Early Mortality Risk in Acute Trauma Patients: Predictive Value of Injury Severity Score, Trauma Index, and Different Types of Shock Indices
Abstract
:1. Introduction
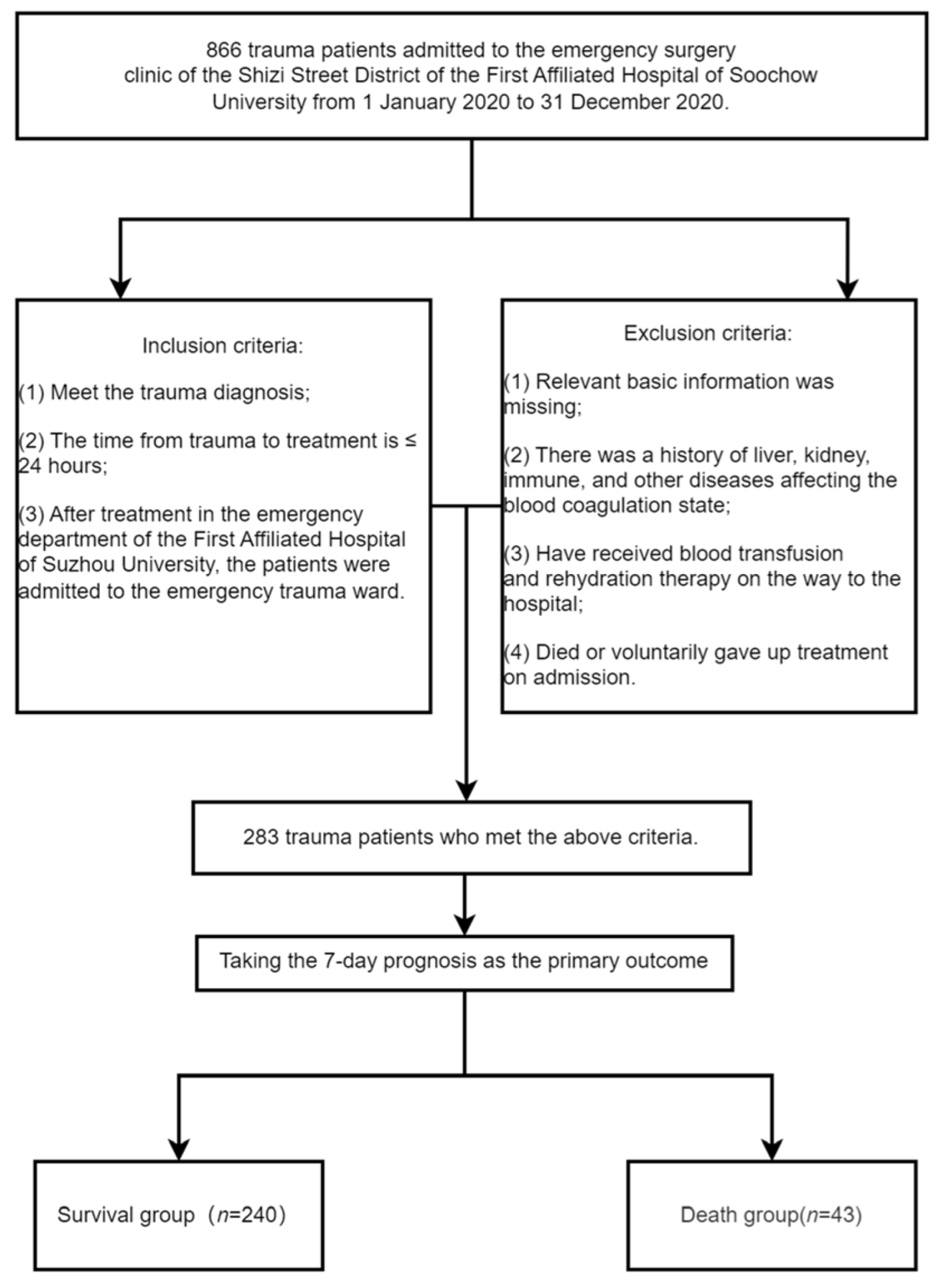
2. Materials and Methods
2.1. Clinical Information
2.2. Research Design
2.3. Statistical Methods
3. Results
3.1. Comparison of Basic Clinical Data
3.2. Comparison of Different Trauma Assessment Tools
3.3. Prediction of Early Mortality Risk in Trauma Patients by ISS, TI, SI, MSI, and ASI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Shanthakumar, D.; Payne, A.; Leitch, T.; Alfa-Wali, M. Trauma Care in Low-and Middle-Income Countries. Surg. J. 2021, 7, e281–e285. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gauss, T.; Ageron, F.X.; Devaud, M.L.; Debaty, G.; Travers, S.; Garrigue, D.; Raux, M.; Harrois, A.; Bouzat, P.; French Trauma Research Initiative; et al. Association of Prehospital Time to In-Hospital Trauma Mortality in a Physician-Staffed Emergency Medicine System. JAMA Surg. 2019, 154, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Voskens, F.J.; van Rein, E.A.J.; van der Sluijs, R.; Houwert, R.M.; Lichtveld, R.A.; Verleisdonk, E.J.; Segers, M.; van Olden, G.; Dijkgraaf, M.; Leenen, L.P.H.; et al. Accuracy of Prehospital Triage in Selecting Severely Injured Trauma Patients. JAMA Surg. 2018, 153, 322–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abajas Bustillo, R.; Amo Setien, F.J.; Ortego Mate, M.D.C.; Segui Gomez, M.; Dura Ros, M.J.; Leal Costa, C. Predictive capability of the injury severity score versus the new injury severity score in the categorization of the severity of trauma patients: A cross-sectional observational study. Eur. J. Trauma Emerg. Surg. 2020, 46, 903–911. [Google Scholar] [CrossRef] [PubMed]
- Ruan, H.; Ge, W.; Li, B.; Zhu, Y.; Yang, F. The application of a trauma index to assess injury severity and prognosis in hospitalized patients with acute trauma. Int. J. Clin. Exp. Med. 2015, 8, 19114–19119. [Google Scholar] [PubMed]
- Davenport, R.A.; Brohi, K. Cause of trauma-induced coagulopathy. Curr. Opin. Anaesthesiol. 2016, 29, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Balhara, K.S.; Hsieh, Y.H.; Hamade, B.; Circh, R.; Kelen, G.D.; Bayram, J.D. Clinical metrics in emergency medicine: The shock index and the probability of hospital admission and inpatient mortality. Emerg. Med. J. 2017, 34, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-C.; Liu, J.-H.; Fang, Z.A.; Shan, G.-L.; Xu, J.; Qi, Z.-W.; Zhu, H.-D.; Yu, X.-Z. Modified shock index and mortality rate of emergency patients. World J. Emerg. Med. 2012, 3, 114–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rau, C.S.; Wu, S.C.; Kuo, S.C.; Spencer, C.H.; Pao-Jen, K.; Shiun-Yuan, H.; Chen, Y.-C.; Hsieh, H.-Y.; Hsieh, C.-H.; Liu, H.-T. Prediction of Massive Transfusion in Trauma Patients with Shock Index, Modified Shock Index, and Age Shock Index. Int. J. Environ. Res. Public Health 2016, 13, 683. [Google Scholar] [CrossRef] [PubMed]
- Waits, C.M.K.; Bower, A.; Simms, K.N.; Feldman, B.C.; Kim, N.; Sergeant, S.; Chilton, F.H.; VandeVord, P.J.; Langefeld, C.D.; Rahbar, E. A Pilot Study Assessing the Impact of rs174537 on Circulating Polyunsaturated Fatty Acids and the Inflammatory Response in Patients with Traumatic Brain Injury. J. Neurotrauma 2020, 37, 1880–1891. [Google Scholar] [CrossRef] [PubMed]
- Schellenberg, M.; Owattanapanich, N.; Grigorian, A.; Lam, L.; Nahmias, J.; Inaba, K. Surviving Nonsurvivable Injuries: Patients Who Elude the ‘Lethal’ Abbreviated Injury Scale Score of Six. J. Surg. Res. 2021, 268, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Butcher, N.E.; Balogh, Z.J. Update on the definition of polytrauma. Eur. J. Trauma Emerg. Surg. 2014, 40, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Bone, L.B.; McNamara, K.; Shine, B.; Border, J. Mortality in multiple trauma patients with fractures. J. Trauma 1994, 37, 262–264, discussion 264–265. [Google Scholar] [CrossRef] [PubMed]
- Hildebrand, F.; Giannoudis, P.; Kretteck, C.; Pape, H.-C. Damage control: Extremities. Injury 2004, 35, 678–689. [Google Scholar] [CrossRef]
- El-Menyar, A.; Goyal, P.; Tilley, E.; Latifi, R. The clinical utility of shock index to predict the need for blood transfusion and outcomes in trauma. J. Surg. Res. 2018, 227, 52–59. [Google Scholar] [CrossRef]
- Olaussen, A.; Blackburn, T.; Mitra, B.; Fitzgerald, M. Review article: Shock index for prediction of critical bleeding post-trauma: A systematic review. Emerg. Med. Australas. 2014, 26, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Jouini, S.; Jebali, A.; Hedhli, H.; Ben Kaddour, R.; Mrabet, A.; Hebaieb, F. Predictive value of shock index ≥1 in severe trauma patients in emergency department. Tunis. Med. 2019, 97, 802–807. [Google Scholar] [PubMed]
- Vang, M.; Østberg, M.; Steinmetz, J.; Rasmussen, L.S. Shock index as a predictor for mortality in trauma patients: A systematic review and meta-analysis. Eur. J. Trauma Emerg. Surg. 2022, 48, 2559–2566. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Hong, K.J.; Shin, S.D.; Ro, Y.S.; Ahn, K.O.; Kim, Y.J.; Lee, E.J. Validation of the Shock Index, Modified Shock Index, and Age Shock Index for Predicting Mortality of Geriatric Trauma Patients in Emergency Departments. J. Korean Med. Sci. 2016, 31, 2026–2032. [Google Scholar] [CrossRef] [PubMed]

| Variable | Survival Group (n = 240) | Death Group (n = 43) | p Value |
|---|---|---|---|
| Gender | 0.937 b | ||
| male (n, %) | 166 (69.17%) | 30 (69.77%) | |
| female (n, %) | 74 (30.83%) | 13 (30.23%) | |
| Age (years) | 52.9 ± 17.8 | 60.3 ± 17.5 | 0.013 a |
| Main injury site | |||
| head and neck (n, %) | 147 (61.25%) | 32 (74.42%) | 0.099 b |
| face (n, %) | 10 (4.17%) | 1 (2.33%) | 0.540 b |
| chest (n, %) | 24 (10.00%) | 4 (9.30%) | 0.887 b |
| abdomen (n, %) | 7 (2.92%) | 2 (4.65%) | 0.571 b |
| limbs and pelvis (n, %) | 47 (19.58%) | 4 (9.30%) | 0.106 b |
| body surface (n, %) | 5 (2.08%) | 0 (0.00%) | 0.436 b |
| Cause of injury | |||
| motor vehicle accident (n, %) | 163 (67.92%) | 34 (79.07%) | 0.143 b |
| fall from height (n, %) | 50 (20.83%) | 4 (9.30%) | 0.076 b |
| crushed by heavy objects (n, %) | 8 (3.33%) | 1 (2.33%) | 0.718 b |
| other reasons (n, %) | 19 (7.92%) | 4 (9.30%) | 0.763 b |
| Systolic blood pressure (mmHg) | 127 (118, 137) | 89 (76,98) | <0.001 c |
| Diastolic blood pressure (mmHg) | 77 (70, 80) | 65 (58,75) | <0.001 c |
| Mean arterial pressure (mmHg) | 93 (87, 100) | 74 (68,80) | <0.001 c |
| Pulse rate (times/min) | 84 (78, 95) | 117 (105, 134) | <0.001 c |
| The number of days in hospital | 15 (10,20) | 3 (2,5) | <0.001 c |
| Glasgow outcome scale | 5 (4, 5) | 1 (1,1) | <0.001 c |
| Types | Survival Group (n = 240) | Death Group (n = 43) | p Value |
|---|---|---|---|
| ISS | 13 (10, 17) | 21 (18, 26) | <0.001 |
| TI | 10 (9, 12) | 20 (17, 24) | <0.001 |
| SI | 0.66 (0.60, 0.76) | 1.27 (1.13, 1.60) | <0.001 |
| MSI | 0.90 (0.81, 1.05) | 1.58 (1.38, 1.82) | <0.001 |
| ASI | 34.18 (25.99, 45.71) | 81.90 (63.45, 100.62) | <0.001 |
| Predictors | Associated Criterion | Sensitivity (%) | Specificity (%) | AUC | SE | 95%CI | YI |
|---|---|---|---|---|---|---|---|
| ISS | >17.0 | 81.40 | 88.75 | 0.929 | 0.0167 | 0.892–0.956 | 0.7015 |
| TI | >16.0 | 83.72 | 91.67 | 0.932 | 0.0171 | 0.896–0.958 | 0.7539 |
| SI | >0.95 | 100.00 | 90.00 | 0.953 | 0.0116 | 0.921–0.975 | 0.9000 |
| MSI | >1.18 | 95.35 | 87.08 | 0.945 | 0.0133 | 0.911–0.968 | 0.8243 |
| ASI | >52.7 | 83.72 | 87.08 | 0.899 | 0.0272 | 0.858–0.931 | 0.7080 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dai, G.; Lu, X.; Xu, F.; Xu, D.; Li, P.; Chen, X.; Guo, F. Early Mortality Risk in Acute Trauma Patients: Predictive Value of Injury Severity Score, Trauma Index, and Different Types of Shock Indices. J. Clin. Med. 2022, 11, 7219. https://doi.org/10.3390/jcm11237219
Dai G, Lu X, Xu F, Xu D, Li P, Chen X, Guo F. Early Mortality Risk in Acute Trauma Patients: Predictive Value of Injury Severity Score, Trauma Index, and Different Types of Shock Indices. Journal of Clinical Medicine. 2022; 11(23):7219. https://doi.org/10.3390/jcm11237219
Chicago/Turabian StyleDai, Guoyang, Xin Lu, Feng Xu, Deli Xu, Pengfei Li, Xionghui Chen, and Fengbao Guo. 2022. "Early Mortality Risk in Acute Trauma Patients: Predictive Value of Injury Severity Score, Trauma Index, and Different Types of Shock Indices" Journal of Clinical Medicine 11, no. 23: 7219. https://doi.org/10.3390/jcm11237219
APA StyleDai, G., Lu, X., Xu, F., Xu, D., Li, P., Chen, X., & Guo, F. (2022). Early Mortality Risk in Acute Trauma Patients: Predictive Value of Injury Severity Score, Trauma Index, and Different Types of Shock Indices. Journal of Clinical Medicine, 11(23), 7219. https://doi.org/10.3390/jcm11237219






