Magnetic Resonance for Differential Diagnosis of Left Ventricular Hypertrophy: Diagnostic and Prognostic Implications
Abstract
:1. Introduction
2. Methods
2.1. LVH at Echocardiography
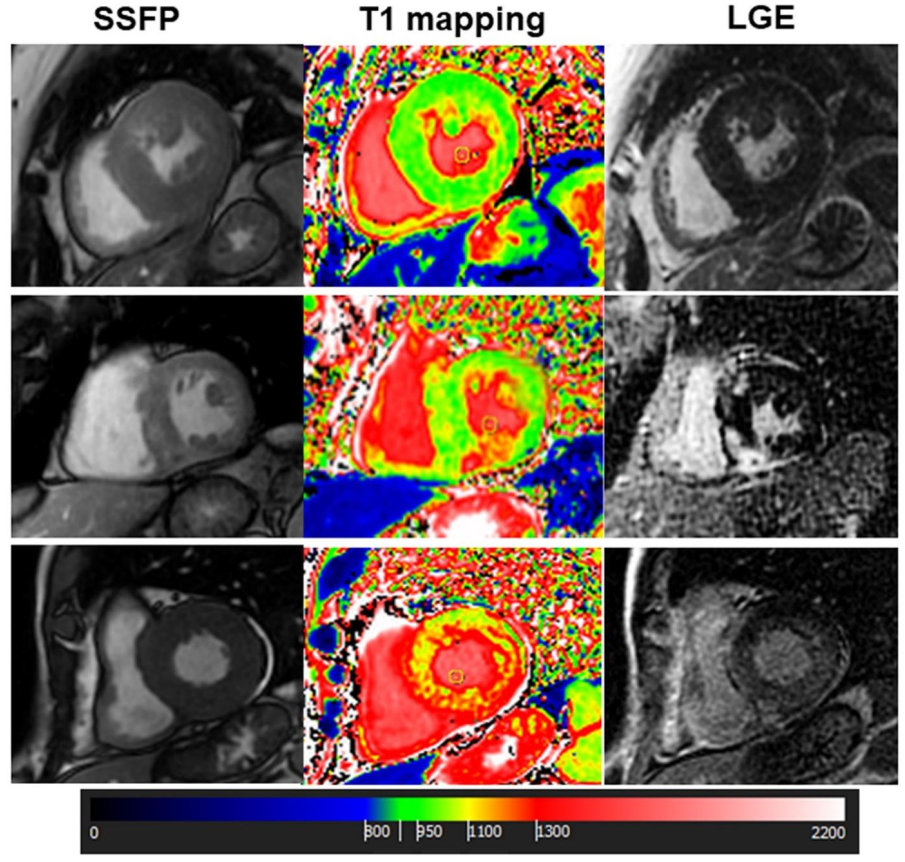
2.2. Cardiac Magnetic Resonance Evaluation
2.3. Additional Evaluation
2.4. Clinical Follow-Up
2.5. Statistical Analysis
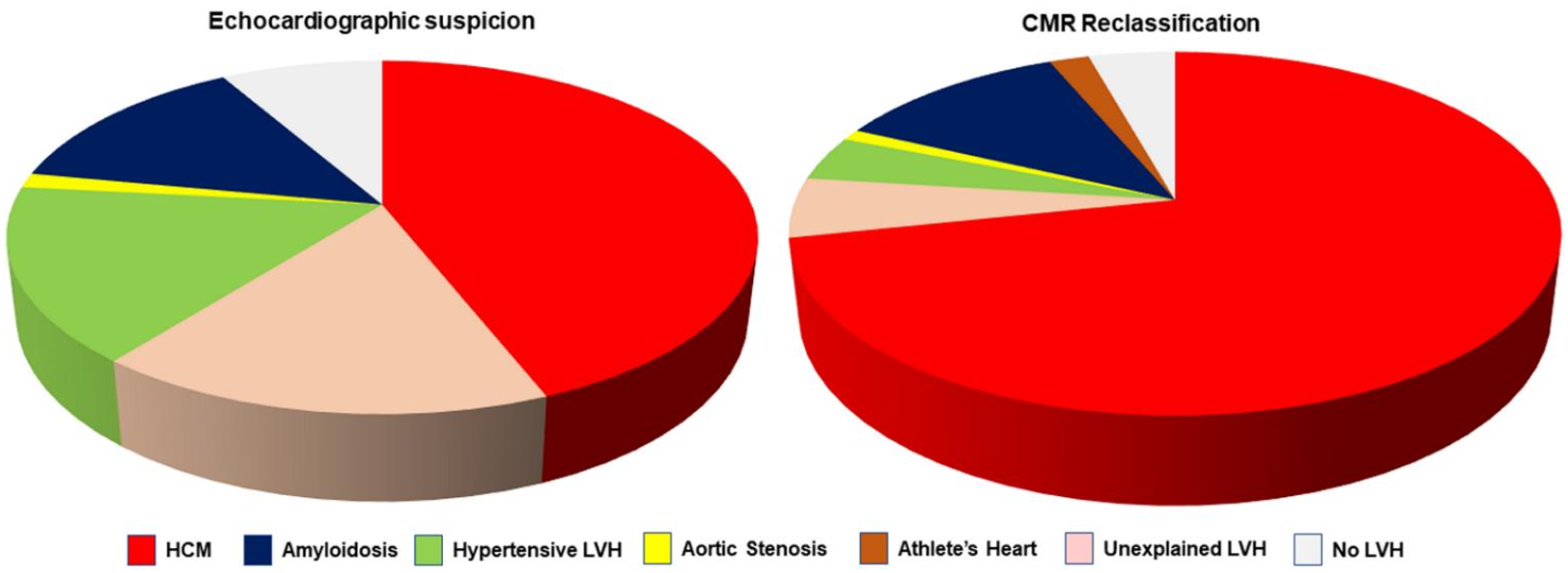
3. Results
3.1. Factors Determining CMR vs. TTE Changes in LVH Diagnosis
3.2. Clinical Follow-Up
4. Discussion
- In patients with LVH at echocardiography or with ECG signs of hypertrophic phenotype, CMR changed the initial echocardiographic suspicion in 42.3% cases, in particular changing the diagnosis of hypertensive LVH in 43% cases.
- The factors changing diagnosis were MWT measurement, the pattern of LVH. Average MWT was higher in CMR vs. echo. Tissue characterization with LGE and T1 mapping was also effective to identify HCM and cardiac amyloidosis.
- The final diagnosis by CMR was prognostically relevant, providing an accurate patient risk stratification in line with the type of diagnosis.
Limitations
5. Conclusions
Clinical Perspective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Levy, D.; Garrison, R.J.; Savage, D.D.; Kannel, W.B.; Castelli, W.P. Prognostic Implications of Echocardiographically Determined Left Ventricular Mass in the Framingham Heart Study. N. Engl. J. Med. 1990, 322, 1561–1566. [Google Scholar] [CrossRef] [PubMed]
- Devereux, R.B.; Roman, M.J. Left ventricular hypertrophy in hypertension: Stimuli, patterns, and consequences. Hypertens. Res. 1999, 22, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; Mahrholdt, H.; et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar] [PubMed]
- O’Mahony, C. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD). Eur. Heart J. 2014, 35, 2010–2020. [Google Scholar] [CrossRef]
- Moon, J.C.; Fisher, N.G.; McKenna, W.J.; Pennell, D.J. Detection of apical hypertrophic cardiomyopathy by cardiovascular magnetic resonance in patients with non-diagnostic echocardiography. Heart 2004, 90, 645–649. [Google Scholar] [CrossRef] [Green Version]
- Bottini, P.B.; Carr, A.A.; Prisant, L.M.; Flickinger, F.W.; Allison, J.D.; Gottdiener, J.S. Magnetic resonance imaging compared to echocardiography to assess left ventricular mass in the hypertensive patient. Am. J. Hypert. 1995, 8, 221–228. [Google Scholar] [CrossRef]
- Aquaro, G.D.; Positano, V.; Pingitore, A. Quantitative analysis of late gadolinium enhancement in hypertrophic cardiomiopathy. J. Cardiovasc. Magn. Reson. 2010, 7, 12–21. [Google Scholar]
- Burrage, M.K.; Ferreira, V.M. Cardiovascular magnetic resonance for the differentiation of left ventricualr hypertrophy. Curr. Heart Fail. Rep. 2020, 17, 192–204. [Google Scholar] [CrossRef]
- Karamitsos, T.D.; Arvanitaki, A.; Karvounis, H.; Neubauer, S.; Ferreira, V.M. Myocardial Tissue Characterization and Fibrosis by Imaging. JACC Cardiovasc. Imaging 2019, 13, 1221–1234. [Google Scholar] [CrossRef]
- Chan, R.H.; Maron, B.J.; Olivotto, I.; Pencina, M.J.; Assenza, G.E.; Haas, T.; Lesser, J.R.; Gruner, C.; Crean, A.M.; Rakowski, H.; et al. Prognostic Value of Quantitative Contrast-Enhanced Cardiovascular Magnetic Resonance for the Evaluation of Sudden Death Risk in Patients with Hypertrophic Cardiomyopathy. Circulation 2014, 130, 484–495. [Google Scholar] [CrossRef] [Green Version]
- Mahrholdt, H.; Wagner, A.; Judd, R.M.; Sechtem, U.; Kim, R.J. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur. Heart J. 2005, 26, 1461–1474. [Google Scholar] [CrossRef] [PubMed]
- Rickers, C.; Wilke, N.M.; Jerosch-Herold, M.; Casey, S.A.; Panse, P.; Panse, N.; Weil, J.; Zenovich, A.G.; Maron, B.J. Utility of cardiac magnetic resonance imaging in the diagnosis of hypertrophic cardiomyopathy. Circulation 2005, 112, 855–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bois, J.P.; Geske, J.B.; Foley, T.A.; Ommen, S.R.; Pellikka, P.A. Comparison of maximal wall thickness in hypertrophic cardiomyopathy differs between magnetic resonance imaging and transthoracic echocardiography. Am. J. Cardiol. 2017, 119, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Devlin, A.M.; Moore, N.R.; Ostman-Smith, I. A comparison of MRI and echocardiography in hypertrophic cardiomyopathy. Br. J. Radiol. 1999, 72, 258–264. [Google Scholar] [CrossRef]
- Hindieh, W.; Weissler-Snir, A.; Hammer, H.; Adler, A.; Rakowsku, H.; Chan, R.H. Discrepant measurements of maximal left ventricular wall thickness beteen cardiac magnetic resonance imaging and echocardiography in patients with hypertrophic cardiomyopathy. Circ. Cardiovasc. Imaging 2017, 10, e006309. [Google Scholar] [CrossRef] [Green Version]
- Sokolow, M.; Lyon, T.P. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am. Hear. J. 1949, 37, 161–186. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39. [Google Scholar] [CrossRef] [Green Version]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104, Correction in Eur. Heart J. 2019, 40, 475. [Google Scholar] [CrossRef]
- Falk, V.; Baumgartner, H.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Muñoz, D.R.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef]
- Pelliccia, A.; Maron, M.S.; Maron, B.J. Assessment of Left Ventricular Hypertrophy in a Trained Athlete: Differential Diagnosis of Physiologic Athlete’s Heart from Pathologic Hypertrophy. Prog. Cardiovasc. Dis. 2012, 54, 387–396. [Google Scholar] [CrossRef]
- Aquaro, G.D.; Camastra, G.; Monti, L.; Lombardi, M.; Pepe, A.; Castelletti, S.; Maestrini, V.; Todiere, G.; Masci, P.; Di Giovine, G.; et al. Working group “Applicazioni della Risonanza Magnetica” of the Italian Society of Cardiology.Reference values of cardiac volumes, dimensions, and new functional parameters by MR: A multicenter, multivendor study. J. Magn. Reson. Imaging 2017, 45, 1055–1067. [Google Scholar] [CrossRef]
- Kramer, C.M.; Barkhausen, J.; Bucciarelli-Ducci, C.; Flamm, S.D.; Kim, R.J.; Nagel, E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J. Cardiovasc. Magn. Reson. 2020, 22, 17. [Google Scholar] [CrossRef]
- Fontana, M.; Chung, R.; Hawkins, P.N.; Moon, J.C. Cardiovascular magnetic resonance for amyloidosis. Heart Fail. Rev. 2014, 20, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Massera, D.; McClelland, R.L.; Ambale-Venkatesh, B.; Gomes, A.S.; Hundley, W.G.; Kawel-Boehm, N.; Yoneyama, K.; Owens, D.S.; Garcia, M.J.; Sherrid, M.; et al. Prevalence of Unexplained Left Ventricular Hypertrophy by Cardiac Magnetic Resonance Imaging in MESA. J. Am. Heart Assoc. 2019, 8, e012250. [Google Scholar] [CrossRef] [PubMed]
- Syed, I.S.; Glockner, J.F.; Feng, D.; Araoz, P.A.; Martinez, M.W.; Edwards, W.D.; Gertz, M.A.; Dispenzieri, A.; Oh, J.K.; Bellavia, D.; et al. Role of Cardiac Magnetic Resonance Imaging in the Detection of Cardiac Amyloidosis. JACC Cardiovasc. Imaging 2010, 3, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Weng, Z.; Yao, J.; Chan, R.H.; He, J.; Yang, X.; Zhou, Y.; He, Y. Prognosis value of LGE-CMR in HCM: A meta-analysis. JACC Cardiovasc. Imaging 2016, 9, 1392–1402. [Google Scholar] [CrossRef]
- Todiere, G.; Aquaro, G.D.; Piaggi, P.; Formisano, F.; Barison, A.; Masci, P.G.; Strata, E.; Bacigalupo, L.; Marzilli, M.; Pingitore, A.; et al. Progression of myocardial fobrosis assessed with cardiac magnetic resonance in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2012, 10, 922–929. [Google Scholar] [CrossRef]
- Vakili, B.A.; Okin, P.M.; Devereux, R.B. Prognostic implications of left ventricular hypertrophy. Am. Heart J. 2001, 141, 334–341. [Google Scholar] [CrossRef]


| Age (year) | 56 ± 18 |
| Males, n (%) | 220 (73%) |
| Height (cm) | 171 ± 9 |
| Weight (kg) | 76 ± 14 |
| Hypertension, n (%) | 119 (40%) |
| Dyslipidaemia, n (%) | 64 (21%) |
| Diabetes, n (%) | 29 (10%) |
| Familial history of CAD, n (%) | 24 (8%) |
| Familial history of cardiomyopathy, n (%) | 17 (6%) |
| Familial history of SCD, n (%) | 23 (8%) |
| Atrial fibrillation, n (%) | 26 (9%) |
| Electrocardiographybnormalities: | 151(50%) |
| Sokolow LVH criteria, n (%) | 76 (25%) |
| T negative, n (%) | 89 (20%) |
| Left bundle branch block, n (%) | 9 (3%) |
| Low voltages on peripheral leads, n (%) | 4 (1%) |
| Short PR interval, n (%) | 2 (1%) |
| Echographic criteria of LVH, n (%) | 275 (92%) |
| LVH patterns at echo: | |
| Septal, n (%) | 131 (44%) |
| Concentric, n (%) | 127 (42%) |
| Septo-apical, n (%) | 2 (0.7%) |
| Apical, n (%) | 7 (2%) |
| Inferolateral, n (%) | 1 (0.3%) |
| Maximal wall thickness at echocardiography (mm) | 15 (13–18) |
| Diastolic dysfunction, n (%) | 193 (64%) |
| Grade 1, n (%) | 127 (42%) |
| Grade 2, n (%) | 37 (12%) |
| Grade 3, n (%) | 29 (10%) |
| LVOT obstruction, n (%) | 31 (10%) |
| Systolic dysfunction, n (%) | 35 (12%) |
| Aortic valvular stenosis, n (%) | 4 (1%) |
| CMR Reclassification: | ||||||||
|---|---|---|---|---|---|---|---|---|
| TTE Suspicion: | HCM | CA | Hypertensive LVH | Aortic Stenosis | Undetermined LVH | Athlete’s Heart | No LVH | Sum |
| HCM | 124 (94%) | 2 | 2 | 0 | 1 | 0 | 3 | 132 (44.0%) |
| CA | 9 | 23 (56%) | 2 | 0 | 5 | 0 | 2 | 41 (13.7%) |
| Hypertensive LVH | 36 | 3 | 8 (17%) | 0 | 0 | 0 | 1 | 48 (16.0%) |
| Aortic stenosis | 1 | 0 | 0 | 3 (75%) | 0 | 0 | 0 | 4 (1.4%) |
| Undetermined LVH | 28 | 7 | 0 | 0 | 9 (18%) | 4 | 2 | 50 (16.7%) |
| No LVH | 17 | 0 | 0 | 0 | 1 | 2 | 5 (20%) | 25 (8.3%) |
| 215 (71.7%) | 35 (11.7%) | 12 (4.0%) | 3 (1.0%) | 16 (5.0%) | 6 (2%) | 13 (4.3%) | 300 | |
| HCM (n = 215) | Amyloidosis (n = 35) | Hypertensive LVH (n = 12) | Athletes’s Heart (n = 6) | Aortic Stenosis (n = 3) | Undetermined LVH (n = 16) | p | |
|---|---|---|---|---|---|---|---|
| Age (years) | 56 ± 16 2,4 | 68 ± 11 1,4 | 60 ± 14 4 | 18 ± 5 * | 73 ± 17 4 | 50 ± 22 4 | <0.001 |
| Males, n (%) | 156 (73%) | 28 (80%) | 9 (75%) | 7 (100%) | 2 (67%) | 10 (67%) | 0.37 |
| Hypertension, n (%) | 92 (43%) 2,3 | 6 (17%) 1,3 | 12 (100%) 1,2,4,5 | 2 (29%) 3 | 2 (67%) | 0 3 | 0.007 |
| Diabetes, n (%) | 27 (13%) 2 | 0 1 | 1 (8%) | 0 | 0 | 0 | 0.84 |
| Dyslipidaemia, n (%) | 56 (26%) 6 | 4 (11%) | 3 (25%) | 0 | 1 (33%) | 0 1 | 0.45 |
| Family history of CAD, n (%) | 14 (7%) | 0 | 1 (8%) | 0 | 0 | 2 (13%) | 0.04 |
| ECG signs of LVH, n (%) | 25 (12%) 2 | 0 1,3 | 3 (25%) 2 | 0 | 1 (33%) | 2 (13%) | 0.29 |
| T negative, n (%) | 44 (20%) | 4 (11%) | 2 (17%) | 1 (14%) | 1 (33%) | 2 (13%) | 0.19 |
| Low voltages, n (%) | 02 | 4 (11%) 1 | 0 | 0 | 0 | 0 | 0.016 |
| Diastolic dysfunction: | <0.0001 | ||||||
| Grade 1, n (%) | 108 (50%) 2,4 | 5 (14%) 1,3 | 8 (67%) 2,4 | 0 1,3 | 2 (67%) | 4 (29%) | |
| Grade 2, n (%) | 17 (8%) 2 | 16 (46%) 1,4 | 2 (17%) | 0 2 | 0 | 2 (14%) | |
| Grade 3, n (%) | 15 (7%) 2 | 14 (40%) 1,3,5 | 0 2 | 0 | 0 | 0 2 | |
| CMR parameters | |||||||
| Max telediastolic wall thickness (mm) | 19 ± 4 | 19 ± 4 | 14 ± 2 | 13 ± 2 | 18 ± 2 | 15 ± 3 | 0.001 |
| LVEF (%) | 69 ± 11 2 | 54 ± 4 1,3,4,5 | 66 ± 14 2 | 70 ± 8 2 | 53 ± 12 | 68 ± 9 2 | <0.001 |
| LVEDVi (mL/mq) | 73 ± 19 | 76 ± 27 | 77 ± 23 | 97 ± 21 | 87 ± 27 | 77 ± 18 | 0.14 |
| Mass (g/mq) | 95 ± 26 | 115 ± 36 | 87 ± 26 | 104 ± 18 | 130 ± 37 | 96 ± 28 | <0.001 |
| RVEF (%) | 69 ± 9 2 | 53 ± 14 1 | 67 ± 13 | 66 ± 7 | 62 ± 9 | 65 ± 11 | <0.001 |
| RVEDVi (mL/mq) | 67 ± 17 4 | 66 ± 17 4 | 71 ± 17 | 105 ± 23 1,2 | 62 ± 10 | 80 ± 23 | <0.001 |
| Septal LVH, n (%) | 155 (72%) 2,4,5 | 8 (23%) 1 | 6 (50%) | 1 (14%) 1 | 1 (33%) | 4 (27%) 1 | <0.0001 |
| Septal apical LVH, n (%) | 12 (6%) | 0 | 0 | 0 | 0 | 0 | 0.83 |
| Apical LVH, n (%) | 18 (8%) | 0 | 0 | 0 | 0 | 0 | 0.58 |
| Concentric LVH, n (%) | 28 (13%) 2,3,4,5 | 26 (74%) 1 | 6 (50%) 1 | 5 (72%) 1 | 2 (67%) | 10 (67%) 1 | 0.88 |
| Inferior and inferolateral LVH, n (%) | 2 (1%) | 0 | 0 | 0 | 0 | 0 | 0.98 |
| Presence of LGE, n (%) | 163 (76%) 2,3,4,5 | 34 (97%) * | 0 1,2 | 0 1,2 | 1 (33%) 2 | 0 1,2 | <0.001 |
| Abnormal native T1 | 104 (48%) | 35 (100%) | 0 | 0 | 1(33%) | 0 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aquaro, G.D.; Corsi, E.; Todiere, G.; Grigoratos, C.; Barison, A.; Barra, V.; Di Bella, G.; Emdin, M.; Ricci, F.; Pingitore, A. Magnetic Resonance for Differential Diagnosis of Left Ventricular Hypertrophy: Diagnostic and Prognostic Implications. J. Clin. Med. 2022, 11, 651. https://doi.org/10.3390/jcm11030651
Aquaro GD, Corsi E, Todiere G, Grigoratos C, Barison A, Barra V, Di Bella G, Emdin M, Ricci F, Pingitore A. Magnetic Resonance for Differential Diagnosis of Left Ventricular Hypertrophy: Diagnostic and Prognostic Implications. Journal of Clinical Medicine. 2022; 11(3):651. https://doi.org/10.3390/jcm11030651
Chicago/Turabian StyleAquaro, Giovanni Donato, Elisabetta Corsi, Giancarlo Todiere, Crysanthos Grigoratos, Andrea Barison, Valerio Barra, Gianluca Di Bella, Michele Emdin, Fabrizio Ricci, and Alessandro Pingitore. 2022. "Magnetic Resonance for Differential Diagnosis of Left Ventricular Hypertrophy: Diagnostic and Prognostic Implications" Journal of Clinical Medicine 11, no. 3: 651. https://doi.org/10.3390/jcm11030651
APA StyleAquaro, G. D., Corsi, E., Todiere, G., Grigoratos, C., Barison, A., Barra, V., Di Bella, G., Emdin, M., Ricci, F., & Pingitore, A. (2022). Magnetic Resonance for Differential Diagnosis of Left Ventricular Hypertrophy: Diagnostic and Prognostic Implications. Journal of Clinical Medicine, 11(3), 651. https://doi.org/10.3390/jcm11030651







