Radiological Evaluation of Combined Anteroposterior Fusion with Vertebral Body Replacement Using a Minimally Invasive Lateral Approach for Osteoporotic Vertebral Fractures: Verification of Optimal Surgical Procedure
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects of the Study
2.2. Surgical Procedure
2.3. Measurement Parameters
3. Results
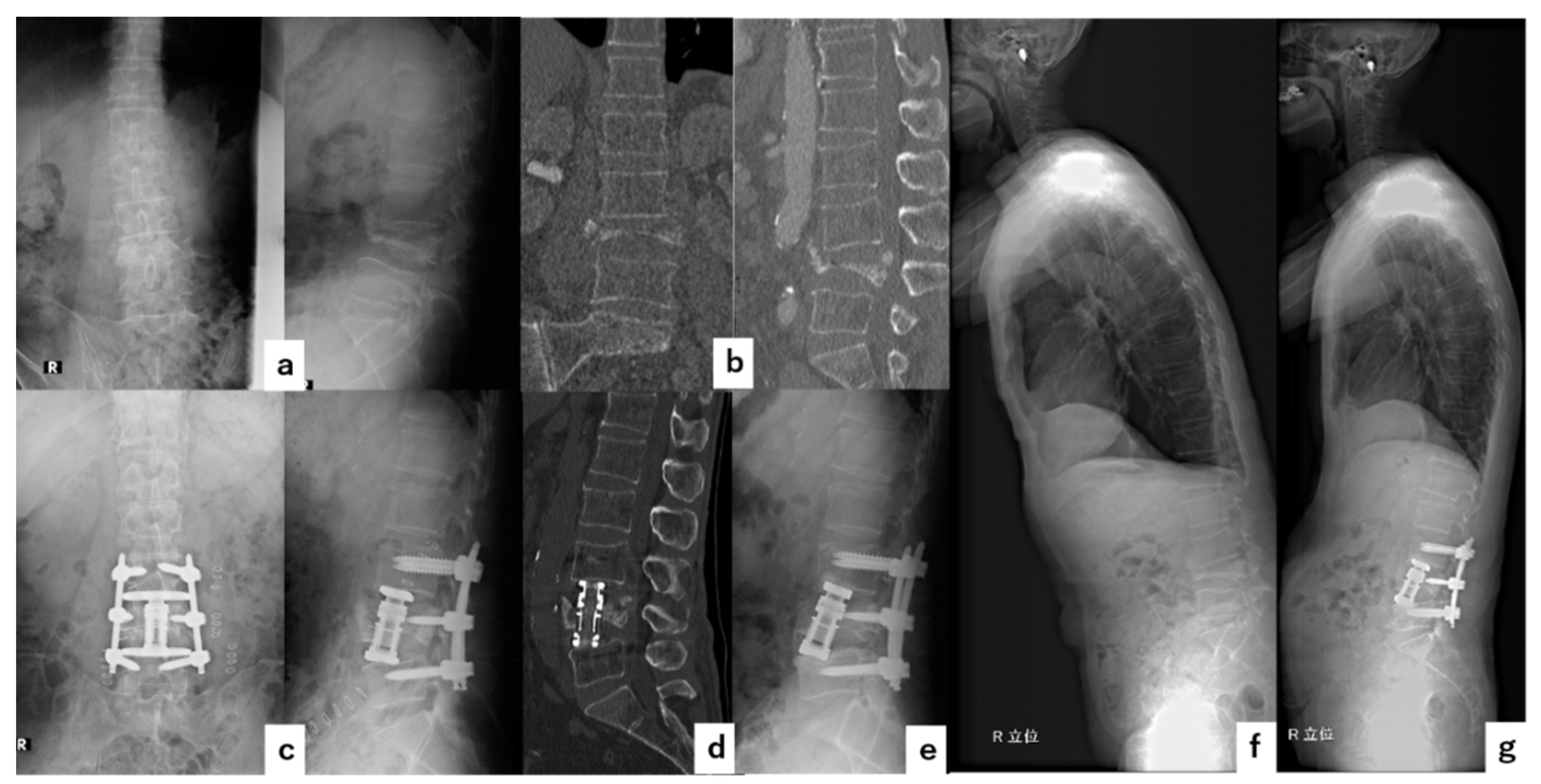
4. Illustrative Cases
4.1. Case 1
4.2. Case 2
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Lau, E.; Ong, K.; Kurtz, S.; Schmier, J.; Edidin, A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J. Bone Joint Surg. Am. 2008, 90, 1479–1486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bliuc, D.; Nguyen, N.D.; Milch, V.E.; Nguyen, T.V.; Eisman, J.A.; Center, J.R. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 2009, 301, 513–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosogane, N.; Nojiri, K.; Suzuki, S.; Funao, H.; Okada, E.; Isogai, N.; Ueda, S.; Hikata, T.; Shiono, Y.; Watanabe, K.; et al. Surgical Treatment of Osteoporotic Vertebral Fracture with Neurological Deficit-A Nationwide Multicenter Study in Japan. Spine Surg. Relat. Res. 2019, 3, 361–367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wardlaw, D.; Cummings, S.R.; Van Meirhaeghe, J.; Bastian, L.; Tillman, J.B.; Ranstam, J.; Eastell, R.; Shabe, P.; Talmadge, K.; Boonen, S. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): A randomised controlled trial. Lancet 2009, 373, 1016–1024. [Google Scholar] [CrossRef]
- Minamide, A.; Maeda, T.; Yamada, H.; Murakami, K.; Okada, M.; Enyo, Y.; Nakagawa, Y.; Iwasaki, H.; Tsutsui, S.; Takami, M.; et al. Early versus delayed kyphoplasty for thoracolumbar osteoporotic vertebral fractures: The effect of timing on clinical and radiographic outcomes and subsequent compression fractures. Clin. Neurol. Neurosurg. 2018, 173, 176–181. [Google Scholar] [CrossRef]
- Takahashi, S.; Hoshino, M.; Yasuda, H.; Hori, Y.; Ohyama, S.; Terai, H.; Hayashi, K.; Tsujio, T.; Kono, H.; Suzuki, A.; et al. Characteristic radiological findings for revision surgery after balloon kyphoplasty. Sci. Rep. 2019, 9, 18513. [Google Scholar] [CrossRef]
- Ito, M.; Harada, A.; Nakano, T.; Kuratsu, S.; Deguchi, M.; Sueyoshi, Y.; Machida, M.; Yonezawa, Y.; Matsuyama, Y.; Wakao, N. Retrospective multicenter study of surgical treatments for osteoporotic vertebral fractures. J. Orthop. Sci. 2010, 15, 289–293. [Google Scholar] [CrossRef]
- Watanabe, K.; Katsumi, K.; Ohashi, M.; Shibuya, Y.; Hirano, T.; Endo, N.; Kaito, T.; Yamashita, T.; Fujiwara, H.; Nagamoto, Y.; et al. Surgical outcomes of spinal fusion for osteoporotic vertebral fracture in the thoracolumbar spine: Comprehensive evaluations of 5 typical surgical fusion techniques. J. Orthop. Sci. 2019, 24, 1020–1026. [Google Scholar] [CrossRef]
- Kaneda, K.; Asano, S.; Hashimoto, T.; Satoh, S.; Fujiya, M. The treatment of osteoporotic-posttraumatic vertebral collapse using the Kaneda device and a bioactive ceramic vertebral prosthesis. Spine 1992, 17 (Suppl. 8), S295–S303. [Google Scholar] [CrossRef]
- Uchida, K.; Kobayashi, S.; Nakajima, H.; Kokubo, Y.; Yayama, T.; Sato, R.; Timbihurira, G.; Baba, H. Anterior expandable strut cage replacement for osteoporotic thoracolumbar vertebral collapse. J. Neurosurg. Spine. 2006, 4, 454–462. [Google Scholar] [CrossRef] [Green Version]
- Kanayama, M.; Ishida, T.; Hashimoto, T.; Shigenobu, K.; Togawa, D.; Oha, F.; Kaneda, K. Role of major spine surgery using Kaneda anterior instrumentation for osteoporotic vertebral collapse. J. Spinal Disord. Tech. 2010, 23, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Matsuyama, Y.; Goto, M.; Yoshihara, H.; Tsuji, T.; Sakai, Y.; Nakamura, H.; Sato, K.; Kamiya, M.; Ishiguro, N. Vertebral reconstruction with biodegradable calcium phosphate cement in the treatment of osteoporotic vertebral compression fracture using instrumentation. J. Spinal Disord. Tech. 2004, 17, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Sudo, H.; Ito, M.; Abumi, K.; Kotani, Y.; Takahata, M.; Hojo, Y.; Minami, A. One-stage posterior instrumentation surgery for the treatment of osteoporotic vertebral collapse with neurological deficits. Eur. Spine J. 2010, 19, 907–915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uchida, K.; Nakajima, H.; Yayama, T.; Miyazaki, T.; Hirai, T.; Kobayashi, S.; Chen, K.; Guerrero, A.R.; Baba, H. Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: Comparisons with posterior surgery without vertebroplasty and anterior surgery. J. Neurosurg. Spine 2010, 13, 612–621. [Google Scholar] [CrossRef]
- Kashii, M.; Yamazaki, R.; Yamashita, T.; Okuda, S.; Fujimori, T.; Nagamoto, Y.; Tamura, Y.; Oda, T.; Ohwada, T.; Yoshikawa, H.; et al. Surgical treatment for osteoporotic vertebral collapse with neurological deficits: Retrospective comparative study of three procedures--anterior surgery versus posterior spinal shorting osteotomy versus posterior spinal fusion using vertebroplasty. Eur. Spine J. 2013, 22, 1633–1642. [Google Scholar] [CrossRef] [Green Version]
- Sudo, H.; Ito, M.; Kaneda, K.; Abumi, K.; Kotani, Y.; Nagahama, K.; Minami, A.; Iwasaki, N. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J. 2013, 13, 1726–1732. [Google Scholar] [CrossRef]
- Nakashima, H.; Imagama, S.; Yukawa, Y.; Kanemura, T.; Kamiya, M.; Deguchi, M.; Wakao, N.; Sato, T.; Matsuzaki, K.; Yoshida, G.; et al. Comparative study of 2 surgical procedures for osteoporotic delayed vertebral collapse: Anterior and posterior combined surgery versus posterior spinal fusion with vertebroplasty. Spine 2015, 40, E120–E126. [Google Scholar] [CrossRef]
- Katsumi, K.; Hirano, T.; Watanabe, K.; Ohashi, M.; Yamazaki, A.; Ito, T.; Sawakami, K.; Sano, A.; Kikuchi, R.; Endo, N. Surgical treatment for osteoporotic thoracolumbar vertebral collapse using vertebroplasty with posterior spinal fusion: A prospective multicenter study. Int. Orthop. 2016, 40, 2309–2315. [Google Scholar] [CrossRef]
- Suk, S.I.; Chung, E.R.; Kim, J.H.; Kim, S.S.; Lee, J.S.; Choi, W.K. Posterior vertebral column resection for severe rigid scoliosis. Spine 2005, 30, 1682–1687. [Google Scholar] [CrossRef]
- Okuda, S.; Oda, T.; Yamasaki, R.; Haku, T.; Maeno, T.; Iwasaki, M. Surgical outcomes of osteoporotic vertebral collapse: A retrospective study of anterior spinal fusion and pedicle subtraction osteotomy. Global Spine J. 2012, 2, 221–226. [Google Scholar] [CrossRef] [Green Version]
- Takenaka, S.; Mukai, Y.; Hosono, N.; Fuji, T. Major surgical treatment of osteoporotic vertebral fractures in the elderly: A comparison of anterior spinal fusion, anterior-posterior combined surgery and posterior closing wedge osteotomy. Asian Spine J. 2014, 8, 322–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakashima, H.; Yukawa, Y.; Ito, K.; Machino, M.; Ishiguro, N.; Kato, F. Combined posterior-anterior surgery for osteoporotic delayed vertebral fracture with neurologic deficit. Nagoya J. Med. Sci. 2014, 76, 307–314. [Google Scholar] [PubMed]
- Sheng, X.; Ren, S. Surgical techniques for osteoporotic vertebral collapse with delayed neurological deficits: A systematic review. Int. J. Surg. 2016, 33 Pt A, 42–48. [Google Scholar] [CrossRef]
- Taiji, R.; Takami, M.; Yukawa, Y.; Hashizume, H.; Minamide, A.; Nakagawa, Y.; Nishi, H.; Iwasaki, H.; Tsutsui, S.; Okada, M.; et al. A short-segment fusion strategy using a wide-foot-plate expandable cage for vertebral pseudarthrosis after an osteoporotic vertebral fracture. J. Neurosurg. Spine 2020, 33, 862–869. [Google Scholar] [CrossRef] [PubMed]
- Terai, H.; Takahashi, S.; Yasuda, H.; Konishi, S.; Maeno, T.; Kono, H.; Matsumura, A.; Namikawa, T.; Kato, M.; Hoshino, M.; et al. Direct Lateral Corpectomy and Reconstruction Using an Expandable Cage Improves Local Kyphosis but Not Global Sagittal Alignment. J. Clin. Med. 2021, 10, 4012. [Google Scholar] [CrossRef]
- Podet, A.G.; Morrow, K.D.; Robichaux, J.M.; Shields, J.A.; DiGiorgio, A.M.; Tender, G.C. Minimally invasive lateral corpectomy for thoracolumbar traumatic burst fractures. Neurosurg. Focus 2020, 49, E12. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.J.; Blondel, B.; Bess, S.; Hostin, R.; Shaffrey, C.I.; Smith, J.S.; Boachie-Adjei, O.; Burton, D.C.; Akbarnia, B.A.; Mundis, G.M.; et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: A prospective multicenter analysis. Spine 2013, 38, E803–E812. [Google Scholar] [CrossRef] [Green Version]
- Tomycz, L.; Parker, S.L.; McGirt, M.J. Minimally invasive transpsoas L2 corpectomy and percutaneous pedicle screw fixation for osteoporotic burst fracture in the elderly: A technical report. J. Spinal Disord. Tech. 2015, 28, 53–60. [Google Scholar] [CrossRef]
- Walker, C.T.; Xu, D.S.; Godzik, J.; Turner, J.D.; Uribe, J.S.; Smith, W.D. Minimally invasive surgery for thoracolumbar spinal trauma. Ann. Transl. Med. 2018, 6, 102. [Google Scholar] [CrossRef] [Green Version]
- Huangxs, S.; Christiansen, P.A.; Tan, H.; Smith, J.S.; Shaffrey, M.E.; Uribe, J.S.; Shaffrey, C.I.; Yen, C.-P. Mini-Open Lateral Corpectomy for Thoracolumbar Junction Lesions. Oper. Neurosurg. 2020, 18, 640–647. [Google Scholar] [CrossRef]
- Mundis, G.M.; Eastlack, R.K.; Moazzaz, P.; Turner, A.W.; Cornwall, G.B. Contribution of Round vs. Rectangular Expandable Cage Endcaps to Spinal Stability in a Cadaveric Corpectomy Model. Int. J. Spine Surg. 2015, 9, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pekmezci, M.; McDonald, E.; Kennedy, A.; Dedini, R.; McClellan, T.; Ames, C.; Deviren, V. Can a novel rectangular footplate provide higher resistance to subsidence than circular footplates? An ex vivo biomechanical study. Spine 2012, 37, E1177–E1181. [Google Scholar] [CrossRef] [PubMed]
- Tamai, K.; Terai, H.; Suzuki, A.; Nakamura, H.; Watanabe, K.; Katsumi, K.; Ohashi, M.; Shibuya, Y.; Izumi, T.; Hirano, T.; et al. Risk Factors for Proximal Junctional Fracture Following Fusion Surgery for Osteoporotic Vertebral Collapse with Delayed Neurological Deficits: A Retrospective Cohort Study of 403 Patients. Spine Surg. Relat. Res. 2019, 3, 171–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Variables | Value | |
|---|---|---|
| Number of patients | 38 | |
| Age | 75.2 ± 7.4 (53–85) | |
| Gender (male/female) | 17/21 | |
| Follow-up period (months) | 21.2 ± 10.4 (12–51) | |
| Affected vertebra | Thoracolumbar junction level (T11-L2) | 27 (71.1%) |
| Lumbar level (L3-4) | 11 (28.9%) | |
| Sequence of surgery | A-P | 21 (55.3%) |
| P-A | 17 (44.7%) | |
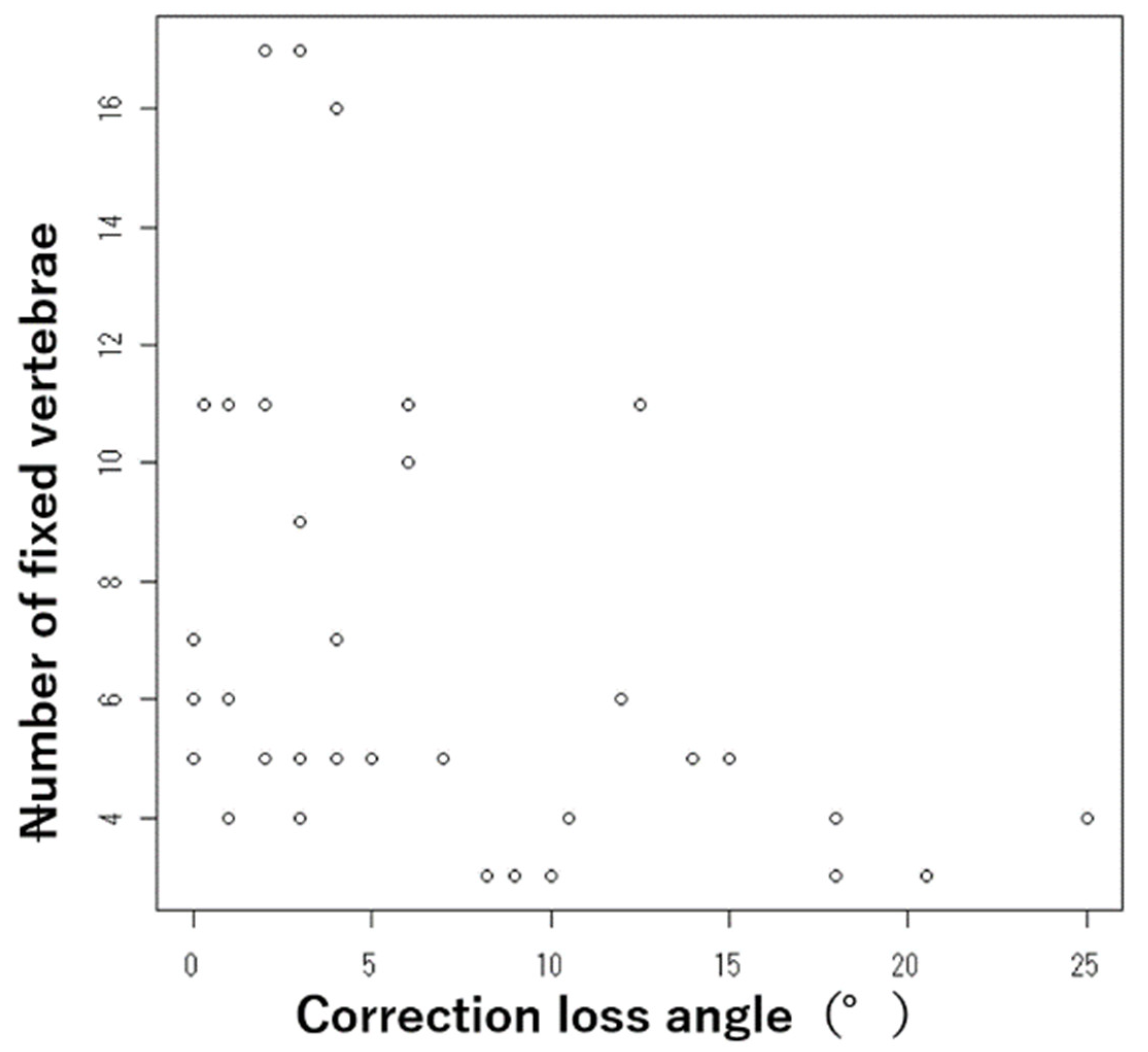
| Number of fixed vertebrae | 6.9 ± 3.9 (3–17) | |
| Local kyphotic angle (°) | Pre-operative angle | 29.3 ± 17.4(−21–62) |
| Correction loss angle | 4.9 ± 8.4 (−15–20) | |
| Mechanical failure (%) | UIV/LIV fracture | 12 (31.6%) |
| Cage subsidence | 10 (26.3%) | |
| PS loosening | 8 (21.1%) | |
| Cage floatation | 3 (7.9%) | |
| Endplate injury | 3 (7.9%) | |
| Adjacent vertebral fracture | 2 (5.3%) | |
| Variables | Cage Subsidence (+) | Cage Subsidence (−) | p-Value | |
|---|---|---|---|---|
| Number of patients | 10 | 28 | ||
| Age | 72.4 ± 8.5 | 76.1 ± 7.1 | 0.118 | |
| Gender (male/female) | 6/4 | 11/17 | 0.223 | |
| Follow-up period (months) | 25.8 ± 10.7 | 19.6 ± 10.1 | 0.083 | |
| Sequence of surgery (%) | A-P | 8 (80%) | 13 (46.4%) | 0.069 |
| P-A | 2 (20%) | 15 (53.6%) | ||
| Number of fixed vertebrae | 5.4 ± 4.5 | 7.4 ± 3.6 | 0.003 | |
| Variables | 5VG | 4LVG | p-Value | |
|---|---|---|---|---|
| Number of patients | 12 | 10 | ||
| Age | 75.6 ± 8.3 | 72.9 ± 9.8 | 0.39 | |
| Gender (male/female) | 2/10 | 6/4 | 0.048 | |
| Follow-up periods (months) | 15.8 ± 5.0 | 25.1 ± 15.8 | 0.017 | |
| Sequence of surgery (%) | A-P | 3 (25%) | 7 (70%) | 0.046 |
| P-A | 9 (75%) | 3 (30%) | ||
| Correction loss angle (°) | 4.8 ± 5.0 | 12.3 ± 7.8 | 0.016 | |
| Cage subsidence (%) | 0 (0%) | 8 (80%) | 0.0001 | |
| UIV/LIV fracture (%) | 8 (66.7%) | 4(40%) | 0.21 | |
| Adjacent vertebral fracture (%) | 1 (8.3%) | 0 (0%) | 0.55 | |
| Variables | Post-Operative Local Kyphosis <5° | Post-Operative Local Kyphosis ≥5 | p-Value | |
|---|---|---|---|---|
| Number of patients | 13 | 9 | ||
| Age | 77.2 ± 5.8 | 73.1 ± 9.7 | 0.226 | |
| Gender (male/female) | 7/6 | 1/8 | 0.052 | |
| Follow-up periods (months) | 19.4 ± 8.1 | 21.0 ± 9.2 | 0.784 | |
| Sequence of surgery (%) | A-P | 6 (46.2%) | 4 (44.4%) | 0.639 |
| P-A | 7 (53.8%) | 5 (55.6%) | ||
| Correction loss angle (°) | 7.0 ± 7.2 | 10.1 ± 7.4 | 0.299 | |
| Cage subsidence (%) | 4 (30.8%) | 4 (44.4%) | 0.246 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takeuchi, T.; Yamagishi, K.; Konishi, K.; Sano, H.; Takahashi, M.; Ichimura, S.; Kono, H.; Hasegawa, M.; Hosogane, N. Radiological Evaluation of Combined Anteroposterior Fusion with Vertebral Body Replacement Using a Minimally Invasive Lateral Approach for Osteoporotic Vertebral Fractures: Verification of Optimal Surgical Procedure. J. Clin. Med. 2022, 11, 629. https://doi.org/10.3390/jcm11030629
Takeuchi T, Yamagishi K, Konishi K, Sano H, Takahashi M, Ichimura S, Kono H, Hasegawa M, Hosogane N. Radiological Evaluation of Combined Anteroposterior Fusion with Vertebral Body Replacement Using a Minimally Invasive Lateral Approach for Osteoporotic Vertebral Fractures: Verification of Optimal Surgical Procedure. Journal of Clinical Medicine. 2022; 11(3):629. https://doi.org/10.3390/jcm11030629
Chicago/Turabian StyleTakeuchi, Takumi, Kenichiro Yamagishi, Kazumasa Konishi, Hideto Sano, Masato Takahashi, Shoichi Ichimura, Hitoshi Kono, Masaichi Hasegawa, and Naobumi Hosogane. 2022. "Radiological Evaluation of Combined Anteroposterior Fusion with Vertebral Body Replacement Using a Minimally Invasive Lateral Approach for Osteoporotic Vertebral Fractures: Verification of Optimal Surgical Procedure" Journal of Clinical Medicine 11, no. 3: 629. https://doi.org/10.3390/jcm11030629
APA StyleTakeuchi, T., Yamagishi, K., Konishi, K., Sano, H., Takahashi, M., Ichimura, S., Kono, H., Hasegawa, M., & Hosogane, N. (2022). Radiological Evaluation of Combined Anteroposterior Fusion with Vertebral Body Replacement Using a Minimally Invasive Lateral Approach for Osteoporotic Vertebral Fractures: Verification of Optimal Surgical Procedure. Journal of Clinical Medicine, 11(3), 629. https://doi.org/10.3390/jcm11030629





