Accuracy of Deep Learning Echocardiographic View Classification in Patients with Congenital or Structural Heart Disease: Importance of Specific Datasets
Abstract
:1. Introduction
2. Methods
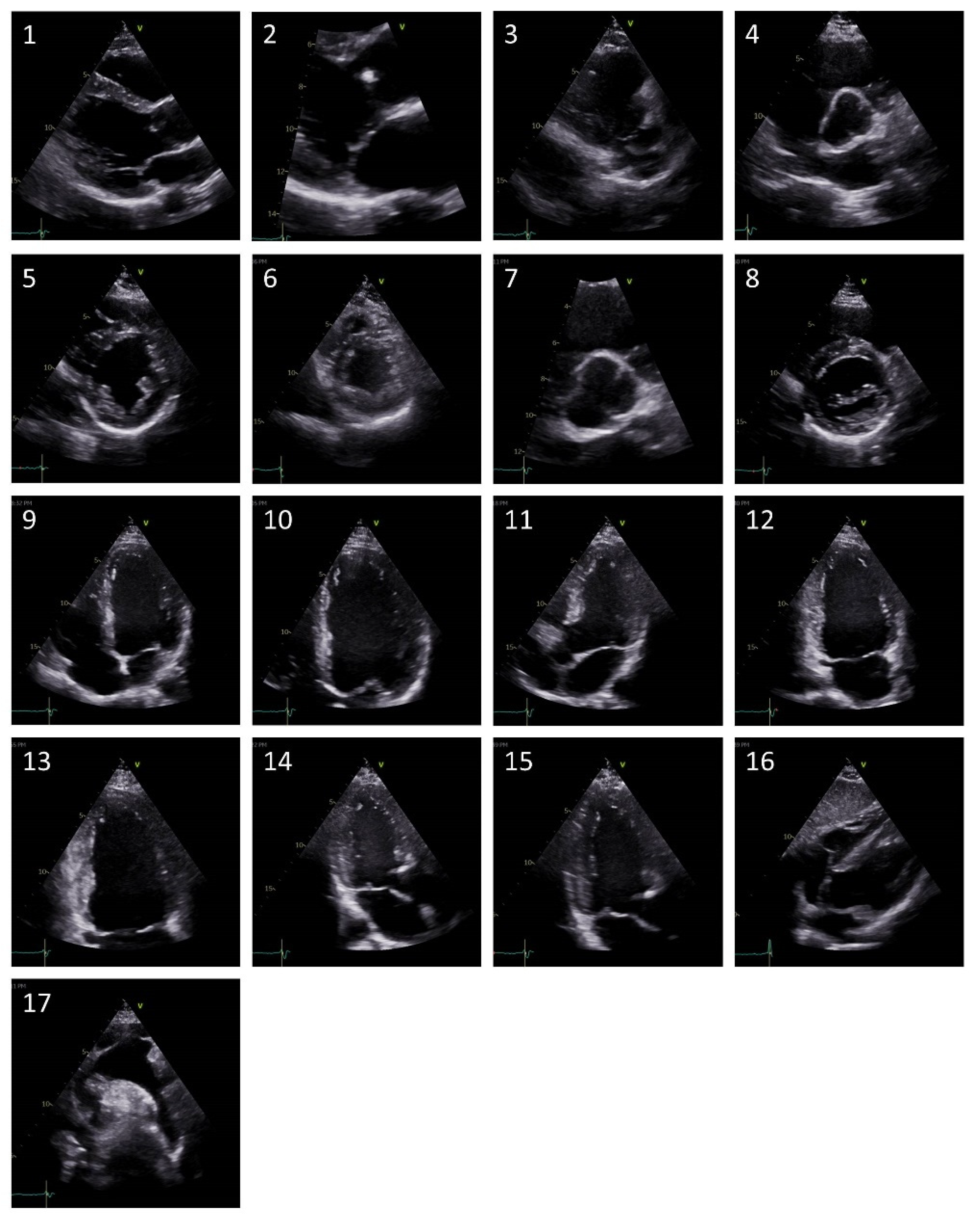
2.1. Imaging Database
2.2. Convolutional Neural Networks
2.3. Statistical Analysis
3. Results
3.1. Deep Neural Network (DNN) Trained with a General Dataset
3.2. DNN Trained with a Congenital or Structural Heart Disease (C/SHD)-Specific Dataset
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Mitchell, C.; Rahko, P.S.; Blauwet, L.A.; Canaday, B.; Finstuen, J.A.; Foster, M.C.; Horton, K.; Ogunyankin, K.O.; Palma, R.A.; Velazquez, E.J. Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2019, 32, 1–64. [Google Scholar] [CrossRef] [PubMed]
- Lauzier, P.T.; Avram, R.; Dey, D.; Slomka, P.; Afilalo, J.; Chow, B.J. The evolving role of artificial intelligence in cardiac image analysis. Can. J. Cardiol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, D.; He, B.; Ghorbani, A.; Yuan, N.; Ebinger, J.; Langlotz, C.P.; Heidenreich, P.A.; Harrington, R.A.; Liang, D.H.; Ashley, E.A.; et al. Video-based AI for beat-to-beat assessment of cardiac function. Nature 2020, 580, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Diller, G.-P.; Babu-Narayan, S.; Li, W.; Radojevic, J.; Kempny, A.; Uebing, A.; Dimopoulos, K.; Baumgartner, H.; Gatzoulis, M.A.; Orwat, S. Utility of machine learning algorithms in assessing patients with a systemic right ventricle. Eur. Heart. J. Cardiovasc. Imaging 2019, 20, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Al’Aref, S.J.; Anchouche, K.; Singh, G.; Slomka, P.J.; Kolli, K.K.; Kumar, A.; Pandey, M.; Maliakal, G.; van Rosendael, A.R.; Beecy, A.N.; et al. Clinical applications of machine learning in cardiovascular disease and its relevance to cardiac imaging. Eur. Heart J. 2019, 40, 1975–1986. [Google Scholar] [CrossRef] [PubMed]
- Narang, A.; Bae, R.; Hong, H.; Thomas, Y.; Surette, S.; Cadieu, C.; Chaudhry, A.; Martin, R.P.; McCarthy, P.M.; Rubenson, D.S.; et al. Utility of a Deep-Learning Algorithm to Guide Novices to Acquire Echocardiograms for Limited Diagnostic Use. JAMA Cardiol. 2021, 6, 624–632. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.; Bartko, P.; Geller, W.; Dannenberg, V.; König, A.; Binder, C.; Goliasch, G.; Hengstenberg, C.; Binder, T. A machine learning algorithm supports ultrasound-naïve novices in the acquisition of diagnostic echocardiography loops and provides accurate estimation of LVEF. Int. J. Cardiovasc. Imaging 2021, 37, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Boman, K.; Olofsson, M.; Berggren, P.; Sengupta, P.P.; Narula, J. Robot-assisted remote echocardiographic examination and teleconsultation: A randomized comparison of time to diagnosis with standard of care referral approach. JACC Cardiovasc. Imaging 2014, 7, 799–803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation: A Report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 16, 233–271. [Google Scholar]
- Chang, R.-K.R.; Gurvitz, M.; Rodriguez, S. Missed diagnosis of critical congenital heart disease. Arch. Pediatr. Adolesc. Med. 2008, 162, 969–974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Gajjala, S.; Agrawal, P.; Tison, G.H.; Hallock, L.A.; Beussink-Nelson, L.; Lassen, M.H.; Fan, E.; Aras, M.A.; Jordan, C.; et al. Fully Automated Echocardiogram Interpretation in Clinical Practice. Circulation 2018, 138, 1623–1635. [Google Scholar] [CrossRef] [PubMed]
- Azarmehr, N.; Ye, X.; Howard, J.P.; Lane, E.S.; Labs, R.; Shun-Shin, M.J.; Cole, G.D.; Bidaut, L.; Francis, D.P.; Zolgharni, M. Neural architecture search of echocardiography view classifiers. J. Med. Imaging (Bellingham) 2021, 8, 34002. [Google Scholar] [CrossRef] [PubMed]
- Madani, A.; Arnaout, R.; Mofrad, M.; Arnaout, R. Fast and accurate view classification of echocardiograms using deep learning. NPJ Digit. Med. 2018, 1, 6. [Google Scholar] [CrossRef] [PubMed]
- Diller, G.-P.; Kempny, A.; Alonso-Gonzalez, R.; Swan, L.; Uebing, A.; Li, W.; Babu-Narayan, S.; Wort, S.J.; Dimopoulos, K.; Gatzoulis, M.A. Survival Prospects and Circumstances of Death in Contemporary Adult Congenital Heart Disease Patients Under Follow-Up at a Large Tertiary Centre. Circulation 2015, 132, 2118–2125. [Google Scholar] [CrossRef] [Green Version]
- Baumgartner, H.; de Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.-P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef]
- Krittanawong, C.; Zhang, H.; Wang, Z.; Aydar, M.; Kitai, T. Artificial Intelligence in Precision Cardiovascular Medicine. J. Am. Coll. Cardiol. 2017, 69, 2657–2664. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.W.; Torres Soto, J.; Glicksberg, B.S.; Shameer, K.; Miotto, R.; Ali, M.; Ashley, E.; Dudley, J.T. Artificial Intelligence in Cardiology. J. Am. Coll. Cardiol. 2018, 71, 2668–2679. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liu, X.; Wang, F.; Zheng, L.; Gao, F.; Zhang, H.; Zhang, X.; Xie, W.; Wang, B. Automated interpretation of congenital heart disease from multi-view echocardiograms. Med. Image Anal. 2021, 69, 101942. [Google Scholar] [CrossRef] [PubMed]
| Diagnosis | Number (%) | Mean Age in Years | Male (%) |
|---|---|---|---|
| Ebstein anomaly | 18 (7%) | 40 | 14 (78%) |
| Hypoplastic left heart | 3 (1%) | 23 | 2 (67%) |
| Tricuspid atresia | 1 (<1%) | 36 | 1 (100%) |
| Non-compaction cardiomyopathy | 9 (3%) | 37 | 7 (78%) |
| Transposition of the great arteries (TGA) | 48 (18%) | 39 | 25 (52%) |
| Tetralogy of Fallot | 30 (11%) | 47 | 15 (50%) |
| Incomplete atrio-ventricular septal defect | 6 (2%) | 39 | 1 (17%) |
| Complete atrio-ventricular septal defect | 5 (2%) | 55 | 2 (40%) |
| Double outlet right ventricle | 1 (<1%) | 50 | 1 (100%) |
| Atrial septal defect | 7 (3%) | 37 | 4 (57%) |
| Amyloidosis | 23 (9%) | 68 | 20 (87%) |
| Hypertrophic obstructive cardiomyopathy | 7 (3%) | 58 | 3 (43%) |
| Fabry disease | 11 (4%) | 60 | 7 (64%) |
| Dilatative cardiomyopathy | 54 (21%) | 58 | 35 (65%) |
| Congenitally corrected TGA | 34 (13%) | 48 | 18 (53%) |
| Muscular ventricular septal defect | 5 (2%) | 42 | 1 (20%) |
| All patients | 262 | 49 ± 17 | 156 (60%) |
| General Algorithm Interpretation in % | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ground truth | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | other | |
| PLAX left ventricle (1) | 76.5 | 5.9 | 0.4 | 4.8 | 0.4 | 0.4 | 0.2 | 3.6 | 0.2 | 7.9 | |||||||||
| PLAX zoomed MV (2) | 33.3 | 33.3 | 33.3 | ||||||||||||||||
| PLAX RV inflow (3) | 18.2 | 40.9 | 18.2 | 4.5 | 9.1 | 4.5 | 4.5 | ||||||||||||
| PSAX focus on AV (4) | 6.5 | 0.7 | 69.9 | 0.3 | 0.3 | 4.794 | 8.2 | 0.3 | 8.9 | ||||||||||
| PSAX papillary muscles (5) | 7.7 | 2.7 | 5.4 | 63.0 | 0.8 | 0.3 | 3.8 | 0.5 | 0.3 | 0.3 | 0.3 | 10.2 | 4.8 | ||||||
| PSAX apex (6) | 9.6 | 0.8 | 3.2 | 59.7 | 3.2 | 1.6 | 0.8 | 11.3 | 2.4 | 7.3 | |||||||||
| PSAX zoomed AV (7) | 40.0 | 20.0 | 40.0 | ||||||||||||||||
| PSAX MV (8) | 20.8 | 0.4 | 2.0 | 7.5 | 33.8 | 0.5 | 0.4 | 11.3 | 0.5 | 1.1 | 0.2 | 0.5 | 0.2 | 10.7 | 0.2 | 10.0 | |||
| Apical 4 chamber (9) | 1.8 | 0.2 | 0.5 | 3.1 | 0.3 | 52.7 | 1.9 | 23.7 | 1.1 | 2.4 | 1.1 | 3.0 | 2.6 | 3.3 | |||||
| A4C zoomed left ventricle (10) | 2.8 | 2.8 | 4.7 | 0.5 | 10.4 | 62.7 | 0.5 | 10.4 | 0.5 | 0.9 | 0.5 | 3.3 | |||||||
| Apical 5 chamber (11) | 2.7 | 2.7 | 0.9 | 20.0 | 26.4 | 25.5 | 1.8 | 2.7 | 1.8 | 4.5 | 10.9 | ||||||||
| Apical 2 chamber (12) | 5.6 | 0.9 | 0.6 | 3.8 | 0.6 | 4.1 | 2.8 | 31.3 | 30 | 3.7 | 4.0 | 4.4 | 8.1 | ||||||
| A2C zoomed left ventricle (13) | 2.2 | 3.3 | 1.1 | 1.1 | 15.4 | 2.2 | 57.1 | 1.1 | 6.6 | 3.3 | 6.6 | ||||||||
| Apical 3 chamber (14) | 14.4 | 1.6 | 1.0 | 5.5 | 0.3 | 2.6 | 2.0 | 0.7 | 1.0 | 1.6 | 28.5 | 31.3 | 1.3 | 8.8 | |||||
| A3C zoomed left ventricle (15) | 11.1 | 11.1 | 11.1 | 11.1 | 11.1 | 44.4 | |||||||||||||
| Subcostal 4 chamber (16) | 0.5 | 1.0 | 1.0 | 1.5 | 0.5 | 87.7 | 7.8 | ||||||||||||
| Suprasternal aortic arch (17) | 1.9 | 17.9 | 6.0 | 6.0 | 1.5 | 19.4 | 34.3 | 13.0 | |||||||||||
| General Algorithm Interpretation in % | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ground truth | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | other | |
| PLAX left ventricle (1) | 98.4 | 1.6 | |||||||||||||||||
| PLAX zoomed MV (2) | 33.3 | 66.6 | |||||||||||||||||
| PLAX RV inflow (3) | 75.0 | 25.0 | |||||||||||||||||
| PSAX focus on AV (4) | 19.4 | 2.8 | 63.8 | 8.3 | 2.8 | 2.8 | |||||||||||||
| PSAX papillary muscles (5) | 7.2 | 1.0 | 2.0 | 1.0 | 79.4 | 6.2 | 3.1 | ||||||||||||
| PSAX apex (6) | 94.5 | 0 | 5.5 | ||||||||||||||||
| PSAX zoomed AV (7) | - | ||||||||||||||||||
| PSAX MV (8) | 10.6 | 2.1 | 2.1 | 4.3 | 48.9 | 19.1 | 10.6 | 2.1 | |||||||||||
| Apical 4 chamber (9) | 0.7 | 77.5 | 20.5 | 1.3 | |||||||||||||||
| A4C zoomed left ventricle (10) | 16.7 | 66.7 | 4.2 | 4.2 | 4.2 | 4.2 | |||||||||||||
| Apical 5 chamber (11) | 14.3 | 35.7 | 21.4 | 28.6 | |||||||||||||||
| Apical 2 chamber (12) | 57.1 | 21.4 | 21.4 | ||||||||||||||||
| A2C zoomed left ventricle (13) | 11.1 | 11.1 | 22.2 | 22.2 | 11.1 | 11.1 | 11.1 | ||||||||||||
| Apical 3 chamber (14) | 13.3 | 6.7 | 6.7 | 6.7 | 6.7 | 33.3 | 26.7 | ||||||||||||
| A3C zoomed left ventricle (15) | 66.7 | 33.3 | |||||||||||||||||
| Subcostal 4 chamber (16) | 100 | ||||||||||||||||||
| Suprasternal aortic arch (17) | 20.0 | 40.0 | 40.0 | ||||||||||||||||
| CSHD-Specific Algorithm Interpretation in % | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ground truth | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | other | |
| PLAX left ventricle (1) | 94 | 2 | 1 | 1 | 1 | 1 | |||||||||||||
| PLAX zoomed MV (2) | 94 | 5 | 1 | ||||||||||||||||
| PLAX RV inflow (3) | 1 | 80 | 1 | 9 | 3 | 4 | 2 | ||||||||||||
| PSAX focus on AV (4) | 2 | 3 | 88 | 2 | 1 | 3 | |||||||||||||
| PSAX papillary muscles (5) | 1 | 1 | 68 | 26 | 3 | 1 | 1 | ||||||||||||
| PSAX apex (6) | 2 | 48 | 6 | 2 | 26 | 6 | 6 | 3 | 6 | 1 | |||||||||
| PSAX zoomed AV (7) | |||||||||||||||||||
| PSAX MV (8) | 1 | 1 | 46 | 52 | |||||||||||||||
| Apical 4 chamber (9) | 1 | 1 | 91 | 4 | 1 | 1 | 1 | ||||||||||||
| A4C zoomed left ventricle (10) | 10 | 69 | 20 | 1 | |||||||||||||||
| Apical 5 chamber (11) | 21 | 1 | 78 | ||||||||||||||||
| Apical 2 chamber (12) | 6 | 6 | 80 | 5 | 2 | 1 | |||||||||||||
| A2C zoomed left ventricle (13) | 3 | 6 | 27 | 32 | 32 | ||||||||||||||
| Apical 3 chamber (14) | 4 | 3 | 2 | 3 | 88 | ||||||||||||||
| A3C zoomed left ventricle (15) | 3 | 90 | 7 | ||||||||||||||||
| Subcostal 4 chamber (16) | 100 | ||||||||||||||||||
| Suprasternal aortic arch (17) | 6 | 1 | 93 | ||||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wegner, F.K.; Benesch Vidal, M.L.; Niehues, P.; Willy, K.; Radke, R.M.; Garthe, P.D.; Eckardt, L.; Baumgartner, H.; Diller, G.-P.; Orwat, S. Accuracy of Deep Learning Echocardiographic View Classification in Patients with Congenital or Structural Heart Disease: Importance of Specific Datasets. J. Clin. Med. 2022, 11, 690. https://doi.org/10.3390/jcm11030690
Wegner FK, Benesch Vidal ML, Niehues P, Willy K, Radke RM, Garthe PD, Eckardt L, Baumgartner H, Diller G-P, Orwat S. Accuracy of Deep Learning Echocardiographic View Classification in Patients with Congenital or Structural Heart Disease: Importance of Specific Datasets. Journal of Clinical Medicine. 2022; 11(3):690. https://doi.org/10.3390/jcm11030690
Chicago/Turabian StyleWegner, Felix K., Maria L. Benesch Vidal, Philipp Niehues, Kevin Willy, Robert M. Radke, Philipp D. Garthe, Lars Eckardt, Helmut Baumgartner, Gerhard-Paul Diller, and Stefan Orwat. 2022. "Accuracy of Deep Learning Echocardiographic View Classification in Patients with Congenital or Structural Heart Disease: Importance of Specific Datasets" Journal of Clinical Medicine 11, no. 3: 690. https://doi.org/10.3390/jcm11030690
APA StyleWegner, F. K., Benesch Vidal, M. L., Niehues, P., Willy, K., Radke, R. M., Garthe, P. D., Eckardt, L., Baumgartner, H., Diller, G.-P., & Orwat, S. (2022). Accuracy of Deep Learning Echocardiographic View Classification in Patients with Congenital or Structural Heart Disease: Importance of Specific Datasets. Journal of Clinical Medicine, 11(3), 690. https://doi.org/10.3390/jcm11030690






