Patterns of Long COVID Symptoms: A Multi-Center Cross Sectional Study
Abstract
:1. Background
2. Methods
2.1. Study Design, Participants and Data Collection
2.2. Statistical Analysis
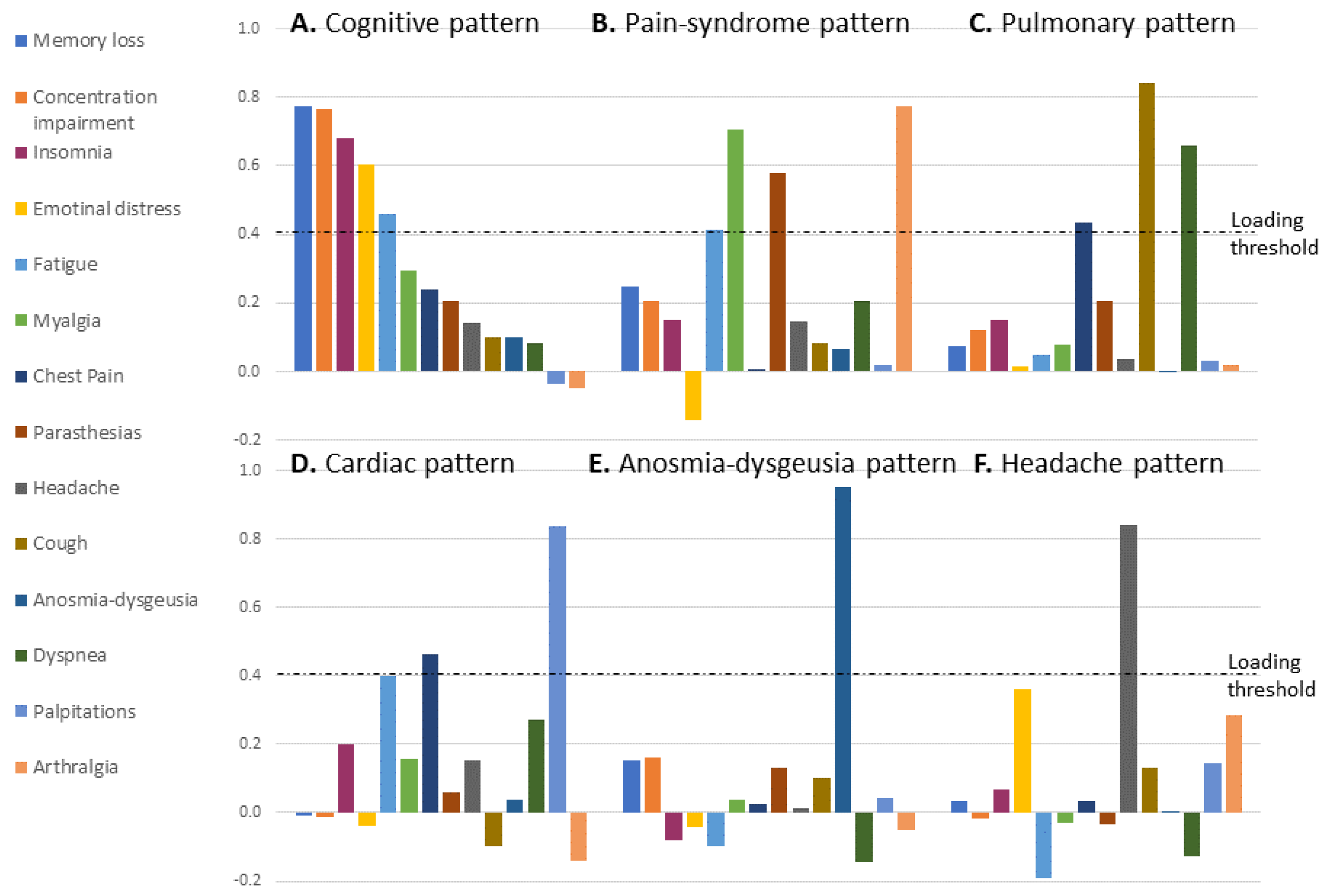
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Townsend, L.; Dyer, A.H.; Jones, K.; Dunne, J.; Mooney, A.; Gaffney, F.; O’Connor, L.; Leavy, D.; O’Brien, K.; Dowds, J.; et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE 2020, 15, e0240784. [Google Scholar] [CrossRef] [PubMed]
- Bliddal, S.; Banasik, K.; Pedersen, O.B.; Nissen, J.; Cantwell, L.; Schwinn, M.; Tulstrup, M.; Westergaard, D.; Ullum, H.; Brunak, S.; et al. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Sci. Rep. 2021, 11, 13153. [Google Scholar] [CrossRef] [PubMed]
- Peghin, M.; Palese, A.; Venturini, M.; De Martino, M.; Gerussi, V.; Graziano, E.; Bontempo, G.; Marrella, F.; Tommasini, A.; Fabris, M.; et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin. Microbiol. Infect. 2021, 27, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Carvalho-Schneider, C. Follow-up of adults with non-critical COVID-19 two months after symptoms’ onset. Clin. Microbiol. Infect. 2020, 27, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Del Rio, C.; Collins, L.F.; Malani, P. Long-term Health Consequences of COVID-19. JAMA 2020, 324, 1723–1724. [Google Scholar] [CrossRef]
- Yelin, D.; Wirtheim, E.; Vetter, P.; Kalil, A.C.; Bruchfeld, J.; Runold, M.; Guaraldi, G.; Mussini, C.; Gudiol, C.; Pujol, M.; et al. Long-term consequences of COVID-19: Research needs. Lancet Infect. Dis. 2020, 20, 1115–1117. [Google Scholar] [CrossRef]
- Nehme, M.; Braillard, O.; Chappuis, F.; Courvoisier, D.S.; Guessous, I. Prevalence of Symptoms More Than Seven Months After Diagnosis of Symptomatic COVID-19 in an Outpatient Setting. Ann. Intern. Med. 2021, 174, 1252–1260. [Google Scholar] [CrossRef]
- WHO. WHO Interim Clinical Guidance May 27 2020. Available online: https://www.who.int/publications/i/item/clinical-management-of-covid-19 (accessed on 28 April 2021).
- Scoppettuolo, P.; Borrelli, S.; Naeije, G. Neurological involvement in SARS-CoV-2 infection: A clinical systematic review. Brain Behav. Immun. Health 2020, 5, 100094. [Google Scholar] [CrossRef]
- Zhang, P.; Li, J.; Liu, H.; Han, N.; Ju, J.; Kou, Y.; Chen, L.; Jiang, M.; Pan, F.; Zheng, Y.; et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: A 15-year follow-up from a prospective cohort study. Bone Res. 2020, 8, 8. [Google Scholar] [CrossRef] [Green Version]
- Kim, E.A.; Lee, K.S.; Primack, S.L.; Yoon, H.K.; Byun, H.S.; Kim, T.S.; Suh, G.Y.; Kwon, O.J.; Han, J. Viral Pneumonias in Adults: Radiologic and Pathologic Findings. RadioGraphics 2002, 22, S137–S149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neufeld, K.J.; Leoutsakos, J.-M.S.; Yan, H.; Lin, S.; Zabinski, J.S.; Dinglas, V.D.; Hosey, M.M.; Parker, A.M.; Hopkins, R.O.; Needham, D.M. Fatigue Symptoms During the First Year Following ARDS. Chest 2020, 158, 999–1007. [Google Scholar] [CrossRef]
- Hui, D.S.C.; Wong, K.T.; Antonio, G.E.; Tong, M.; Chan, D.P.; Sung, J.J.Y. Long-term sequelae of SARS: Physical, neuropsychiatric, and quality-of-life assessment. Hong Kong Med. J. 2009, 15, 21–23. [Google Scholar] [PubMed]
- Lam, M.H.-B.; Wing, Y.-K.; Yu, M.W.-M.; Leung, C.-M.; Ma, R.C.W.; Kong, A.P.S.; So, W.; Fong, S.Y.-Y.; Lam, S.-P. Mental Morbidities and Chronic Fatigue in Severe Acute Respiratory Syndrome Survivors: Long-term Follow-up. Arch. Intern. Med. 2009, 169, 2142–2147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reichenberg, A.; Yirmiya, R.; Schuld, A.; Kraus, T.; Haack, M.; Morag, A.; Pollmächer, T. Cytokine-Associated Emotional and Cognitive Disturbances in Humans. Arch. Gen. Psychiatry 2001, 58, 445–452. [Google Scholar] [CrossRef]
- Abramovitch, A.; McCormack, B.; Brunner, D.; Johnson, M.; Wofford, N. The impact of symptom severity on cognitive function in obsessive-compulsive disorder: A meta-analysis. Clin. Psychol. Rev. 2018, 67, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Hickie, I.; Davenport, T.; Wakefield, D.; Vollmer-Conna, U.; Cameron, B.; Vernon, S.D.; Reeves, W.C.; Lloyd, A. Post infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: Prospective cohort study. BMJ 2006, 333, 575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buchwald, D.; Ashley, R.L.; Pearlman, T.; Kith, P.; Komaroff, A.L. Viral serologies in patients with chronic fatigue and chronic fatigue syndrome. J. Med. Virol. 1996, 50, 25–30. [Google Scholar] [CrossRef]
- Imazio, M.; Klingel, K.; Kindermann, I.; Brucato, A.; De Rosa, F.G.; Adler, Y.; De Ferrari, G.M. COVID-19 pandemic and troponin: Indirect myocardial injury, myocardial inflammation or myocarditis? Heart 2020, 106, 1127–1131. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265–1273. [Google Scholar] [CrossRef]
- Zheng, J.; Wong, L.-Y.R.; Li, K.; Verma, A.K.; Ortiz, M.E.; Wohlford-Lenane, C.; Leidinger, M.R.; Knudson, C.M.; Meyerholz, D.K.; McCray, P.B., Jr.; et al. COVID-19 treatments and pathogenesis including anosmia in K18-hACE2 mice. Nature 2021, 589, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazi-Hoffnung, L.; Shmueli, E.; Ehrlich, S.; Ziv, A.; Bar-On, O.; Birk, E.; Lowenthal, A.; Prais, D. Long COVID in Children: Observations from a Designated Pediatric Clinic. Pediatr. Infect. Dis. J. 2021, 40, e509–e511. [Google Scholar] [CrossRef] [PubMed]
- Buonsenso, D.; Munblit, D.; De Rose, C.; Sinatti, D.; Ricchiuto, A.; Carfi, A.; Valentini, P. Preliminary evidence on long COVID in children. Acta Paediatr. 2021, 110, 2208–2211. [Google Scholar] [CrossRef] [PubMed]
| All | Israel | Switzerland | Spain | Italy | |
|---|---|---|---|---|---|
| No. of patients, N (%) | 1027 | 544 (53) | 256 (24.9) | 115 (11.2) | 112 (10.9) |
| Gender–women, N (%) | 559 (54.4) | 307 (56.4) | 144 (56.3) | 60 (52.2) | 48 (42.9) |
| Age, mean (SD) | 49.2 (16.1) | 46.4 (15.5) | 45.5 (15.1) | 58.4 (12.4) | 61.2 (15.5) |
| BMI, mean (SD) Obese, N (%) * missing 280 | 28 (5.6) 223 (30.2) N = 738 | 27.6 (5.6) 149 (29.0) N = 518 | 28.7 (7.7) 3 (15.7) N = 19 | 29.8 (6.1) 42 (42.4) N = 99 | 28.2 (4.6) 29 (26.1) N = 111 |
| Smoking, N (%) * missing 79 | 255 (24.8) | 132 (24.3) | 59 (23.0) | 41 (35.7) | 23 (20.5) |
| Diabetes, N (%) | 92 (9.0) | 45 (8.3) | 10 (3.9) | 22 (19.1) | 15 (13.4) |
| Hypertension, N (%) | 206 (20.1) | 89 (16.4) | 27 (10.5) | 50 (43.5) | 40 (35.7) |
| IHD, N (%) | 52 (5.1) | 25 (4.6) | 17 (6.6) | 1 (0.9) | 9 (8.0) |
| Prior lung disease, N (%) | 79 (7.7) | 35 (6.4) | 19 (7.4) | 16 (13.9) | 9 (8.0) |
| Hospitalization, N (%) * Missing 78 | 337 (32.8) | 122 (22.4) | 26 (10.2) | 79 (68.7) | 112 (100) |
| Severe disease a, N (%) | 264 (25.7) | 86 (15.8) | 26 (10.2) | 72 (62.6) | 80 (71.4) |
| Time to clinic visit (days), median (IQR) * Missing 26 | 123 (80–204) | 97 (66–130) | 217 (203–233) | 115 (87–224) | 146 (127–185) |
| Fatigue b, N (%) | 691 (67.2) | 411 (75.6) | 129 (50.4) | 90 (78.3) | 61 (54.5) |
| Dyspnea b, N (%) | 480 (46.7) | 277 (50.9) | 62 (24.2) | 85 (73.9) | 56 (50.0) |
| Cough b, N (%) | 187 (18.2) | 108 (19.9) | 21 (8.2) | 35 (30.4) | 23 (20.5) |
| Chest pain b, N (%) | 204 (19.9) | 166 (30.5) | 14 (5.5) | 24 (20.9) | 0 (0) |
| Palpitations b, N (%) | 104 (10.1) | 67 (12.3) | 18 (7.0) | 19 (16.5) | 0 (0) |
| Myalgia b, N (%) | 332 (32.3) | 204 (37.5) | 37 (14.5) | 46 (40.0) | 45 (40.2) |
| Arthralgia b, N (%) | 157 (15.3) | 51 (9.4) | 23 (9.0) | 33 (28.7) | 50 (44.6) |
| Parasthesias b, N (%) | 193 (18.8) | 109 (20.0) | 13 (5.1) | 32 (27.8) | 39 (34.8) |
| Insomnia b, N (%) | 259 (25.2) | 204 (37.5) | 27 (10.5) | 28 (24.3) | 0 (0) |
| Headacheb, N (%) | 153 (14.9) | 69 (12.7) | 44 (17.2) | 24 (20.9) | 16 (14.3) |
| Memory loss b, N (%) | 315 (30.7) | 201 (36.9) | 35 (13.7) | 33 (28.7) | 46 (41.1) |
| Concentration impairment b, N (%) | 312 (30.4) | 212 (39.0) | 31 (12.1) | 26 (22.6) | 43 (38.4) |
| Anosmia/dysguesia b, N (%) | 289 (28.2) | 160 (29.4) | 70 (27.3) | 24 (20.9) | 30 (26.8) |
| Worse physical activity status c, N (%) * missing 42 | 326 (31.7) | 142 (26.1) | 134 (52.3) | 43 (37.4) | 7 (6.3) |
| Worse employment status c, N (%) * missing 292 | 131 (12.8) | 102 (18.8) | ---- | 22 (19.1) | 7 (6.3) |
| Pulmonary function testing performed, N (%) | 665 (64.8) | 517 (95.0) | ---- | 51 (44.3) | 97 (86.6) |
|
Feature N (%) | Cognitive-Emotional Pattern | Pain Syndrome Pattern | Pulmonary Pattern | Palpitations-Chest Pain Pattern | Anosmia-Dysgeusia Pattern | Headache Pattern | |
|---|---|---|---|---|---|---|---|
| Gender | Women 559 (54.5) | 0.08 (1.05) | 0.11 (1.08) | 0.03 (1.06) | 0.04 (1.03) | 0.05 (1.04) | 0.13 (1.13) |
| Men 466 (45.5) | −0.10 (0.93) | −0.13 (0.88) | −0.04 (0.93) | −0.05 (0.96) | −0.06 (0.94) | −0.15 (0.79) | |
| Age | ≥65 years 168 (16.4) | −0.17 (0.95) | 0.09 (0.86) | 0.06 (1.01) | −0.28 (0.63) | −0.17 (0.74) | −0.19 (0.72) |
| <65 years 858 (83.6) | 0.03 (1.01) | −0.02 (1.02) | −0.01 (1.00) | 0.06 (1.05) | 0.03 (1.04) | 0.04 (1.04) | |
| Rho (p) b | −0.05 (0.12) | 0.15 (<0.001) | 0.03 (0.34) | −0.12 (<0.001) | −0.06 (0.06) | −0.09 (0.006) | |
| BMI | ≥30 226 (30.2) | 0.07 (1.09) | 0.13 (0.95) | 0.11 (1.09) | 0.09 (1.07) | −0.06 (0.97) | −0.17 (0.98) |
| <30 521 (69.8) | 0.02 (1.02) | 0.10 (0.99) | 0.06 (0.99) | 0.04 (1.02) | −0.02 (0.91) | −0.15 (0.86) | |
| Rho (p) b | −0.02 (0.61) | 0.04 (0.28) | 0.04 (0.29) | 0.01 (0.97) | −0.08 (0.03) | −0.05 (0.16) | |
| Smoker (ever) | Yes 255 (26.9) | 0.01 (1.04) | 0.08 (1.04) | −0.02 (0.99) | 0.04 (1.00) | 0.00 (0.98) | −0.03 (0.98) |
| No 693 (73.1) | 0.02 (0.99) | −0.10 (0.93) | 0.13 (1.05) | −0.05 (1.05) | 0.00 (1.00) | −0.04 (1.04) | |
| Comorbidities | |||||||
| Prior lung disease | Yes 79 (7.7) | −0.01 (1.11) | −0.04 (0.94) | 0.41 (1.24) | −0.08 (0.82) | −0.10 (1.02) | −0.08 (1.00) |
| No 948 (92.3) | 0.00 (0.99) | 0.00 (1.01) | −0.03 (0.97) | 0.01 (1.01) | 0.01 (1.00) | 0.01 (1.00) | |
| Diabetes | Yes 92 (9.0) | −0.03 (1.03) | 0.23 (0.97) | 0.20 (1.14) | −0.01 (0.96) | −0.17 (0.80) | −0.27 (0.82) |
| No 926 (91.0) | 0.01 (1.00) | −0.02 (1.00) | −0.02 (0.99) | 0.00 (1.01) | 0.02 (1.02) | 0.03 (1.02) | |
| HTN | Yes 206 (20.2) | −0.07 (0.98) | 0.10 (0.94) | 0.12 (1.02) | −0.12 (0.82) | −0.10 (0.93) | −0.21 (0.78) |
| No 812 (79.8) | 0.02 (1.01) | −0.02 (1.02) | −0.03 (1.00) | 0.04 (1.04) | 0.03 (1.02) | 0.05 (1.05) | |
| IHD | Yes 52 (5.1) | 0.14 (1.27) | −0.13 (0.77) | 0.11 (1.05) | −0.22 (0.66) | −0.14 (1.02) | 0.02 (1.25) |
| No 966 (94.9) | −0.01 (0.99) | 0.01 (1.01) | 0.00 (1.00) | 0.01 (1.02) | 0.01 (1.00) | 0.00 (0.99) | |
| Atrial fibrillation | Yes 27 (2.6) | −0.33 (0.99) | 0.12 (0.68) | 0.00 (0.67) | −0.33 (0.44) | −0.33 (0.54) | −0.20 (0.72) |
| No 1000 (97.4) | 0.01 (1.00) | 0.00 (1.01) | 0.00 (1.01) | 0.01 (1.01) | 0.01 (1.01) | 0.01 (1.01) | |
| Acute COVID-19 features | |||||||
| Hospitalization | Yes 337 (35.5) | −0.15 (1.00) | 0.15 (0.95) | 0.17 (0.98) | −0.11 (0.95) | −0.16 (0.79) | −0.17 (0.82) |
| No 612 (64.5) | 0.10 (1.03) | −0.02 (1.04) | −0.07 (1.01) | 0.09 (1.08) | 0.07 (1.07) | 0.04 (1.07) | |
| Abnormal CXR | Yes 140 (39.5) | −0.14 (1.05) | 0.17 (0.96) | 0.31 (1.06) | −0.04 (0.94) | −0.25 (0.72) | −0.10 (0.95) |
| No 214 (60.5) | −0.07 (1.05) | 0.40 (1.12) | 0.12 (1.00) | 0.04 (1.12) | 0.04 (0.99) | −0.07 (0.92) | |
| WHO severity | Severe 264 (25.6) | −0.16 (0.99) | 0.22 (0.98) | 0.20 (1.07) | −0.08 (0.94) | −0.19 (0.78) | −0.13 (0.86) |
| Non-severe 763 (74.4) | 0.05 (1.00) | −0.08 (1.00) | −0.07 (0.97) | 0.03 (1.02) | 0.07 (1.06) | 0.05 (1.04) | |
| Symptoms of the acute disease | |||||||
| Fatigue c | Yes 529 (69.0) | 0.25 (1.13) | 0.19 (1.08) | 0.12 (1.09) | 0.22 (1.12) | 0.00 (1.02) | −0.17 (0.97) |
| No 209 (31.0) | −0.37 (0.75) | 0.03 (0.88) | 0.04 (0.98) | −0.19 (0.87) | −0.03 (0.80) | −0.11 (0.78) | |
| Dyspnea c | Yes 405 (54.5) | 0.12 (1.13) | 0.24 (1.09) | 0.33 (1.16) | 0.19 (1.15) | −0.03 (0.98) | −0.14 (0.97) |
| No 338 (45.5) | −0.02 (0.99) | 0.04 (0.94) | −0.16 (0.85) | −0.01 (0.96) | 0.01 (0.94) | −0.15 (0.86) | |
| Anosmia c | Yes 360 (49.2) | 0.34 (1.17) | 0.13 (1.05) | 0.12 (1.09) | 0.21 (1.04) | 0.36 (1.16) | −0.23 (0.92) |
| No 371 (50.8) | −0.18 (0.90) | 0.15 (1.00) | 0.09 (1.04) | 0.00 (1.10) | −0.34 (0.54) | −0.05 (0.93) | |
| Myalgia c | Yes 418 (56.6) | 0.29 (1.18) | 0.37 (1.15) | 0.16 (1.16) | 0.19 (1.03) | 0.02 (1.01) | −0.14 (1.06) |
| No 321 (43.4) | −0.22 (0.84) | −0.14 (0.75) | 0.03 (0.92) | −0.02 (1.10) | −0.05 (0.89) | −0.15 (0.71) | |
| Time to clinic visit rho (p) | N = 1001 | −0.04 (0.204) | −0.149 (<0.001) | −0.122 (<0.001) | −0.255 (<0.001) | 0.032 (0.316) | 0.163 (<0.001) |
|
Feature N (%) | Cognitive-Emotional Pattern | Pain Syndrome Pattern | Pulmonary Pattern | Palpitations-Chest Pain Pattern | Anosmia-Dysgeusia Pattern | Headache Pattern | |
|---|---|---|---|---|---|---|---|
| Failure to return to physical activity | Yes 326 (33.1) | 0.18 (1.10) | 0.07 (1.14) | 0.08 (1.18) | 0.18 (1.18) | −0.12 (1.02) | 0.09 (1.18) |
| No 659 (66.9) | −0.09 (0.94) | −0.02 (0.94) | −0.02 (0.97) | −0.08 (0.91) | 0.06 (0.99) | −0.05 (0.90) | |
| Failure to return to full employment | Yes 131 (17.8) | 0.49 (1.26) | 0.14 (1.12) | 0.26 (1.27) | 0.44 (1.29) | −0.02 (1.01) | −0.02 (1.13) |
| No 604 (82.2) | −0.04 (1.00) | 0.15 (1.00) | 0.06 (1.00) | 0.02 (1.00) | −0.02 (0.93) | −0.16 (0.89) | |
| DLCO | Abnormal a 178 (26.7) | 0.13 (1.15) | 0.14 (0.90) | 0.38 (1.18) | 0.16 (1.21) | −0.09 (0.93) | −0.05 (1.01) |
| Normal 487 (73.3) | 0.03 (1.01) | 0.07 (0.95) | −0.04 (0.94) | 0.08 (1.00) | −0.02 (0.92) | −0.24 (0.82) | |
| Rho, (p) b | −0.03 (0.43) | −0.09 (0.02) | −0.18 (<0.001) | −0.05 (0.23) | 0.13 (<0.001) | 0.01 (0.89) | |
| TLC | Abnormal a 95 (14.5) | −0.07 (1.10) | 0.25 (1.00) | 0.29 (1.11) | 0.01 (0.85) | −0.14 (0.87) | −0.19 (0.93) |
| Normal 562 (85.5) | 0.08 (1.05) | 0.06 (0.92) | 0.02 (1.00) | 0.12 (1.10) | −0.02 (0.93) | −0.19 (0.87) | |
| Rho, (p) b | 0.3 (0.46) | −0.4 (0.29) | −0.09 (0.02) | −0.06 (0.16) | 0.08 (0.06) | 0.05 (0.25) | |
| FeV1 to FVC ratio | Abnormal c 24 (3.6) | 0.12 (1.05) | −0.01 (0.99) | 0.67 (1.30) | 0.23 (1.28) | 0.07 (1.21) | 0.14 (1.07) |
| Normal 643 (96.4) | 0.06 (1.05) | 0.10 (0.93) | 0.04 (1.00) | 0.10 (1.06) | −0.04 (0.93) | −0.21 (0.87) | |
| Rho, (p) b | −0.16 (<0.001) | 0.11 (0.01) | 0.01 (0.94) | −0.15 (<0.001) | 0.11 (0.01) | 0.11 (0.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yelin, D.; Margalit, I.; Nehme, M.; Bordas-Martínez, J.; Pistelli, F.; Yahav, D.; Guessous, I.; Durà-Miralles, X.; Carrozzi, L.; Shapira-Lichter, I.; et al. Patterns of Long COVID Symptoms: A Multi-Center Cross Sectional Study. J. Clin. Med. 2022, 11, 898. https://doi.org/10.3390/jcm11040898
Yelin D, Margalit I, Nehme M, Bordas-Martínez J, Pistelli F, Yahav D, Guessous I, Durà-Miralles X, Carrozzi L, Shapira-Lichter I, et al. Patterns of Long COVID Symptoms: A Multi-Center Cross Sectional Study. Journal of Clinical Medicine. 2022; 11(4):898. https://doi.org/10.3390/jcm11040898
Chicago/Turabian StyleYelin, Dana, Ili Margalit, Mayssam Nehme, Jaume Bordas-Martínez, Francesco Pistelli, Dafna Yahav, Idris Guessous, Xavier Durà-Miralles, Laura Carrozzi, Irit Shapira-Lichter, and et al. 2022. "Patterns of Long COVID Symptoms: A Multi-Center Cross Sectional Study" Journal of Clinical Medicine 11, no. 4: 898. https://doi.org/10.3390/jcm11040898







