Topographic Relationships among Deep Optic Nerve Head Parameters in Patients with Primary Open-Angle Glaucoma
Abstract
:1. Introduction
2. Methods
2.1. Participants
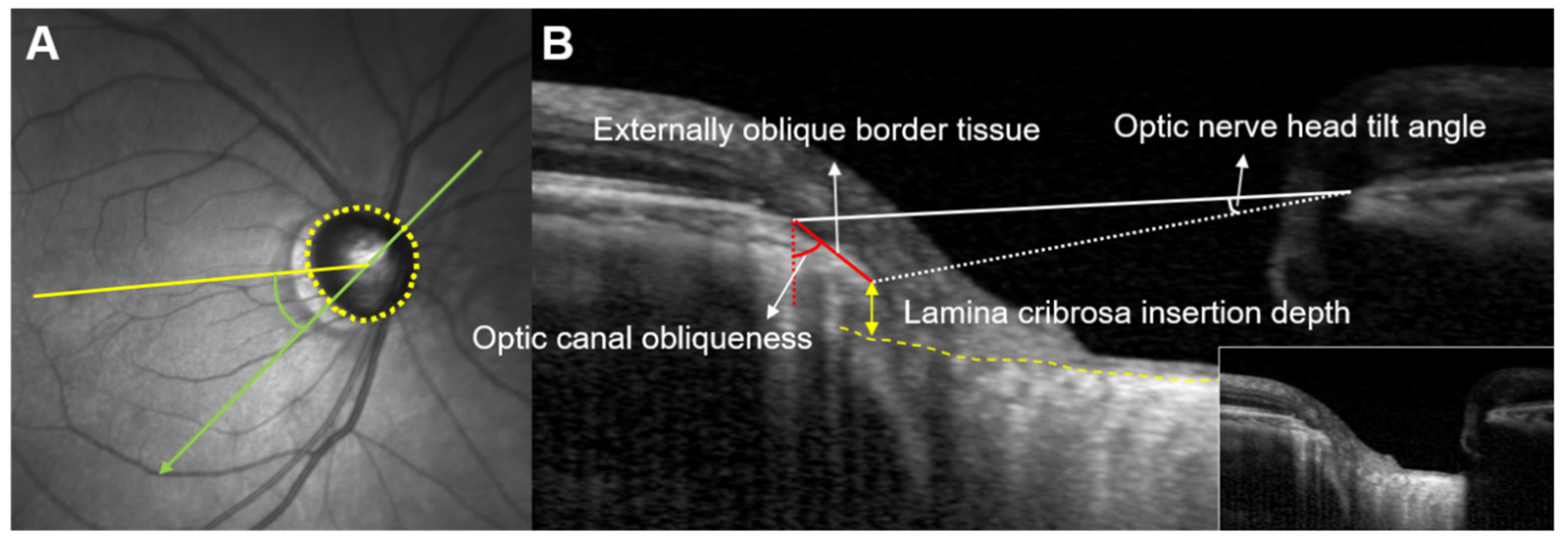
2.2. Imaging of Optic Nerve Head Using SD-OCT
2.3. Measurement of the Extent and Angular Location of Deep ONH Parameters Using SD-OCT
2.4. Determination of Dominant VF Defect Locations
2.5. Statistical Analysis
3. Results
3.1. Spatial Correspondence between Deep ONH Structures and VF Defects
3.2. Extent and Location of Deep ONH Parameters According to AL
3.3. Relationship between RNFL Thickness and Location of Deep ONH Parameters
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burgoyne, C.F.; Downs, J.C.; Bellezza, A.J.; Suh, J.K.F.; Hart, R.T. The optic nerve head as a biomechanical structure: A new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog. Retin. Eye Res. 2005, 24, 39–73. [Google Scholar] [CrossRef]
- Bellezza, A.J.; Hart, R.T.; Burgoyne, C.F. The optic nerve head as a biomechanical structure: Initial finite element modeling. Investig. Ophthalmol. Vis. Sci. 2000, 41, 2991–3000. [Google Scholar]
- Downs, J.C.; Girkin, C.A. Lamina cribrosa in glaucoma. Curr. Opin. Ophthalmol. 2017, 28, 113–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, B.J.; Park, K.H. Topographic correlation between beta-zone parapapillary atrophy and retinal nerve fiber layer defect. Ophthalmology 2013, 120, 528–534. [Google Scholar] [CrossRef]
- Choi, J.A.; Park, H.Y.L.; Shin, H.Y.; Park, C.K. Optic disc tilt direction determines the location of initial glaucomatous damage. Investig. Ophthalmol. Vis. Sci. 2014, 55, 4991–4998. [Google Scholar] [CrossRef]
- Han, J.C.; Choi, J.H.; Park, D.Y.; Lee, E.J.; Kee, C. Deep optic nerve head morphology is associated with pattern of glaucomatous visual field defect in open-angle glaucoma. Investig. Ophthalmol. Vis. Sci. 2018, 59, 3842–3851. [Google Scholar] [CrossRef] [Green Version]
- Han, J.C.; Lee, E.J.; Kim, S.B.; Kee, C. The characteristics of deep optic nerve head morphology in myopic normal tension glaucoma. Investig. Ophthalmol. Vis. Sci. 2017, 58, 2695–2704. [Google Scholar] [CrossRef] [Green Version]
- Reis, A.S.C.; O’Leary, N.; Yang, H.L.; Sharpe, G.P.; Nicolela, M.T.; Burgoyne, C.F.; Chauhan, B.C. Influence of clinically invisible, but optical coherence tomography detected, optic disc margin anatomy on neuroretinal rim evaluation. Investig. Ophthalmol. Vis. Sci. 2012, 53, 1852–1860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reis, A.S.C.; Sharpe, G.P.; Yang, H.L.; Nicolela, M.T.; Burgoyne, C.F.; Chauhan, B.C. Optic disc margin anatomy in patients with glaucoma and normal controls with spectral domain optical coherence tomography. Ophthalmology 2012, 119, 738–747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosseini, H.; Nassiri, N.; Azarbod, P.; Giaconi, J.; Chou, T.; Caprioli, J.; Nouri-Mahdavi, K. Measurement of the optic disc vertical tilt angle with spectral-domain optical coherence tomography and influencing factors. Am. J. Ophthalmol. 2013, 156, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Strouthidis, N.G.; Grimm, J.; Williams, G.A.; Cull, G.A.; Wilson, D.J.; Burgoyne, C.F. A comparison of optic nerve head morphology viewed by spectral domain optical coherence tomography and by serial histology. Investig. Ophthalmol. Vis. Sci. 2010, 51, 1464–1474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.M.; Kim, T.W.; Weinreb, R.N.; Lee, E.J.; Girard, M.J.; Mari, J.M. Anterior lamina cribrosa insertion in primary open-Angle glaucoma patients and healthy subjects. PLoS ONE 2014, 9, e114935. [Google Scholar] [CrossRef] [PubMed]
- Park, S.C.; Kiumehr, S.; Teng, C.C.; Tello, C.; Liehmann, J.M.; Ritch, R. Horizontal central ridge of the lamina cribrosa and regional differences in laminar insertion in healthy subjects. Investig. Ophthalmol. Vis. Sci. 2012, 53, 1610–1616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.W.; Jeoung, J.W.; Kim, D.W.; Girard, M.J.; Mari, J.M.; Park, K.H.; Kim, D.M. Clinical assessment of lamina cribrosa curvature in eyes with primary open-Angle glaucoma. PLoS ONE 2016, 11, e0150260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.W.; Kim, D.W.; Jeoung, J.W.; Kim, D.M.; Park, K.H. Peripheral lamina cribrosa depth in primary open-angle glaucoma: A swept-source optical coherence tomography study of lamina cribrosa. Eye 2015, 29, 1368–1374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sawada, Y.; Hangai, M.; Murata, K.; Ishikawa, M.; Yoshitomi, T. Lamina cribrosa depth variation measured by spectral-Domain optical coherence tomography within and between four glaucomatous optic disc phenotypes. Investig. Ophthalmol. Vis. Sci. 2015, 56, 5777–5784. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.L.; Williams, G.; Downs, J.C.; Sigal, I.A.; Roberts, M.D.; Thompson, H.; Burgoyne, C.F. Posterior (outward) migration of the lamina cribrosa and early cupping in monkey experimental glaucoma. Investig. Ophthalmol. Vis. Sci. 2011, 52, 7109–7121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, R.H.; Wang, X.; Wei, Y.H.; Fang, Y.; Tian, T.; Li, M.; Cai, Y.; Pan, Y. Structure-Function relationship between Bruch’s membrane opening-Minimum rim width and perimetry in open-Angle glaucoma subtypes. Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.W.; Jeoung, J.W.; Girard, M.J.A.; Mari, J.M.; Park, K.H. Positional and curvature difference of lamina cribrosa according to the baseline intraocular pressure in primary open-Angle glaucoma: A swept-Source optical coherence tomography (ss-oct) study. PLoS ONE 2016, 11, e0162182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gmeiner, J.M.D.; Schrems, W.A.; Mardin, C.Y.; Laemmer, R.; Kruse, F.E. Schrems-Hoesl LM. Comparison of bruch’s membrane opening minimum rim width and peripapillary retinal nerve fiber layer thickness in early glaucoma assessment. Investig. Ophthalmol. Vis. Sci. 2016, 57, 575–584. [Google Scholar] [CrossRef] [PubMed]


| Total (n = 100) | Superior Dominant VF Defect (n = 68) | Inferior Dominant VF Defect (n = 32) | p Value | |
|---|---|---|---|---|
| Age, years | 50.7 ± 11.7 | 49.4 ± 12.2 | 53.5 ± 10.4 | 0.102 * |
| IOP, mmHg | 16.8 ± 3.1 | 16.8 ± 2.6 | 16.7 ± 3.9 | 0.921 * |
| AL, mm | 25.4 ± 1.4 | 25.4 ± 1.5 | 25.5 ± 1.2 | 0.699 * |
| CCT, µm | 538.8 ± 35.0 | 541.2 ± 36.4 | 533.7 ± 31.9 | 0.319 * |
| MD, dB | −3.9 ± 2.9 | −4.1 ± 2.8 | −3.4 ± 3.0 | 0.262 * |
| Deep ONH parameters | ||||
| Extent | ||||
| Maximum EOBT length, µm | 445.0 ± 203.2 | 456.4 ± 213.2 | 420.8 ± 181.0 | 0.417 * |
| Maximum ONH tilt angle, ° | 10.6 ± 4.2 | 10.6 ± 4.2 | 10.6 ± 4.3 | 0.962 * |
| Maximum OC obliqueness, ° | 52.4 ± 16.0 | 51.2 ± 16.3 | 54.7 ± 15.4 | 0.309 * |
| Maximum ALID, µm | 573.0 ± 119.1 | 579.4 ± 119.1 | 559.5 ± 119.8 | 0.440 * |
| Angular location, ° | ||||
| Maximum EOBT location | 16.9 ± 34.9 | 23.2 ± 34.0 | 3.5 ± 33.5 | 0.008 * |
| Maximum ONH tilt angle location | 17.7 ± 33.2 | 23.7 ± 33.3 | 5.0 ± 29.8 | 0.008 * |
| Maximum OC obliqueness location | 20.0 ± 34.0 | 27.4 ± 31.0 | 4.2 ± 35.3 | 0.001 * |
| Maximum ALID location | 38.6 ± 27.6 | 41.4 ± 25.9 | 32.8 ± 30.5 | 0.150 * |
| Inferior dominant location, n (%) | ||||
| Maximum EOBT location | 71 (71.0) | 53 (77.9) | 18 (56.3) | 0.026† |
| Maximum ONH tilt angle location | 73 (73.0) | 54 (79.4) | 19 (59.4) | 0.035† |
| Maximum OC obliqueness location | 74 (74.0) | 57 (83.8) | 17 (53.1) | 0.001† |
| Maximum ALID location | 91 (91.0) | 65 (95.6) | 26 (81.3) | 0.028† |
| Parameters, Extent | Maximum ONH Tilt Angle | Maximum OC Obliqueness | Maximum ALID |
| Maximum EOBT | |||
| Pearson’s coefficient | 0.707 | 0.577 | −0.050 |
| p value * | <0.001 | <0.001 | 0.619 |
| Maximum ONH tilt angle | |||
| Pearson’s coefficient | 0.255 | 0.149 | |
| p value * | 0.011 | 0.140 | |
| Maximum OC Obliqueness | |||
| Pearson’s coefficient | −0.172 | ||
| p value * | 0.087 | ||
| Parameters, Location | Maximum ONH Tilt Angle Location | Maximum OC Obliqueness Location | Maximum ALID Location |
| Maximum EOBT location | |||
| Pearson’s coefficient | 0.883 | 0.819 | 0.290 |
| p value * | <0.001 | <0.001 | 0.003 |
| Maximum ONH tilt angle location | |||
| Pearson’s coefficient | 0.803 | 0.159 | |
| p value * | <0.001 | 0.114 | |
| Maximum OC Obliqueness location | |||
| Pearson’s coefficient | 0.243 | ||
| p value * | 0.015 |
| Inferior Maximum EOBT Location, n = 71 | Superior Maximum EOBT Location, n = 29 | p Value | |
| RNFL thickness, µm | |||
| Superior | 93.5 ± 16.8 (58 to 138) | 95.8 ± 18.8 (64 to 145) | 0.555 * |
| Temporal | 64.1 ± 12.5 (37 to 97) | 64.9 ± 11.0 (41 to 81) | 0.761 * |
| Inferior | 77.8 ± 15.0 (47 to 117) | 92.7 ± 17.2 (65 to 129) | <0.001 * |
| Nasal | 63.1 ± 8.9 (43 to 87) | 64.4 ± 9.2 (49 to 84) | 0.508 * |
| Inferior Maximum ONH Tilt Location, n = 73 | Superior Maximum ONH Tilt Location, n = 27 | p Value | |
| RNFL thickness, µm | |||
| Superior | 94.6 ± 16.9 (58 to 138) | 93.1 ± 18.8 (64 to 145) | 0.720 * |
| Temporal | 64.5 ± 12.2 (37 to 97) | 63.9 ± 11.8 (41 to 89) | 0.829 * |
| Inferior | 79.4 ± 15.7 (47 to 129) | 89.5 ± 18.5 (55 to 125) | 0.008 * |
| Nasal | 62.7 ± 8.8 (43 to 87) | 65.5 ± 9.3 (49 to 84) | 0.168 * |
| Inferior Maximum OC Obliqueness Location, n = 74 | Superior Maximum OC Obliqueness Location, n = 26 | p Value | |
| RNFL thickness, µm | |||
| Superior | 94.3 ± 17.1 (58 to 145) | 93.8 ± 18.4 (64 to 129) | 0.910 * |
| Temporal | 64.2 ± 12.5 (37 to 97) | 64.6 ± 10.7 (41 to 81) | 0.885 * |
| Inferior | 79.0 ± 14.5 (47 to 117) | 90.1 ± 19.6 (55 to 129) | 0.002 * |
| Nasal | 63.7 ± 9.2 (43 to 87) | 62.7 ± 8.5 (49 to 83) | 0.623 * |
| Inferior Maximum ALID location, n = 91 | Superior Maximum ALID location, n = 9 | p Value | |
| RNFL thickness, µm | |||
| Superior | 94.7 ± 17.7 (58 to 145) | 89.2 ± 13.0 (71 to 115) | 0.323 * |
| Temporal | 64.3 ± 12.3 (37 to 97) | 64.9 ± 9.0 (53 to 78) | 0.763 * |
| Inferior | 81.5 ± 17.3 (47 to 129) | 88.1 ± 14.1 (73 to 120) | 0.250 * |
| Nasal | 63.3 ± 9.1 (43 to 87) | 65.0 ± 7.0 (57 to 76) | 0.531 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, D.-Y.; Noh, H.; Kee, C.; Han, J.-C. Topographic Relationships among Deep Optic Nerve Head Parameters in Patients with Primary Open-Angle Glaucoma. J. Clin. Med. 2022, 11, 1320. https://doi.org/10.3390/jcm11051320
Park D-Y, Noh H, Kee C, Han J-C. Topographic Relationships among Deep Optic Nerve Head Parameters in Patients with Primary Open-Angle Glaucoma. Journal of Clinical Medicine. 2022; 11(5):1320. https://doi.org/10.3390/jcm11051320
Chicago/Turabian StylePark, Do-Young, Hoon Noh, Changwon Kee, and Jong-Chul Han. 2022. "Topographic Relationships among Deep Optic Nerve Head Parameters in Patients with Primary Open-Angle Glaucoma" Journal of Clinical Medicine 11, no. 5: 1320. https://doi.org/10.3390/jcm11051320
APA StylePark, D. -Y., Noh, H., Kee, C., & Han, J. -C. (2022). Topographic Relationships among Deep Optic Nerve Head Parameters in Patients with Primary Open-Angle Glaucoma. Journal of Clinical Medicine, 11(5), 1320. https://doi.org/10.3390/jcm11051320





