Three-Dimensional Automated, Machine-Learning-Based Left Heart Chamber Metrics: Associations with Prevalent Vascular Risk Factors and Cardiovascular Diseases
Abstract
:1. Introduction
2. Materials and Methods
2.1. Echocardiographic Data
2.2. Definition of Vascular Risk Factors and Cardiovascular Disease
2.3. Reproducibility
2.4. Statistical Analysis
3. Results
3.1. Population Characteristics
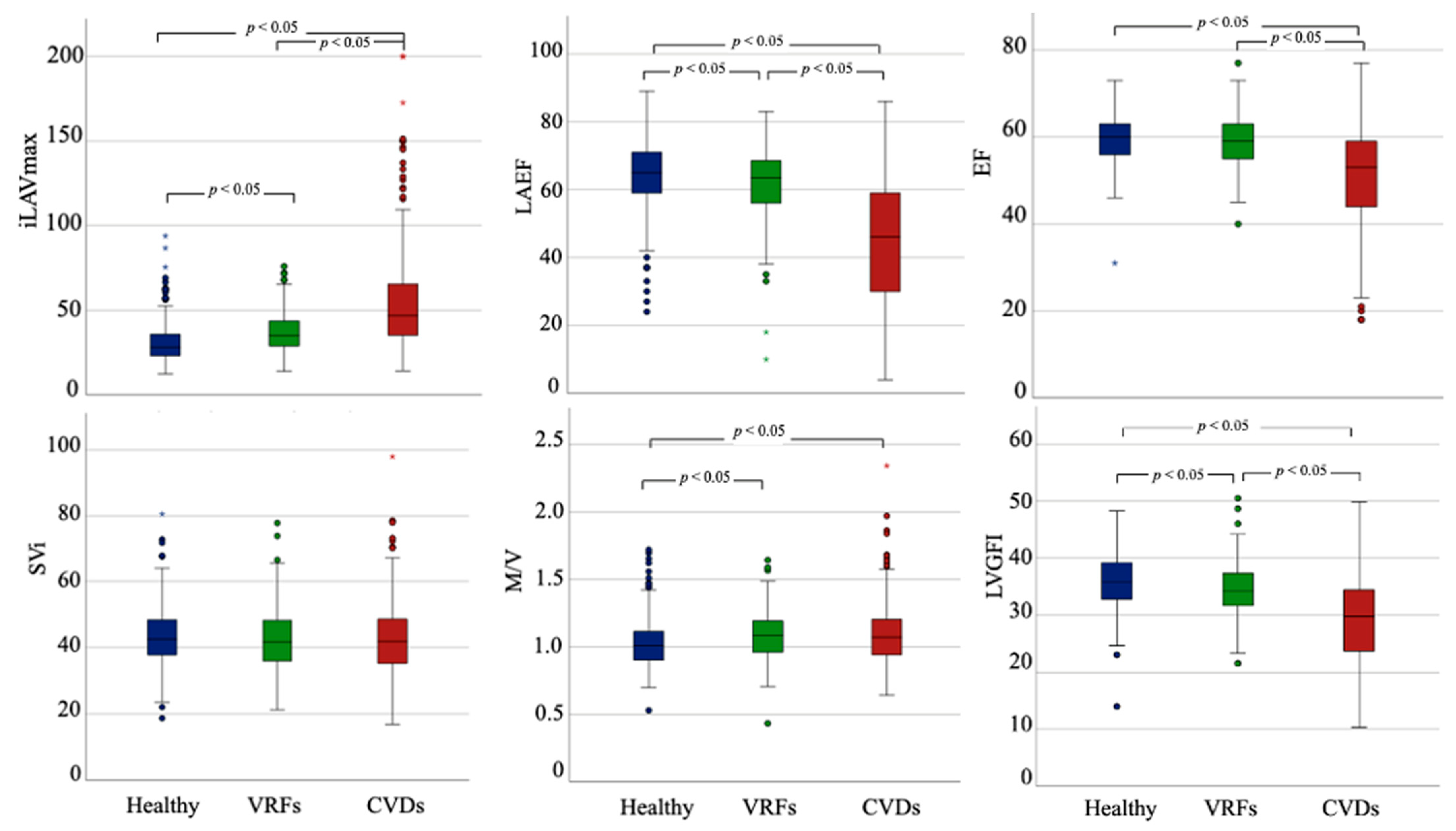
3.2. DHM Metrics According to the Presence of VRFs and CVDs
3.3. Reliability Analysis
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yuan, N.; Jain, I.; Rattehalli, N.; He, B.; Pollick, C.; Liang, D.; Heidenreich, P.; Zou, J.; Cheng, S.; Ouyang, D. Systematic Quantification of Sources of Variation in Ejection Fraction Calculation Using Deep Learning. JACC Cardiovasc. Imaging 2021, 14, 2260–2262. [Google Scholar] [CrossRef] [PubMed]
- NAjmone Marsan, N.; Michalski, B.; Cameli, M.; Podlesnikar, T.; Manka, R.; Sitges, M.; Dweck, M.R.; Haugaa, K.H. EACVI survey on standardization of cardiac chambers quantification by transthoracic echocardiography. Eur. Hear. J. Cardiovasc. Imaging 2020, 21, 119–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nolan, M.T.; Thavendiranathan, P. Automated Quantification in Echocardiography. JACC Cardiovasc. Imaging 2019, 12, 1073–1092. [Google Scholar] [CrossRef] [PubMed]
- Tsang, W.; Salgo, I.S.; Medvedofsky, D.; Takeuchi, M.; Prater, D.; Weinert, L.; Yamat, M.; Mor-Avi, V.; Patel, A.R.; Lang, R.M. Transthoracic 3D Echocardiographic Left Heart Chamber Quantification Using an Automated Adaptive Analytics Algorithm. JACC Cardiovasc. Imaging 2016, 9, 769–782. [Google Scholar] [CrossRef]
- Tamborini, G.; Piazzese, C.; Lang, R.M.; Muratori, M.; Chiorino, E.; Mapelli, M.; Fusini, L.; Ali, S.G.; Gripari, P.; Pontone, G.; et al. Feasibility and Accuracy of Automated Software for Transthoracic Three-Dimensional Left Ventricular Volume and Function Analysis: Comparisons with Two-Dimensional Echocardiography, Three-Dimensional Transthoracic Manual Method, and Cardiac Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 1049–1058. [Google Scholar]
- Medvedofsky, D.; Mor-Avi, V.; Amzulescu, M.; Fernández-Golfin, C.; Hinojar, R.; Monaghan, M.J.; Otani, K.; Reiken, J.; Takeuchi, M.; Tsang, W.; et al. Three-dimensional echocardiographic quantification of the left-heart chambers using an automated adaptive analytics algorithm: Multicentre validation study. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 47–58. [Google Scholar] [CrossRef] [Green Version]
- Narang, A.; Mor-Avi, V.; Prado, A.; Volpato, V.; Prater, D.; Tamborini, G.; Fusini, L.; Pepi, M.; Goyal, N.; Addetia, K.; et al. Machine learning based automated dynamic quantification of left heart chamber volumes. Eur. Hear. J.-Cardiovasc. Imaging 2019, 20, 541–549. [Google Scholar] [CrossRef]
- Italiano, G.; Tamborini, G.; Fusini, L.; Mantegazza, V.; Doldi, M.; Celeste, F.; Gripari, P.; Muratori, M.; Lang, R.M.; Pepi, M. Feasibility and Accuracy of the Automated Software for Dynamic Quantification of Left Ventricular and Atrial Volumes and Function in a Large Unselected Population. J. Clin. Med. 2021, 10, 5030. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American society of echocardiography and the European association of cardiovascular imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Mitchell, C.; Rahko, P.S.; Blauwet, L.A.; Canaday, B.; Finstuen, J.A.; Foster, M.C.; Horton, K.; Ogunyankin, K.O.; Palma, R.A.; Velazquez, E.J. Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2018, 32, 1–64. [Google Scholar] [CrossRef]
- Barbieri, A.; Bursi, F.; Camaioni, G.; Maisano, A.; Imberti, J.F.; Albini, A.; De Mitri, G.; Mantovani, F.; Boriani, G. Echocardiographic Left Ventricular Mass Assessment: Correlation between 2D-Derived Linear Dimensions and 3-Dimensional Automated, Machine Learning-Based Methods in Unselected Patients. J. Clin. Med. 2021, 10, 1279. [Google Scholar] [CrossRef] [PubMed]
- Volpato, V.; Mor-Avi, V.; Narang, A.; Prater, D.; Gonçalves, A.; Tamborini, G.; Fusini, L.; Pepi, M.; Patel, A.R.; Lang, R.M. Automated, machine learning-based, 3D echocardiographic quantification of left ventricular mass. Echocardiography 2019, 36, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Mewton, N.; Opdahl, A.; Choi, E.Y.; Almeida, A.L.; Kawel, N.; Wu, C.O.; Burke, G.L.; Liu, S.; Liu, K.; Bluemke, D.A.; et al. Left ventricular global function index by magnetic resonance imaging—A novel marker for assessment of cardiac performance for the prediction of cardiovascular events: The multi-ethnic study of atherosclerosis. Hypertension 2013, 61, 770–778. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schober, A.L.; Jungbauer, C.; Poschenrieder, F.; Schober, A.D.; Hubauer, U.; Keyser, A.; Fredersdorf-Hahn, S.; Debl, K.; Maier, L.S.; Sossalla, S.; et al. Cardiac MRI Based Left Ventricular Global Function Index: Association with Disease Severity in Patients with ICD for Secondary Prevention. J. Clin. Med. 2021, 10, 4980. [Google Scholar] [CrossRef]
- Liu, T.; Zhou, Z.; Bo, K.; Gao, Y.; Wang, H.; Wang, R.; Liu, W.; Chang, S.; Liu, Y.; Sun, Y.; et al. Association Between Left Ventricular Global Function Index and Outcomes in Patients with Dilated Cardiomyopathy. Front. Cardiovasc. Med. 2021, 8, 751907. [Google Scholar] [CrossRef]
- Nwabuo, C.C.; Moreira, H.T.; Vasconcellos, H.D.; Mewton, N.; Opdahl, A.; O Ogunyankin, K.; Ambale-Venkatesh, B.; Schreiner, P.J.; Armstrong, A.A.C.; E Lewis, C.; et al. Left ventricular global function index predicts incident heart failure and cardiovascular disease in young adults: The coronary artery risk development in young adults (CARDIA) study. Eur. Hear. J.-Cardiovasc. Imaging 2019, 20, 533–540. [Google Scholar] [CrossRef]
- Thomas, L.; Muraru, D.; Popescu, B.A.; Sitges, M.; Rosca, M.; Pedrizzetti, G.; Henein, M.Y.; Donal, E.; Badano, L.P. Evaluation of Left Atrial Size and Function: Relevance for Clinical Practice. J. Am. Soc. Echocardiogr. 2020, 33, 934–952. [Google Scholar] [CrossRef]
- Polovina, M.M.; Coats, A.; Seferovic, P. Is left atrium the best kept secret of the heart? Left atrial dilatation and cardiovascular outcomes. Heart 2019, 105, 1848–1849. [Google Scholar] [CrossRef]
- Coats, A.J.S.; Heymans, S.; Farmakis, D.; Anker, S.D.; Backs, J.; Bauersachs, J.; A de Boer, R.; Čelutkienė, J.; Cleland, J.G.F.; Dobrev, D.; et al. Atrial disease and heart failure: The common soil hypothesis proposed by the Heart Failure Association of the European Society of Cardiology. Eur. Hear. J. 2021, 43, 863–867. [Google Scholar] [CrossRef]
- Froehlich, L.; Meyre, P.; Aeschbacher, S.; Blum, S.; Djokic, D.; Kühne, M.; Osswald, S.; Kaufmann, B.; Conen, D. Left atrial dimension and cardiovascular outcomes in patients with and without atrial fibrillation: A systematic review and meta-analysis. Heart 2019, 105, 1884–1891. [Google Scholar] [CrossRef] [Green Version]
- Inciardi, R.M.; Claggett, B.; Minamisawa, M.; Shin, S.-H.; Selvaraj, S.; Gonçalves, A.; Wang, W.; Kitzman, D.; Matsushita, K.; Prasad, N.G.; et al. Association of Left Atrial Structure and Function With Heart Failure in Older Adults. J. Am. Coll. Cardiol. 2022, 79, 1549–1561. [Google Scholar] [CrossRef] [PubMed]
- Tsang, M.Y.C.; Barnes, M.E.; Tsang, T.S.M. Left atrial volume: Clinical value revisited. Curr. Cardiol. Rep. 2012, 14, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Smiseth, O.A.; Morris, D.A.; Cardim, N.; Cikes, M.; Delgado, V.; Donal, E.; Flachskampf, F.A.; Galderisi, M.; Gerber, B.L.; Gimelli, A.; et al. Multimodality imaging in patients with heart failure and preserved ejection fraction: An expert consensus document of the European Association of Cardiovascular Imaging. Eur. Hear. J. Cardiovasc. Imaging 2022, 23, e34–e61. [Google Scholar] [CrossRef]
- Russo, C.; Jin, Z.; Homma, S.; Rundek, T.; Elkind, M.S.V.; Sacco, R.L.; Di Tullio, M.R. Left atrial minimum volume and reservoir function as correlates of left ventricular diastolic function: Impact of left ventricular systolic function. Heart 2012, 98, 813–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedberg, P.; Selmeryd, J.; Leppert, J.; Henriksen, E. Left atrial minimum volume is more strongly associated with N-terminal pro-B-type natriuretic peptide than the left atrial maximum volume in a community-based sample. Int. J. Cardiovasc. Imaging 2016, 32, 417–425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shin, S.-H.; Jang, J.-H.; Baek, Y.-S.; Kwon, S.-W.; Park, S.-D.; Woo, S.-I.; Kim, D.-H.; Kwan, J. Prognostic Impact of Left Atrial Minimal Volume on Clinical Outcome in Patients with Non-Obstructive Hypertrophic Cardiomyopathy. Int. Heart J. 2018, 59, 991–995. [Google Scholar] [CrossRef] [Green Version]
- Huynh, Q.L.; Kalam, K.; Iannaccone, A.; Negishi, K.; Thomas, L.; Marwick, T.H. Functional and Anatomic Responses of the Left Atrium to Change in Estimated Left Ventricular Filling Pressure. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 2015, 28, 1428–1433.e1. [Google Scholar] [CrossRef]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 1321–1360. [Google Scholar] [CrossRef]
- Badano, L.P.; Miglioranza, M.H.; Mihăilă, S.; Peluso, D.; Xhaxho, J.; Marra, M.P.; Cucchini, U.; Soriani, N.; Iliceto, S.; Muraru, D. Left Atrial Volumes and Function by Three-Dimensional Echocardiography: Reference Values, Accuracy, Reproducibility, and Comparison With Two-Dimensional Echocardiographic Measurements. Circ. Cardiovasc. Imaging 2016, 9, e004229. [Google Scholar] [CrossRef] [Green Version]
- Raisi-Estabragh, Z.; McCracken, C.; Condurache, D.-G.; Aung, N.; Vargas, J.D.; Naderi, H.; Munroe, P.B.; Neubauer, S.; Harvey, N.C.; E Petersen, S. Left atrial structure and function are associated with cardiovascular outcomes independent of left ventricular measures: A UK Biobank CMR study. Eur. Hear. J. Cardiovasc. Imaging 2022, 23, 1191–1200. [Google Scholar] [CrossRef]
- Inoue, Y.Y.; Alissa, A.; Khurram, I.M.; Fukumoto, K.; Habibi, M.; Venkatesh, B.A.; Zimmerman, S.L.; Nazarian, S.; Berger, R.D.; Calkins, H.; et al. Quantitative tissue-tracking cardiac magnetic resonance (CMR) of left atrial deformation and the risk of stroke in patients with atrial fibrillation. J. Am. Hear. Assoc. 2015, 4, e001844. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Zhang, X.; Leng, W.; Lei, X.; Chen, L.; Liang, Z.; Wang, J. Left atrium passive ejection fraction is the most sensitive index of type 2 diabetes mellitus-related cardiac changes. Int. J. Cardiovasc. Imaging 2018, 34, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Graça, B.; Ferreira, M.J.; Donato, P.; Gomes, L.; Castelo-Branco, M.; Caseiro-Alves, F. Left atrial dysfunction in type 2 diabetes mellitus: Insights from cardiac MRI. Eur. Radiol. 2014, 24, 2669–2676. [Google Scholar] [CrossRef] [Green Version]
- Petersen, S.E.; Sanghvi, M.M.; Aung, N.; Cooper, J.A.; Paiva, J.M.; Zemrak, F.; Fung, K.; Lukaschuk, E.; Lee, A.M.; Carapella, V.; et al. The impact of cardiovascular risk factors on cardiac structure and function: Insights from the UK Biobank imaging enhancement study. PLoS ONE 2017, 12, e0185114. [Google Scholar] [CrossRef] [Green Version]
- Jensen, M.T.; Fung, K.; Aung, N.; Sanghvi, M.M.; Chadalavada, S.; Paiva, J.M.; Khanji, M.Y.; de Knegt, M.C.; Lukaschuk, E.; Lee, A.M.; et al. Changes in Cardiac Morphology and Function in Individuals With Diabetes Mellitus: The UK Biobank Cardiovascular Magnetic Resonance Substudy. Circ. Cardiovasc. Imaging 2019, 12, e009476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Packer, M. Heart Failure With a Mid-Range Ejection Fraction: A Disorder That a Psychiatrist Would Love. JACC Heart Fail. 2017, 5, 805–807. [Google Scholar] [CrossRef]
- McComb, C.; Berry, C. Prognostic importance of a new measure of global systolic heart function in healthy adults. Hypertension 2013, 61, 762–764. [Google Scholar] [CrossRef] [Green Version]
- Reinstadler, S.J.; Klug, G.; Feistritzer, H.-J.; Kofler, M.; Pernter, B.; Göbel, G.; Henninger, B.; Müller, S.; Franz, W.-M.; Metzler, B. Prognostic value of left ventricular global function index in patients after ST-segment elevation myocardial infarction. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 169–176. [Google Scholar] [CrossRef] [Green Version]
- Pezel, T.; Horts, T.B.D.; Schaaf, M.; Croisille, P.; Bière, L.; Garcia-Dorado, D.; Jossan, C.; Roubille, F.; Cung, T.-T.; Prunier, F.; et al. Predictive value of early cardiac magnetic resonance imaging functional and geometric indexes for adverse left ventricular remodelling in patients with anterior ST-segment elevation myocardial infarction: A report from the CIRCUS study. Arch. Cardiovasc. Dis. 2020, 113, 710–720. [Google Scholar] [CrossRef]
- Huang, S.; Xu, H.-Y.; Diao, K.-Y.; Shi, K.; He, Y.; He, S.; Zhang, Y.; Gao, Y.; Shen, M.-T.; Guo, Y.-K.; et al. Left ventricular global function index by magnetic resonance imaging—A novel marker for differentiating cardiac amyloidosis from hypertrophic cardiomyopathy. Sci. Rep. 2020, 10, 4707. [Google Scholar] [CrossRef] [Green Version]
- Barletta, V.; Hinojar, R.; Carbonell, A.; González-Gómez, A.; Fabiani, I.; Di Bello, V.; Jiménez-Nacher, J.J.; Zamorano, J.; Fernández-Golfín, C. Three-dimensional full automated software in the evaluation of the left ventricle function: From theory to clinical practice. Int. J. Cardiovasc. Imaging 2018, 34, 1205–1213. [Google Scholar] [CrossRef] [PubMed]
- Addetia, K.; Miyoshi, T.; Amuthan, V.; Citro, R.; Daimon, M.; Fajardo, P.G.; Kasliwal, R.R.; Kirkpatrick, J.N.; Monaghan, M.J.; Muraru, D.; et al. Normal Values of Left Ventricular Size and Function on Three-Dimensional Echocardiography: Results of the World Alliance Societies of Echocardiography Study. J. Am. Soc. Echocardiogr. 2022, 35, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Singulane, C.C.; Miyoshi, T.; Prado, A.D.; Addetia, K.; Bellino, M.; Daimon, M.; Fajardo, P.G.; Kasliwal, R.R.; Kirkpatrick, J.N.; et al. Normal Values of Left Atrial Size and Function and the Impact of Age: Results of the World Alliance Societies of Echocardiography Study. J. Am. Soc. Echocardiogr. 2022, 35, 154–164.e3. [Google Scholar] [CrossRef] [PubMed]
- Kawel-Boehm, N.; Hetzel, S.J.; Ambale-Venkatesh, B.; Captur, G.; Francois, C.J.; Jerosch-Herold, M.; Salerno, M.; Teague, S.D.; Valsangiacomo-Buechel, E.; van der Geest, R.J.; et al. Reference ranges (‘normal values’) for cardiovascular magnetic resonance (CMR) in adults and children: 2020 update. J. Cardiovasc. Magn. Reson. 2020, 22, 87. [Google Scholar] [CrossRef]
- Chuang, M.L.; Gona, P.; Hautvast, G.L.; Salton, C.J.; Blease, S.J.; Yeon, S.B.; Breeuwer, M.; O’Donnell, C.J.; Manning, W.J. Correlation of trabeculae and papillary muscles with clinical and cardiac characteristics and impact on CMR measures of LV anatomy and function. JACC Cardiovasc. Imaging 2012, 5, 1115–1123. [Google Scholar] [CrossRef] [Green Version]
- Patel, H.N.; Miyoshi, T.; Addetia, K.; Henry, M.P.; Citro, R.; Daimon, M.; Fajardo, P.G.; Kasliwal, R.R.; Kirkpatrick, J.N.; Monaghan, M.J.; et al. Normal Values of Cardiac Output and Stroke Volume According to Measurement Technique, Age, Sex, and Ethnicity: Results of the World Alliance of Societies of Echocardiography Study. J. Am. Soc. Echocardiogr. Off. Publ. Am. Soc. Echocardiogr. 2021, 34, 1077–1085.e1. [Google Scholar] [CrossRef]
- Wu, V.C.-C.; Kitano, T.; Chu, P.-H.; Takeuchi, M. Left ventricular volume and ejection fraction measurements by fully automated 3D echocardiography left chamber quantification software versus CMR: A systematic review and meta-analysis. J. Cardiol. 2023, 81, 19–25. [Google Scholar] [CrossRef]
- Nicol, P.; Rank, A.; Lenz, T.; Schürmann, F.; Syryca, F.; Trenkwalder, T.; Reinhard, W.; Adolf, R.; Hadamitzky, M.; Kastrati, A.; et al. Echocardiographic evaluation of left ventricular function using an automated analysis algorithm is feasible for beginners and experts: Comparison with invasive and non-invasive methods. J. Echocardiogr. 2022. [Google Scholar] [CrossRef]

| Men (n = 528; 49.4%) | Women (n = 541; 50.6%) | Total (n = 1069) | p-Value | |
|---|---|---|---|---|
| Age (years), median (IQR) | 63 (49–74) | 61 (49–73) | 62 (49–74) | 0.18 |
| Weight (Kg), median (IQR) | 78 (70–88) | 64 (57–72) | 70 (62–82) | <0.001 |
| Height (cm), median (IQR) | 174 (169–180) | 161 (158–165) | 167 (150–175) | <0.001 |
| BMI (Kg/m2) | 25.7 (23.5–28.4) | 24.7 (21.6–27.7) | 25.2 (22.3–28.1) | <0.001 |
| Hypertension, n (%) | 217/528 (41.1) | 179/541 (33.1) | 396/1069 (37.0) | 0.007 |
| Diabetes, n (%) | 73/528 (13.8) | 43/541 (7.9) | 116/1069 (10.9) | 0.002 |
| Coronary artery disease, n (%) | 121/528 (22.9) | 36/541 (6.7) | 157/1069 (14.7) | <0.001 |
| DCM, n (%) | 48/528 (9.1) | 30/541 (5.5) | 78/1069 (7.3) | 0.02 |
| Acute heart failure, n (%) | 28/528 (5.3) | 17/541 (3.1) | 45/1069 (4.2) | 0.08 |
| HCM, n (%) | 31/528 (5.9) | 13/541 (2.4) | 44/1069 (4.1) | 0.004 |
| Valvular heart disease, n (%) | 86/528 (16.3) | 82/541 (15.2) | 168/1069 (15.7) | 0.61 |
| Moderate/severe MR n (%) | 31/528 (6.1) | 23/541 (4.3) | 55/1069 (5.1) | 0.18 |
| Moderate/severe AR n (%) | 19/527 (3.6) | 12/541 (2.2) | 31/1069 (2.9) | 0.17 |
| Moderate/severe AS n (%) | 12/528 (2.3) | 13/539 (2.4) | 25/1069 (2.3) | 0.88 |
| Moderate/severe TR n (%) | 12/528 (2.3) | 24/541 (4.4) | 36/1069 (3.4) | 0.05 |
| Atrial fibrillation, n (%) | 106/528 (20.1) | 65/541 (12.0) | 171/1069 (16.0) | <0.001 |
| Pericarditis/myocarditis, n (%) | 10/528 (1.9) | 8/541 (1.5) | 18/1069 (1.7) | 0.59 |
| Previous PE, n (%) | 12/528 (2.3) | 16/541 (3.0) | 28/1069 (2.6) | 0.48 |
| COPD, n (%) | 21/528 (4.0) | 12/541 (2.2) | 33/1069 (3.1) | 0.09 |
| Previous stroke/TIA, n (%) | 27/528 (5.1) | 17/541 (3.1) | 44/1069 (4.1) | 0.11 |
| Previous CHT, n (%) | 74/528 (14.0) | 162/541 (29.9) | 236/1069 (22.1) | <0.001 |
| Malignancy (prior or active), n (%) | 138/528 (26.1) | 240/541 (44.4) | 378/1069 (35.4) | <0.001 |
| Liver disease, n (%) | 32/528 (6.1) | 12/541 (2.2) | 44/1069 (4.1) | 0.002 |
| Echocardiographic Parameters | Total n = 1069 | Healthy Subjects (n = 396; 37%) | VRFs Patients (n = 190, 17.8%) | CVDs Patients (n = 483, 45.2%) | p-Value * |
|---|---|---|---|---|---|
| Frame rate (Hz), median (IQR) | 20 (16–22) | 21 (20–22) | 21 (20–22) | 20 (16–21) | <0.001 |
| EDVi 3D, mL/m2, median (IQR) | 74.6 [63.7–87.6] | 71.8 [63.2–81.9] | 70.1 [59.8–81.0] | 80.6 [66.9–99.5] | <0.001 |
| ESVi 3D, mL/m2, median (IQR) | 30.8 [25-0-39.5] | 28.7 [24.5–33.6] | 27.9 [23.1–33.7] | 37.1 [27.5–54.2] | <0.001 |
| LVEF 3D (%), median (IQR) | 58 [53–62] | 60 [56–63] | 60 [56–63] | 54 [44–59] | <0.001 |
| LAEF 3D (%), median (IQR) | 59 [46–67] | 65 [59–71] | 64 [57–69] | 47 [30–59] | <0.001 |
| LV mass/m2, median (IQR) | 77.9 [67.0–92.2] | 70.8 [63.3–81.7] | 74.5 [64.1–87.3] | 87.7 [74.3–101.8] | <0.001 |
| LAVi, max (mL/m2), median (IQR) | 35.8 [27.2–49.7] | 28.2 [23.2–35.9] | 34.9 [29.0–43.4] | 46.8 [34.7–65.5] | <0.001 |
| LAVi min (mL/m2) median (IQR) | 13.9 [9.5–24.8] | 9.9 [7.5–13.5] | 12.3 [9.8–17.2] | 24.4 [14.7–43.7] | <0.001 |
| SVi (mL/m2) median (IQR) | 42.1 [36.2–48.3] | 42.9 [37.9–48.5] | 41.4 [35.5–47.4] | 42.3 [37.3–48.2] | 0.072 |
| LVGFI, median (IQR) | 33.6 [29.0–37.4] | 35.9 [32.8–39.3] | 34.4 [32.0–37.5] | 29.7 [23.8–34.6] | <0.001 |
| LVM/LVEDV ratio (g/mL), median (IQR) | 1.05 [0.93–1.17] | 1.01 [0.90–1.11] | 1.08 [0.96–1.19] | 1.07 [0.93–1.20] | <0.001 |
| Echocardiographic Parameters | 3D-DHM (n = 396) | WASES [42,43] | SCMR [44] | |||
|---|---|---|---|---|---|---|
| Men (n = 150, 37.9%) | Women (n = 246, 62.1%) | Men | Women | Men | Women | |
| EDVi, mL/m2, m ± SD) | 80.4 ± 14.3 | 68.2 ± 12.0 | 70 ± 15 § | 65 ± 12 § | 77 ± 15 * | 69 ± 12 * |
| ESVi, mL/m2 m ± SD) | 33.6 ± 7.3 | 26.9 ± 5.9 | 26 ± 8 § | 28 ± 7 § | 29 ± 9 * | 24 ± 7 * |
| LVEF (%), m ± SD | 58.3 ± 4.3 | 60.7 ± 4.9 | 60 ± 5 § | 62 ± 5 § | 63 ± 6 | 66 ± 7 |
| LAEF (%), m ± SD | 64.4 ± 9.0 | 64.2 ± 9.1 | 61.8 ± 7.6 ¶ | 62.6 ± 7.7 ¶ | 54 + 8 ° | 57 + 6 ° |
| LV mass/m2, m ± SD | 81.1 ± 15.2 | 69.2 ± 12.9 | -- | -- | 56 ± 10 * | 45 ± 7 * |
| LAVi, max (mL/m2), m ± SD | 33.7 ± 13.8 | 29 ± 8.8 | 28.1 ± 7.1 ¶ | 28 ± 6.7 ¶ | 41 ± 8 ° | 44 ± 8 ° |
| LAVi min (mL/m2), m ± SD | 12.5 ± 7.4 | 10.5 ± 4.6 | 10.8 ± 3.7 ¶ | 10.5 ± 3.7 ¶ | 19 ± 5 ° | 19 ± 5 ° |
| SVi (mL/m2), m ± SD | 47 ± 8.8 | 41.4 ± 8.3 | 42 ± 9 § | 41 ± 8 § | 48 + 9 # | 45 + 7 # |
| LVM/LVEDV ratio (g/mL), m ± SD | 1.01 ± 0.16 | 1.02 ± 0.17 | -- | -- | 0.7 ± 0.2 * | 0.7 ± 0.1 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbieri, A.; Albini, A.; Chiusolo, S.; Forzati, N.; Laus, V.; Maisano, A.; Muto, F.; Passiatore, M.; Stuani, M.; Torlai Triglia, L.; et al. Three-Dimensional Automated, Machine-Learning-Based Left Heart Chamber Metrics: Associations with Prevalent Vascular Risk Factors and Cardiovascular Diseases. J. Clin. Med. 2022, 11, 7363. https://doi.org/10.3390/jcm11247363
Barbieri A, Albini A, Chiusolo S, Forzati N, Laus V, Maisano A, Muto F, Passiatore M, Stuani M, Torlai Triglia L, et al. Three-Dimensional Automated, Machine-Learning-Based Left Heart Chamber Metrics: Associations with Prevalent Vascular Risk Factors and Cardiovascular Diseases. Journal of Clinical Medicine. 2022; 11(24):7363. https://doi.org/10.3390/jcm11247363
Chicago/Turabian StyleBarbieri, Andrea, Alessandro Albini, Simona Chiusolo, Nicola Forzati, Vera Laus, Anna Maisano, Federico Muto, Matteo Passiatore, Marco Stuani, Laura Torlai Triglia, and et al. 2022. "Three-Dimensional Automated, Machine-Learning-Based Left Heart Chamber Metrics: Associations with Prevalent Vascular Risk Factors and Cardiovascular Diseases" Journal of Clinical Medicine 11, no. 24: 7363. https://doi.org/10.3390/jcm11247363
APA StyleBarbieri, A., Albini, A., Chiusolo, S., Forzati, N., Laus, V., Maisano, A., Muto, F., Passiatore, M., Stuani, M., Torlai Triglia, L., Vitolo, M., Ziveri, V., & Boriani, G. (2022). Three-Dimensional Automated, Machine-Learning-Based Left Heart Chamber Metrics: Associations with Prevalent Vascular Risk Factors and Cardiovascular Diseases. Journal of Clinical Medicine, 11(24), 7363. https://doi.org/10.3390/jcm11247363






