; De Cruz, P.; Wang, C.P.; Manosa, M.; Ollech, J.; Allez, M.; Nachury, M.; et al. Comparison of the risk of Crohn’s disease postoperative recurrence between modified Rutgeerts score i2a and i2b categories: An individual patient data meta-analysis. J. Crohn’s Colitis 2022, jjac137. [Google Scholar] [CrossRef] [PubMed]
- Hanzel, J. A Novel Endoscopic Score for Postoperative Recurrence of Crohn’s Disease: More Information Needed. Am. J. Gastroenterol. 2020, 116, 217–218. [Google Scholar] [CrossRef] [PubMed]
- De Cruz, P.; Hamilton, A.L.; Burrell, K.J.; Gorelik, A.; Liew, D.; Kamm, M.A. Endoscopic Prediction of Crohn’s Disease Postoperative Recurrence. Inflamm. Bowel Dis. 2021, 28, 680–688. [Google Scholar] [CrossRef] [PubMed]
- Khanna, R.; Zou, G.; D’Haens, G.; Rutgeerts, P.; McDonald, J.W.; Daperno, M.; Feagan, B.G.; Sandborn, W.J.; Dubcenco, E.; Stitt, L.; et al. Reliability among central readers in the evaluation of endoscopic findings from patients with Crohn’s disease. Gut 2016, 65, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Buisson, A.; Gonzalez, F.; Poullenot, F.; Nancey, S.; Sollellis, E.; Fumery, M.; Pariente, B.; Flamant, M.; Trang-Poisson, C.; Bonnaud, G.; et al. Comparative Acceptability and Perceived Clinical Utility of Monitoring Tools: A Nationwide Survey of Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 1425–1433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Amico, F.; Rubin, D.T.; Kotze, P.G.; Magro, F.; Siegmund, B.; Kobayashi, T.; Olivera, P.A.; Bossuyt, P.; Pouillon, L.; Louis, E.; et al. International consensus on methodological issues in standardization of fecal calprotectin measurement in inflammatory bowel diseases. United Eur. Gastroenterol. J. 2021, 9, 451–460. [Google Scholar] [CrossRef] [PubMed]
- D’Haens, G.R.; Geboes, K.; Peeters, M.; Baert, F.; Penninckx, F.; Rutgeerts, P. Early lesions of recurrent Crohn’s disease caused by infusion of intestinal contents in excluded ileum. Gastroenterology 1998, 114, 262–267. [Google Scholar] [CrossRef]
- Qiu, Y.; Mao, R.; Chen, B.L.; He, Y.; Zeng, Z.R.; Xue, L.; Song, X.M.; Li, Z.P.; Chen, M.H. Fecal calprotectin for evaluating postoperative recurrence of Crohn’s disease: A meta-analysis of prospective studies. Inflamm. Bowel Dis. 2015, 21, 315–322. [Google Scholar] [CrossRef]
- Tham, Y.S.; Yung, D.E.; Fay, S.; Yamamoto, T.; Ben-Horin, S.; Eliakim, R.; Koulaouzidis, A.; Kopylov, U. Fecal calprotectin for detection of postoperative endoscopic recurrence in Crohn’s disease: Systematic review and meta-analysis. Ther. Adv. Gastroenterol. 2018, 11, 175628481878557. [Google Scholar] [CrossRef] [Green Version]
- Boschetti, G.; Laidet, M.; Moussata, D.; Stefanescu, C.; Roblin, X.; Phelip, G.; Cotte, E.; Passot, G.; Francois, Y.; Drai, J.; et al. Levels of Fecal Calprotectin Are Associated With the Severity of Postoperative Endoscopic Recurrence in Asymptomatic Patients With Crohn’s Disease. Am. J. Gastroenterol. 2015, 110, 865–872. [Google Scholar] [CrossRef]
- Lopes, S.; Andrade, P.; Afonso, J.; Rodrigues-Pinto, E.; Dias, C.C.; Macedo, G.; Magro, F. Correlation Between Calprotectin and Modified Rutgeerts Score. Inflamm. Bowel Dis. 2016, 22, 2173–2181. [Google Scholar] [CrossRef]
- Boube, M.; Laharie, D.; Nancey, S.; Hebuterne, X.; Fumery, M.; Pariente, B.; Roblin, X.; Peyrin-Biroulet, L.; Minet-Quinard, R.; Pereira, B.; et al. Variation of faecal calprotectin level within the first three months after bowel resection is predictive of endoscopic postoperative recurrence in Crohn’s disease. Dig. Liver Dis. 2020, 52, 740–744. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Shimoyama, T.; Umegae, S.; Matsumoto, K. Serial monitoring of faecal calprotectin for the assessment of endoscopic recurrence in asymptomatic patients after ileocolonic resection for Crohn’s disease: A long-term prospective study. Ther. Adv. Gastroenterol. 2016, 9, 664–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Haens, G.; Kelly, O.; Battat, R.; Silverberg, M.S.; Laharie, D.; Louis, E.; Savarino, E.; Bodini, G.; Yarur, A.; Boland, B.S.; et al. Development and Validation of a Test to Monitor Endoscopic Activity in Patients with Crohn’s Disease Based on Serum Levels of Proteins. Gastroenterology 2020, 158, 515–526.e10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamilton, A.L.; De Cruz, P.; Wright, E.K.; Dervieux, T.; Jain, A.; Kamm, M.A. Non-Invasive Serological Monitoring for Crohn’s Disease Post-Operative Recurrence. J. Crohn’s Colitis 2022, jjac076. [Google Scholar] [CrossRef] [PubMed]
- Wright, E.K.; Kamm, M.A.; De Cruz, P.; Hamilton, A.L.; Ritchie, K.J.; Krejany, E.O.; Leach, S.; Gorelik, A.; Liew, D.; Prideaux, L.; et al. Measurement of fecal calprotectin improves monitoring and detection of recurrence of Crohn’s disease after surgery. Gastroenterology 2015, 148, 938–947.e1. [Google Scholar] [CrossRef] [Green Version]
- Cerrillo, E.; Moret, I.; Iborra, M.; Pamies, J.; Hervás, D.; Tortosa, L.; Sáez-González, E.; Nos, P.; Beltrán, B. A Nomogram Combining Fecal Calprotectin Levels and Plasma Cytokine Profiles for Individual Prediction of Postoperative Crohn’s Disease Recurrence. Inflamm. Bowel Dis. 2019, 25, 1681–1691. [Google Scholar] [CrossRef]
- DiCandio, G.; Mosca, F.; Campatelli, A.; Bianchini, M.; D’Elia, F.; Dellagiovampaola, C. Sonographic detection of postsurgical recurrence of Crohn disease. AJR Am. J. Roentgenol. 1986, 146, 523–526. [Google Scholar] [CrossRef]
- Rispo, A.; Imperatore, N.; Testa, A.; Nardone, O.M.; Luglio, G.; Caporaso, N.; Castiglione, F. Diagnostic Accuracy of Ultrasonography in the Detection of Postsurgical Recurrence in Crohn’s Disease: A Systematic Review with Meta-analysis. Inflamm. Bowel Dis. 2018, 24, 977–988. [Google Scholar] [CrossRef]
- Sturm, A.; Maaser, C.; Calabrese, E.; Annese, V.; Fiorino, G.; Kucharzik, T.; Vavricka, S.R.; Verstockt, B.; van Rheenen, P.; Tolan, D.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 2: IBD scores and general principles and technical aspects. J. Crohn’s Colitis 2019, 13, 273–284. [Google Scholar] [CrossRef]
- Paredes, J.M.; Ripollés, T.; Cortés, X.; Moreno, N.; Martínez, M.J.; Bustamante-Balén, M.; Delgado, F.; Moreno-Osset, E. Contrast-enhanced ultrasonography: Usefulness in the assessment of postoperative recurrence of Crohn’s disease. J. Crohn’s Colitis 2013, 7, 192–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martínez, M.J.; Ripollés, T.; Paredes, J.M.; Moreno-Osset, E.; Pazos, J.M.; Blanc, E. Intravenous Contrast-Enhanced Ultrasound for Assessing and Grading Postoperative Recurrence of Crohn’s Disease. Dig. Dis. Sci. 2019, 64, 1640–1650. [Google Scholar] [CrossRef] [PubMed]
- Soyer, P.; Boudiaf, M.; Sirol, M.; Dray, X.; Aout, M.; Duchat, F.; Vahedi, K.; Fargeaudou, Y.; Martin-Grivaud, S.; Hamzi, L.; et al. Suspected anastomotic recurrence of Crohn disease after ileocolic resection: Evaluation with CT enteroclysis. Radiology 2010, 254, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Paparo, F.; Revelli, M.; Puppo, C.; Bacigalupo, L.; Garello, I.; Garlaschi, A.; Biscaldi, E.; Rollandi, L.; Binda, G.A.; Rollandi, G.A. Crohn’s disease recurrence in patients with ileocolic anastomosis: Value of computed tomography enterography with water enema. Eur. J. Radiol. 2013, 82, e434–e440. [Google Scholar] [CrossRef] [PubMed]
- Mao, R.; Gao, X.; Zhu, Z.H.; Feng, S.T.; Chen, B.L.; He, Y.; Cui, Y.; Li, Z.P.; Hu, P.J.; Chen, M.H. CT enterography in evaluating postoperative recurrence of Crohn’s disease after ileocolic resection: Complementary role to endoscopy. Inflamm. Bowel Dis. 2013, 19, 977–982. [Google Scholar] [CrossRef]
- Choi, I.Y.; Park, S.H.; Park, S.H.; Yu, C.S.; Yoon, Y.S.; Lee, J.L.; Ye, B.D.; Kim, A.Y.; Yang, S.K. CT Enterography for Surveillance of Anastomotic Recurrence within 12 Months of Bowel Resection in Patients with Crohn’s Disease: An Observational Study Using an 8-Year Registry. Korean J. Radiol. 2017, 18, 906–914. [Google Scholar] [CrossRef] [Green Version]
- Bachour, S.P.; Shah, R.S.; Lyu, R.; Nakamura, T.; Shen, M.; Li, T.; Dane, B.; Barnes, E.L.; Rieder, F.; Cohen, B.; et al. Test Characteristics of Cross-sectional Imaging and Concordance with Endoscopy in Postoperative Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2021, 20, 2327–2336.e4. [Google Scholar] [CrossRef]
- Schaefer, M.; Laurent, V.; Grandmougin, A.; Vuitton, L.; Bourreille, A.; Luc, A.; Clerc-Urmes, I.; Orry, X.; Frampas, E.; De Billy, M.; et al. A Magnetic Resonance Imaging Index to Predict Crohn’s Disease Postoperative Recurrence: The MONITOR Index. Clin. Gastroenterol. Hepatol. 2022, 20, e1040–e1049. [Google Scholar] [CrossRef]
- Wang, M.H.; Friton, J.J.; Raffals, L.E.; Leighton, J.A.; Pasha, S.F.; Picco, M.F.; Monroe, K.; Nix, B.D.; Newberry, R.D.; Faubion, W.A. Novel Genetic Variant Predicts Surgical Recurrence Risk in Crohn’s Disease Patients. Inflamm. Bowel Dis. 2021, 27, 1968–1974. [Google Scholar] [CrossRef]
- Cushing, K.C.; McLean, R.; McDonald, K.G.; Gustafsson, J.K.; Knoop, K.A.; Kulkarni, D.H.; Sartor, R.B.; Newberry, R.D. Predicting Risk of Postoperative Disease Recurrence in Crohn’s Disease: Patients With Indolent Crohn’s Disease Have Distinct Whole Transcriptome Profiles at the Time of First Surgery. Inflamm. Bowel Dis. 2019, 25, 180–193. [Google Scholar] [CrossRef]
- Keshteli, A.H.; Tso, R.; Dieleman, L.A.; Park, H.; Kroeker, K.I.; Jovel, J.; Gillevet, P.M.; Sikaroodi, M.; Mandal, R.; Fedorak, R.N.; et al. A Distinctive Urinary Metabolomic Fingerprint Is Linked With Endoscopic Postoperative Disease Recurrence in Crohn’s Disease Patients. Inflamm. Bowel Dis. 2018, 24, 861–870. [Google Scholar] [CrossRef]
- Machiels, K.; Pozuelo Del Río, M.; Martinez-De la Torre, A.; Xie, Z.; Pascal Andreu, V.; Sabino, J.; Santiago, A.; Campos, D.; Wolthuis, A.; D’Hoore, A.; et al. Early Postoperative Endoscopic Recurrence in Crohn’s Disease Is Characterised by Distinct Microbiota Recolonisation. J. Crohn’s Colitis 2020, 14, 1535–1546. [Google Scholar] [CrossRef] [PubMed]
- Joustra, V.; Duijvestein, M.; Mookhoek, A.; Bemelman, W.; Buskens, C.; Kozelj, M.; Novak, G.; Hindryckx, P.; Mostafavi, N.; D’Haens, G. Natural History and Risk Stratification of Recurrent Crohn’s Disease After Ileocolonic Resection: A Multicenter Retrospective Cohort Study. Inflamm. Bowel Dis. 2022, 28, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Joustra, V.; van Sabben, J.; van der Does de Willebois, E.M.L.; Duijvenstein, M.; de Boer, N.K.; Jansen, J.; van der Bilt, J.D.; Lameris, W.; Bemelman, W.; Buskens, C.; et al. Benefit of risk-stratified prophylactic treatment on clinical outcome in post-operative Crohn’s disease. J. Crohn’s Colitis 2022. [Google Scholar] [CrossRef]
- Arkenbosch, J.H.C.; Beelen, E.M.J.; Dijkstra, G.; Romberg-Camps, M.; Duijvestein, M.; Hoentjen, F.; van der Marel, S.; Maljaars, P.W.J.; Jansen, S.; de Boer, N.K.H.; et al. Prophylactic medication for the prevention of endoscopic recurrence in Crohn’s disease: A prospective study based on clinical risk stratification. J. Crohn’s Colitis 2022, jjac128. [Google Scholar] [CrossRef] [PubMed]
- Hanzel, J.; Jairath, V.; De Cruz, P.; Guizzetti, L.; Shackelton, L.M.; Bossuyt, P.; Duijvestein, M.; Dulai, P.S.; Grossmann, J.; Hirten, R.P.; et al. Recommendations for Standardizing Clinical Trial Design and Endoscopic Assessment in Postoperative Crohn’s Disease. Inflamm. Bowel Dis. 2021, 28, 1321–1331. [Google Scholar] [CrossRef] [PubMed]
- Mowat, C.; Arnott, I.; Cahill, A.; Smith, M.; Ahmad, T.; Subramanian, S.; Travis, S.; Morris, J.; Hamlin, J.; Dhar, A.; et al. Mercaptopurine versus placebo to prevent recurrence of Crohn’s disease after surgical resection (TOPPIC): A multicentre, double-blind, randomised controlled trial. Lancet Gastroenterol. Hepatol. 2016, 1, 273–282. [Google Scholar] [CrossRef] [Green Version]
- Beelen, E.M.J.; Nieboer, D.; Arkenbosch, J.H.C.; Regueiro, M.D.; Satsangi, J.; Ardizzone, S.; Lopez-Sanroman, A.; Savarino, E.; Armuzzi, A.; Janneke van der Woude, C.; et al. Risk Prediction and Comparative Efficacy of Anti-TNF vs Thiopurines, for Preventing Postoperative Recurrence in Crohn’s Disease: A Pooled Analysis of 6 Trials. Clin. Gastroenterol. Hepatol. 2021. [Google Scholar] [CrossRef]
- Shinagawa, T.; Hata, K.; Ikeuchi, H.; Fukushima, K.; Futami, K.; Sugita, A.; Uchino, M.; Watanabe, K.; Higashi, D.; Kimura, H.; et al. Rate of Reoperation Decreased Significantly after Year 2002 in Patients with Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2020, 18, 898–907.e5. [Google Scholar] [CrossRef]
- Cosquer, G.L.; Altwegg, R.; Riviere, P.; Bournet, B.; Boivineau, L.; Poullenot, F.; Bozon, A.; Buscail, L.; Laharie, D.; Gilletta, C. Prevention of post-operative recurrence of Crohn’s disease among patients with prior anti-TNFalpha failure: A retrospective multicenter study. Dig. Liver Dis. 2022. [Google Scholar] [CrossRef]
- Yamada, A.; Komaki, Y.; Patel, N.; Komaki, F.; Pekow, J.; Dalal, S.; Cohen, R.D.; Cannon, L.; Umanskiy, K.; Smith, R.; et al. The Use of Vedolizumab in Preventing Postoperative Recurrence of Crohn’s Disease. Inflamm. Bowel Dis. 2018, 24, 502–509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buisson, A.; Nancey, S.; Manlay, L.; Rubin, D.T.; Hebuterne, X.; Pariente, B.; Fumery, M.; Laharie, D.; Roblin, X.; Bommelaer, G.; et al. Ustekinumab is more effective than azathioprine to prevent endoscopic postoperative recurrence in Crohn’s disease. United Eur. Gastroenterol. J. 2021, 9, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Axelrad, J.E.; Li, T.; Bachour, S.P.; Nakamura, T.I.; Shah, R.; Sachs, M.C.; Chang, S.; Hudesman, D.P.; Holubar, S.D.; Lightner, A.L.; et al. Early Initiation of Antitumor Necrosis Factor Therapy Reduces Postoperative Recurrence of Crohn’s Disease Following Ileocecal Resection. Inflamm. Bowel Dis. 2022, izac158. [Google Scholar] [CrossRef] [PubMed]
- Yanai, H.; Kagramanova, A.; Knyazev, O.; Sabino, J.; Haenen, S.; Mantzaris, G.J.; Mountaki, K.; Armuzzi, A.; Pugliese, D.; Furfaro, F.; et al. Endoscopic Postoperative Recurrence In Crohn’s Disease After Curative Ileocecal Resection With Early Prophylaxis By Anti-Tnf, Vedolizumab Or Ustekinumab: A Real-World Multicenter European Study. J. Crohn’s Colitis 2022. [Google Scholar] [CrossRef] [PubMed]
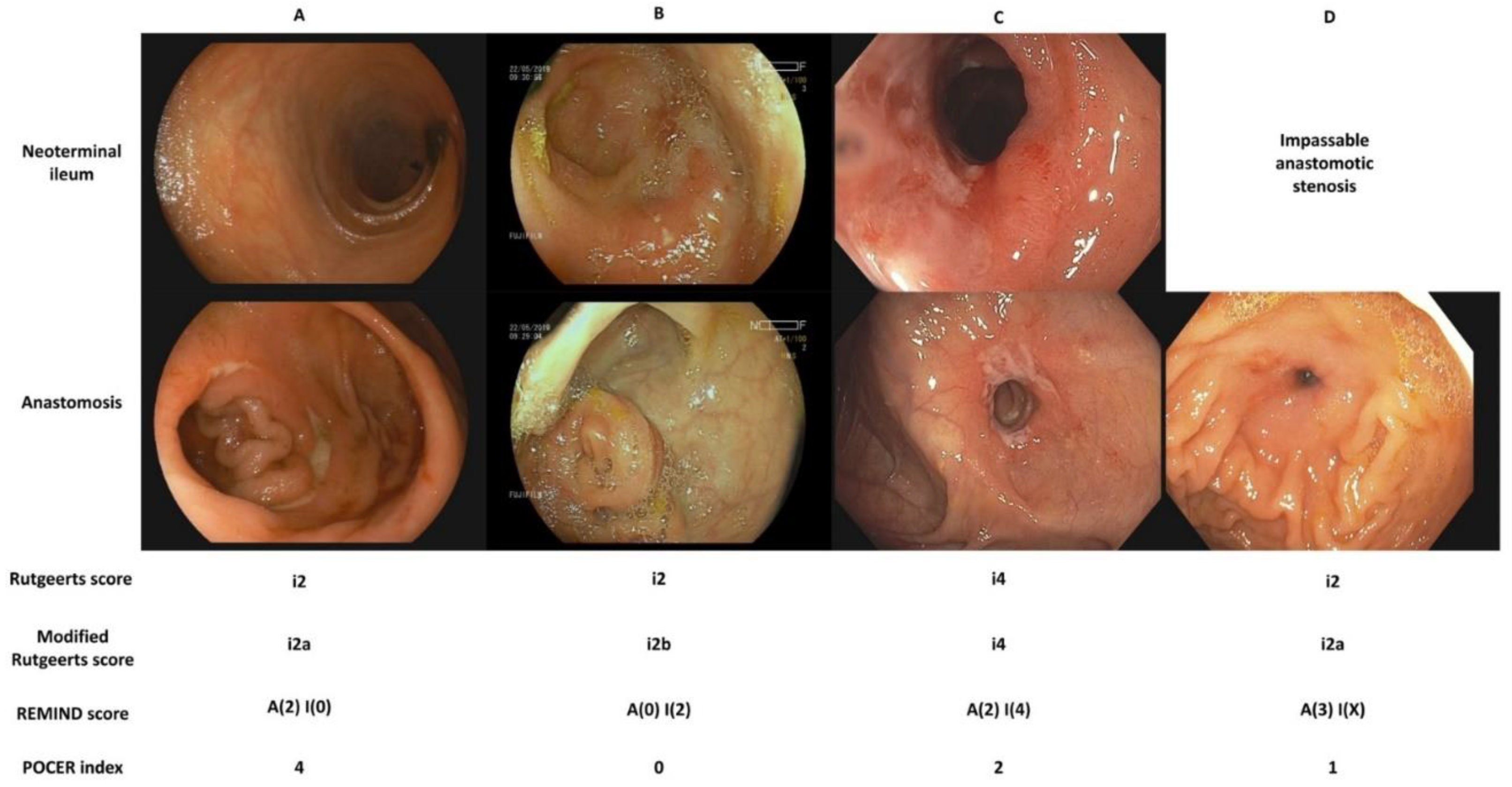

| Rutgeerts Score [10] | |
| i0 | No lesions |
| i1 | ≤5 aphthous lesions in the neoterminal ileum |
| i2 | >5 aphthous lesions with normal intervening mucosa or skip area of large lesions or lesions confined to the ileo-colonic anastomosis |
| i3 | Diffuse aphthous ileitis with diffusely inflamed mucosa |
| i4 | Large ulcers with diffuse mucosal inflammation or nodules or stenosis in the neo-terminal ileum |
| Modified Rutgeerts Score [14] | |
| i0 | No lesions |
| i1 | ≤5 aphthous lesions in the neoterminal ileum |
| i2a | Lesions confined to the ileo-colonic anastomosis (including anastomotic stenosis) |
| i2b | >5 aphthous ulcers or large lesions, with normal mucosa in-between, in the neo-terminal ileum (with or without anastomotic lesions) |
| i3 | Diffuse aphthous ileitis with diffusely inflamed mucosa |
| i4 | Large ulcers with diffuse mucosal inflammation or nodules or stenosis in the neo-terminal ileum |
| REMIND Score [15] | |
| Anastomotic lesions (<1 cm in length after the anastomosis | |
| A (0) | No lesions |
| A (1) | Ulcerations covering less than 50% of the anastomosis circumference |
| A (2) | Ulcerations covering more than 50% of the anastomosis circumference |
| A (3) | Anastomotic stenosis |
| Ileal lesions | |
| I (0) | No lesions |
| I (1) | ≤5 aphthous lesions in the neoterminal ileum |
| I (2) | >5 aphthous lesions with normal intervening mucosa or skip areas of larger lesions |
| I (3) | Diffuse aphthous ileitis with diffusely inflamed mucosa |
| I (4) | Diffuse inflammation with larger ulcers |
| POCER Index [16] | |
| 0 | No anastomotic ulcers |
| 1 | Superficial anastomotic ulcers (<2 mm in depth), <25% circumferential extent |
| 2 | Superficial anastomotic ulcers (<2 mm in depth), ≥25% circumferential extent |
| 3 | Deep anastomotic ulcer (≥1 ulcer with ≥2 mm depth), <25% circumferential extent |
| 4 | Deep anastomotic ulcer (≥1 ulcer with ≥2 mm depth), ≥25% circumferential extent |
| Endoscopic Recurrence (%) | ||
|---|---|---|
| Study | Vedolizumab | Ustekinumab |
| Yamada et al. [61] | 17/22 (75) | NA |
| Buisson et al. [62] | NA | 9/32 (28) |
| Axelrad et al. [63] 1 | 13/27 (48) | 10/28 (36) |
| Yanai et al. [64] | 13/39 (33) | 21/34 (62) |
| Aspect of Management | Current State of Knowledge | Future Perspectives |
|---|---|---|
| Risk stratification |
|
|
| Diagnosing recurrence |
|
|
| Treatment |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanzel, J.; Drobne, D. Contemporary Management of Postoperative Crohn’s Disease after Ileocolonic Resection. J. Clin. Med. 2022, 11, 6746. https://doi.org/10.3390/jcm11226746
Hanzel J, Drobne D. Contemporary Management of Postoperative Crohn’s Disease after Ileocolonic Resection. Journal of Clinical Medicine. 2022; 11(22):6746. https://doi.org/10.3390/jcm11226746
Chicago/Turabian StyleHanzel, Jurij, and David Drobne. 2022. "Contemporary Management of Postoperative Crohn’s Disease after Ileocolonic Resection" Journal of Clinical Medicine 11, no. 22: 6746. https://doi.org/10.3390/jcm11226746
APA StyleHanzel, J., & Drobne, D. (2022). Contemporary Management of Postoperative Crohn’s Disease after Ileocolonic Resection. Journal of Clinical Medicine, 11(22), 6746. https://doi.org/10.3390/jcm11226746






