Neurodynamic Functions and Their Correlations with Postural Parameters in Adolescents with Idiopathic Scoliosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
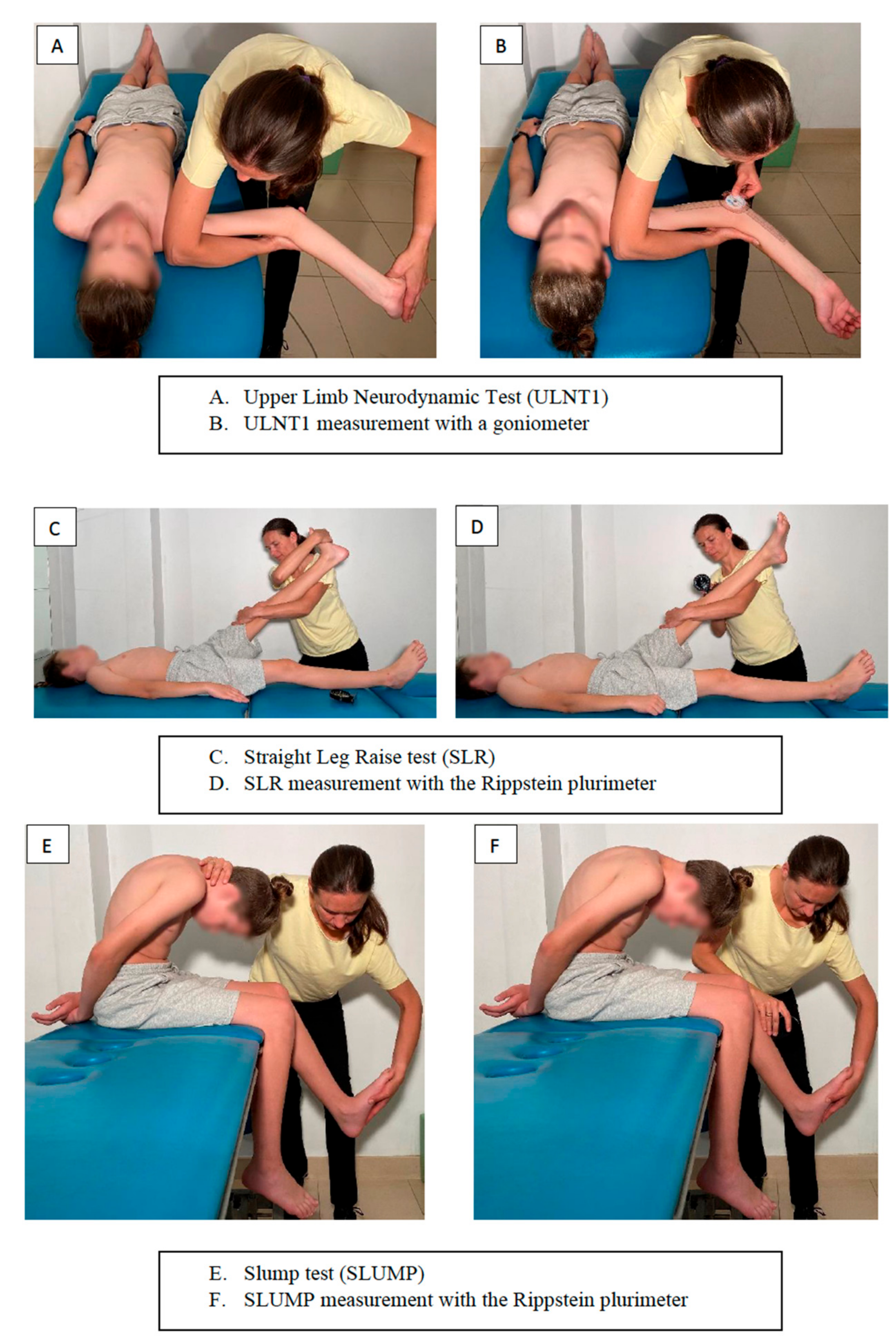
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Neurodynamic Tests, Postural Parameters, and Range of Motion
3.2. Correlations between Neurodynamic Tests and Postural Parameters
3.3. Neurodynamic Tests and Pain
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schlösser, T.P.C.; van der Heijden, G.J.M.G.; Versteeg, A.L.; Castelein, R.M. How ‘Idiopathic’ Is Adolescent Idiopathic Scoliosis? A Systematic Review on Associated Abnormalities. PLoS ONE 2014, 9, e97461. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT Guidelines: Orthopaedic and Rehabilitation Treatment of Idiopathic Scoliosis during Growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Shacklock, M. Clinical Neurodynamics: A New System of Neuromusculoskeletal Treatment, 1st ed.; Elsevier: Oxford, UK, 2005; ISBN 978-0-7506-5456-2. [Google Scholar]
- Ellis, R.; Carta, G.; Andrade, R.J.; Coppieters, M.W. Neurodynamics: Is Tension Contentious? J. Man. Manip. Ther. 2022, 30, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Butler, D.S. The Neurodynamic Techniques DVD and Handbook; NOI Group Publications: Haarlem, The Netherlands, 2005. [Google Scholar]
- Dwornik, M.; Kujawa, J.; Białoszewski, D.; Słupik, A.; Kiebzak, W. Electromyographic and Clinical Evaluation of the Efficacy of Neuromobilization in Patients with Low Back Pain. Ortop. Traumatol. Rehabil. 2009, 11, 164–176. [Google Scholar] [CrossRef] [PubMed]
- Basson, A.; Olivier, B.; Ellis, R.; Coppieters, M.; Stewart, A.; Mudzi, W. The Effectiveness of Neural Mobilization for Neuromusculoskeletal Conditions: A Systematic Review and Meta-Analysis. J. Orthop. Sports Phys. Ther. 2017, 47, 593–615. [Google Scholar] [CrossRef] [PubMed]
- Kleinrensink, G.J.; Stoeckart, R.; Mulder, P.G.; Hoek, G.; Broek, T.; Vleeming, A.; Snijders, C.J. Upper Limb Tension Tests as Tools in the Diagnosis of Nerve and Plexus Lesions. Anatomical and Biomechanical Aspects. Clin. Biomech. 2000, 15, 9–14. [Google Scholar] [CrossRef]
- Van der Heide, B.; Allison, G.T.; Zusman, M. Pain and Muscular Responses to a Neural Tissue Provocation Test in the Upper Limb. Man. Ther. 2001, 6, 154–162. [Google Scholar] [CrossRef]
- Majlesi, J.; Togay, H.; Unalan, H.; Toprak, S. The Sensitivity and Specificity of the Slump and the Straight Leg Raising Tests in Patients with Lumbar Disc Herniation. J. Clin. Rheumatol. 2008, 14, 87–91. [Google Scholar] [CrossRef]
- Boyd, B.S.; Wanek, L.; Gray, A.T.; Topp, K.S. Mechanosensitivity of the Lower Extremity Nervous System during Straight-Leg Raise Neurodynamic Testing in Healthy Individuals. J. Orthop. Sports Phys. Ther. 2009, 39, 780–790. [Google Scholar] [CrossRef]
- Walsh, J.; Hall, T. Agreement and Correlation between the Straight Leg Raise and Slump Tests in Subjects with Leg Pain. J. Manip. Physiol. Ther. 2009, 32, 184–192. [Google Scholar] [CrossRef]
- Ekedahl, H.; Jönsson, B.; Frobell, R.B. Fingertip-to-Floor Test and Straight Leg Raising Test: Validity, Responsiveness, and Predictive Value in Patients with Acute/Subacute Low Back Pain. Arch. Phys. Med. Rehabil. 2012, 93, 2210–2215. [Google Scholar] [CrossRef]
- Hines, T.; Noakes, R.; Manners, B. The Upper Limb Tension Test: Inter-Tester Reliability for Assessing the Onset of Passive Resistance R 1. J. Man. Manip. Ther. 1993, 1, 95–98. [Google Scholar] [CrossRef]
- Vanti, C.; Conteddu, L.; Guccione, A.; Morsillo, F.; Parazza, S.; Viti, C.; Pillastrini, P. The Upper Limb Neurodynamic Test 1: Intra- and Intertester Reliability and the Effect of Several Repetitions on Pain and Resistance. J. Manip. Physiol. Ther. 2010, 33, 292–299. [Google Scholar] [CrossRef]
- Oliver, G.S.; Rushton, A. A Study to Explore the Reliability and Precision of Intra and Inter-Rater Measures of ULNT1 on an Asymptomatic Population. Man. Ther. 2011, 16, 203–206. [Google Scholar] [CrossRef]
- Philip, K.; Lew, P.; Matyas, T.A. The Inter-Therapist Reliability of the Slump Test. Aust. J. Physiother. 1989, 35, 89–94. [Google Scholar] [CrossRef]
- Tucker, N.; Reid, D.; McNair, P. Reliability and Measurement Error of Active Knee Extension Range of Motion in a Modified Slump Test Position: A Pilot Study. J. Man. Manip. Ther. 2007, 15, E85–E91. [Google Scholar] [CrossRef]
- Hunt, D.G.; Zuberbier, O.A.; Kozlowski, A.J.; Robinson, J.; Berkowitz, J.; Schultz, I.Z.; Milner, R.A.; Crook, J.M.; Turk, D.C. Reliability of the Lumbar Flexion, Lumbar Extension, and Passive Straight Leg Raise Test in Normal Populations Embedded within a Complete Physical Examination. Spine 2001, 26, 2714–2718. [Google Scholar] [CrossRef]
- Marsico, P.; Tal-Akabi, A.; Van Hedel, H.J.A. Reliability and Practicability of the Straight Leg Raise Test in Children with Cerebral Palsy. Dev. Med. Child. Neurol. 2016, 58, 173–179. [Google Scholar] [CrossRef]
- Von Piekartz, H.J.M.; Schouten, S.; Aufdemkampe, G. Neurodynamic Responses in Children with Migraine or Cervicogenic Headache versus a Control Group. A Comparative Study. Man. Ther. 2007, 12, 153–160. [Google Scholar] [CrossRef]
- Sato, T.; Hirano, T.; Ito, T.; Morita, O.; Kikuchi, R.; Endo, N.; Tanabe, N. Back Pain in Adolescents with Idiopathic Scoliosis: Epidemiological Study for 43,630 Pupils in Niigata City, Japan. Eur. Spine J. 2011, 20, 274–279. [Google Scholar] [CrossRef]
- Théroux, J.; Le May, S.; Fortin, C.; Labelle, H. Prevalence and Management of Back Pain in Adolescent Idiopathic Scoliosis Patients: A Retrospective Study. Pain Res. Manag. 2015, 20, 153–157. [Google Scholar] [CrossRef]
- Wong, A.Y.L.; Samartzis, D.; Cheung, P.W.H.; Yin Cheung, J.P. How Common Is Back Pain and What Biopsychosocial Factors Are Associated With Back Pain in Patients With Adolescent Idiopathic Scoliosis? Clin. Orthop. Relat. Res. 2019, 477, 676–686. [Google Scholar] [CrossRef]
- Teles, A.R.; St-Georges, M.; Abduljabbar, F.; Simões, L.; Jiang, F.; Saran, N.; Ouellet, J.A.; Ferland, C.E. Back Pain in Adolescents with Idiopathic Scoliosis: The Contribution of Morphological and Psychological Factors. Eur. Spine J. 2020, 29, 1959–1971. [Google Scholar] [CrossRef]
- Balagué, F.; Pellisé, F. Adolescent Idiopathic Scoliosis and Back Pain. Scoliosis Spinal Disord. 2016, 11, 27. [Google Scholar] [CrossRef]
- Negrini, S.; Grivas, T.B.; Kotwicki, T.; Maruyama, T.; Rigo, M.; Weiss, H.R.; Members of the Scientific society On Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT). Why Do We Treat Adolescent Idiopathic Scoliosis? What We Want to Obtain and to Avoid for Our Patients. SOSORT 2005 Consensus Paper. Scoliosis 2006, 1, 4. [Google Scholar] [CrossRef]
- Côté, P.; Kreitz, B.G.; Cassidy, J.D.; Dzus, A.K.; Martel, J. A Study of the Diagnostic Accuracy and Reliability of the Scoliometer and Adam’s Forward Bend Test. Spine 1998, 23, 796–802; discussion 803. [Google Scholar] [CrossRef]
- Grivas, T.B.; Vasiliadis, E.S.; Koufopoulos, G.; Segos, D.; Triantafyllopoulos, G.; Mouzakis, V. Study of Trunk Asymmetry in Normal Children and Adolescents. Scoliosis 2006, 1, 19. [Google Scholar] [CrossRef]
- Kluszczyński, M.; Czernicki, J.; Kubacki, J. The Plurimetric Assessment Of Spinal Curvature Changes In The Sagittal Plane In Children And Youths, Measured During 10 Years’ Observation. Adv. Rehabil. 2013, 27, 1–8. [Google Scholar] [CrossRef]
- Stolinski, L.; Kozinoga, M.; Czaprowski, D.; Tyrakowski, M.; Cerny, P.; Suzuki, N.; Kotwicki, T. Two-Dimensional Digital Photography for Child Body Posture Evaluation: Standardized Technique, Reliable Parameters and Normative Data for Age 7–10 Years. Scoliosis Spinal Disord 2017, 12, 38. [Google Scholar] [CrossRef]
- Norkin, C.C.; White, D.J. Measurement of Joint Motion: A Guide to Goniometry, 5th ed.; F.A. Davis Company: Philadelphia, PA, USA, 2016; ISBN 978-0-8036-4566-0. [Google Scholar]
- Stępień, A.; Jędrzejowska, M.; Guzek, K.; Rekowski, W.; Stępowska, J. Reliability of Four Tests to Assess Body Posture and the Range of Selected Movements in Individuals with Spinal Muscular Atrophy. BMC Musculoskelet Disord. 2019, 20, 54. [Google Scholar] [CrossRef]
- Stępień, A.; Guzek, K.; Rekowski, W.; Radomska, I.; Stępowska, J. Assessment of the Lumbo-Pelvic-Hip Complex Mobility with the Trunk-Pelvis-Hip Angle Test: Intraobserver Reliability and Differences in Ranges of Motion between Girls with Idiopathic Scoliosis and Their Healthy Counterparts. Adv. Rehabil. 2020, 30, 27–39. [Google Scholar] [CrossRef]
- Stępień, A.; Fabian, K.; Graff, K.; Podgurniak, M.; Wit, A. An Immediate Effect of PNF Specific Mobilization on the Angle of Trunk Rotation and the Trunk-Pelvis-Hip Angle Range of Motion in Adolescent Girls with Double Idiopathic Scoliosis-a Pilot Study. Scoliosis Spinal Disord. 2017, 12, 29. [Google Scholar] [CrossRef]
- Perret, C.; Poiraudeau, S.; Fermanian, J.; Colau, M.M.; Benhamou, M.A.; Revel, M. Validity, Reliability, and Responsiveness of the Fingertip-to-Floor Test. Arch. Phys. Med. Rehabil. 2001, 82, 1566–1570. [Google Scholar] [CrossRef] [PubMed]
- Mukaka, M.M. Statistics Corner: A Guide to Appropriate Use of Correlation Coefficient in Medical Research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar] [PubMed]
- World Health Organization. Adolescent Health; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Thakur, R.; Gautam, R. Differential Onset of Puberty and Adolescence among Girls and Boys of a Central Indian Town (Sagar). Orient Anthropol. 2017, 17, 137–147. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The Age of Adolescence. Lancet Child Adolesc. Health 2018, 2, 223–228. [Google Scholar] [CrossRef]
- Boyd, B.S. Measurement Properties of a Hand-Held Inclinometer during Straight Leg Raise Neurodynamic Testing. Physiotherapy 2012, 98, 174–179. [Google Scholar] [CrossRef]
- Stalioraitis, V.; Robinson, K.; Hall, T. Side-to-Side Range of Movement Variability in Variants of the Median and Radial Neurodynamic Test Sequences in Asymptomatic People. Man. Ther. 2014, 19, 338–342. [Google Scholar] [CrossRef]
- Burkus, M.; Schlégl, Á.T.; O’Sullivan, I.; Márkus, I.; Vermes, C.; Tunyogi-Csapó, M. Sagittal Plane Assessment of Spino-Pelvic Complex in a Central European Population with Adolescent Idiopathic Scoliosis: A Case Control Study. Scoliosis Spinal Disord. 2018, 13, 10. [Google Scholar] [CrossRef]
- Schlösser, T.P.C.; Shah, S.A.; Reichard, S.J.; Rogers, K.; Vincken, K.L.; Castelein, R.M. Differences in Early Sagittal Plane Alignment between Thoracic and Lumbar Adolescent Idiopathic Scoliosis. Spine J. 2014, 14, 282–290. [Google Scholar] [CrossRef]
- Czaprowski, D.; Kotwicki, T.; Pawłowska, P.; Stoliński, L. Joint Hypermobility in Children with Idiopathic Scoliosis: SOSORT Award 2011 Winner. Scoliosis 2011, 6, 22. [Google Scholar] [CrossRef]
- Stępień, A. A Range of Rotation of the Trunk and Pelvis in Girls with Idiopathic Scoliosis. Adv. Rehabil. 2011, 25, 5–12. [Google Scholar] [CrossRef]
- Burwell, R.G.; Cole, A.A.; Cook, T.A.; Grivas, T.B.; Kiel, A.W.; Moulton, A.; Thirlwall, A.S.; Upadhyay, S.S.; Webb, J.K.; Wemyss-Holden, S.A. Pathogenesis of Idiopathic Scoliosis. The Nottingham Concept. Acta Orthop. Belg. 1992, 58 (Suppl. 1), 33–58. [Google Scholar]
- Watson, K.D.; Papageorgiou, A.C.; Jones, G.T.; Taylor, S.; Symmons, D.P.M.; Silman, A.J.; Macfarlane, G.J. Low Back Pain in Schoolchildren: Occurrence and Characteristics. Pain 2002, 97, 87–92. [Google Scholar] [CrossRef]
- Calvo-Muñoz, I.; Gómez-Conesa, A.; Sánchez-Meca, J. Prevalence of Low Back Pain in Children and Adolescents: A Meta-Analysis. BMC Pediatr. 2013, 13, 14. [Google Scholar] [CrossRef]
- Kędra, A.; Czaprowski, D. Epidemiology of Back Pain in Children and Youth Aged 10–19 from the Area of the Southeast of Poland. BioMed Res. Int. 2013, 2013, 506823. [Google Scholar] [CrossRef][Green Version]



| Characteristics | Idiopathic Scoliosis (n = 69) | Control Group (n = 57) | p |
|---|---|---|---|
| Age [years] | 0.410 | ||
| Median ± Q (range) | 13.0 ± 1.5 (11.0–14.0) | 12.0 ± 1.5 (11.0–14.0) | |
| Mean ± SD (range) | 12.7 ± 1.7 (10.0–15.0) | 12.4 ± 1.7 (10.0–15.0) | |
| Body mass [kg] | 0.944 | ||
| Median ± Q (range) | 49.0 ± 5.0 (44.0–54.0) | 48.0 ± 7.5 (40.0–55.0) | |
| Mean ± SD (range) | 48.0 ± 10.2 (28.0–71.0) | 47.9 ± 12.0 (29.0–75.0) | |
| Body height [cm] | 0.815 | ||
| Median ± Q (range) | 160.0 ± 6.5 (154.0–167.0) | 162.0 ± 10.0 (148.0–168.0) | |
| Mean ± SD (range) | 159.3 ± 10.9 (132.0–181.0) | 158.8 ± 12.5 (136.0 –186.0) | |
| Gender n (%) | |||
| Girls | 57 (82.6%) | 42 (73.7%) | |
| Boys | 12 (17.4%) | 15 (26.3%) | |
| Cobb angle [°] | |||
| Double scoliosis Th | n = 54 (78.3%) | ||
| Median ± Q (range) | 22.5 ± 6.5 (20.0–33.0) | ||
| Mean ± SD (range) | 26.1 ± 12.6 (11.0–69.0) | ||
| Double scoliosis L | n = 54 (78.3%) | ||
| Median ± Q (range) | 23.00 ± 7.50 (15.0–30.0) | ||
| Mean ± SD (range) | 24.8 ± 11.5 (11.0–68.0) | ||
| Single scoliosis ThL | n = 15 (21.7%) | ||
| Median ± Q (range) | 16.0 ± 5.0 (15.0–25.0) | ||
| Mean ± SD (range) | 24.9 ± 11.5 (11.0–45.0) | ||
| Physiotherapy | 54 (78.3%) | 18 (31.6%) | <0.001 |
| (last year) n (%) | |||
| Brace n (%) | 25 (36.2%) | - | |
| Pain (last 3 months) n (%) | 26 (37.7%) | 7 (12.3%) | 0.001 |
| Head | |||
| Back pain | 3 (4.3%) | 0 (0.0%) | |
| Cervical spine | 20 (29.0%) | 6 (10.5%) | |
| Thoracic spine | 5 (7.2%) | 0 (0.0%) | |
| Lumbar spine | 12 (17.4%) | 4 (7.0%) | |
| Upper limbs | 15 (21.7%) | 4 (7.0%) | |
| Lower limbs | 1 (1.4%) | 0 (0.0%) | |
| Several body parts | 4 (5.8%) | 2 (3.5%) | |
| 13 (18.8%) | 3 (5.3%) |
| Measurements | Idiopathic Scoliosis (n = 69) | Control Group (n = 57) | p | ||
|---|---|---|---|---|---|
| Median ± Q | Mean ± SD | Median ± Q | Mean ± SD | ||
| Neurodynamic tests (°) | |||||
| ULNT1left | 5.0 ± 15.0 *** | 14.3 ± 17.2 | 0.0 ± 0.0 | 4.9 ± 11.3 | <0.001 |
| ULNT1right | 5.0 ± 15.0 ** | 14.9 ± 17.4 | 0.0 ± 0.0 | 6.0 ± 12.9 | 0.002 |
| SLRleft | 58.0 ± 15.0 | 55.7 ± 15.2 | 60.0 ± 17.5 | 58.6 ± 19.0 | 0.323 |
| SLRright | 58.0 ± 15.0 | 55.3 ± 18.00 | 60.0 ± 17.0 | 58.3 ± 19.4 | 0.304 |
| SLUMPleft | 35.0 ± 22.0 *** | 32.7 ± 16.7 | 18.0 ± 12.0 | 22.1 ± 15.7 | <0.001 |
| SLUMPright | 36.0 ± 21.5 *** | 33.4 ± 15.5 | 17.0 ± 11.3 | 22.8 ± 16.8 | <0.001 |
| Postural parameters (°) | |||||
| ATRT | 6.0 ± 3.5 *** | 6.9 ± 4.9 | 2.0 ± 1.5 | 2.0 ± 1.9 | <0.001 |
| ATRL | 4.0 ± 2.0 *** | 4.2 ± 3.8 | 1.0 ± 1.0 | 1.4 ± 1.7 | <0.001 |
| Sternum | 24.0 ± 2.5 | 25.3 ± 5.6 | 27.0 ± 3.5 | 26.7 ± 5.6 | 0.064 |
| C | 24.0 ± 5.0 | 24.7 ± 6.3 | 24.0 ± 3.0 | 25.7 ± 6.0 | 0.284 |
| T1 | 13.0 ± 3.5 ** | 13.2 ± 6.1 | 16.0 ± 3.0 | 16.5 ± 5.0 | 0.001 |
| T2 | 12.0 ± 4.0 ** | 12.3 ± 5.5 | 14.0 ± 3.0 | 14.8 ± 4.7 | 0.009 |
| LS | 20.0 ± 3.5 | 20.2 ± 5.2 | 20.0 ± 4.0 | 19.7 ± 5.8 | 0.331 |
| Ranges of motion | |||||
| FTF (cm) | 0.0 ± 6.5 | 6.5 ± 8.1 | 0.0 ± 5.5 | 5.9 ± 7.3 | 0.735 |
| CRleft (°) | 34.0 ± 4.0 | 32.9 ± 7.1 | 34.0 ± 3.0 | 32.7 ± 4.9 | 0.412 |
| CRright (°) | 30.0 ± 3.5 | 30.2 ±7.3 | 31.0 ± 3.0 | 30.1 ± 5.6 | 0.549 |
| HEleft (°) | 22.0 ± 2.0 | 23.4 ± 4.2 | 22.0 ± 2.0 | 22.05 ± 5.7 | 0.142 |
| HEright (°) | 22.0 ± 3.0 | 23.0 ± 5.6 | 22.0 ± 2.0 | 22.2 ± 5.6 | 0.205 |
| HFleft (°) | 68.0 ± 11.0 | 64.1 ± 14.8 | 66.0 ± 12.0 | 63.7 ± 16.2 | 0.943 |
| HFright (°) | 70.0 ± 11.0 | 65.0 ± 15.2 | 66.0 ± 12.0 | 63.8 ± 16.6 | 0.737 |
| TPHAleft (°) | 12.0 ± 2.0 | 11.9 ± 6.0 | 12.0 ± 2.0 | 12.1 ± 3.6 | 0.941 |
| TPHAright (°) | 10.0 ± 5.0 | 8.3 ± 9.4 | 10.0 ± 3.0 | 10.7 ± 5.8 | 0.165 |
| JHM score | 3.5 ± 1.5 ** | 3.5 ± 2.3 | 2.0 ± 1.5 | 2.3 ± 2.4 | 0.001 |
| Idiopathic Scoliosis (n = 69) | ||||||
| ULNT1 Left | ULNT1 Right | SLR Left | SLR Right | SLUMP Left | SLUMP Right | |
| ULNT1 right | 0.665 *** | – | – | – | – | – |
| SLR left | −0.518 *** | −0.497 *** | – | – | – | – |
| SLR right | −0.506 *** | −0.529 *** | 0.950 *** | – | – | – |
| SLUMP left | 0.313 ** | 0.432 ** | −0.575 *** | −0.524 *** | – | – |
| SLUMP right | 0.383 ** | 0.462 ** | −0.545 *** | −0.514 *** | 0.900 *** | – |
| Cobb angle | 0.016 | −0.073 | 0.197 | 0.177 | −0.176 | −0.126 |
| Age | 0.370 ** | 0.215 | −0.113 | −0.112 | −0.014 | 0.090 |
| Body mass | 0.226 | 0.115 | −0.186 | −0.176 | 0.030 | 0.102 |
| Body height | 0.325 ** | 0.217 | −0.212 | −0.184 | 0.118 | 0.189 |
| Control Group (n = 57) | ||||||
| ULNT1 Left | ULNT1 Right | SLR Left | SLR Right | SLUMP Left | SLUMP Right | |
| ULNT1 right | 0.928 *** | – | – | – | – | – |
| SLR left | −0.589 *** | −0.625 *** | – | – | – | – |
| SLR right | −0.601 *** | −0.622 *** | 0.979 *** | – | – | – |
| SLUMP left | 0.384 ** | 0.423 ** | −0.650 *** | −0.644 *** | – | – |
| SLUMP right | 0.373 ** | 0.426 ** | −0.636 *** | −0.624 *** | 0.976 *** | – |
| Age | 0.140 | 0.147 | −0.239 | −0.218 | 0.190 | 0.184 |
| Body mass | 0.199 | 0.215 | −0.321 * | −0.300 * | 0.045 | 0.040 |
| Body height | 0.216 | 0.260 | −0.316 * | −0.298 * | 0.137 | 0.148 |
| Idiopathic Scoliosis (n = 69) | ||||||
| ULNT1 Left | ULNT1 Right | SLR Left | SLR Right | SLUMP Left | SLUMP Right | |
| Sternum | 0.067 | −0.043 | −0.010 | −0.074 | 0.007 | −0.002 |
| C | 0.425 *** | 0.324 ** | −0.377 ** | −0.407 ** | 0.103 | 0.131 |
| T1 | 0.487 *** | 0.370 ** | −0.450 *** | −0.432 *** | 0.158 | 0.216 |
| T2 | 0.294 * | 0.175 | −0.264 * | −0.281 * | 0.118 | 0.164 |
| LS | 0.300 * | 0.412 ** | −0.135 | −0.098 | 0.256 * | 0.243 * |
| ATRT | −0.249 * | −0.282 * | 0.160 | 0.169 | −0.119 | −0.198 |
| ATRL | 0.283 * | 0.104 | −0.124 | −0.122 | 0.122 | 0.130 |
| Control Group (n = 57) | ||||||
| ULNT1 Left | ULNT1 Right | SLR Left | SLR Right | SLUMP Left | SLUMP Right | |
| Sternum | 0.023 | −0.007 | −0.122 | −0.104 | 0.045 | 0.059 |
| C | 0.297 * | 0.356 ** | −0.526 *** | −0.544 *** | 0.152 | 0.171 |
| T1 | 0.352 ** | 0.265 * | −0.370 ** | −0.383 ** | 0.173 | 0.125 |
| T2 | 0.240 | 0.270 * | −0.253 | −0.282 * | 0.191 | 0.200 |
| LS | 0.190 | 0.272 * | −0.374 ** | −0.346 ** | 0.292 * | 0.301 * |
| ATRT | −0.429 ** | −0.419 ** | 0.301 * | 0.297 * | −0.021 | −0.066 |
| ATRL | −0.057 | −0.109 | 0.141 | 0.174 | −0.109 | −0.136 |
| Idiopathic Scoliosis (n = 69) | ||||||
| ULNT1 Left | ULNT1 Right | SLR Left | SLR Right | SLUMP Left | SLUMP Right | |
| FTF | −0.026 | −0.141 | −0.396 ** | −0.370 ** | 0.189 | 0.201 |
| CR left | −0.139 | −0.015 | 0.096 | 0.058 | −0.105 | −0.125 |
| CR right | −0.058 | 0.031 | 0.022 | −0.020 | −0.178 | −0.168 |
| HE left | 0.120 | 0.049 | 0.268 * | 0.211 | −0.159 | −0.120 |
| HE right | 0.213 | −0.011 | 0.133 | 0.067 | −0.124 | −0.095 |
| HF left | −0.447 ** | −0.426 *** | 0.941 *** | 0.905 *** | −0.533 *** | −0.485 *** |
| HF right | −0.403 ** | −0.347 ** | 0.895 *** | 0.886 *** | −0.465 *** | −0.432 *** |
| TPHA left | 0.206 | 0.202 | −0.078 | −0.101 | −0.011 | 0.029 |
| TPHA right | 0.364 ** | 0.398 ** | −0.350 ** | −0.347 ** | 0.124 | 0.151 |
| JHM | −0.136 | −0.099 | 0.123 | 0.108 | −0.082 | −0.077 |
| Control Group (n = 57) | ||||||
| ULNT1 Left | ULNT1 Right | SLR Left | SLR Right | SLUMP Left | SLUMP Right | |
| FTF | 0.214 | 0.245 | −0.543 *** | −0.504 *** | 0.433 ** | 0.462 *** |
| CR left | 0.025 | −0.009 | 0.188 | 0.199 | −0.275 * | −0.254 |
| CR right | −0.097 | −0.172 | 0.273 * | 0.267 * | −0.477 *** | −0.462 *** |
| HE left | −0.045 | −0.096 | 0.228 | 0.207 | −0.026 | −0.066 |
| HE right | −0.192 | −0.196 | 0.281 * | 0.279 * | 0.005 | −0.030 |
| HF left | −0.544 *** | −0.572 *** | 0.965 *** | 0.939 *** | −0.604 *** | −0.589 *** |
| HF right | −0.561 *** | −0.581 *** | 0.952 *** | 0.955 *** | −0.586 *** | −0.571 *** |
| TPHA left | 0.350 ** | 0.353 ** | −0.099 | −0.113 | 0.208 | 0.215 |
| TPHA right | 0.303 * | 0.250 | 0.180 | −0.205 | 0.173 | 0.153 |
| JHM | 0.095 | 0.027 | 0.077 | 0.047 | −0.017 | −0.054 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stępień, A.; Pałdyna, B. Neurodynamic Functions and Their Correlations with Postural Parameters in Adolescents with Idiopathic Scoliosis. J. Clin. Med. 2022, 11, 1115. https://doi.org/10.3390/jcm11041115
Stępień A, Pałdyna B. Neurodynamic Functions and Their Correlations with Postural Parameters in Adolescents with Idiopathic Scoliosis. Journal of Clinical Medicine. 2022; 11(4):1115. https://doi.org/10.3390/jcm11041115
Chicago/Turabian StyleStępień, Agnieszka, and Beata Pałdyna. 2022. "Neurodynamic Functions and Their Correlations with Postural Parameters in Adolescents with Idiopathic Scoliosis" Journal of Clinical Medicine 11, no. 4: 1115. https://doi.org/10.3390/jcm11041115
APA StyleStępień, A., & Pałdyna, B. (2022). Neurodynamic Functions and Their Correlations with Postural Parameters in Adolescents with Idiopathic Scoliosis. Journal of Clinical Medicine, 11(4), 1115. https://doi.org/10.3390/jcm11041115





