The Safety of Chemotherapy for Ovarian Malignancy during Pregnancy
Abstract
:1. Introduction
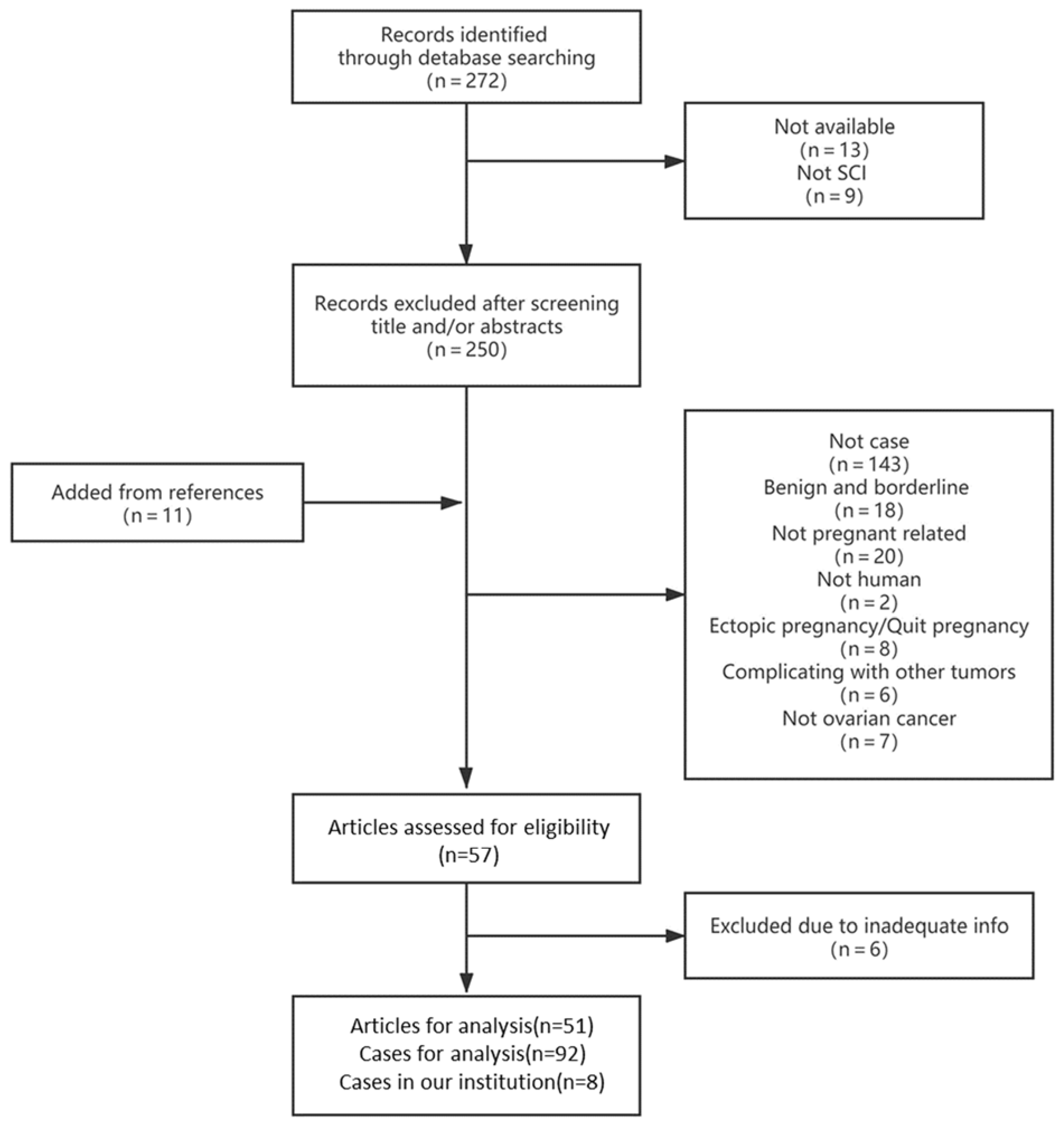
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Epidemiological Characteristics of Pregnant Patients Complicated with Ovarian Malignancy
3.2. Tumor Markers Used to Diagnose Ovarian Malignancy in Patients during Pregnancy
3.3. Maternal and Neonatal Outcomes of Pregnant Patients Diagnosed with Ovarian Malignancy
3.4. The Management of Pregnant Patients with Ovarian Malignancy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schwab, R.; Anic, K.; Hasenburg, A. Cancer and Pregnancy: A Comprehensive Review. Cancers 2021, 13, 3048. [Google Scholar] [CrossRef] [PubMed]
- Leiserowitz, G.S.; Xing, G.; Cress, R.; Brahmbhatt, B.; Dalrymple, J.L.; Smith, L.H. Adnexal masses in pregnancy: How often are they malignant? Gynecol. Oncol. 2006, 101, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Ercan, S.; Kaymaz, O.; Yücel, N.; Orçun, A. Serum concentrations of CA 125, CA 15-3, CA 19-9 and CEA in normal pregnancy: A longitudinal study. Arch. Gynecol. Obstet. 2011, 285, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Sarandakou, A.; Protonotariou, E.; Rizos, D. Tumor Markers in Biological Fluids Associated with Pregnancy. Crit. Rev. Clin. Lab. Sci. 2007, 44, 151–178. [Google Scholar] [CrossRef] [PubMed]
- Bredaki, F.E.; Sciorio, C.; Wright, A.; Wright, D.; Nicolaides, K.H. Serum alpha-fetoprotein in the three trimesters of pregnancy: Effects of maternal characteristics and medical history. Ultrasound Obstet. Gynecol. 2015, 46, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Amant, F.; Berveiller, P.; Boere, I.; Cardonick, E.; Fruscio, R.; Fumagalli, M.; Halaska, M.; Hasenburg, A.; Johansson, A.; Lambertini, M.; et al. Gynecologic cancers in pregnancy: Guidelines based on a third international consensus meeting. Ann. Oncol. 2019, 30, 1601–1612. [Google Scholar] [CrossRef] [Green Version]
- Morice, P.; Uzan, C.; Gouy, S.; Verschraegen, C.; Haie-Meder, C. Gynaecological cancers in pregnancy. Lancet 2012, 379, 558–569. [Google Scholar] [CrossRef]
- Amant, F.; Vandenbroucke, T.; Verheecke, M.; Fumagalli, M.; Halaska, M.J.; Boere, I.; Han, S.; Gziri, M.M.; Peccatori, F.; Rob, L.; et al. Pediatric Outcome after Maternal Cancer Diagnosed during Pregnancy. N. Engl. J. Med. 2015, 373, 1824–1834. [Google Scholar] [CrossRef]
- Koren, G.; Carey, N.; Gagnon, R.; Maxwell, C.; Nulman, I.; Senikas, V. Cancer chemotherapy and pregnancy. J. Obstet. Gynaecol. Can. J. D′obstetrique Gynecol. Can. JOGC 2013, 35, 263–278. [Google Scholar]
- Franciszek Dłuski, D.; Mierzyński, R.; Poniedziałek-Czajkowska, E.; Leszczyńska-Gorzelak, B. Ovarian Cancer and Pregnancy-A Current Problem in Perinatal Medicine: A Comprehensive Review. Cancers 2020, 12, 3795. [Google Scholar] [CrossRef]
- Boussios, S.; Moschetta, M.; Tatsi, K.; Tsiouris, A.K.; Pavlidis, N. A review on pregnancy complicated by ovarian epithelial and non-epithelial malignant tumors: Diagnostic and therapeutic perspectives. J. Adv. Res. 2018, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Weed, J.C.; Roh, R.A.; Mendenhall, H.W. Recurrent endodermal sinus tumor during pregnancy. Obstet. Gynecol. 1979, 54, 653–656. [Google Scholar] [PubMed]
- Young, R.H.; Dudley, A.; Scully, R.E. Granulosa cell, Sertoli-Leydig cell, and unclassified sex cord-stromal tumors associated with pregnancy: A clinicopathological analysis of thirty-six cases. Gynecol. Oncol. 1984, 18, 181–205. [Google Scholar] [CrossRef] [PubMed]
- Malone, J.M.; Gershenson, D.M.; Creasy, R.K.; Kavanagh, J.J.; Silva, E.G.; Stringer, C.A. Endodermal sinus tumor of the ovary associated with pregnancy. Obstet. Gynecol. 1986, 68, 86S–89S. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.S.; Park, M.I. Maternal and fetal survival following surgery and chemotherapy of endodermal sinus tumor of the ovary during pregnancy: A case report. Obstet. Gynecol. 1989, 73, 503–507. [Google Scholar]
- Metz, S.; Day, T.; Pursell, S. Adjuvant chemotherapy in a pregnant patient with endodermal sinus tumor of the ovary. Gynecol. Oncol. 1989, 32, 371–374. [Google Scholar] [CrossRef]
- Christman, J.E.; Teng, N.; Lebovic, G.S.; Sikic, B.I. Delivery of a normal infant following cisplatin, vinblastine, and bleomycin (PVB) chemotherapy for malignant teratoma of the ovary during pregnancy. Gynecol. Oncol. 1990, 37, 292–295. [Google Scholar] [CrossRef]
- Malfetano, J.H.; Goldkrand, J.W. Cis-platinum combination chemotherapy during pregnancy for advanced epithelial ovarian carcinoma. Obstet. Gynecol. 1990, 75, 545–547. [Google Scholar]
- King, L.A.; Nevin, P.C.; Williams, P.P.; Carson, L.F. Treatment of advanced epithelial ovarian carcinoma in pregnancy with cisplatin-based chemotherapy. Gynecol. Oncol. 1991, 41, 78–80. [Google Scholar] [CrossRef]
- Van der Zee, A.G.; de Bruijn, H.W.; Bouma, J.; Aalders, J.G.; Oosterhuis, J.W.; de Vries, E.G. Endodermal sinus tumor of the ovary during pregnancy: A case report. Am. J. Obstet. Gynecol. 1991, 164, 504–506. [Google Scholar] [CrossRef]
- Buller, R.E.; Darrow, V.; Manetta, A.; Porto, M.; DiSaia, P.J. Conservative surgical management of dysgerminoma concomitant with pregnancy. Obstet. Gynecol. 1992, 79, 887–890. [Google Scholar] [PubMed]
- Méndez, L.E.; Mueller, A.; Salom, E.; González-Quintero, V.H. Paclitaxel and Carboplatin Chemotherapy Administered During Pregnancy for Advanced Epithelial Ovarian Cancer. Obstet. Gynecol. 2003, 102, 1200–1202. [Google Scholar] [CrossRef] [PubMed]
- Horbelt, D.; Delmore, J.; Meisel, R.; Cho, S.; Roberts, D.; Logan, D. Mixed germ cell malignancy of the ovary concurrent with pregnancy. Obstet. Gynecol. 1994, 84, 662–664. [Google Scholar]
- Sasano, H.; Imaizumi, H.; Nagura, H. Juvenile granulosa cell tumor discovered during pregnancy: Case report with immunohistochemical study of steroidogenesis. Pathol. Int. 1997, 47, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Elit, L.; Bocking, A.; Kenyon, C.; Natale, R. An Endodermal Sinus Tumor Diagnosed in Pregnancy: Case Report and Review of the Literature. Gynecol. Oncol. 1999, 72, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Arima, N.; Tanimoto, A.; Hayashi, R.; Hamada, T.; Sasaguri, Y. Ovarian yolk sac tumor with virilization during pregnancy: Immunohistochemical demonstration of Leydig cells as functioning stroma. Pathol. Int. 2000, 50, 520–525. [Google Scholar] [CrossRef]
- Otton, G.; Higgins, S.; Phillips, K.A.; Quinn, M. A case of early-stage epithelial ovarian cancer in pregnancy. Off. J. Int. Gynecol. Cancer Soc. 2001, 11, 413–417. [Google Scholar] [CrossRef]
- Sood, A.K.; Shahin, M.S.; Sorosky, J.I. Paclitaxel and Platinum Chemotherapy for Ovarian Carcinoma during Pregnancy. Gynecol. Oncol. 2001, 83, 599–600. [Google Scholar] [CrossRef]
- Shimizu, Y.; Komiyama, S.-I.; Kobayashi, T.; Nakata, K.; Iida, T. Successful management of endodermal sinus tumor of the ovary associated with pregnancy. Gynecol. Oncol. 2003, 88, 447–450. [Google Scholar] [CrossRef]
- Picone, O.; Lhommé, C.; Tournaire, M.; Pautier, P.; Camatte, S.; Vacher-Lavenue, M.-C.; Castaigne, D.; Morice, P. Preservation of pregnancy in a patient with a stage IIIB ovarian epithelial carcinoma diagnosed at 22 weeks of gestation and treated with initial chemotherapy: Case report and literature review. Gynecol. Oncol. 2004, 94, 600–604. [Google Scholar] [CrossRef]
- Aoki, Y.; Higashino, M.; Ishii, S.; Tanaka, K. Yolk sac tumor of the ovary during pregnancy: A case report. Gynecol. Oncol. 2005, 99, 497–499. [Google Scholar] [CrossRef]
- Ferrandina, G.; Distefano, M.; Testa, A.; De Vincenzo, R.; Scambia, G. Management of an advanced ovarian cancer at 15 weeks of gestation: Case report and literature review. Gynecol. Oncol. 2005, 97, 693–696. [Google Scholar] [CrossRef] [PubMed]
- Han, J.-Y.; Nava-Ocampo, A.A.; Kim, T.-J.; Shim, J.-U.; Park, C.-T. Pregnancy outcome after prenatal exposure to bleomycin, etoposide and cisplatin for malignant ovarian germ cell tumors: Report of 2 cases. Reprod. Toxicol. 2005, 19, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Ghaemmaghami, F.; Hasanzadeh, M. Good fetal outcome of pregnancies with gynecologic cancer conditions: Cases and literature review. Off. J. Int. Gynecol. Cancer Soc. 2006, 16, 225–230. [Google Scholar] [CrossRef]
- Hubalek, M.; Smekal-Schindelwig, C.; Zeimet, A.G.; Sergi, C.; Brezinka, C.; Mueller-Holzner, E.; Marth, C. Chemotherapeutic treatment of a pregnant patient with ovarian dysgerminoma. Arch. Gynecol. Obstet. 2007, 276, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Kodama, M.; Grubbs, B.; Blake, E.A.; Cahoon, S.S.; Murakami, R.; Kimura, T.; Matsuo, K. Feto-maternal outcomes of pregnancy complicated by ovarian malignant germ cell tumor: A systematic review of literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 181, 145–156. [Google Scholar] [CrossRef]
- Mantovani, G.; Mais, V.; Parodo, G.; Gramignano, G.; Carrucciu, G.M.; Melis, G.B. Use of chemotherapy for ovarian cancer during human pregnancy: Case report and literature review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2007, 131, 238–239. [Google Scholar] [CrossRef]
- Modares, G.M.; Karimi, Z.M.; Behtash, N.; Ghaemmaghami, F.; Mousavi, A.S.; Behnamfar, F. Preservation of pregnancy in a patient with advanced ovarian cancer at 20 weeks of gestation: Case report and literature review. Off. J. Int. Gynecol. Cancer Soc. 2007, 17, 1140–1143. [Google Scholar] [CrossRef]
- Motegi, M.; Takakura, S.; Takano, H.; Tanaka, T.; Ochiai, K. Adjuvant Chemotherapy in a Pregnant Woman with Endodermal Sinus Tumor of the Ovary. Obstet. Gynecol. 2007, 109, 537–540. [Google Scholar] [CrossRef]
- Robova, H.; Rob, L.; Hrehorcak, M.; Zoban, P.; Prusa, R. Endodermal sinus tumor diagnosed in pregnancy: A case report. Off. J. Int. Gynecol. Cancer Soc. 2007, 17, 914–916. [Google Scholar] [CrossRef]
- Karimi, Z.M.; Behtash, N.; Modares, G.M. Good pregnancy outcome after prenatal exposure to bleomycin, etoposide and cisplatin for ovarian immature teratoma: A case report and literature review. Arch. Gynecol. Obstet. 2008, 277, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Tabata, T.; Nishiura, K.; Tanida, K.; Kondo, E.; Okugawa, T.; Sagawa, N. Carboplatin chemotherapy in a pregnant patient with undifferentiated ovarian carcinoma: Case report and review of the literature. Int. J. Gynecol. Cancer 2008, 18, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Doi, D.; Boh, Y.; Konishi, H.; Asakura, H.; Takeshita, T. Combined chemotherapy with paclitaxel and carboplatin for mucinous cystadenocarcinoma of the ovary during pregnancy. Arch. Gynecol. Obstet. 2009, 280, 633–636. [Google Scholar] [CrossRef] [PubMed]
- Ghaemmaghami, F.; Abbasi, F.; Abadi, A.G.N. A favorable maternal and neonatal outcome following chemotherapy with etoposide, bleomycin, and cisplatin for management of grade 3 immature teratoma of the ovary. J. Gynecol. Oncol. 2009, 20, 257–259. [Google Scholar] [CrossRef]
- Pafilis, I.; Haidopoulos, D.; Rodolakis, A.; Vlachos, G.; Voulgaris, Z.; Sotiropoulou, M.; Antsaklis, A. Management of a pregnancy complicated by yolk sac tumor. Arch. Gynecol. Obstet. 2009, 280, 803–806. [Google Scholar] [CrossRef]
- Rouzi, A.A.; Sahly, N.N.; Sahly, N.F.; Alahwal, M.S. Cisplatinum and docetaxel for ovarian cancer in pregnancy. Arch. Gynecol. Obstet. 2009, 280, 823–825. [Google Scholar] [CrossRef]
- Benjapibal, M.; Chaopotong, P.; Leelaphatanadit, C.; Jaishuen, A. Ruptured ovarian endodermal sinus tumor diagnosed during pregnancy: Case report and review of the literature. J. Obstet. Gynaecol. Res. 2010, 36, 1137–1141. [Google Scholar] [CrossRef]
- Malhotra, N.; Sumana, G.; Singh, A.; Deka, D.; Mittal, S. Rupture of a malignant ovarian tumor in pregnancy presenting as acute abdomen. Arch. Gynecol. Obstet. 2009, 281, 959–961. [Google Scholar] [CrossRef]
- Agarwal, R.; Radhakrishnan, G.; Radhika, A.G.; Jain, J.; Sharma, S.; Srivastava, H. Pregnancy concomitant with metastatic adult granulosa cell tumor. Arch. Gynecol. Obstet. 2011, 284, 743–747. [Google Scholar] [CrossRef]
- Hasegawa, T.; Ishii, Y.; Yonezawa, R.; Yoneda, N.; Shima, T.; Nakashima, A.; Hidaka, T.; Saito, S. Stage I ovarian cancer cases during early, mid and late pregnancy periods: Three case reports and review of the literature. J. Obstet. Gynaecol. Res. 2010, 37, 650–655. [Google Scholar] [CrossRef]
- Serkies, K.; Węgrzynowicz, E.; Jassem, J. Paclitaxel and cisplatin chemotherapy for ovarian cancer during pregnancy: Case report and review of the literature. Arch. Gynecol. Obstet. 2011, 283, 97–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viana, L.S.; Tsunoda, A.T.; Nunes, J.S.; Fregnani, J.H.T.G.; Vieira, M.A.; Borges, A.K.N.; Andrade, C.E.M.D.C.; Serrano, S.V. Preservation of Pregnancy in a Patient with Acute Abdominal Pain Secondary to Advanced and Hemorrhagic Yolk Sac Tumor of the Right Ovary. J. Clin. Oncol. 2011, 29, e758–e762. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Shu, C.; Li, N.; Xia, M.; Li, T.; Zhong, Y.; Yan, X.; Wang, H.; Zhang, H.; He, J. Early Pregnancy Complicated with Juvenile Granulosa Cell Tumor. Am. J. Med. Sci. 2011, 342, 435–437. [Google Scholar] [CrossRef]
- Zivanovic, A.; Dimitrijevic, A.; Kastratovic, T.; Djuric, J.; Stankovic, V.; Tanaskovic, I. Ovarian endometroid adenocarcinoma in pregnancy. Vojn. Pregl. 2011, 68, 181–184. [Google Scholar] [CrossRef] [PubMed]
- He, S.-Y.; Shen, H.-W.; Xu, L.; Li, X.-L.; Yao, S.-Z. Successful management of mucinous ovarian cancer by conservative surgery in week 6 of pregnancy: Case report and literature review. Arch. Gynecol. Obstet. 2012, 286, 989–993. [Google Scholar] [CrossRef] [Green Version]
- Ruiz Ramos, J.; Roma, E.; Palomar, L.; Poveda, J.L. Paclitaxel and carboplatin treatment for advanced ovarian cancer during pregnancy. Chemotherapy 2013, 59, 344–345. [Google Scholar] [CrossRef]
- Smith, E.R.; Borowsky, M.E.; Jain, V.D. Intraperitoneal Chemotherapy in a Pregnant Woman with Ovarian Cancer. Obstet. Gynecol. 2013, 122, 481–483. [Google Scholar] [CrossRef]
- Chen, C.-H.; Chiu, L.-H.; Chan, C.; Liu, W.-M. Management of Ovarian Cancer in 14th Gestational Week of Pregnancy by Robotic Approach with Preservation of the Fetus. Gynecol. Obstet. Investig. 2015, 80, 139–144. [Google Scholar] [CrossRef]
- Xu, T.; Wang, L.; Jia, Y.; Jia, Z.; Li, Z.; Cui, S.; Cui, M. Long-term multidisciplinary integrative therapy management resulted in favorable outcomes for ovarian cancer during pregnancy: A case report and literature review. J. Ovarian Res. 2019, 12, 108. [Google Scholar] [CrossRef] [Green Version]
- Zong, X.; Yang, J.-X.; Zhang, Y.; Cao, D.-Y.; Shen, K. Clinicopathological Characteristics and Treatment Outcomes of Pregnancy Complicated by Malignant Ovarian Germ Cell Tumors. Cancer Manag. Res. 2020, 12, 1347–1354. [Google Scholar] [CrossRef] [Green Version]
- Bueno Moral, A.I.; Vilches Jiménez, J.C.; Serrano Olave, A.; Espejo Reina, M.P.; Valdivia de Dios, M.E.; Jiménez López, J.S. Advanced Ovarian Cancer during Pregnancy. Tumour Evolution Analysis and Treatment Approach. Medicina 2021, 57, 426. [Google Scholar] [CrossRef] [PubMed]
- Henderson, C.E.; Elia, G.; Garfinkel, D.; Poirier, M.C.; Shamkhani, H.; Runowicz, C.D. Platinum Chemotherapy during Pregnancy for Serous Cystadenocarcinoma of the Ovary. Gynecol. Oncol. 1993, 49, 92–94. [Google Scholar] [CrossRef] [PubMed]
- Mutch, D.G.; Prat, J. 2014 FIGO staging for ovarian, fallopian tube and peritoneal cancer. Gynecol. Oncol. 2014, 133, 401–404. [Google Scholar] [CrossRef]
- Han, S.N.; Lotgerink, A.; Gziri, M.M.; Van Calsteren, K.; Hanssens, M.; Amant, F. Physiologic variations of serum tumor markers in gynecological malignancies during pregnancy: A systematic review. BMC Med. 2012, 10, 86. [Google Scholar] [CrossRef] [PubMed]
- Raty, R.; Anttila, L.; Virtanen, A.; Koskinen, P.; Laitien, P.; Morsky, P.; Tiitinen, A.; Martikainen, H.; Ekblad, U. Maternal midtrimester free beta-HCG and AFP serum levels in spontaneous singleton pregnancies complicated by gestational diabetes mellitus, pregnancy-induced hypertension or obstetric cholestasis. Prenat. Diagn. 2003, 23, 1045–1048. [Google Scholar] [CrossRef]
- Krause, T.G.; Christens, P.; Wohlfahrt, J.; Lei, U.; Westergaard, T.; Pedersen, B.N.; Melbye, M. Second-trimester maternal serum alpha-fetoprotein and risk of adverse pregnancy outcome. Obstet. Gynecol. 2001, 97, 277–282. [Google Scholar]
- Mizejewski, G.J. Levels of Alpha-Fetoprotein During Pregnancy and Early Infancy in Normal and Disease States. Obstet. Gynecol. Surv. 2003, 58, 804–826. [Google Scholar] [CrossRef]
- Blake, E.A.; Kodama, M.; Yunokawa, M.; Ross, M.S.; Ueda, Y.; Grubbs, B.; Matsuo, K. Feto-maternal outcomes of pregnancy complicated by epithelial ovarian cancer: A systematic review of literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 186, 97–105. [Google Scholar] [CrossRef]
- Bar-Joseph, H.; Peccatori, F.A.; Goshen-Lago, T.; Cribiu, F.M.; Scarfone, G.; Miller, I.; Nmerovsky, L.; Levi, M.; Shalgi, R.; Ben-Aharon, I. Cancer During Pregnancy: The Role of Vascular Toxicity in Chemother-apy-Induced Placental Toxicity. Cancers 2020, 12, 1277. [Google Scholar] [CrossRef]
- Abdalla, N.; Bizon, M.; Piorkowski, R.; Stanirowski, P.; Cendrowski, K.; Sawicki, W. Does Chemotherapy for Gynecological Malignancies during Pregnancy Cause Fetal Growth Restriction? BioMed Res. Int. 2017, 2017, 7543421. [Google Scholar] [CrossRef] [Green Version]
- Cardonick, E.; Bhat, A.; Gilmandyar, D.; Somer, R. Maternal and fetal outcomes of taxane chemotherapy in breast and ovarian cancer during pregnancy: Case series and review of the literature. Ann. Oncol. 2012, 23, 3016–3023. [Google Scholar] [CrossRef] [PubMed]
- Cardonick, E.; Iacobucci, A. Use of chemotherapy during human pregnancy. Lancet Oncol. 2004, 5, 283–291. [Google Scholar] [CrossRef]
- World Health Statistics. Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Gray, K.; Pacey, V.; Gibbons, P.; Little, D.; Burns, J. Interventions for congenital talipes equinovarus (clubfoot). Cochrane Database Syst. Rev. 2014, 2014, CD008602. [Google Scholar] [CrossRef] [PubMed]
- Amant, F.; van Calsteren, K.; Halaska, M.J.; Gziri, M.M.; Hui, W.; Lagae, L.; Willemsen, M.A.; Kapusta, L.; Calster, B.V.; Wouters, H.; et al. Long-term cognitive and cardiac outcomes after prenatal exposure to chemotherapy in children aged 18 months or older: An observational study. Lancet Oncol. 2012, 13, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Van Calsteren, K.; Heyns, L.; De Smet, F.; van Eycken, L.; Gziri, M.M.; van Gemert, W.; Halaska, M.; Vergote, I.; Ottevanger, N.; Amant, F. Cancer during pregnancy: An analysis of 215 patients emphasizing the obstetrical and the neonatal outcomes. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 683–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Haan, J.; Verheecke, M.; van Calsteren, K.; Calster, B.V.; Shmakov, R.G.; Gziri, M.M.; Halaska, M.J.; Fruscio, R.; Lok, C.A.R.; Boere, I.A.; et al. Oncological management and obstetric and neonatal outcomes for women diagnosed with cancer during pregnancy: A 20-year international cohort study of 1170 patients. Lancet Oncol. 2018, 19, 337–346. [Google Scholar] [CrossRef]


| Epithelial Ovarian Cancer Group (n = 34) | Germ Cell Tumors Group (n = 38) | Sex Cord-Stromal Tumors Group (n = 28) | ||
|---|---|---|---|---|
| Area of cases | p = 0.035 | |||
| Asia | 15 | 23 | 3 | 41(41%) |
| Europe | 11 | 7 | 0 | 18(18%) |
| North America | 7 | 8 | 25 | 40(40%) |
| Australia | 1 | 0 | 0 | 1(1%) |
| Maternal age at diagnosis | 32.8 ± 5.6 | 26.9 ± 4.7 | 23.6 ± 4.3 | p < 0.001 |
| <20 | 0 | 2 | 4 | 6(6%) |
| 20–29 | 8 | 24 | 22 | 54(54%) |
| ≥30 | 26 | 12 | 2 | 40(40%) |
| Multipara | p = 0.135 | |||
| Yes | 11 | 8 | 15 | 34(34%) |
| No | 16 | 13 | 8 | 37(37%) |
| Missing | 7 | 17 | 5 | 29(29%) |
| Clinical presentation | p = 0.036 | |||
| Abdominal pain | 6 | 11 | 9 | 26(23.6%) |
| Abdominal distention | 1 | 4 | 1 | 6(5.5%) |
| Pelvic mass | 22 | 13 | 5 | 40(36.4%) |
| Vaginal bleeding | 1 | 1 | 1 | 3(2.7%) |
| Virilization | 0 | 0 | 3 | 3(2.7%) |
| Missing | 6 | 14 | 12 | 32(29.1%) |
| Ascites | p = 0.234 | |||
| Yes | 8 | 9 | 2 | 19(19%) |
| No | 4 | 3 | 24 | 31(31%) |
| Missing | 22 | 26 | 2 | 50(50%) |
| Gestational age at diagnosis | p = 0.027 | |||
| Before pregnancy a | 0 | 3 | 0 | 3(3%) |
| 1st trimester | 5 | 0 | 2 | 7(7%) |
| 2nd trimester | 16 | 24 | 1 | 41(41%) |
| 3rd trimester | 0 | 1 | 0 | 1(1%) |
| Postpartum b | 11 | 8 | 15 | 34(34%) |
| Missing | 2 | 2 | 10 | 14(14%) |
| Tumor laterality | p = 0.033 | |||
| Unilateral | 23 | 32 | 27 | 82(82%) |
| Bilateral | 4 | 2 | 1 | 7(7%) |
| Missing | 7 | 4 | 0 | 11(11%) |
| Tumor stage | p = 0.027 | |||
| I-II | 18 | 23 | 25 | 66(66%) |
| III-IV | 14 | 8 | 1 | 23(23%) |
| Missing | 2 | 7 | 2 | 11(11%) |
| Epithelial Ovarian Cancer Group (n = 34) | Germ Cell Tumors Group (n = 38) | Sex Cord-Stromal Tumors Group (n = 28) | ||
|---|---|---|---|---|
| Mode of delivery | p = 0.021 | |||
| Vaginal delivery | 2(6.0%) | 13(34.2%) | 2(7.2%) | 17(17%) |
| Cesarean section | 32(94.0%) | 25(65.8%) | 13(46.4%) | 70(70%) |
| Missing | 0 | 0 | 13(46.4%) | 13(13%) |
| Timing of birth | p = 0.032 | |||
| Preterm | 17 | 21 | 2 | 40(39.6%) |
| Full-term | 11 | 13 | 2 | 26(25.7%) |
| Missing | 6 | 5 | 24 | 35(34.7%) |
| Birth weight (g) | 2595.7 ± 656.7 | 2341.8 ± 614.2 | - | p = 0.127 |
| Sex of neonate | p = 0.109 | |||
| Male | 16 | 12 | 1 | 29(28.7%) |
| Female | 10 | 11 | 2 | 23(22.8%) |
| Missing | 8 | 16 | 25 | 49(48.5%) |
| Apgar scores | p = 0.276 | |||
| 1 min | 9 | 9 | - | |
| 5 min | 9 | 10 | - | |
| Maternal complications | p = 0.036 | |||
| Rupture or torsion of tumor | 10 | 9 | 7 | 26(26%) |
| Oligohydramnios | 1 | 4 | 0 | 5(5%) |
| Premature rupture of membrane | 3 | 1 | 0 | 4(4%) |
| Recurrence during pregnancy | 1 | 4 | 1 | 6(6%) |
| Maternal death | 0 | 1 | 0 | 1(1%) |
| Fetal complications | p = 0.042 | |||
| Fetal malformations | 1 | 2 | 0 | 3(2.97%) |
| Neonatal death | 1 | 1 | 0 | 2(1.98%) |
| Respiratory distress | 1 | 6 | 0 | 7(6.93%) |
| Routine blood abnormality | 0 | 4 | 0 | 4(3.96%) |
| Neonatal infection | 1 | 0 | 0 | 1(0.99%) |
| Neonatal intensive care unit | 1 | 0 | 0 | 1(0.99%) |
| Intrauterine growth restriction | 0 | 4 | 0 | 4(3.96%) |
| Intussusception | 0 | 1 | 0 | 1(0.99%) |
| N (%) | |
|---|---|
| Gestational age at surgery during pregnancy | 53 |
| 1st | 7(13.2%) |
| 2nd | 41(77.4%) |
| 3rd | 1(1.9%) |
| Missing | 4(7.5%) |
| Adnexal surgery during pregnancy | 53 |
| Cystectomy | 2(3.8%) |
| Unilateral | 41(77.4%) |
| Bilateral | 6(11.2%) |
| Missing | 4(7.6%) |
| Chemotherapy during pregnancy | |
| Yes | 43(43%) |
| No | 57(57%) |
| Beginning time of chemotherapy | |
| 1st | 0 |
| 2nd | 29(67.4%) |
| 3rd | 3(7.0%) |
| Missing | 11(25.6%) |
| Type of chemotherapy | 43 |
| Single-agent | 7(16.3%) |
| Double-agent combined | 19(44.2%) |
| Three-drug combined | 16(37.2%) |
| Missing | 1(2.3%) |
| Staging surgery after pregnancy | 49 |
| Fertility-sparing surgery | 11(22.4%) |
| Radical surgery | 34(69.4%) |
| Missing | 4(8.2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xing, N.; Wang, L.; Sui, X.; Zhao, C.; Huang, Y.; Peng, J. The Safety of Chemotherapy for Ovarian Malignancy during Pregnancy. J. Clin. Med. 2022, 11, 7520. https://doi.org/10.3390/jcm11247520
Xing N, Wang L, Sui X, Zhao C, Huang Y, Peng J. The Safety of Chemotherapy for Ovarian Malignancy during Pregnancy. Journal of Clinical Medicine. 2022; 11(24):7520. https://doi.org/10.3390/jcm11247520
Chicago/Turabian StyleXing, Naidong, Lihui Wang, Xinlei Sui, Chunru Zhao, Yan Huang, and Jin Peng. 2022. "The Safety of Chemotherapy for Ovarian Malignancy during Pregnancy" Journal of Clinical Medicine 11, no. 24: 7520. https://doi.org/10.3390/jcm11247520
APA StyleXing, N., Wang, L., Sui, X., Zhao, C., Huang, Y., & Peng, J. (2022). The Safety of Chemotherapy for Ovarian Malignancy during Pregnancy. Journal of Clinical Medicine, 11(24), 7520. https://doi.org/10.3390/jcm11247520




