Primary Orbital Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type, without Nasal Involvement
Abstract
:1. Introduction
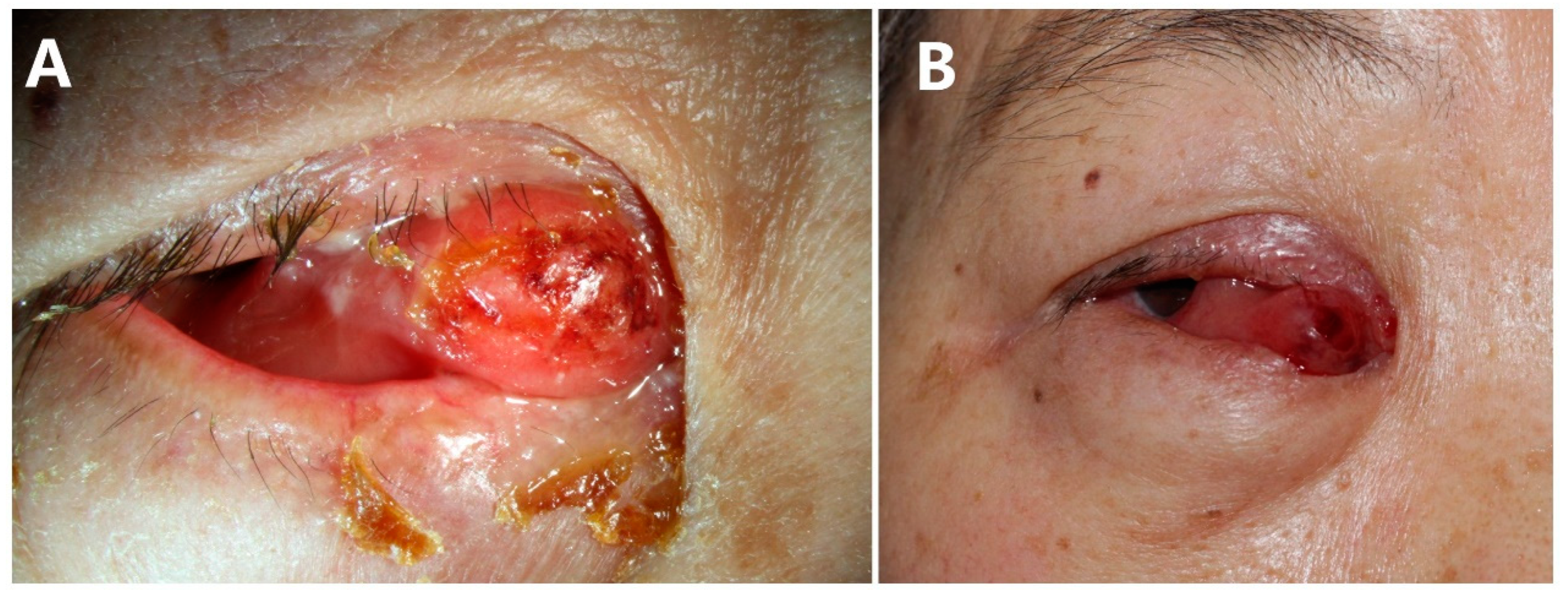
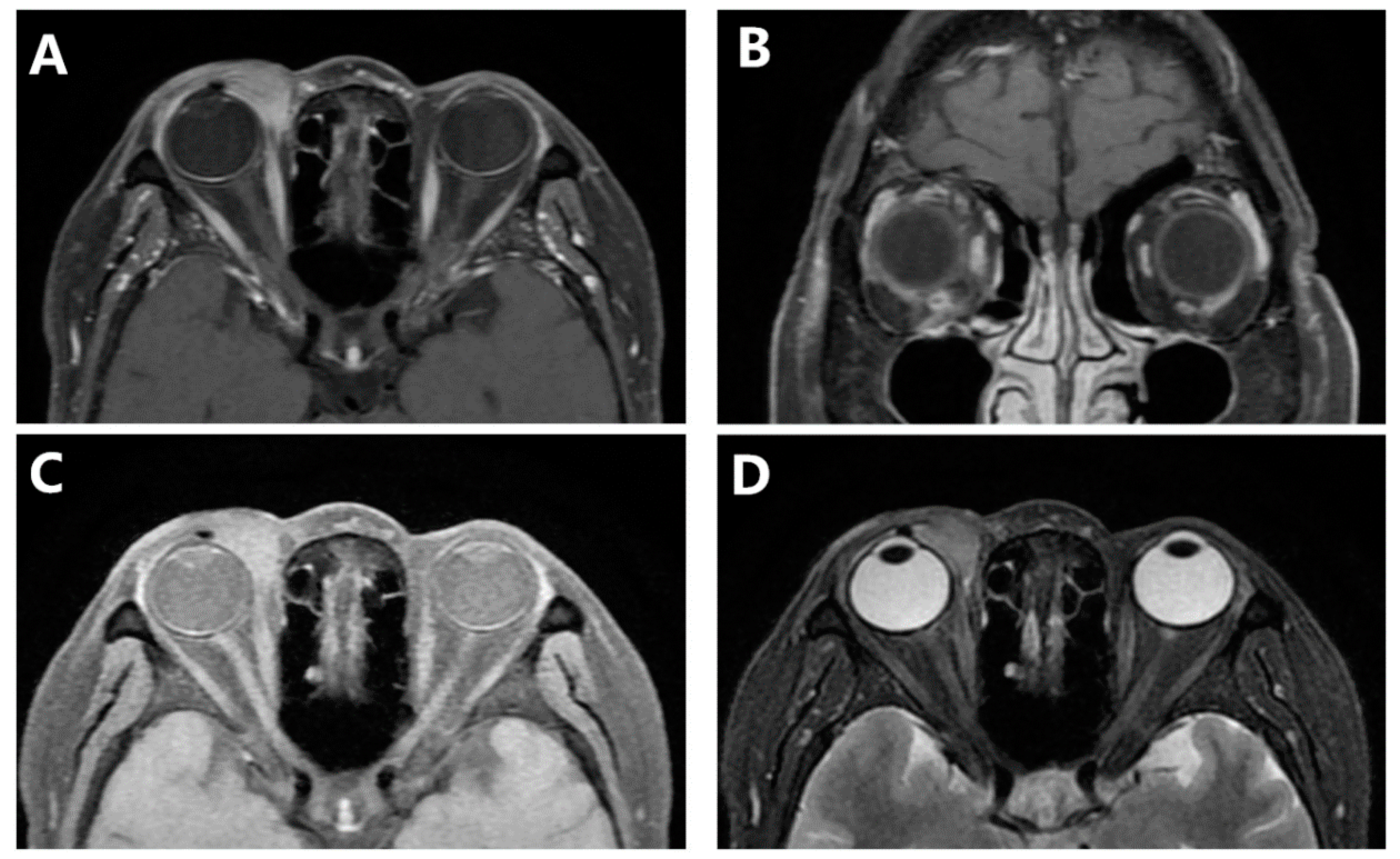
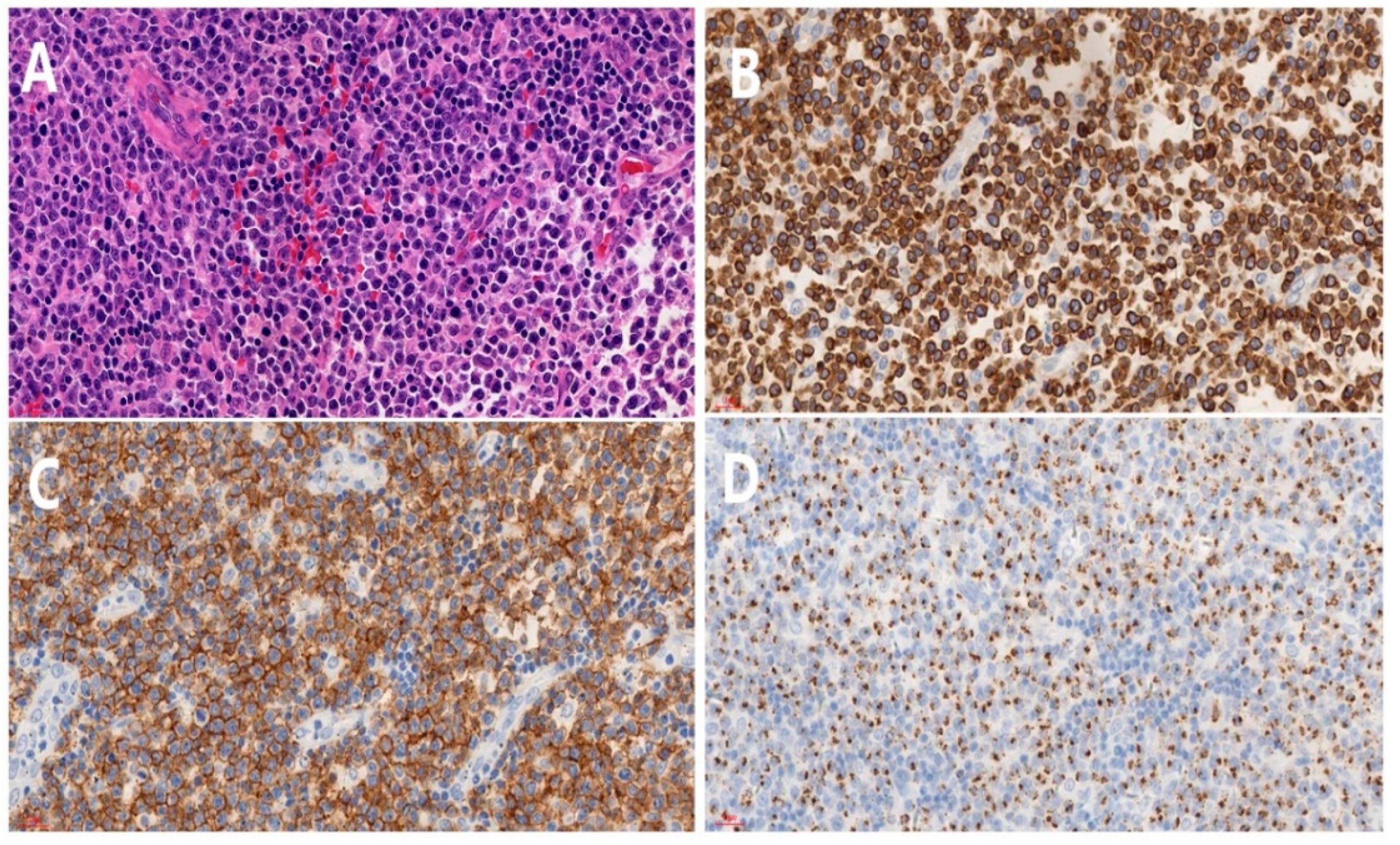
2. Case Presentation
3. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ENKTL | extranodal natural killer/T-cell lymphoma |
| NKTCL | natural killer/T-cell lymphoma |
| MRI | magnetic resonance imaging |
| NHL | Non-Hodgkin lymphoma |
| IOP | intraocular pressure |
| CT | Computed tomography |
| 18F-FDG | 18F-fluorodeoxyglucose |
| EBER | Epstein-Barr virus-encoded small RNA |
| CR | complete remission |
| MALT | mucosa-associated lymphoid tissue lymphoma |
References
- Cimino, L.; Chan, C.C.; Shen, D.; Masini, L.; Ilariucci, F.; Masetti, M.; Asioli, S.; Sartori, A.; Cappuccini, L. Ocular involvement in nasal natural killer t-cell lymphoma. Int. Ophthalmol. 2009, 29, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, E.S.; Nicolae, A.; Pittaluga, S. Peripheral t-cell and nk-cell lymphomas in the who classification: Pearls and pitfalls. Mod. Pathol. 2013, 26 (Suppl. 1), S71–S87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hon, C.; Kwok, A.K.; Shek, T.W.; Chim, J.C.; Au, W.Y. Vision-threatening complications of nasal t/nk lymphoma. Am. J. Ophthalmol. 2002, 134, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Woog, J.J.; Kim, Y.D.; Yeatts, R.P.; Kim, S.; Esmaeli, B.; Kikkawa, D.; Lee, H.B.; Korn, B.S.; Punja, K.; Habermann, T.M.; et al. Natural killer/t-cell lymphoma with ocular and adnexal involvement. Ophthalmology 2006, 113, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, K.; Kunikata, H.; Sugita, S.; Mochizuki, M.; Ichinohasama, R.; Nakazawa, T. First case of primary intraocular natural killer t-cell lymphoma. Bmc Ophthalmol. 2015, 15, 169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ely, A.; Evans, J.; Sundstrom, J.M.; Malysz, J.; Specht, C.S.; Wilkinson, M. Orbital involvement in extranodal natural killer t cell lymphoma: An atypical case presentation and review of the literature. Orbit 2012, 31, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Dai, W.; Zhong, M.; Shen, W.; Zou, K.; Bai, C.G. Natural killer t-cell lymphoma originating from the orbit. Chin. Med. J. 2012, 125, 1677–1680. [Google Scholar] [PubMed]
- Yang, Y.; Luo, Q.; He, W.; Tang, L. Primary ocular natural killer/t-cell lymphomas: Clinicopathologic features and diagnosis. Ophthalmologica 2007, 221, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Marchino, T.; Ibanez, N.; Prieto, S.; Novelli, S.; Szafranska, J.; Mozos, A.; Graell, X.; Buil, J.A. An aggressive primary orbital natural killer/t-cell lymphoma case: Poor response to chemotherapy. Ophthalmic Plast. Reconstr. Surg. 2014, 30, e131–e134. [Google Scholar] [CrossRef] [PubMed]
- Au, W.Y.; Weisenburger, D.D.; Intragumtornchai, T.; Nakamura, S.; Kim, W.S.; Sng, I.; Vose, J.; Armitage, J.O.; Liang, R. Clinical differences between nasal and extranasal natural killer/t-cell lymphoma: A study of 136 cases from the international peripheral t-cell lymphoma project. Blood 2009, 113, 3931–3937. [Google Scholar] [CrossRef] [PubMed]
- Coupland, S.E.; Foss, H.D.; Assaf, C.; Auw-Haedrich, C.; Anastassiou, G.; Anagnostopoulos, I.; Hummel, M.; Karesh, J.W.; Lee, W.R.; Stein, H. T-cell and t/natural killer-cell lymphomas involving ocular and ocular adnexal tissues: A clinicopathologic, immunohistochemical, and molecular study of seven cases. Ophthalmology 1999, 106, 2109–2120. [Google Scholar] [CrossRef] [PubMed]
- Meel, R.; Dhiman, R.; Wadhwani, M.; Kashyap, S.; Sharma, S.; Gogia, A. Isolated extranodal natural killer t-cell lymphoma of the orbit in a young patient: Complete regression with the smile regimen. Ocul. Oncol. Pathol. 2017, 3, 45–48. [Google Scholar] [CrossRef] [Green Version]
- Okada, A.; Harada, Y.; Inoue, T.; Okikawa, Y.; Ichinohe, T.; Kiuchi, Y. A case of primary extranodal natural killer/t-cell lymphoma in the orbit and intraocular tissues with cerebrospinal fluid involvement. Am J Ophthalmol Case Rep 2018, 11, 37–40. [Google Scholar] [CrossRef]
- Ooi, G.C.; Chim, C.S.; Liang, R.; Tsang, K.W.; Kwong, Y.L. Nasal t-cell/natural killer cell lymphoma: Ct and mr imaging features of a new clinicopathologic entity. Am. J. Roentgenol. 2000, 174, 1141–1145. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Perez, J.C.; Yoon, M.K. Natural killer t-cell lymphoma of the orbit: An evidence-based approach. Semin. Ophthalmol. 2017, 32, 116–124. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jing, D.; You, D.; Liu, Z.; Wang, W. Primary Orbital Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type, without Nasal Involvement. J. Clin. Med. 2022, 11, 7010. https://doi.org/10.3390/jcm11237010
Jing D, You D, Liu Z, Wang W. Primary Orbital Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type, without Nasal Involvement. Journal of Clinical Medicine. 2022; 11(23):7010. https://doi.org/10.3390/jcm11237010
Chicago/Turabian StyleJing, Dalan, Debo You, Ziyuan Liu, and Wei Wang. 2022. "Primary Orbital Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type, without Nasal Involvement" Journal of Clinical Medicine 11, no. 23: 7010. https://doi.org/10.3390/jcm11237010





