Central versus Peripheral Postcardiotomy Veno-Arterial Extracorporeal Membrane Oxygenation: Systematic Review and Individual Patient Data Meta-Analysis
Abstract
:1. Introduction
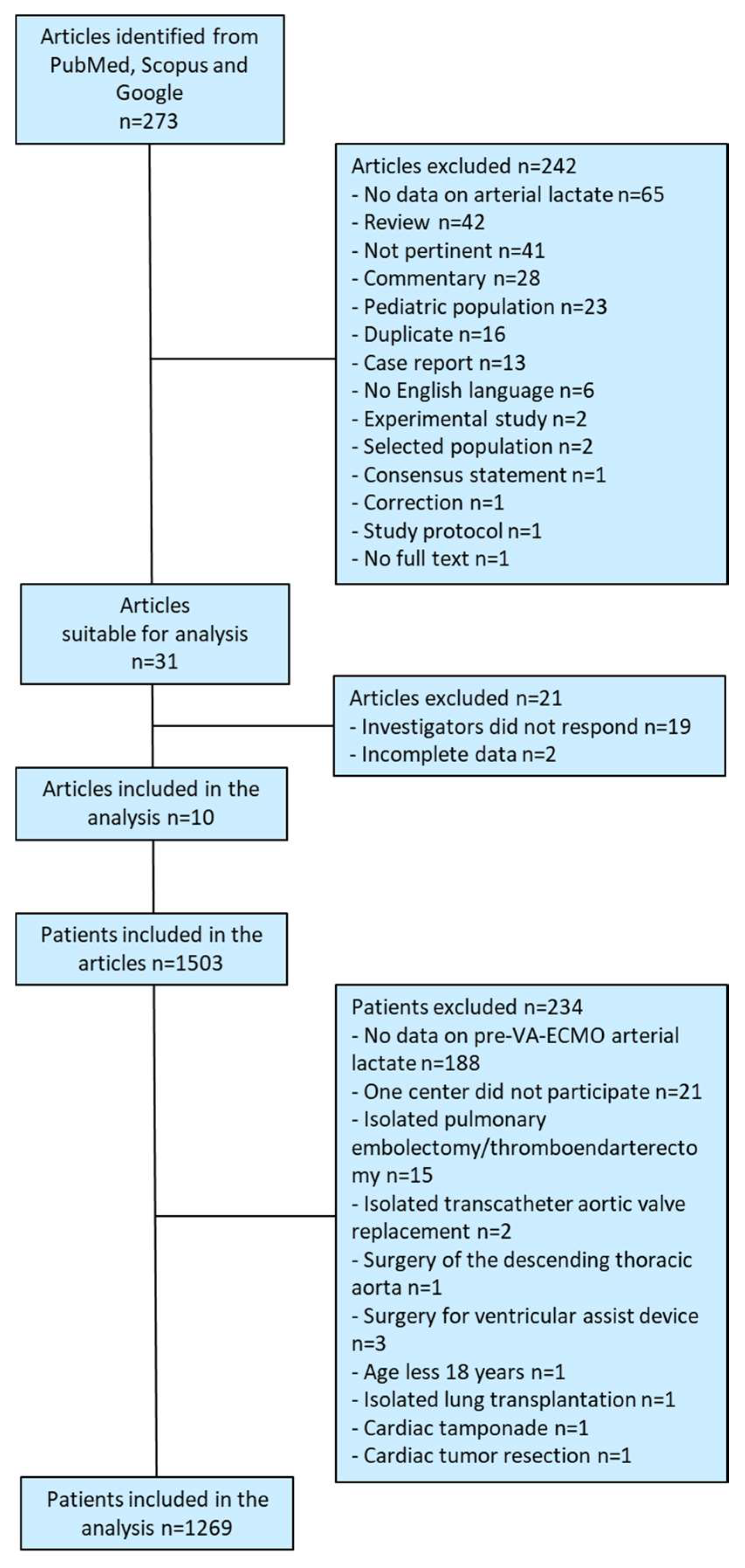
2. Methods
Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kowalewski, M.; Zieliński, K.; Brodie, D.; MacLaren, G.; Whitman, G.; Raffa, G.M.; Boeken, U.; Shekar, K.; Chen, Y.S.; Bermudez, C.; et al. Venoarterial extracorporeal membrane oxygenation for postcardiotomy shock-analysis of the extracorporeal life support organization registry. Crit. Care Med. 2021, 49, 1107–1117. [Google Scholar] [CrossRef]
- Biancari, F.; Dalén, M.; Fiore, A.; Ruggieri, V.G.; Saeed, D.; Jónsson, K.; Gatti, G.; Zipfel, S.; Perrotti, A.; Bounader, K.; et al. Multicenter study on postcardiotomy venoarterial extracorporeal membrane oxygenation. J. Thorac. Cardiovasc. Surg. 2020, 159, 1844–1854. [Google Scholar] [CrossRef]
- Biancari, F.; Perrotti, A.; Dalén, M.; Guerrieri, M.; Fiore, A.; Reichart, D.; Dell’Aquila, A.M.; Gatti, G.; Ala-Kokko, T.; Kinnunen, E.M.; et al. Meta-analysis of the outcome after postcardiotomy venoarterial extracorporeal membrane oxygenation in adult patients. J. Cardiothorac. Vasc. Anesth. 2018, 32, 1175–1182. [Google Scholar] [CrossRef] [Green Version]
- Bowles, C.; Hiesinger, W. Postcardiotomy shock extracorporeal membrane oxygenation: Peripheral or central? JTCVS Open 2021, 8, 66–69. [Google Scholar] [CrossRef]
- Mariscalco, G.; Salsano, A.; Fiore, A.; Dalén, M.; Ruggieri, V.G.; Saeed, D.; Jónsson, K.; Gatti, G.; Zipfel, S.; Dell’Aquila, A.M.; et al. Peripheral versus central extracorporeal membrane oxygenation for postcardiotomy shock: Multicenter registry, systematic review, and meta-analysis. J. Thorac. Cardiovasc. Surg. 2020, 160, 1207–1216.e44. [Google Scholar] [CrossRef]
- Raffa, G.M.; Kowalewski, M.; Brodie, D.; Ogino, M.; Whitman, G.; Meani, P.; Pilato, M.; Arcadipane, A.; Delnoij, T.; Natour, E.; et al. Meta-analysis of peripheral or central extracorporeal membrane oxygenation in postcardiotomy and non-postcardiotomy shock. Ann. Thorac. Surg. 2019, 107, 311–321. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Menon, P.R.; Flo Forner, A.; Marin-Cuartas, M.; Lehmann, S.; Saeed, D.; Ginther, A.; Borger, M.A.; Ender, J. 30-Day perioperative mortality following venoarterial extracorporeal membrane oxygenation for postcardiotomy cardiogenic shock in patients with normal preoperative ejection fraction. Interact. Cardiovasc. Thorac. Surg. 2021, 32, 817–824. [Google Scholar] [CrossRef]
- Saha, A.; Kurlansky, P.; Ning, Y.; Sanchez, J.; Fried, J.; Witer, L.J.; Kaku, Y.; Takayama, H.; Naka, Y.; Takeda, K. Early venoarterial extracorporeal membrane oxygenation improves outcomes in post-cardiotomy shock. J. Artif. Organs 2021, 24, 7–14. [Google Scholar] [CrossRef]
- Rastan, A.J.; Dege, A.; Mohr, M.; Doll, N.; Falk, V.; Walther, T.; Mohr, F.W. Early and late outcomes of 517 consecutive adult patients treated with extracorporeal membrane oxygenation for refractory postcardiotomy cardiogenic shock. J. Thorac. Cardiovasc. Surg. 2010, 139, 302–311. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 1 October 2022).
- Al-Kawaz, M.; Shou, B.; Prokupets, R.; Whitman, G.; Geocadin, R.; Cho, S.M. Mild hypothermia and neurologic outcomes in patients undergoing venoarterial extracorporeal membrane oxygenation. J. Card. Surg. 2022, 37, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Alhijab, F.A.; Tantawy, T.M.; Ismail, H.H.; AlBarrak, M.; Adam, A.I.; Belghith, M.; Hassan, E.; Pragliola, C.; Albabtain, M.A.; Arafat, A.A. Venoarterial extracorporeal membrane oxygenation for postcardiotomy cardiogenic shock: The impact of cannulation strategy on survival. Perfusion, 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Fernandez-Gatta, M.; Merchan-Gomez, S.; Gonzalez-Cebrian, M.; Diego-Nieto, A.; Alzola, E.; Toranzo-Nieto, I.; Barrio, A.; Martin-Herrero, F.; Sanchez, P.L. Levosimendan in veno-arterial extracorporeal membrane oxygenator supported patients: Impact on the success of weaning and survival. Artif. Organs 2021, 45, 717–725. [Google Scholar] [CrossRef]
- Djordjevic, I.; Deppe, A.-C.; Sabashnikov, A.; Kuhn, E.; Eghbalzadeh, K.; Merkle, J.; Gerfer, S.; Gaisendrees, C.; Ivanov, B.; Moellenbeck, L.; et al. Concomitant ECMO and IABP support in postcardiotomy cardiogenic shock patients. Heart Lung Circ. 2021, 30, 1533–1539. [Google Scholar] [CrossRef]
- Hernández-Pérez, F.J.; Álvarez-Avelló, J.M.; Forteza, A.; Gómez-Bueno, M.; González, A.; López-Ibor, J.V.; Silva-Melchor, L.; Goicolea, J.; Martín, C.E.; Iranzo, R.; et al. Initial outcomes of a multidisciplinary network for the care of patients with cardiogenic shock. Rev. Esp. Cardiol. 2021, 74, 33–43. [Google Scholar] [CrossRef]
- L’Acqua, C.; De Tisi, C.; Lerva, G.; Ballotta, A. Postcardiotomy VA ECMO in adult patients: Italian single center experience in 2021. Int. J. Artif. Organs 2022, 45, 799–800. [Google Scholar] [CrossRef]
- Laimoud, M.; Alanazi, M. The clinical significance of blood lactate levels in evaluation of adult patients with veno-arterial extracorporeal membrane oxygenation. Egypt. Hear. J. 2020, 72, 74. [Google Scholar] [CrossRef]
- Sahli, S.D.; Kaserer, A.; Braun, J.; Halbe, M.; Dahlem, Y.; Spahn, M.A.; Rössler, J.; Krüger, B.; Maisano, F.; Spahn, D.R.; et al. Predictors associated with mortality of extracorporeal life support therapy for acute heart failure: Single-center experience with 679 patients. J. Thorac. Dis. 2022, 14, 1960–1971. [Google Scholar] [CrossRef]
- Samalavicius, R.; Norkiene, I.; Scupakova, N.; Sabliauskas, J.; Urbonas, K.; Andrijauskas, P.; Jankuviene, A.; Puodziukaite, L.; Zorinas, A.; Janusauskas, V. Evaluation of risk factors for adverse outcome in extracorporeal membrane oxygenation-supported elderly postcardiotomy patients. Perfusion 2020, 35 (Suppl. S1), 50–56. [Google Scholar] [CrossRef]
- Rupprecht, L.; Lunz, D.; Philipp, A.; Lubnow, M.; Schmid, C. Pitfalls in percutaneous ECMO cannulation. Heart Lung Vessel. 2015, 7, 320–326. [Google Scholar]
- Radakovic, D.; Hamouda, K.; Penov, K.; Bening, C.; Sayed, S.; Gietzen, C.; Leyh, R.G.; Aleksic, I. Central versus peripheral arterial cannulation for veno-arterial extracorporeal membrane oxygenation in post-cardiotomy patients. ASAIO J. 2021, 67, 67–73. [Google Scholar] [CrossRef]
- Merritt-Genore, H.; Schwabe, M.; Luksan, A.; Ryan, T.; Lyden, E.; Moulton, M. Postcardiotomy extracorporeal membrane oxygenator: No longer a bridge to no where? J. Card. Surg. 2020, 35, 2208–2215. [Google Scholar] [CrossRef]
- Kalampokas, N.; Sipahi, N.F.; Aubin, H.; Akhyari, P.; Petrov, G.; Albert, A.; Westenfeld, R.; Lichtenberg, A.; Saeed, D. Postcardiotomy veno-arterial extracorporeal membrane oxygenation: Does the cannulation technique influence the outcome? Front. Cardiovasc. Med. 2021, 8, 658412. [Google Scholar] [CrossRef]
- Djordjevic, I.; Eghbalzadeh, K.; Sabashnikov, A.; Deppe, A.C.; Kuhn, E.; Merkle, J.; Weber, C.; Ivanov, B.; Ghodsizad, A.; Rustenbach, C. Central vs. peripheral venoarterial ECMO in postcardiotomy cardiogenic shock. J. Card. Surg. 2020, 35, 1037–1042. [Google Scholar] [CrossRef]
- Kinnunen, E.M.; Juvonen, T.; Airaksinen, K.E.; Heikkinen, J.; Kettunen, U.; Mariscalco, G.; Biancari, F. Clinical significance and determinants of the universal definition of perioperative bleeding classification in patients undergoing coronary artery bypass surgery. J. Thorac. Cardiovasc. Surg. 2014, 148, 1640–1646. [Google Scholar] [CrossRef] [Green Version]
- Meng, W.; Li, R.; Lihua, E.; Zha, N. Postoperative acute kidney injury and early and long-term mortality in acute aortic dissection patients: A meta-analysis. Medicine 2021, 100, e23426. [Google Scholar] [CrossRef]

| Population | Patients who underwent any adult cardiac surgery procedure |
| Intervention | Veno-arterial extracorporeal membrane oxygenation for cardiogenic shock after adult cardiac surgery |
| Comparison | Central versus peripheral arterial cannulation for veno-arterial extracorporeal membrane oxygenation |
| Outcomes | Mortality during the index hospitalization, mortality during veno-arterial extracorporeal membrane oxygenation |
| Al-Kawaz 2022 [12] | Alhijab 2022 [13] | Alonso-Fernandez-Gatta 2021 [14] | Biancari 2020 [2] | Djordjevic 2021 [15] | Hernández-Pérez 2021 [16] | L’Acqua 2022 [17] | Laimoud 2020 [18] | Sahli 2022 [19] | Samalavicius 2020 [20] | |
|---|---|---|---|---|---|---|---|---|---|---|
| No. of patients * | 50 | 101 | 34 | 781 | 172 | 32 | 17 | 61 | 215 | 40 |
| No. of patients included in the analysis | 48 | 88 | 31 | 645 | 149 | 31 | 16 | 60 | 183 | 39 |
| Multicenter study | No | No | No | Yes | No | No | No | No | No | No |
| Prospective study | No | No | No | No | No | No | No | No | No | No |
| NHLBI study quality criteria | ||||||||||
| 1. Was the study question or objective clearly stated? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2. Was the study population clearly and fully described, including a case definition? | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| 3. Were the cases consecutive? | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4. Were the subjects comparable? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 5. Was the intervention clearly described? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6. Were the outcome measures clearly defined, valid, reliable, and implemented consistently across all study participants? | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | No |
| 7. Was the length of follow-up adequate? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 8. Were the statistical methods well-described? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9. Were the results well-described? | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Quality rating | Good | Good | Good | Good | Good | Good | Fair | Good | Good | Fair |
| Clinical Variables | Alive N = 422 | In-Hospital Death N = 847 | Univariable Analysis p-Value | Multivariate Analysis |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age, years | 58.2 (14.5) | 63.8 (13.2) | <0.0001 | 1.03, 1.02–1.04 |
| Female gender | 109 (25.8) | 290 (34.2) | 0.002 | 1.43, 1.09–1.88 |
| eGFR, mL/min/1.73 m2 | 74 (34) | 65 (32) | <0.0001 | |
| Coronary artery disease | 203 (48.1) | 392 (46.3) | 0.540 | |
| Type A aortic dissection | 23 (5.5) | 73 (8.6) | 0.044 | |
| Preop. acute neurological event | 14 (3.3) | 60 (7.1) | 0.007 | 2.13, 1.14–3.97 |
| Prior cardiac surgery | 83 (19.7) | 224 (26.4) | 0.008 | 1.55, 1.14–2.10 |
| Arterial lactate, mmol/L | 6.7 (4.3) | 9.3 (5.9) | <0.0001 | 1.11, 1.08–1.14 |
| Procedural data | ||||
| Urgent/emergency surgery | 206 (48.8) | 430 (50.8) | 0.512 | |
| Isolated CABG | 98 (23.2) | 188 (22.2) | 0.680 | |
| Any CABG | 200 (47.4) | 397 (46.9) | 0.861 | |
| Aortic valve procedure | 164 (38.9) | 296 (34.9) | 0.172 | |
| Mitral valve procedure | 151 (35.8) | 297 (35.1) | 0.801 | |
| Tricuspid valve procedure | 54 (12.8) | 125 (14.8) | 0.344 | |
| Pulmonary valve procedure | 2 (0.5) | 4 (0.5) | 1.000 | |
| VSD or ventricular wall repair | 14 (3.3) | 30 (3.5) | 0.837 | |
| Septal myectomy | 1 (0.2) | 6 (0.7) | 0.285 | |
| Aortic surgery | 73 (17.3) | 172 (20.3) | 0.201 | |
| Aortic root replacement | 44 (10.4) | 84 (9.9) | 0.777 | |
| Aortic arch surgery | 9 (2.1) | 54 (6.4) | 0.001 | 2.94, 1.40–6.20 |
| Heart/heart and lung transplantation | 8 (1.9) | 23 (2.7) | 0.373 | |
| Other procedures | 15 (3.6) | 53 (6.3) | 0.044 | |
| VA-ECMO at primary surgery | 268 (63.7) | 506 (60.0) | 0.203 | |
| IABP during VA-ECMO | 172 (40.8) | 347 (41.0) | 0.930 | |
| Central VA-ECMO | 163 (38.6) | 393 (46.4) | 0.009 | 1.31, 1.02–1.70 |
| VA-ECMO duration, days | 7.0 (5.7) | 6.2 (6.8) | <0.0001 |
| Unmatched Patients | Propensity Score Matched Patients | |||||
|---|---|---|---|---|---|---|
| Clinical Variables | Peripheral ECMO N = 713 | Central ECMO N = 556 | Standardized Difference | Peripheral ECMO N = 538 | Central ECMO N = 538 | Standardized Difference |
| Baseline characteristics | ||||||
| Age, years | 62.6 (13.0) | 60.9 (15.0) | 0.118 | 62.3 (13.1) | 61.1 (14.8) | 0.083 |
| Septuagenarian | 224 (31.4) | 178 (32.0) | 0.013 | 167 (31.0) | 173 (32.2) | 0.024 |
| Female gender | 207 (29.0) | 192 (34.5) | 0.118 | 171 (31.8) | 183 (34.0) | 0.047 |
| eGFR, mL/min/1.73 m2 | 67 (31) | 69 (36) | 0.063 | 68 (32) | 69 (36) | 0.029 |
| Coronary artery disease | 334 (46.8) | 261 (46.9) | 0.002 | 253 (47.0) | 254 (47.2) | 0.004 |
| Type A aortic dissection | 54 (7.6) | 42 (7.6) | 0.001 | 44 (8.2) | 42 (7.8) | 0.013 |
| Preop. acute neurological event | 48 (6.7) | 26 (4.7) | 0.089 | 28 (5.2) | 26 (4.8) | 0.017 |
| Prior cardiac surgery | 169 (23.7) | 138 (24.8) | 0.026 | 133 (24.7) | 130 (24.2) | 0.013 |
| Arterial lactate, mmol/L | 7.9 (5.2) | 9.2 (5.8) | 0.233 | 8.6 (5.3) | 9.0 (5.6) | 0.076 |
| Procedural data | ||||||
| Urgent/emergency surgery | 386 (54.1) | 250 (45.0) | 0.182 | 262 (48.7) | 243 (45.2) | 0.071 |
| Isolated CABG | 161 (22.6) | 125 (22.5) | 0.002 | 130 (24.2) | 123 (22.9) | 0.031 |
| Any CABG | 328 (46.0) | 269 (48.4) | 0.048 | 259 (48.1) | 261 (48.5) | 0.007 |
| Aortic valve procedure | 262 (36.7) | 198 (35.6) | 0.024 | 195 (36.2) | 192 (35.7) | 0.012 |
| Mitral valve procedure | 238 (33.4) | 210 (37.8) | 0.092 | 187 (34.8) | 203 (37.7) | 0.062 |
| Tricuspid valve procedure | 94 (13.2) | 85 (15.3) | 0.060 | 73 (13.6) | 83 (15.4) | 0.053 |
| Pulmonary valve procedure | 1 (0.1) | 5 (0.9) | 0.110 | 1 (0.2) | 2 (0.4) | 0.036 |
| VSD or ventricular wall repair | 31 (4.3) | 13 (2.3) | 0.112 | 15 (2.8) | 13 (2.4) | 0.023 |
| Septal myectomy | 2 (0.3) | 5 (0.9) | 0.081 | 1 (0.2) | 2 (0.4) | 0.036 |
| Aortic surgery | 138 (19.4) | 107 (19.2) | 0.003 | 107 (19.9) | 106 (19.7) | 0.005 |
| Aortic root replacement | 71 (10.0) | 57 (10.3) | 0.010 | 54 (10.0) | 57 (10.6) | 0.018 |
| Aortic arch surgery | 34 (4.8) | 29 (5.2) | 0.021 | 30 (5.6) | 29 (5.4) | 0.008 |
| Heart/heart and lung transplantation | 10 (1.4) | 21 (3.8) | 0.150 | 10 (1.9) | 18 (3.3) | 0.094 |
| Other procedures | 29 (4.1) | 39 (7.0) | 0.129 | 24 (4.5) | 37 (6.9) | 0.011 |
| VA-ECMO at primary surgery | 411 (57.9) | 363 (65.4) | 0.155 | 332 (61.7) | 349 (64.9) | 0.066 |
| IABP during VA-ECMO | 258 (3.2) | 261 (47.0) | 0.221 | 226 (42.0) | 249 (46.3) | 0.086 |
| VA-ECMO duration, days | 6.6 (6.2) | 6.2 (6.6) | 0.057 | 6.7 (6.4) | 6.2 (6.5) | 0.073 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biancari, F.; Kaserer, A.; Perrotti, A.; Ruggieri, V.G.; Cho, S.-M.; Kang, J.K.; Dalén, M.; Welp, H.; Jónsson, K.; Ragnarsson, S.; et al. Central versus Peripheral Postcardiotomy Veno-Arterial Extracorporeal Membrane Oxygenation: Systematic Review and Individual Patient Data Meta-Analysis. J. Clin. Med. 2022, 11, 7406. https://doi.org/10.3390/jcm11247406
Biancari F, Kaserer A, Perrotti A, Ruggieri VG, Cho S-M, Kang JK, Dalén M, Welp H, Jónsson K, Ragnarsson S, et al. Central versus Peripheral Postcardiotomy Veno-Arterial Extracorporeal Membrane Oxygenation: Systematic Review and Individual Patient Data Meta-Analysis. Journal of Clinical Medicine. 2022; 11(24):7406. https://doi.org/10.3390/jcm11247406
Chicago/Turabian StyleBiancari, Fausto, Alexander Kaserer, Andrea Perrotti, Vito G. Ruggieri, Sung-Min Cho, Jin Kook Kang, Magnus Dalén, Henryk Welp, Kristján Jónsson, Sigurdur Ragnarsson, and et al. 2022. "Central versus Peripheral Postcardiotomy Veno-Arterial Extracorporeal Membrane Oxygenation: Systematic Review and Individual Patient Data Meta-Analysis" Journal of Clinical Medicine 11, no. 24: 7406. https://doi.org/10.3390/jcm11247406
APA StyleBiancari, F., Kaserer, A., Perrotti, A., Ruggieri, V. G., Cho, S.-M., Kang, J. K., Dalén, M., Welp, H., Jónsson, K., Ragnarsson, S., Hernández Pérez, F. J., Gatti, G., Alkhamees, K., Loforte, A., Lechiancole, A., Rosato, S., Spadaccio, C., Pettinari, M., Fiore, A., ... Mariscalco, G. (2022). Central versus Peripheral Postcardiotomy Veno-Arterial Extracorporeal Membrane Oxygenation: Systematic Review and Individual Patient Data Meta-Analysis. Journal of Clinical Medicine, 11(24), 7406. https://doi.org/10.3390/jcm11247406
















