A Novel Workflow with a Customizable 3D Printed Vaginal Template and a Direction Modulated Brachytherapy (DMBT) Tandem Applicator for Adaptive Interstitial Brachytherapy of the Cervix
Abstract
1. Introduction
2. Materials and Methods
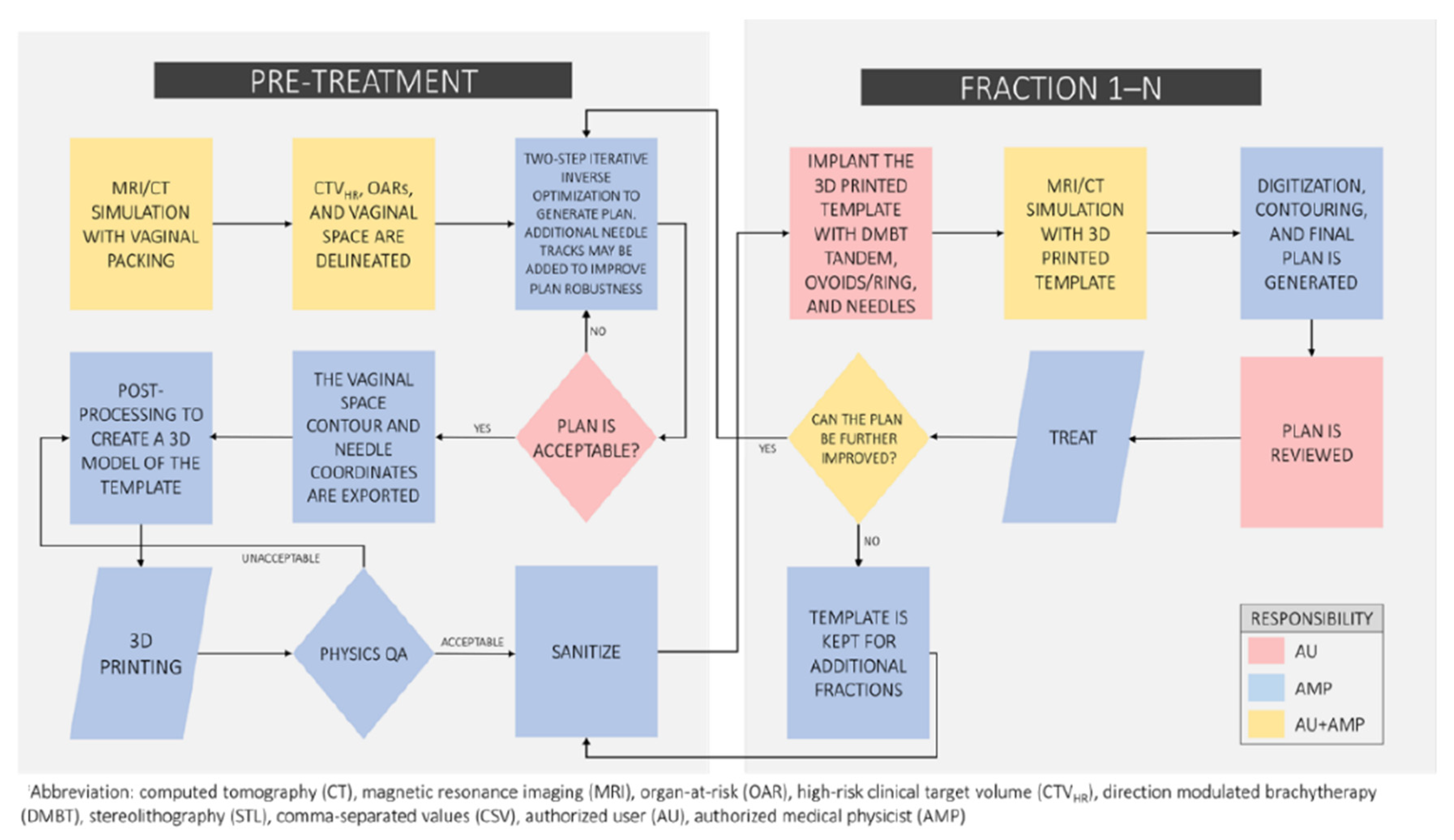
2.1. The Proposed Workflow
2.2. A Patient Example
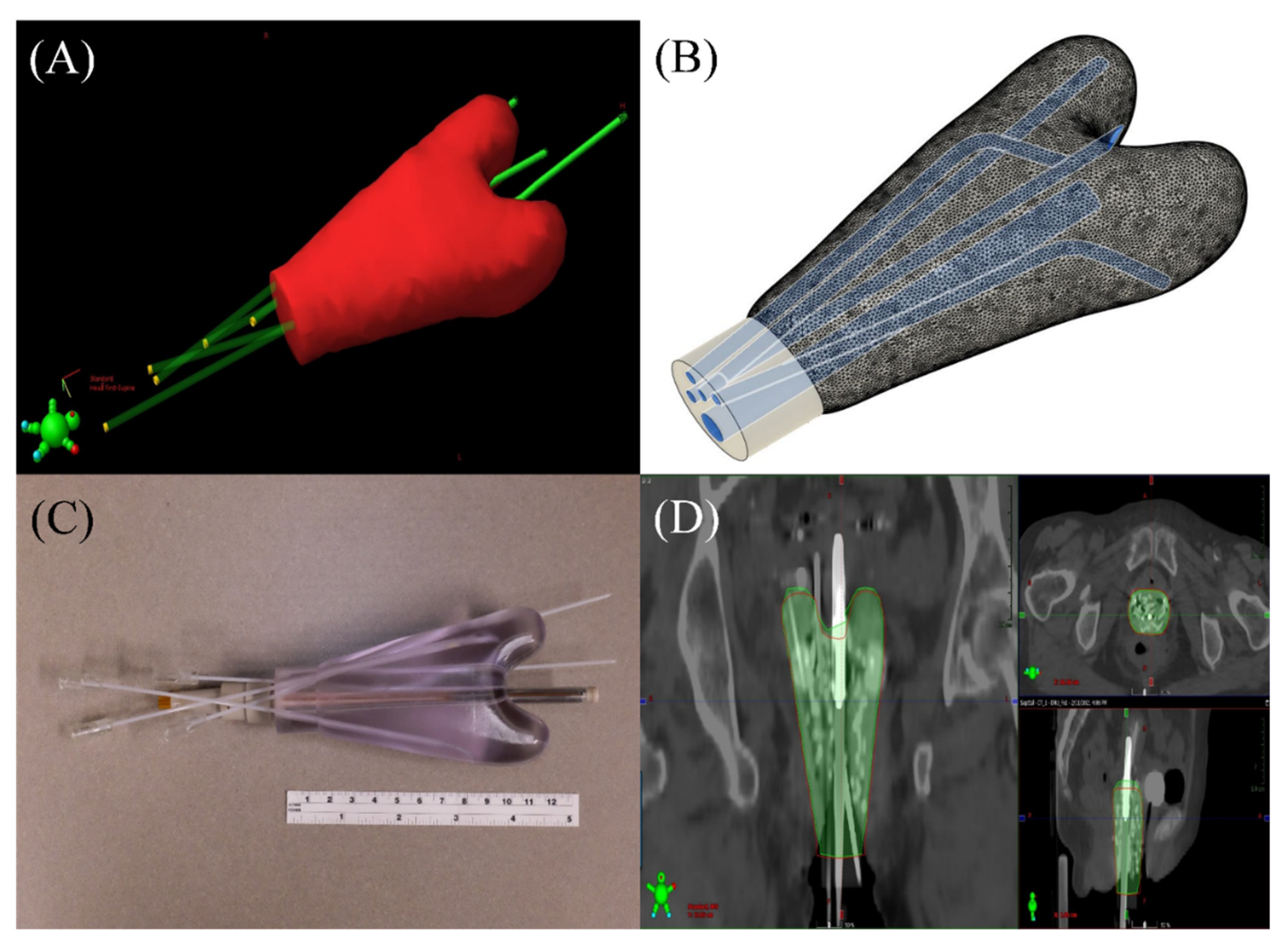
2.3. 3D Printed Vaginal Template
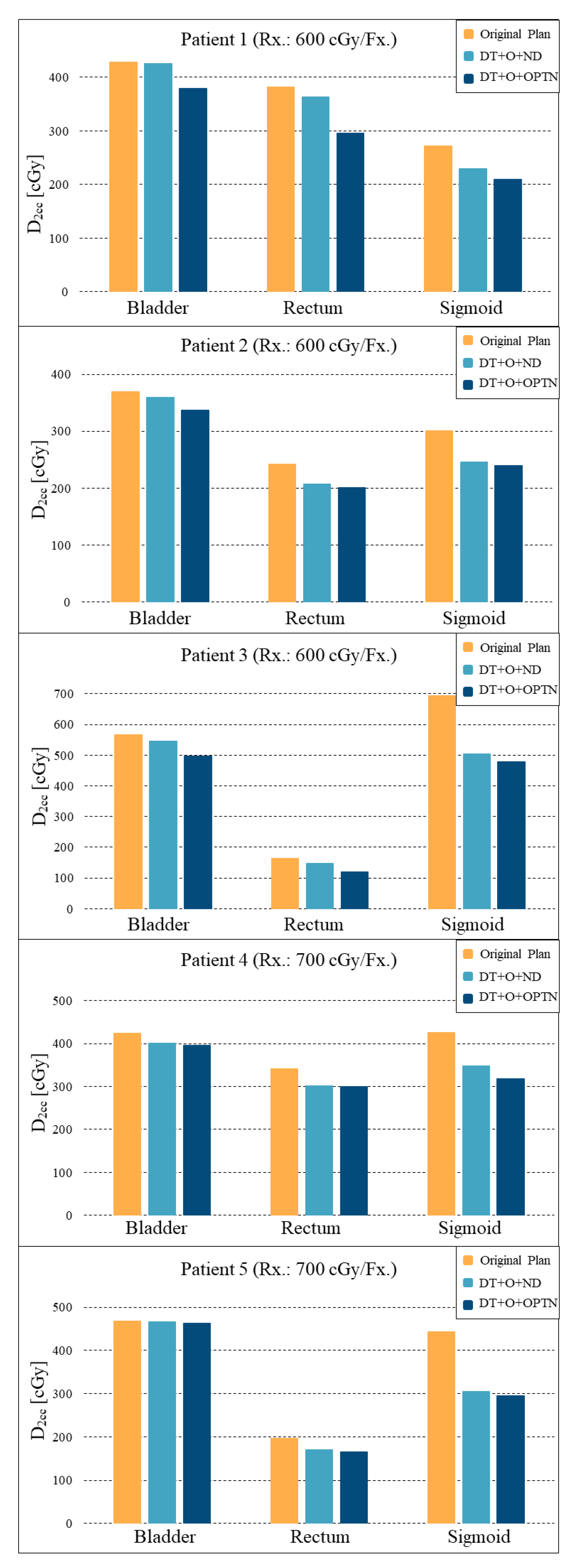
2.4. Retrospective Plan Comparison
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Haie-Meder, C.; Thomas, L.; Barillot, I.; Pommier, P.; Nickers, P. Image-guided adaptive brachytherapy in the treatment of patients with cervix cancer. Cancer Radiother. 2013, 17, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Pötter, R.; Fidarova, E.; Kirisits, C.; Dimopoulos, J. Image-guided Adaptive Brachytherapy for Cervix Carcinoma. Clin. Oncol. 2008, 20, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulos, J.C.; Petrow, P.; Tanderup, K.; Petric, P.; Berger, D.; Kirisits, C.; Pedersen, E.M.; van Limbergen, E.; Haie-Meder, C.; Pötter, R. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (IV): Basic principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother. Oncol. 2012, 103, 113–122. [Google Scholar] [CrossRef]
- Nomden, C.N.; de Leeuw, A.A.; Moerland, M.A.; Roesink, J.M.; Tersteeg, R.J.; Jürgenliemk-Schulz, I.M. Clinical Use of the Utrecht Applicator for Combined Intracavitary/Interstitial Brachytherapy Treatment in Locally Advanced Cervical Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 1424–1430. [Google Scholar] [CrossRef] [PubMed]
- Kirisits, C.; Lang, S.; Dimopoulos, J.; Berger, D.; Georg, D.; Pötter, R. The Vienna applicator for combined intracavitary and interstitial brachytherapy of cervical cancer: Design, application, treatment planning, and dosimetric results. Int. J. Radiat. Oncol. Biol. Phys. 2006, 65, 624–630. [Google Scholar] [CrossRef]
- Callaghan, C.M.; Adams, Q.; Flynn, R.T.; Wu, X.; Xu, W.; Kim, Y. Systematic Review of Intensity-Modulated Brachytherapy (IMBT): Static and Dynamic Techniques. Int. J. Radiat. Oncol. Biol. Phys. 2019, 105, 206–221. [Google Scholar] [CrossRef]
- Cunha, J.A.M.; Flynn, R.; Bélanger, C.; Callaghan, C.; Kim, Y.; Jia, X.; Chen, Z.; Beaulieu, L. Brachytherapy Future Directions. Semin. Radiat. Oncol. 2020, 30, 94–106. [Google Scholar] [CrossRef]
- Webster, M.J.; Devic, S.; Vuong, T.; Han, D.Y.; Park, J.C.; Scanderbeg, D.; Lawson, J.; Song, B.; Watkins, W.T.; Pawlicki, T.; et al. Dynamic modulated brachytherapy (DMBT) for rectal cancer. Med. Phys. 2013, 40, 11718. [Google Scholar] [CrossRef]
- Webster, M.J.; Devic, S.; Vuong, T.; Han, D.Y.; Scanderbeg, D.; Choi, D.; Song, B.; Song, W.Y. HDR brachytherapy of rectal cancer using a novel grooved-shielding applicator design. Med. Phys. 2013, 40, 91704. [Google Scholar] [CrossRef]
- Han, D.Y.; Webster, M.J.; Scanderbeg, D.J.; Yashar, C.; Choi, D.; Song, B.; Devic, S.; Ravi, A.; Song, W.Y. Direction-Modulated Brachytherapy for High-Dose-Rate Treatment of Cervical Cancer. I: Theoretical Design. Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 666–673. [Google Scholar] [CrossRef]
- Han, D.Y.; Safigholi, H.; Soliman, A.; Ravi, A.; Leung, E.; Scanderbeg, D.J.; Liu, Z.; Owrangi, A.; Song, W.Y. Direction modulated brachytherapy for treatment of cervical cancer. II: Comparative planning study with intracavitary and intracavitary-interstitial techniques. Int. J. Radiat. Oncol. Biol. Phys. 2016, 96, 440–448. [Google Scholar] [CrossRef]
- Soliman, A.S.; Elzibak, A.; Easton, H.; Kim, J.Y.; Han, D.Y.; Safigholi, H.; Mashouf, S.; Owrangi, A.; Ravi, A.; Song, W.Y. Quantitative MRI assessment of a novel direction modulated brachytherapy tandem applicator for cervical cancer at 1.5T. Radiother. Oncol. 2016, 120, 500–506. [Google Scholar] [CrossRef]
- Soliman, A.S.; Owrangi, A.; Ravi, A.; Song, W.Y. Metal artefacts in MRI-guided brachytherapy of cervical cancer. J. Contemp. Brachytherapy 2016, 8, 363–369. [Google Scholar] [CrossRef]
- Safigholi, H.; Meigooni, A.S.; Song, W.Y. Comparison of 192Ir, 169Yb, and 60Co high-dose rate brachytherapy sources for skin cancer treatment. Med. Phys. 2017, 44, 4426–4436. [Google Scholar] [CrossRef]
- Safigholi, H.; Han, D.Y.; Mashouf, S.; Soliman, A.; Meigooni, A.S.; Owrangi, A.; Song, W.Y. Direction modulated brachytherapy (DMBT) for treatment of cervical cancer: A planning study with 192Ir, 169Yb, and 60Co HDR sources. Med. Phys. 2017, 44, 6538–6547. [Google Scholar] [CrossRef]
- Elzibak, A.H.; Kager, P.M.; Soliman, A.; Paudel, M.R.; Safigholi, H.; Han, D.Y.; Karotki, A.; Ravi, A.; Song, W.Y. Quantitative CT assessment of a novel direction-modulated brachytherapy tandem applicator. Brachytherapy 2018, 17, 465–475. [Google Scholar] [CrossRef]
- Safigholi, H.; Han, D.Y.; Soliman, A.; Song, W.Y. Direction modulated brachytherapy (DMBT) tandem applicator for cervical cancer treatment: Choosing the optimal shielding material. Med. Phys. 2018, 45, 3524–3533. [Google Scholar] [CrossRef] [PubMed]
- Safigholi, H.; van Veelen, B.; Niatsetski, Y.; Song, W.Y. Modeling of the direction modulated brachytherapy tandem applicator using the Oncentra Brachy advanced collapsed cone engine. Brachytherapy 2018, 17, 1030–1036. [Google Scholar] [CrossRef] [PubMed]
- Guy, C.L.; Oh, S.J.; Han, D.Y.; Kim, S.; Arthur, D.; Song, W.Y. Dynamic Modulated Brachytherapy (DMBT) Balloon Applicator for Accelerated Partial Breast Irradiation. Int. J. Radiat. Oncol. Biol. Phys. 2019, 104, 953–961. [Google Scholar] [CrossRef]
- Fokdal, L.; Sturdza, A.; Mazeron, R.; Haie-Meder, C.; Tan, L.T.; Gillham, C.; Šegedin, B.; Jürgenliemk-Schultz, I.; Kirisits, C.; Hoskin, P.; et al. Image guided adaptive brachytherapy with combined intracavitary and interstitial technique improves the therapeutic ratio in locally advanced cervical cancer: Analysis from the retroEMBRACE study. Radiother. Oncol. 2016, 120, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Pötter, R.; Tanderup, K.; Kirisits, C.; De Leeuw, A.; Kirchheiner, K.; Nout, R.; Tan, L.T.; Haie-Meder, C.; Mahantshetty, U.; Segedin, B.; et al. The EMBRACE II study: The outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin. Transl. Radiat. Oncol. 2018, 9, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Patil, S.; Siauw, T.; Cunha, J.A.M.; Hsu, I.C.; Abbeel, P.; Pouliot, J.; Goldberg, K. An algorithm for computing customized 3D printed implants with curvature constrained channels for enhancing intracavitary brachytherapy radiation delivery. In Proceedings of the 2013 IEEE International Conference on Automation Science and Engineering (CASE), Madison, WI, USA, 17–20 August 2013; pp. 466–473. [Google Scholar]
- Beaulieu, L.; Tedgren, C.; Carrier, J.-F.; Davis, S.D.; Mourtada, F.; Rivard, M.J.; Thomson, R.M.; Verhaegen, F.; Wareing, T.A.; Williamson, J.F. Report of the Task Group 186 on model-based dose calculation methods in brachytherapy beyond the TG-43 formalism: Current status and recommendations for clinical implementation. Med. Phys. 2012, 39, 6208–6236. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-López, J.L.; Ling, D.C.; Keller, A.; Kim, H.; Mojica-Márquez, A.E.; Glaser, S.M.; Beriwal, S. Ureteral stenosis after 3D MRI-based brachytherapy for cervical cancer—Have we identified all the risk factors? Radiother. Oncol. 2021, 155, 86–92. [Google Scholar] [CrossRef]
- Sharma, M.; Fields, E.C.; Todor, D.A. A novel two-step optimization method for tandem and ovoid high-dose-rate brachytherapy treatment for locally advanced cervical cancer. Brachytherapy 2015, 14, 613–618. [Google Scholar] [CrossRef]
- Wiebe, E.; Easton, H.; Thomas, G.; Barbera, L.; D’Alimonte, L.; Ravi, A. Customized vaginal vault brachytherapy with computed tomography imaging-derived applicator prototyping. Brachytherapy 2015, 14, 380–384. [Google Scholar] [CrossRef]
- Lindegaard, J.C.; Madsen, M.L.; Traberg, A.; Meisner, B.; Nielsen, S.K.; Tanderup, K.; Spejlborg, H.; Fokdal, L.U.; Nørrevang, O. Individualised 3D printed vaginal template for MRI guided brachytherapy in locally advanced cervical cancer. Radiother. Oncol. 2016, 118, 173–175. [Google Scholar] [CrossRef]
- Serban, M.; Fokdal, L.; Nielsen, S.K.; Hokland, S.B.; Hansen, A.T.; Spejlborg, H.; Rylander, S.; Petric, P.; Lindegaard, J.C.; Tanderup, K. Characterization of combined intracavitary/interstitial brachytherapy including oblique needles in locally advanced cervix cancer. Brachytherapy 2021, 20, 796–806. [Google Scholar] [CrossRef] [PubMed]
- Morén, B.; Larsson, T.; Tedgren, C. Optimization in treatment planning of high dose-rate brachytherapy—Review and analysis of mathematical models. Med. Phys. 2021, 48, 2057–2082. [Google Scholar] [CrossRef] [PubMed]
- Deufel, C.L.; Epelman, M.A.; Pasupathy, K.S.; Sir, M.Y.; Wu, V.W.; Herman, M.G. PNaV: A tool for generating a high-dose-rate brachytherapy treatment plan by navigating the Pareto surface guided by the visualization of multidimensional trade-offs. Brachytherapy 2020, 19, 518–531. [Google Scholar] [CrossRef] [PubMed]
- Tambas, M.; Tavli, B.; Bilici, N.; Dizman, A.; Sertel, H.; Fayda, M. Computed Tomography-Guided Optimization of Needle Insertion for Combined Intracavitary/Interstitial Brachytherapy With Utrecht Applicator in Locally Advanced Cervical Cancer. Pract. Radiat. Oncol. 2021, 11, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Guthier, C.V.; Damato, A.L.; Hesser, J.W.; Viswanathan, A.N.; Cormack, R.A. A fast inverse treatment planning strategy facilitating optimized catheter selection in image-guided high-dose-rate interstitial gynecologic brachytherapy. Med. Phys. 2017, 44, 6117–6127. [Google Scholar] [CrossRef] [PubMed]
- Adaptiiv. Brachytherapy—3D Printed Applicators. Available online: https://www.adaptiiv.com/product/brachytherapy/ (accessed on 25 May 2022).
- Casey, S.; Bahl, G.; Awotwi-Pratt, J.B. High Dose Rate 192-Ir-Brachytherapy for Basal Cell Carcinoma of the Skin using a 3D Printed Surface Mold. Cureus 2019, 11, e4913. [Google Scholar] [CrossRef]
- Dancewicz, O.; Sylvander, S.; Markwell, T.; Crowe, S.; Trapp, J. Radiological properties of 3D printed materials in kilovoltage and megavoltage photon beams. Phys. Med. 2017, 38, 111–118. [Google Scholar] [CrossRef]
- Kim, S.W.; Shin, H.J.; Kay, C.S.; Son, S.H. A customized bolus produced using a 3-dimensional printer for radiotherapy. PLoS ONE 2014, 9, e110746. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Milosevic, M.; Fyles, A.; Pintilie, M.; Viswanathan, A. Trends in the Utilization of Brachytherapy in Cervical Cancer in the United States. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 111–119. [Google Scholar] [CrossRef]
- Viswanathan, A.N.; Moughan, J.; Small, W.; Levenback, C.; Iyer, R.B.; Hymes, S.R.; Dicker, A.; Miller, B.; Erickson, B.; Gaffney, D.K. The Quality of Cervical Cancer Brachytherapy Implantation and the Impact on Local Recurrence and Disease-Free Survival in Radiation Therapy Oncology Group Prospective Trials 0116 and 0128. Int. J. Gynecol. Cancer 2012, 22, 123–131. [Google Scholar] [CrossRef] [PubMed]


| Volume of CTVHR [cc] | Rx. Dose [cGy] | D90 of CTVHR [cGy] | ||
|---|---|---|---|---|
| Patient 1 | Original Plan | 58.8 | 600.0 | 567.4 |
| DMBT + O + ND | 568.4 | |||
| DMBT + O + OptN | 572.6 | |||
| Patient 2 | Original Plan | 51.2 | 600.0 | 608.2 |
| DMBT + O + ND | 613.1 | |||
| DMBT + O + OptN | 610.1 | |||
| Patient 3 | Original Plan | 45.3 | 600.0 | 537.0 |
| DMBT + O + ND | 537.9 | |||
| DMBT + O + OptN | 538.3 | |||
| Patient 4 | Original Plan | 53.5 | 700.0 | 684.2 |
| DMBT + O + ND | 681.7 | |||
| DMBT + O + OptN | 684.5 | |||
| Patient 5 | Original Plan | 59.7 | 700.0 | 686.0 |
| DMBT + O + ND | 684.6 | |||
| DMBT + O + OptN | 689.5 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sohn, J.J.; Polizzi, M.; Richeson, D.; Gholami, S.; Das, I.J.; Song, W.Y. A Novel Workflow with a Customizable 3D Printed Vaginal Template and a Direction Modulated Brachytherapy (DMBT) Tandem Applicator for Adaptive Interstitial Brachytherapy of the Cervix. J. Clin. Med. 2022, 11, 6989. https://doi.org/10.3390/jcm11236989
Sohn JJ, Polizzi M, Richeson D, Gholami S, Das IJ, Song WY. A Novel Workflow with a Customizable 3D Printed Vaginal Template and a Direction Modulated Brachytherapy (DMBT) Tandem Applicator for Adaptive Interstitial Brachytherapy of the Cervix. Journal of Clinical Medicine. 2022; 11(23):6989. https://doi.org/10.3390/jcm11236989
Chicago/Turabian StyleSohn, James J., Mitchell Polizzi, Dylan Richeson, Somayeh Gholami, Indra J. Das, and William Y. Song. 2022. "A Novel Workflow with a Customizable 3D Printed Vaginal Template and a Direction Modulated Brachytherapy (DMBT) Tandem Applicator for Adaptive Interstitial Brachytherapy of the Cervix" Journal of Clinical Medicine 11, no. 23: 6989. https://doi.org/10.3390/jcm11236989
APA StyleSohn, J. J., Polizzi, M., Richeson, D., Gholami, S., Das, I. J., & Song, W. Y. (2022). A Novel Workflow with a Customizable 3D Printed Vaginal Template and a Direction Modulated Brachytherapy (DMBT) Tandem Applicator for Adaptive Interstitial Brachytherapy of the Cervix. Journal of Clinical Medicine, 11(23), 6989. https://doi.org/10.3390/jcm11236989







