ECMO Support in Refractory Cardiogenic Shock: Risk Factors for Mortality
Abstract
:1. Introduction
2. Materials and Methods
2.1. ECMO Support and Anticoagulation
2.2. Outcomes
2.3. Statistical Analyses
3. Results
3.1. Patient and ECMO Characteristics
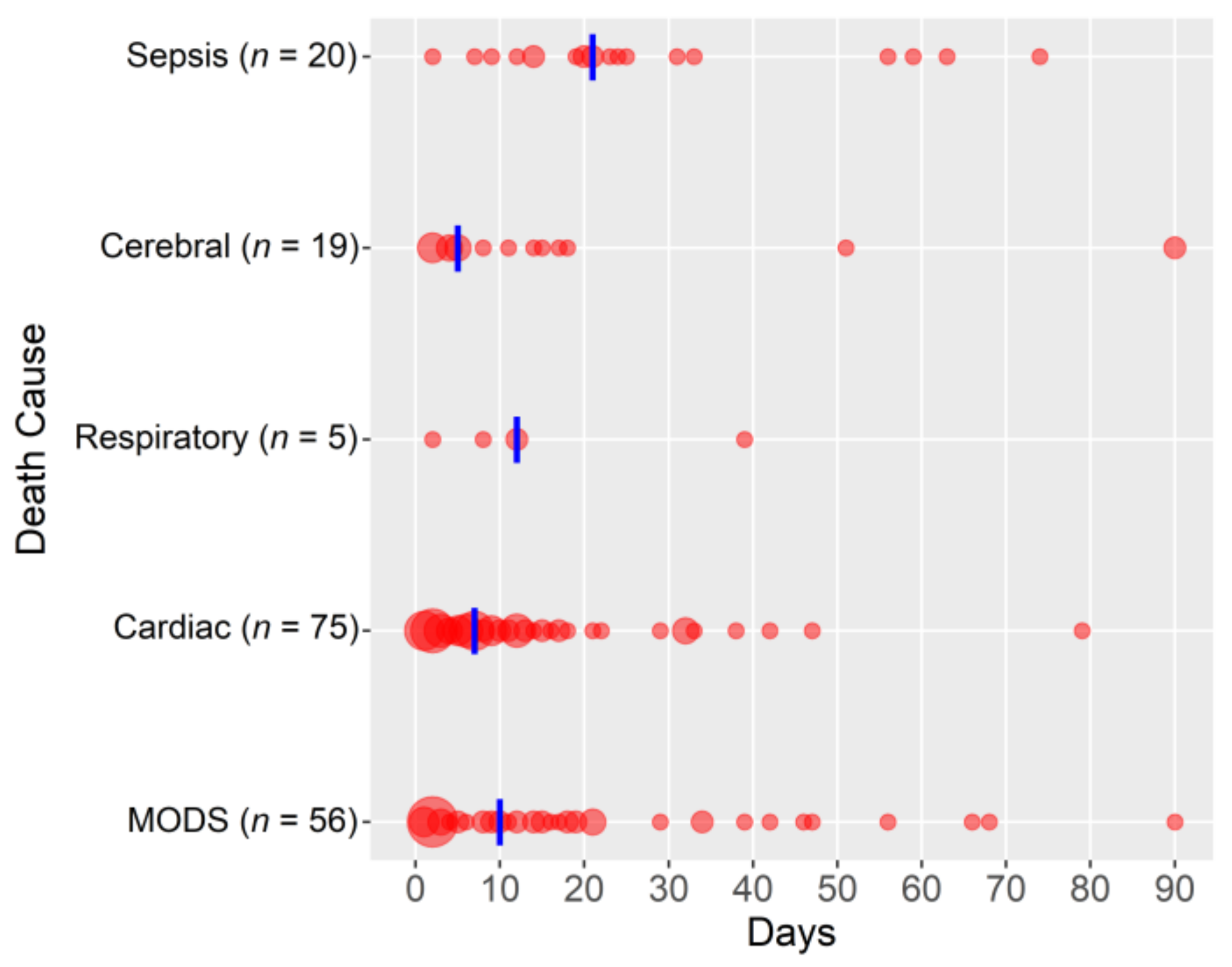
3.2. Outcomes
3.3. Subgroup Analyses
4. Discussion
4.1. Risk Factors for Mortality
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brasseur, A.; Scolletta, S.; Lorusso, R.; Taccone, F.S. Hybrid extracorporeal membrane oxygenation. J. Thorac. Dis. 2018, 10, S707–S715. [Google Scholar] [CrossRef] [PubMed]
- Brogan, T.V.; Lequier, L.; Lorusso, R.; MacLaren, G.; Peek, G.J. Extracorporeal Life Support: The ELSO Red Book, 5th ed.; Extracorporeal Life Support Organization: Ann Arbor, MI, USA, 2017; p. 831. [Google Scholar]
- Sayer, G.T.; Baker, J.N.; Parks, K.A. Heart rescue: The role of mechanical circulatory support in the management of severe refractory cardiogenic shock. Curr. Opin. Crit. Care 2012, 18, 409–416. [Google Scholar] [CrossRef]
- Paden, M.L.; Conrad, S.A.; Rycus, P.T.; Thiagarajan, R.R. Extracorporeal Life Support Organization Registry Report 2012. ASAIO J. 2013, 59, 202–210. [Google Scholar] [CrossRef]
- Cooper, H.A.; Panza, J.A. Cardiogenic shock. Cardiol. Clin. 2013, 31, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Shaefi, S.; O’Gara, B.; Kociol, R.D.; Joynt, K.; Mueller, A.; Nizamuddin, J.; Mahmood, E.; Talmor, D.; Shahul, S. Effect of cardiogenic shock hospital volume on mortality in patients with cardiogenic shock. J. Am. Heart Assoc. 2015, 4, e001462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajsic, S.; Treml, B.; Jadzic, D.; Breitkopf, R.; Oberleitner, C.; Popovic Krneta, M.; Bukumiric, Z. Extracorporeal membrane oxygenation for cardiogenic shock: A meta-analysis of mortality and complications. Ann. Intensive Care 2022, 12, 93. [Google Scholar] [CrossRef] [PubMed]
- Xie, A.; Phan, K.; Tsai, Y.C.; Yan, T.D.; Forrest, P. Venoarterial extracorporeal membrane oxygenation for cardiogenic shock and cardiac arrest: A meta-analysis. J. Cardiothorac. Vasc. Anesth. 2015, 29, 637–645. [Google Scholar] [CrossRef]
- Wilson-Smith, A.R.; Bogdanova, Y.; Roydhouse, S.; Phan, K.; Tian, D.H.; Yan, T.D.; Loforte, A. Outcomes of venoarterial extracorporeal membrane oxygenation for refractory cardiogenic shock: Systematic review and meta-analysis. Ann. Cardiothorac. Surg. 2019, 8, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, H.R.; Hochman, J.S. Cardiogenic Shock. Circulation 2008, 117, 686–697. [Google Scholar] [CrossRef]
- Lequier, L.; Annich, G.; Al-Ibrahim, O.; Bembea, M.; Brodie, D.; Brogan, T.; Buckvold, h.; Chicoine, L.; Conrad, S.; Cooper, D.; et al. ELSO Anticoagulation Guideline; Extracorporeal Life Support Organization, Ed.; Extracorporeal Life Support Organization (ELSO): Ann Arbor, MI, USA, 2014. [Google Scholar]
- McMichael, A.B.V.; Ryerson, L.M.; Ratano, D.; Fan, E.; Faraoni, D.; Annich, G.M. 2021 ELSO Adult and Pediatric Anticoagulation Guidelines. ASAIO J. 2022, 68, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Rajsic, S.; Breitkopf, R.; Jadzic, D.; Popovic Krneta, M.; Tauber, H.; Treml, B. Anticoagulation Strategies during Extracorporeal Membrane Oxygenation: A Narrative Review. J. Clin. Med. 2022, 11, 5147. [Google Scholar] [CrossRef] [PubMed]
- Krisa, V.M.; Kevin, L.; Giles, P.J. ECMO Extracorporeal Cardiopulmonary Support in Critical Care Third Edition, 3rd ed.; Extracorporeal Life Support Organization: Ann Arbor, MI, USA, 2005. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [Green Version]
- Metra, M.; Ponikowski, P.; Dickstein, K.; McMurray, J.J.; Gavazzi, A.; Bergh, C.H.; Fraser, A.G.; Jaarsma, T.; Pitsis, A.; Mohacsi, P.; et al. Advanced chronic heart failure: A position statement from the Study Group on Advanced Heart Failure of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2007, 9, 684–694. [Google Scholar] [CrossRef] [PubMed]
- Sohail, S.; Fan, E.; Foroutan, F.; Ross, H.J.; Billia, F.; Alba, A.C. Predictors of Mortality in Patients Treated with Veno-Arterial ECMO for Cardiogenic Shock Complicating Acute Myocardial Infarction: A Systematic Review and Meta-Analysis. J. Cardiovasc. Transl. Res. 2022, 15, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Sun, H.Y.; Tsai, M.S.; Ko, W.J.; Tsai, P.R.; Hu, F.C.; Chen, Y.C.; Chang, S.C. Predictors of survival in adults undergoing extracorporeal membrane oxygenation with severe infections. J. Thorac. Cardiovasc. Surg. 2016, 152, 1526–1536.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, R.; Hachamovitch, R.; Kittleson, M.; Patel, J.; Arabia, F.; Moriguchi, J.; Esmailian, F.; Azarbal, B. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: A meta-analysis of 1,866 adult patients. Ann. Thorac. Surg. 2014, 97, 610–616. [Google Scholar] [CrossRef]
- Shekar, K.; Badulak, J.; Peek, G.; Boeken, U.; Dalton, H.J.; Arora, L.; Zakhary, B.; Ramanathan, K.; Starr, J.; Akkanti, B.; et al. Extracorporeal Life Support Organization Coronavirus Disease 2019 Interim Guidelines: A Consensus Document from an International Group of Interdisciplinary Extracorporeal Membrane Oxygenation Providers. ASAIO J. 2020, 66, 707–721. [Google Scholar] [CrossRef]
- Rastan, A.J.; Lachmann, N.; Walther, T.; Doll, N.; Gradistanac, T.; Gommert, J.F.; Lehmann, S.; Wittekind, C.; Mohr, F.W. Autopsy findings in patients on postcardiotomy extracorporeal membrane oxygenation (ECMO). Int. J. Artif. Organs 2006, 29, 1121–1131. [Google Scholar] [CrossRef] [PubMed]
- Cartwright, B.; Bruce, H.M.; Kershaw, G.; Cai, N.; Othman, J.; Gattas, D.; Robson, J.L.; Hayes, S.; Alicajic, H.; Hines, A.; et al. Hemostasis, coagulation and thrombin in venoarterial and venovenous extracorporeal membrane oxygenation: The HECTIC study. Sci. Rep. 2021, 11, 7975. [Google Scholar] [CrossRef]
- Mazzeffi, M.; Greenwood, J.; Tanaka, K.; Menaker, J.; Rector, R.; Herr, D.; Kon, Z.; Lee, J.; Griffith, B.; Rajagopal, K.; et al. Bleeding, Transfusion, and Mortality on Extracorporeal Life Support: ECLS Working Group on Thrombosis and Hemostasis. Ann. Thorac. Surg. 2016, 101, 682–689. [Google Scholar] [CrossRef]
- Abruzzo, A.; Gorantla, V.; Thomas, S.E. Venous thromboembolic events in the setting of extracorporeal membrane oxygenation support in adults: A systematic review. Thromb. Res. 2022, 212, 58–71. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.J.; Ha, S.O.; Kim, H.S.; Park, S.; Han, S.J.; Lee, S.H. The Simplified Acute Physiology Score II as a Predictor of Mortality in Patients Who Underwent Extracorporeal Membrane Oxygenation for Septic Shock. Ann. Thorac. Surg. 2017, 103, 1246–1253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.I.; Lee, H.S.; Kim, H.S.; Ha, S.O.; Lee, W.Y.; Park, S.J.; Lee, S.H.; Lee, T.H.; Seo, J.Y.; Choi, H.H.; et al. The pre-ECMO simplified acute physiology score II as a predictor for mortality in patients with initiation ECMO support at the emergency department for acute circulatory and/or respiratory failure: A retrospective study. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 59. [Google Scholar] [CrossRef] [Green Version]
- Fong, K.M.; Au, S.Y.; Ng, G.W.Y.; Leung, A.K.H. Bleeding, thrombosis and transfusion in patients on ECMO: A retrospective study in a tertiary center in Hong Kong. Int. J. Artif. Organs 2021, 44, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Clarke, M.S.; Wills, R.A.; Bowman, R.V.; Zimmerman, P.V.; Fong, K.M.; Coory, M.D.; Yang, I.A. Exploratory study of the ’weekend effect’ for acute medical admissions to public hospitals in Queensland, Australia. Intern. Med. J. 2010, 40, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Aylin, P.; Alexandrescu, R.; Jen, M.H.; Mayer, E.K.; Bottle, A. Day of week of procedure and 30 day mortality for elective surgery: Retrospective analysis of hospital episode statistics. BMJ 2013, 346, f2424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aubron, C.; DePuydt, J.; Belon, F.; Bailey, M.; Schmidt, M.; Sheldrake, J.; Murphy, D.; Scheinkestel, C.; Cooper, D.J.; Capellier, G.; et al. Predictive factors of bleeding events in adults undergoing extracorporeal membrane oxygenation. Ann. Intensive Care 2016, 6, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arachchillage, D.J.; Rajakaruna, I.; Scott, I.; Gaspar, M.; Odho, Z.; Banya, W.; Vlachou, A.; Isgro, G.; Cagova, L.; Wade, J.; et al. Impact of major bleeding and thrombosis on 180-day survival in patients with severe COVID-19 supported with veno-venous extracorporeal membrane oxygenation in the United Kingdom: A multicentre observational study. Br. J. Haematol. 2021, 196, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Rajsic, S.; Breitkopf, R.; Oezpeker, U.C.; Bukumirić, Z.; Dobesberger, M.; Treml, B. The Role of Excessive Anticoagulation and Missing Hyperinflammation in ECMO-Associated Bleeding. J. Clin. Med. 2022, 11, 2314. [Google Scholar] [CrossRef]
- Gray, B.W.; Haft, J.W.; Hirsch, J.C.; Annich, G.M.; Hirschl, R.B.; Bartlett, R.H. Extracorporeal life support: Experience with 2,000 patients. ASAIO J. 2015, 61, 2–7. [Google Scholar] [CrossRef]
- Oude Lansink-Hartgring, A.; de Vries, A.J.; Droogh, J.M.; van den Bergh, W.M. Hemorrhagic complications during extracorporeal membrane oxygenation—The role of anticoagulation and platelets. J. Crit. Care 2019, 54, 239–243. [Google Scholar] [CrossRef]
- Thiagarajan, R.R.; Barbaro, R.P.; Rycus, P.T.; McMullan, D.M.; Conrad, S.A.; Fortenberry, J.D.; Paden, M.L. Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J. 2017, 63, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Olson, S.R.; Murphree, C.R.; Zonies, D.; Meyer, A.D.; McCarty, O.J.T.; Deloughery, T.G.; Shatzel, J.J. Thrombosis and Bleeding in Extracorporeal Membrane Oxygenation (ECMO) Without Anticoagulation: A Systematic Review. ASAIO J. 2021, 67, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Bréchot, N.; Hajage, D.; Kimmoun, A.; Demiselle, J.; Agerstrand, C.; Montero, S.; Schmidt, M.; Luyt, C.E.; Lebreton, G.; Hékimian, G.; et al. Venoarterial extracorporeal membrane oxygenation to rescue sepsis-induced cardiogenic shock: A retrospective, multicentre, international cohort study. Lancet 2020, 396, 545–552. [Google Scholar] [CrossRef]
- Ling, R.R.; Ramanathan, K.; Poon, W.H.; Tan, C.S.; Brechot, N.; Brodie, D.; Combes, A.; MacLaren, G. Venoarterial extracorporeal membrane oxygenation as mechanical circulatory support in adult septic shock: A systematic review and meta-analysis with individual participant data meta-regression analysis. Crit. Care 2021, 25, 246. [Google Scholar] [CrossRef] [PubMed]
- Rajsic, S.; Breitkopf, R.; Bachler, M.; Treml, B. Diagnostic Modalities in Critical Care: Point-of-Care Approach. Diagnostics 2021, 11, 2202. [Google Scholar] [CrossRef] [PubMed]
| Patient Characteristics | All Patients (n = 453) | Survivors (n = 274) | Non-Survivors (n = 179) | p-Value | Missing Data (n/Total) |
|---|---|---|---|---|---|
| Age (years) | 60.9 ± 14.2 | 60.1 ± 14.1 | 62.0 ± 14.3 | 0.165 | 0/453 |
| <30 | 18 (4.0) | 11 (4.0) | 7 (3.9) | 0.198 | 0/453 |
| 31–45 | 41 (9.1) | 27 (9.9) | 14 (7.8) | ||
| 46–60 | 140 (30.9) | 94 (34.3) | 46 (25.7) | ||
| 61–75 | 190 (41.9) | 109 (39.8) | 81 (45.3) | ||
| >75 | 64 (14.1) | 33 (12.0) | 31 (17.3) | ||
| Male sex | 314 (69.3) | 193 (70.4) | 121 (67.6) | 0.533 | 0/453 |
| Body mass index (kg/m2) | 26.5 ± 4.6 | 26.4 ± 4.8 | 26.8 ± 4.3 | 0.294 | 5/453 |
| SAPS III score | 62 (15–104) | 58 (15–99) | 71 (31–104) | <0.001 | 1/453 |
| SAPS III score predicted mortality (%) | 40 (0–93) | 32 (0–91) | 58 (2–93) | <0.001 | 1/453 |
| SOFA score | 11 (1–21) | 11 (2–21) | 12 (1–20) | 0.006 | 1/453 |
| SOFA respiratory | 2 (0–4) | 2 (0–4) | 2 (0–4) | 0.529 | |
| SOFA coagulation | 1 (0–4) | 1 (0–3) | 1 (0–4) | 0.322 | |
| SOFA liver | 1 (0–4) | 1 (0–3) | 0 (0–4) | 0.539 | |
| SOFA cardiovascular | 4 (0–4) | 4 (0–4) | 4 (0–4) | <0.001 | |
| SOFA neurology | 4 (0–4) | 4 (0–4) | 4 (0–4) | 0.024 | |
| SOFA renal | 1 (0–4) | 1 (0–4) | 1 (0–4) | 0.013 | |
| CPR before ECMO initiation | 127 (28.0) | 63 (23.0) | 64 (35.8) | 0.004 | 0/453 |
| Length of ICU stay (days) | 17 (1–170) | 21 (4–98) | 10 (1–170) | <0.001 | 0/453 |
| Cardiogenic shock etiology | 0/453 | ||||
| No cardiotomy | |||||
| Acute heart failure | 126 (27.8) | 63 (23.0) | 63 (35.2) | 0.007 | |
| Right heart failure | 30 (6.6) | 16 (5.8) | 14 (7.8) | ||
| Postcardiotomy | |||||
| Coronary artery bypass surgery (CABG) | 66 (14.6) | 35 (12.8) | 31 (17.3) | ||
| Heart valve surgery (HVS) | 164 (36.2) | 113 (41.2) | 51 (28.5) | ||
| Combined (CABG and HVS, including aortic aneurysm) | 43 (9.5) | 29 (10.6) | 14 (7.8) | ||
| Chronic heart failure | 24 (5.3) | 18 (6.6) | 6 (3.4) | ||
| Mortality-related outcomes | 0/453 | ||||
| Admission to death (days) | 10 (1–79) | - | - | ||
| ECMO initiation to death (days) | 9 (1–79) | - | - | ||
| Death during ECMO support | 86 (19.0) | - | - | ||
| Death during ICU stay | 165 (36.4) | - | - | ||
| Death within 30 days | 150 (33.1) | - | - | ||
| Death within 90 days | 178 (39.3) | - | - | ||
| Death within 180 days | 183 (40.4) | - | - | ||
| Death within 365 days | 185 (40.8) | - | - | ||
| Survival beyond one year | 268 (59.2) | - | - |
| Characteristics | All Patients (n = 453) | Survivors (n = 274) | Non-Survivors (n = 179) | p-Value | Missing Data (n/Total) |
|---|---|---|---|---|---|
| Postcardiotomy | 0/453 | ||||
| No cardiotomy | 156 (34.4) | 79 (28.8) | 77 (43.0) | 0.002 | |
| Postcardiotomy | 297 (65.6) | 195 (71.2) | 102 (57.0) | ||
| ECMO course | 0/453 | ||||
| ECMO duration (days) | 6 (1–22) | 6 (1–20) | 6 (1–22) | 0.364 | |
| ECMO duration <7 days | 326 (72.0) | 204 (74.5) | 122 (68.2) | 0.164 | |
| Admission to ECMO initiation (days) | 0 (0–20) | 0 (0–15) | 0 (0–20) | 0.747 | |
| Day of ECMO initiation | 0/453 | ||||
| Weekday | 355 (78.4) | 224 (81.8) | 131 (73.2) | 0.036 | |
| Weekends | 98 (21.6) | 50 (18.2) | 48 (26.8) | ||
| Anticoagulation during ECMO support | 0/453 | ||||
| UFH | 320 (70.6) | 200 (73.0) | 120 (67.0) | 0.002 | |
| Argatroban | 72 (15.9) | 46 (16.8) | 26 (14.5) | ||
| Epoprostenol | 2 (0.4) | 0 (0.0) | 2 (1.1) | ||
| UFH switch to argatroban | 12 (2.6) | 10 (3.6) | 2 (1.1) | ||
| None | 47 (10.4) | 18 (6.6) | 29 (16.2) | ||
| Reason for ECMO cessation | 0/453 | ||||
| Improvement (weaned) | 328 (72.4) | 247 (90.1) | 81 (45.3) | <0.001 | |
| Bridge to other assistance (heart transplant or VAD) | 32 (7.1) | 26 (9.5) | 6 (3.4) | ||
| Hemorrhage | 7 (1.5) | 1 (0.4) | 6 (3.4) | ||
| Death | 86 (19.0) | - | 86 (48.0) | ||
| Complications | |||||
| Hemorrhage | 209 (46.1) | 107 (39.1) | 102 (57.0) | <0.001 | 0/453 |
| Major hemorrhage | 119 (26.3) | 56 (20.4) | 63 (35.2) | 0.001 | 0/453 |
| Minor hemorrhage | 90 (19.9) | 51 (18.6) | 39 (21.8) | 0.470 | 0/453 |
| Hemorrhage day | 2 (1–14) | 2 (1–14) | 2 (1–14) | 0.578 | 0/453 |
| Hemorrhage within first three days | 150 (74.3) | 76 (73.8) | 74 (74.7) | 1.000 | 0/453 |
| Thrombosis | 114 (25.2) | 71 (25.9) | 43 (24.0) | 0.740 | 0/453 |
| Thrombosis venous | 68 (15.0) | 52 (19.0) | 16 (8.9) | 0.003 | 0/453 |
| Thrombosis arterial | 68 (11.2) | 31 (11.3) | 37 (20.7) | 0.007 | 0/453 |
| Sepsis | 83 (18.4) | 41 (15.0) | 42 (23.6) | 0.025 | 0/453 |
| Variable | B-Coefficient | p-Value | HR | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Hemorrhage | 0.542 | 0.001 | 1.72 | 1.26 | 2.34 |
| SAPS III score | 0.030 | <0.001 | 1.03 | 1.02 | 1.04 |
| ECMO initiation (weekend) | 0.383 | 0.028 | 1.47 | 1.04 | 2.06 |
| Sepsis | 0.381 | 0.032 | 1.46 | 1.03 | 2.07 |
| Resuscitation before ECMO | 0.256 | 0.125 | 1.29 | 0.93 | 1.79 |
| No cardiotomy | 0.149 | 0.362 | 1.16 | 0.84 | 1.60 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajsic, S.; Breitkopf, R.; Bukumiric, Z.; Treml, B. ECMO Support in Refractory Cardiogenic Shock: Risk Factors for Mortality. J. Clin. Med. 2022, 11, 6821. https://doi.org/10.3390/jcm11226821
Rajsic S, Breitkopf R, Bukumiric Z, Treml B. ECMO Support in Refractory Cardiogenic Shock: Risk Factors for Mortality. Journal of Clinical Medicine. 2022; 11(22):6821. https://doi.org/10.3390/jcm11226821
Chicago/Turabian StyleRajsic, Sasa, Robert Breitkopf, Zoran Bukumiric, and Benedikt Treml. 2022. "ECMO Support in Refractory Cardiogenic Shock: Risk Factors for Mortality" Journal of Clinical Medicine 11, no. 22: 6821. https://doi.org/10.3390/jcm11226821





