Long-Term Outcomes following Common Femoral Endarterectomy
Abstract
1. Introduction
2. Materials and Methods
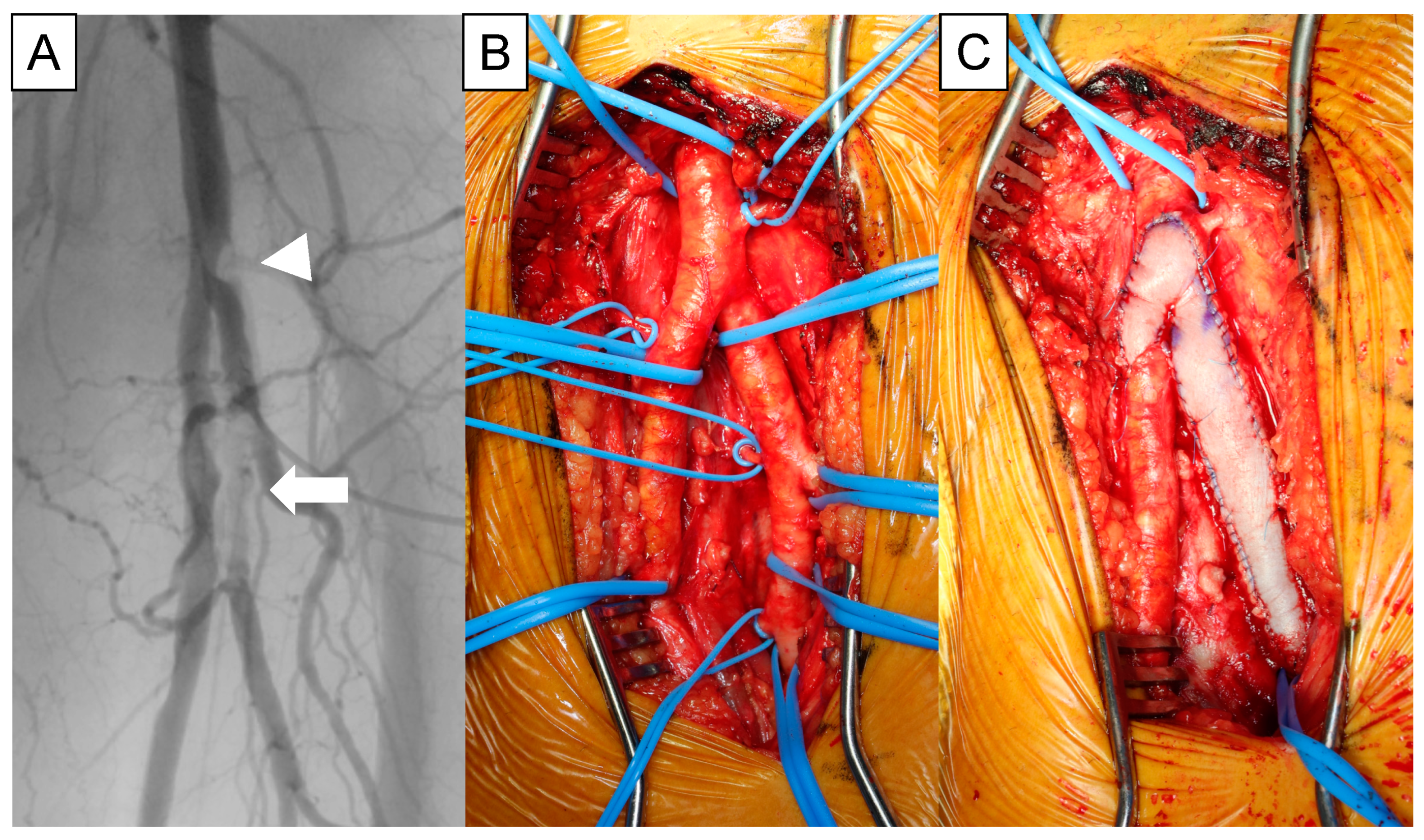
2.1. Operational Technique
2.2. Statistical Analysis
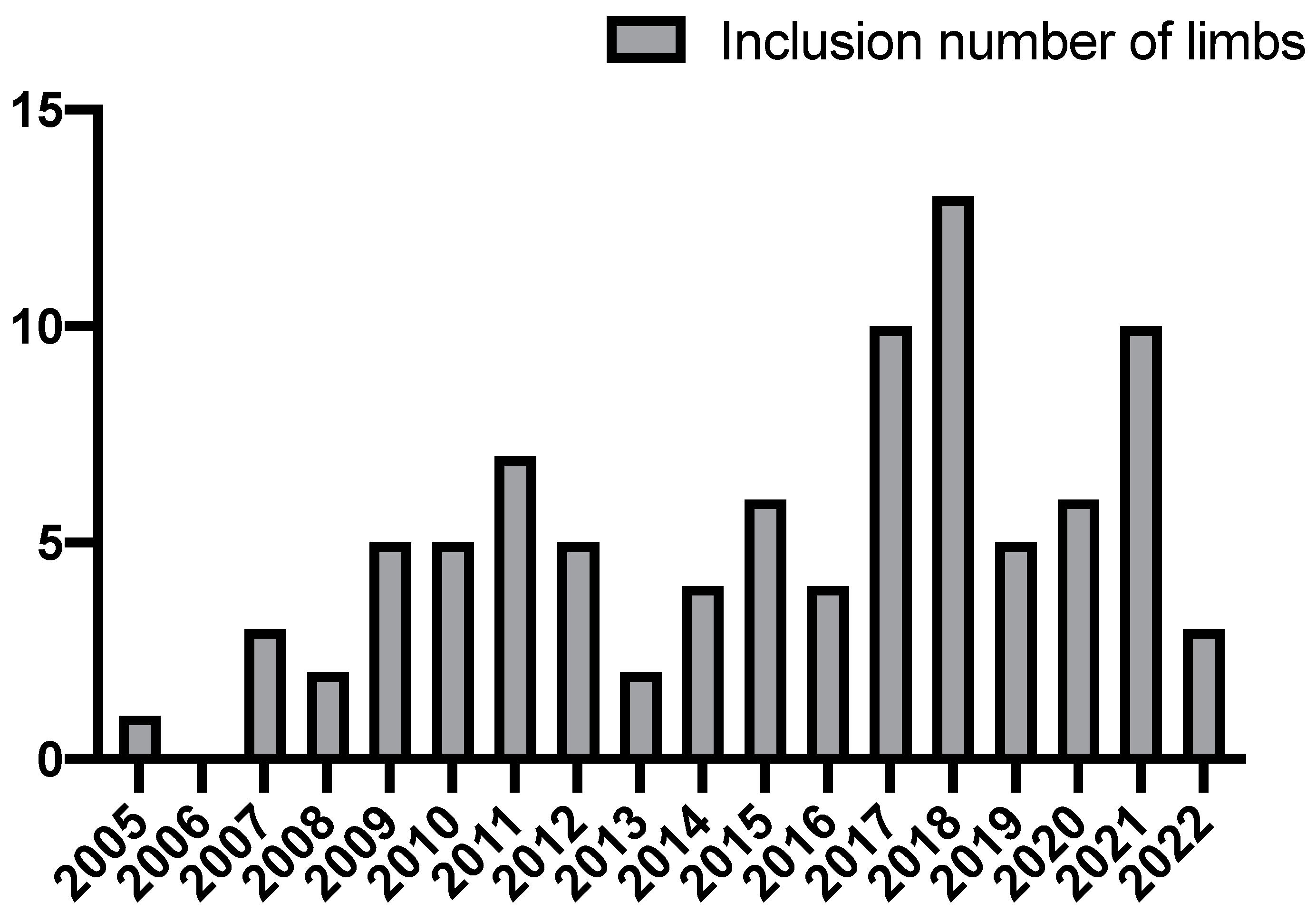
3. Results
3.1. Patient’s Background
3.2. Operative Data
3.3. Thirty-Day Morbidity and Mortality
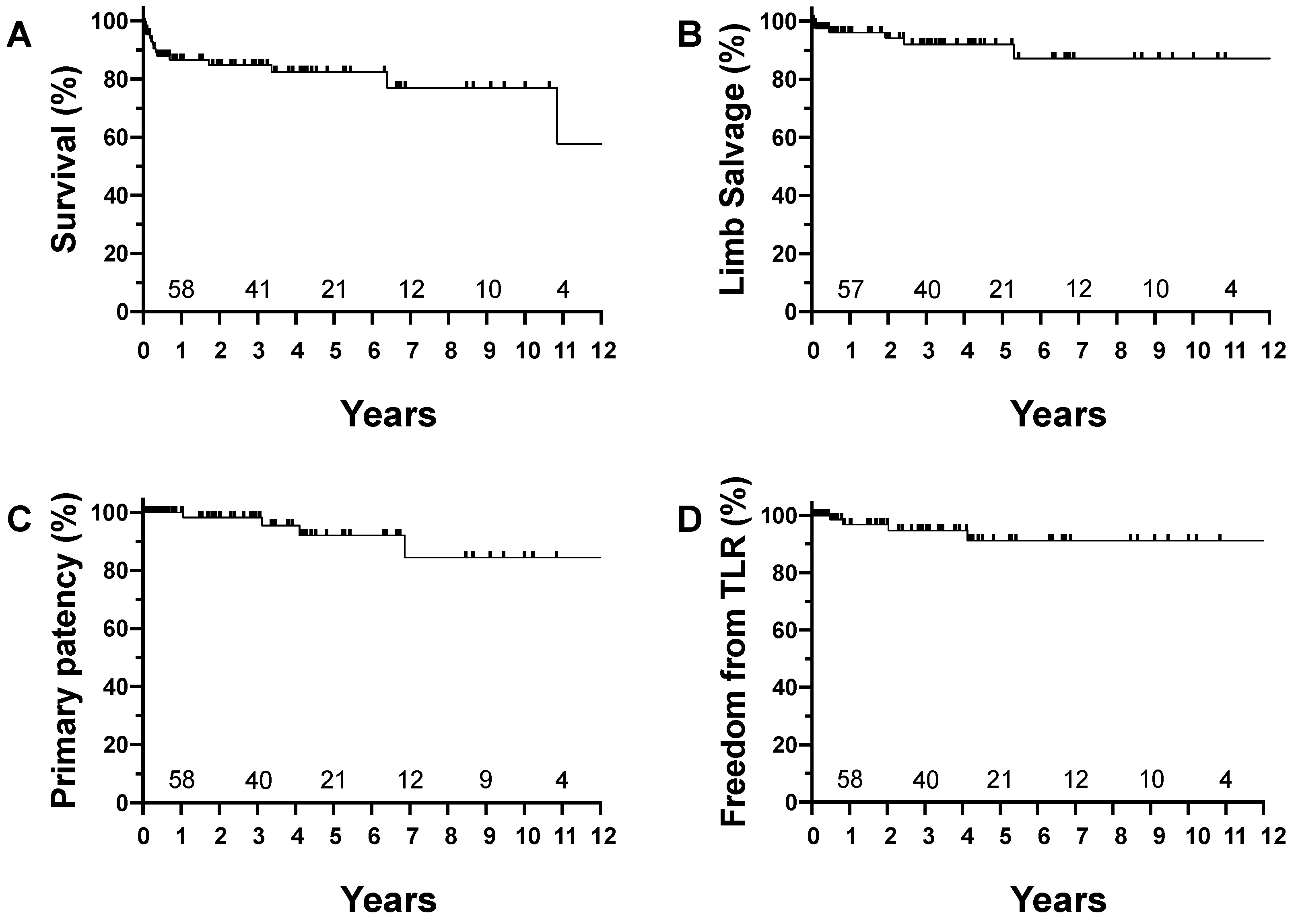
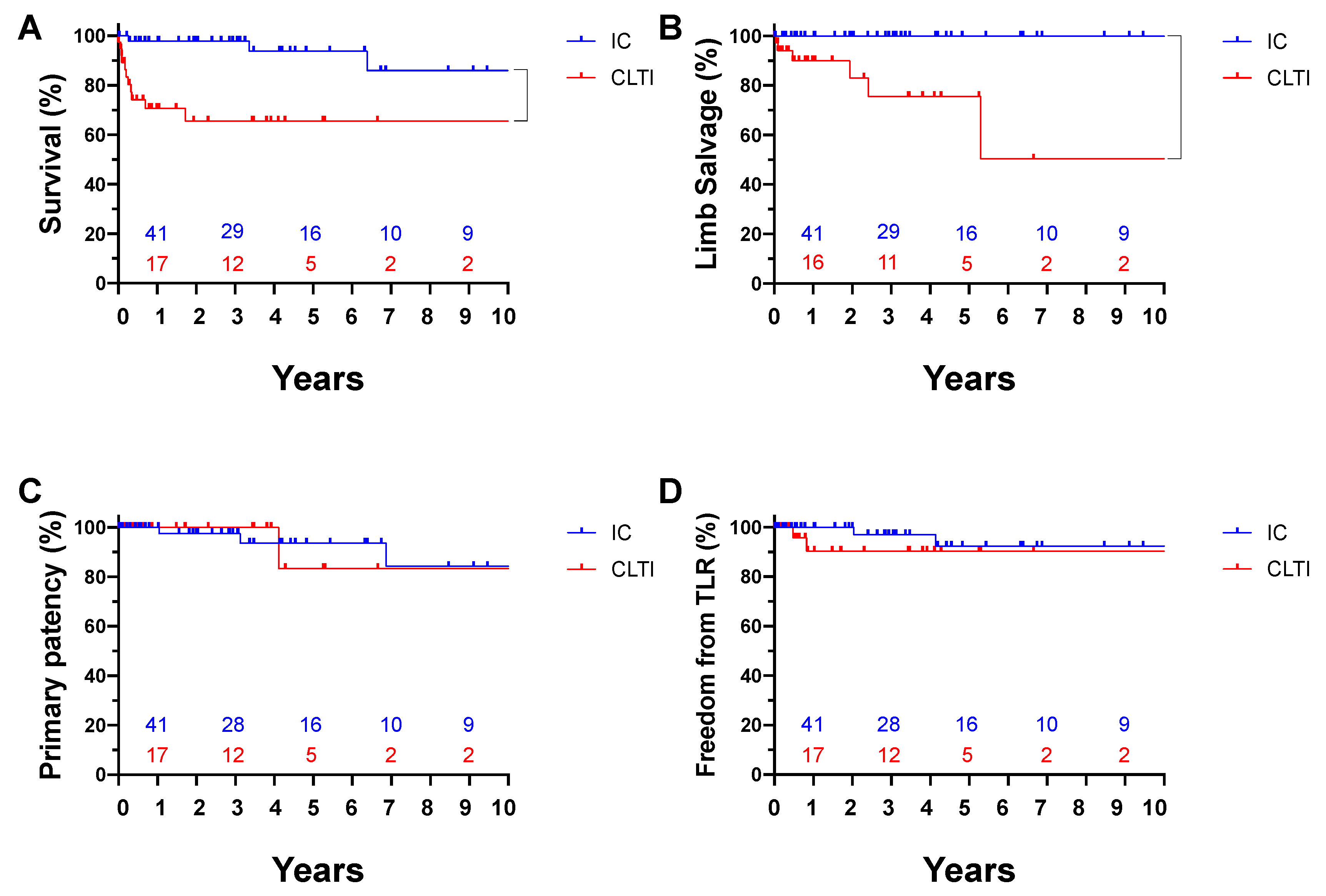
3.4. Ten-Year Outcomes after FEA
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Friedman, S.G. A History of Vascular Surgery; Futura Pub. Co.: Mount Kisco, NY, USA, 1989; 212p. [Google Scholar]
- Kang, J.L.; Patel, V.I.; Conrad, M.F.; LaMuraglia, G.M.; Chung, T.; Cambria, R.P. Common femoral artery occlusive disease: Contemporary results following surgical endarterectomy. J. Vasc. Surg. 2008, 48, 872–877.e1. [Google Scholar] [CrossRef]
- Ballotta, E.; Gruppo, M.; Mazzalai, F.; Da Giau, G. Common femoral artery endarterectomy for occlusive disease: An 8-year single-center prospective study. Surgery 2010, 147, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Kuma, S.; Tanaka, K.; Ohmine, T.; Morisaki, K.; Kodama, A.; Guntani, A.; Ishida, M.; Okazaki, J.; Mii, S. Clinical Outcome of Surgical Endarterectomy for Common Femoral Artery Occlusive Disease. Circ. J. 2016, 80, 964–969. [Google Scholar] [CrossRef]
- Zierler, R.E.; Jordan, W.D.; Lal, B.K.; Mussa, F.; Leers, S.; Fulton, J.; Pevec, W.; Hill, A.; Murad, M.H. The Society for Vascular Surgery practice guidelines on follow-up after vascular surgery arterial procedures. J. Vasc. Surg. 2018, 68, 256–284. [Google Scholar] [CrossRef]
- Kechagias, A.; Ylönen, K.; Biancari, F. Long-term Outcome after Isolated Endarterectomy of the Femoral Bifurcation. World J. Surg. 2007, 32, 51–54. [Google Scholar] [CrossRef]
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; White, J.V.; Dick, F.; Fitridge, R.; Mills, J.L.; Ricco, J.-B.; Suresh, K.R.; Murad, M.H.; et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. J. Vasc. Surg. 2019, 69, 3S–125S.e40. [Google Scholar] [CrossRef]
- Rocha-Singh, K.J.; Zeller, T.; Jaff, M.R. Peripheral arterial calcification: Prevalence, mechanism, detection, and clinical implications. Catheter. Cardiovasc. Interv. 2014, 83, E212–E220. [Google Scholar] [CrossRef]
- Miyahara, T.; Shigematsu, K.; Nishiyama, A.; Hashimoto, T.; Hoshina, K.; Watanabe, T. Long-Term Results of Combined Aortoiliac and Infrainguinal Arterial Reconstruction for the Treatment of Critical Limb Ischemia. Ann. Vasc. Dis. 2015, 8, 14–20. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Takayama, T.; Matsumura, J.S. Complete Lower Extremity Revascularization via a Hybrid Procedure for Patients with Critical Limb Ischemia. Vasc. Endovasc. Surg. 2018, 52, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Guo, Y.; Ziegler, K.; Model, L.S.; Eghbalieh, S.D.; Brenes, R.A.; Kim, S.T.; Shu, C.; Dardik, A. Current Usage and Future Directions for the Bovine Pericardial Patch. Ann. Vasc. Surg. 2011, 25, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Noronen, K.; Söderström, M.; Kouhia, S.; Venermo, M. Bovine pericardial patch—A good alternative in femoral angioplasty. J. Vasc. Surg. 2022. [Google Scholar] [CrossRef] [PubMed]
- Halpin, D.; Erben, Y.; Jayasuriya, S.; Cua, B.; Jhamnani, S.; Mena-Hurtado, C. Management of Isolated Atherosclerotic Stenosis of the Common Femoral Artery: A Review of the Literature. Vasc. Endovasc. Surg. 2017, 51, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Conte, M.S.; Geraghty, P.J.; Bradbury, A.W.; Hevelone, N.D.; Lipsitz, S.R.; Moneta, G.L.; Nehler, M.R.; Powell, R.J.; Sidawy, A.N. Suggested objective performance goals and clinical trial design for evaluating catheter-based treatment of critical limb ischemia. J. Vasc. Surg. 2009, 50, 1462–1473.e3. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, P.J.; Conte, M.S. A critical appraisal of registry-based objective performance goals in peripheral arterial disease. J. Vasc. Surg. 2021, 74, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- Siracuse, J.J.; Gill, H.L.; Schneider, D.B.; Graham, A.R.; Connolly, P.H.; Jones, D.; Meltzer, A.J. Assessing the Perioperative Safety of Common Femoral Endarterectomy in the Endovascular Era. Vasc. Endovasc. Surg. 2013, 48, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.-N.; Amdur, R.L.; Abugideiri, M.; Rahbar, R.; Neville, R.F.; Sidawy, A.N. Postoperative complications after common femoral endarterectomy. J. Vasc. Surg. 2015, 61, 1489–1494.e1. [Google Scholar] [CrossRef] [PubMed]
| Clinical Parameters | Total 80 Patients, 91 Limbs (%) |
|---|---|
| Demographics (n = 80 patients) | |
| Age (years) | 70.8 ± 10 |
| Male | 72 (90.0) |
| Comorbidity (n = 80 patients) | |
| Chronic kidney disease on hemodialysis | 41 (51.3) |
| Diabetes mellitus | 48 (60.0) |
| Coronary artery disease | 35 (43.4) |
| History of tobacco use | 51 (63.8) |
| Symptoms and indications (n = 91 limbs) | |
| Claudication | 50 (54.9) |
| CLTI | 39 (42.9) |
| Others 1 | 2 (2.2) |
| Medication (n = 80 patients) | |
| Antiplatelet agents | 77 (96.3) |
| Anticoagulants | 8 (10.0) |
| Statins | 28 (35.0) |
| Total 91 Limbs (%) | |
|---|---|
| Anesthesia | |
| General | 78 (85.7) |
| Epidural/spinal | 8 (8.8) |
| Regional Nerve Block | 1 (1.1) |
| Local | 4 (4.4) |
| Closure of CFA | |
| Primary closure | 51 (56.0) |
| Patch angioplasty | 40 (44.0) |
| Dacron | 32 (80.0 *) |
| Bovine pericardium | 7 (17.5 *) |
| Rotational flap using SFA | 1 (2.5 *) |
| Total 91 Limbs (%) | |
|---|---|
| Profundaplasty | 13 (14.2) |
| Bypass | 24 (26.3) |
| Cross over | 4 (16.7 *) |
| SFA-popliteal artery | 10 (41.7 *) |
| Distal bypass | 10 (41.7 *) |
| EVT | 29 (31.9) |
| Proximal | 20 (69.0 §) |
| Distal | 7 (24.1 §) |
| Bidirectional | 2 (6.9 §) |
| Contralateral FEA | 10 (11.0) |
| Total 80 Patients, 91 Limbs (%) | |
|---|---|
| Mortality | 2 (2.2) |
| Gastrointestinal bleeding | 1 (1.1) |
| Cardiac | 1 (1.1) |
| Morbidity | 10 (11.0) |
| Gastrointestinal | 2 (2.2) |
| Pneumonia | 4 (4.4) |
| Cardiac | 4 (4.4) |
| Wound complication | 2 (2.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hashimoto, T.; Yamamoto, S.; Kimura, M.; Sano, M.; Sato, O.; Deguchi, J. Long-Term Outcomes following Common Femoral Endarterectomy. J. Clin. Med. 2022, 11, 6873. https://doi.org/10.3390/jcm11226873
Hashimoto T, Yamamoto S, Kimura M, Sano M, Sato O, Deguchi J. Long-Term Outcomes following Common Femoral Endarterectomy. Journal of Clinical Medicine. 2022; 11(22):6873. https://doi.org/10.3390/jcm11226873
Chicago/Turabian StyleHashimoto, Takuya, Satoshi Yamamoto, Masaru Kimura, Masaya Sano, Osamu Sato, and Juno Deguchi. 2022. "Long-Term Outcomes following Common Femoral Endarterectomy" Journal of Clinical Medicine 11, no. 22: 6873. https://doi.org/10.3390/jcm11226873
APA StyleHashimoto, T., Yamamoto, S., Kimura, M., Sano, M., Sato, O., & Deguchi, J. (2022). Long-Term Outcomes following Common Femoral Endarterectomy. Journal of Clinical Medicine, 11(22), 6873. https://doi.org/10.3390/jcm11226873






