Comparison of Procedural Sequences in Sedated Same-Day Bidirectional Endoscopy with Water-Exchange Colonoscopy: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
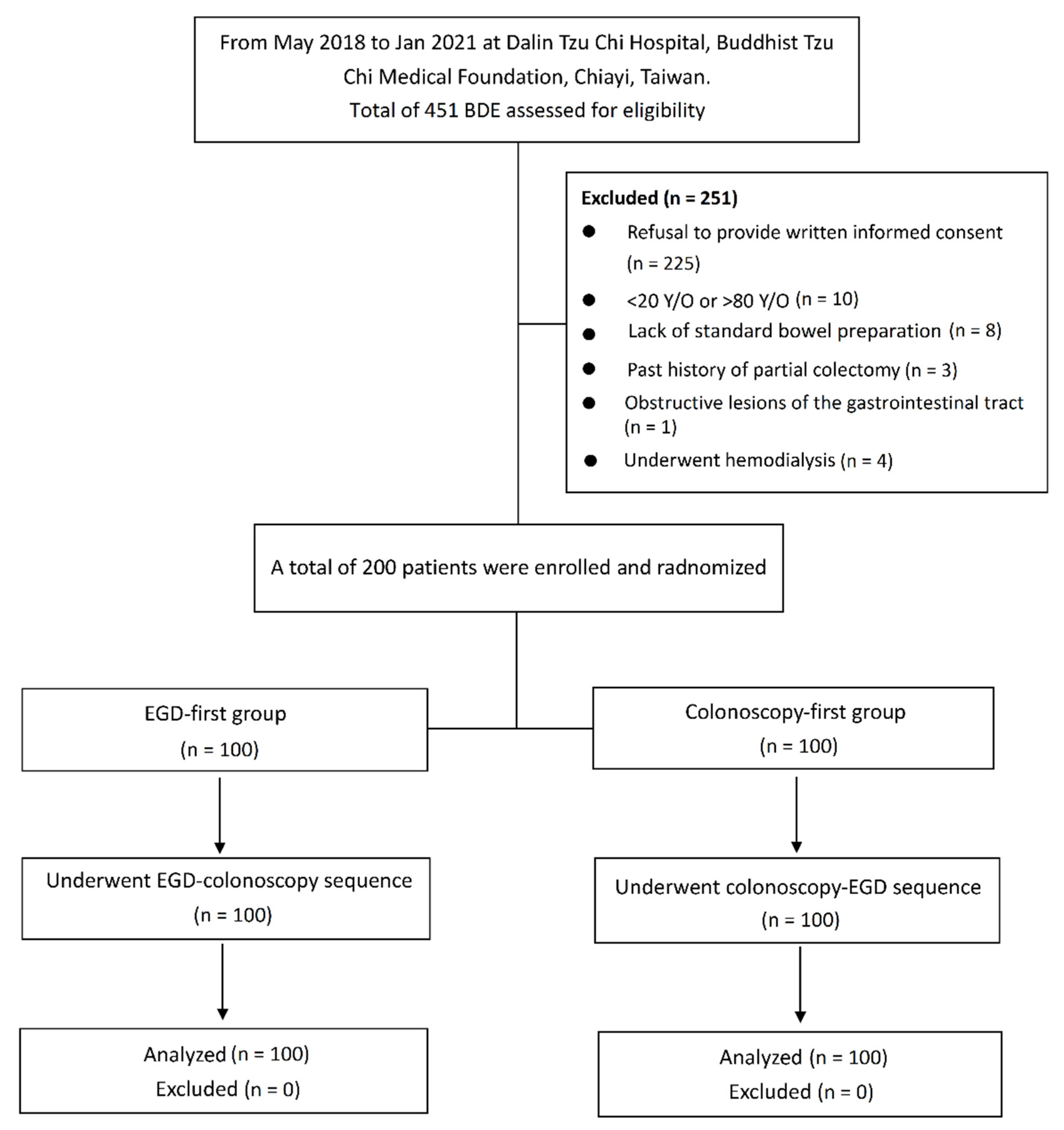
2.1. Study Population
2.2. Randomization and Allocation
2.3. Preparation and Procedure
2.4. Study Endpoints
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Outcomes of Bidirectional Endoscopy
3.3. Propofol Doses, Recovery Time, and Sedation-Related Outcomes
3.4. Patient’s Assessment of Discomfort and Satisfaction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- El-Serag, H.B.; Xu, F.; Biyani, P.; Cooper, G.S. Bundling in medicare patients undergoing bidirectional endoscopy: How often does it happen? Clin. Gastroenterol. Hepatol. 2014, 12, 58–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pongprasobchai, S.; Sriprayoon, T.; Manatsathit, S. Prospective evaluation of gastrointestinal lesions by bidirectional endoscopy in patients with iron deficiency anemia. J. Med. Assoc. Thail. 2011, 94, 1321–1326. [Google Scholar] [PubMed]
- Zuckerman, G.; Benitez, J. A prospective study of bidirectional endoscopy (colonoscopy and upper endoscopy) in the evaluation of patients with occult gastrointestinal bleeding. Am. J. Gastroenterol. 1992, 87, 62–66. [Google Scholar] [PubMed]
- Hsieh, Y.H.; Lin, H.J.; Tseng, K.C. Which should go first during same-day bidirectional endosocopy with propofol sedation? J. Gastroenterol. Hepatol. 2011, 26, 1559–1564. [Google Scholar] [CrossRef]
- Cao, Y.; Yang, J.; Li, J.; Ao, X.; Zhang, K.Y.; Shen, X.C.; Chen, D.F.; Lan, C.H. Comparison of procedural sequences in same-day painless bidirectional endoscopy: Single-center, prospective, randomized study. Dig. Endosc. 2017, 29, 330–337. [Google Scholar] [CrossRef] [Green Version]
- Triadafilopoulos, G.; Aslan, A. Same-day upper and lower inpatient endoscopy: A trend for the future. Am. J. Gastroenterol. 1991, 86, 952–955. [Google Scholar]
- Choi, G.J.; Oh, H.C.; Seong, H.K.; Kim, J.W.; Ko, J.S.; Kang, H. Comparison of procedural sequence in same-day bidirectional endoscopy: A systematic review and meta-analysis. Korean J. Intern. Med. 2020, 35, 331–341. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.W.; Cheng, C.L.; Liu, N.J.; Tang, J.H.; Kuo, Y.L.; Lin, C.H.; Tsui, Y.N.; Lee, B.P.; Hung, H.L. Which should go first during same-day upper and lower gastrointestinal endoscopydy. J. Gastroenterol. Hepatol. 2018, 33, 689–695. [Google Scholar] [CrossRef]
- Tang, J.H.; Cheng, C.L.; Kuo, Y.L.; Tsui, Y.N. Paired comparison of procedural sequence in same-day bidirectional endoscopy with moderate sedation and carbon dioxide insufflation: A prospective observational study. Saudi J. Gastroenterol. 2016, 22, 360–365. [Google Scholar] [CrossRef]
- Carter, D.; Lahat, A.; Papageorgiou, N.P.; Goldstein, S.; Eliakim, R.; Bardan, E. Comparison of procedural sequence in same-day consecutive bidirectional endoscopy using moderate sedation: A prospective randomized study. J. Clin. Gastroenterol. 2014, 48, 236–240. [Google Scholar] [CrossRef]
- Choi, J.S.; Youn, Y.H.; Lee, S.K.; Choi, J.Y.; Kim, H.M.; Kim, Y.J.; Han, K.J.; Cho, H.G.; Song, S.Y.; Cho, J.H. Which should go first during same-day upper and lower gastrointestinal endoscopy? A randomized prospective study focusing on colonoscopy performance. Surg. Endosc. 2013, 27, 2209–2215. [Google Scholar] [CrossRef]
- Cho, J.H.; Kim, J.H.; Lee, Y.C.; Song, S.Y.; Lee, S.K. Comparison of procedural sequences in same-day bidirectional endoscopy without benzodiazepine and propofol sedation: Starting at the bottom or the top. J. Gastroenterol. Hepatol. 2010, 25, 899–904. [Google Scholar] [CrossRef]
- Laoveeravat, P.; Thavaraputta, S.; Suchartlikitwong, S.; Vutthikraivit, W.; Mingbunjerdsuk, T.; Motes, A.; Nugent, K.; Perisetti, A.; Tharian, B.; Islam, S.; et al. Optimal sequences of same-visit bidirectional endoscopy: Systematic review and meta-analysis. Dig. Endosc. 2020, 32, 706–714. [Google Scholar] [CrossRef]
- Hsieh, Y.H.; Tseng, C.W.; Hu, C.T.; Koo, M.; Leung, F.W. Prospective multicenter randomized controlled trial comparing adenoma detection rate in colonoscopy using water exchange, water immersion, and air insufflation. Gastrointest. Endosc. 2017, 86, 192–201. [Google Scholar] [CrossRef]
- Cadoni, S.; Sanna, S.; Gallittu, P.; Argiolas, M.; Fanari, V.; Porcedda, M.L.; Erriu, M.; Leung, F.W. A randomized, controlled trial comparing real-time insertion pain during colonoscopy confirmed water exchange to be superior to water immersion in enhancing patient comfort. Gastrointest. Endosc. 2015, 81, 557–566. [Google Scholar] [CrossRef]
- Hsieh, Y.H.; Koo, M.; Leung, F.W. A patient-blinded randomized, controlled trial comparing air insufflation, water immersion, and water exchange during minimally sedated colonoscopy. Am. J. Gastroenterol. 2014, 109, 1390–1400. [Google Scholar] [CrossRef]
- Cadoni, S.; Ishaq, S.; Hassan, C.; Falt, P.; Fuccio, L.; Siau, K.; Leung, J.W.; Anderson, J.; Binmoeller, K.F.; Radaelli, F.; et al. Water-assisted colonoscopy: An international modified Delphi review on definitions and practice recommendations. Gastrointest. Endosc. 2021, 93, 1411–1420.e18. [Google Scholar] [CrossRef]
- Jia, H.; Koo, M.; Hsieh, Y.H.; Tseng, C.W.; Hu, C.T.; Zhang, L.; Dong, T.; Pan, Y.; Leung, F.W. Factors associated with adenoma detection in propofol-sedated patients. J. Clin. Gastroenterol. 2019, 53, 523–529. [Google Scholar] [CrossRef]
- Katzgraber, F.; Glenewinkel, F.; Fischler, S.; Rittner, C. Mechanism of fatal air embolism after gastrointestinal endoscopy. Int. J. Leg. Med. 1998, 111, 154–156. [Google Scholar] [CrossRef]
- Tseng, C.W.; Koo, M.; Hsieh, Y.H. Cecal intubation time between cap-assisted water exchange and water exchange colonoscopy: A randomized-controlled trial. Eur. J. Gastroenterol. Hepatol. 2017, 29, 1296–1302. [Google Scholar] [CrossRef]
- Tseng, C.W.; Koo, M.; Hsieh, Y.H. Cecal intubation time between the use of one-channel and two-channel water exchange colonoscopy: A randomized controlled trial. J. Gastroenterol. Hepatol. 2020, 35, 1562–1569. [Google Scholar] [CrossRef] [PubMed]
- Aldrete, J.A. The post-anesthesia recovery score revisited. J. Clin. Anesth. 1995, 7, 89–91. [Google Scholar] [CrossRef]
- Hassan, C.; Manning, J.; Gonzalez, M.A.A.; Sharma, P.; Epstein, M.; Bisschops, R. Improved detection of colorectal adenomas by high-quality colon cleansing. Endosc. Int. Open 2020, 8, E928–E937. [Google Scholar] [CrossRef] [PubMed]
- Jowhari, F.; Hookey, L. Gastroscopy should come before colonoscopy using CO2 insufflation in same day bidirectional endoscopies: A randomized controlled trial. J. Can. Assoc. Gastroenterol. 2020, 3, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Barr, J. Propofol: A new drug for sedation in the intensive care unit. Int. Anesthesiol. Clin. 1995, 33, 131–154. [Google Scholar] [CrossRef]
- Chen, S.C.; Rex, D.K. Review article: Registered nurse-administered propofol sedation for endoscopy. Aliment. Pharmacol. Ther. 2004, 19, 147–155. [Google Scholar] [CrossRef]
- Baudet, J.S.; Diaz-Bethencourt, D.; Aviles, J.; Aguirre-Jaime, A. Minor adverse events of colonoscopy on ambulatory patients: The impact of moderate sedation. Eur. J. Gastroenterol. Hepatol. 2009, 21, 656–661. [Google Scholar] [CrossRef]
- Lee, Y.C.; Wang, H.P.; Chiu, H.M.; Lin, C.P.; Huang, S.P.; Lai, Y.P.; Wu, M.S.; Chen, M.F.; Lin, J.T. Factors determining post-colonoscopy abdominal pain: Prospective study of screening colonoscopy in 1000 subjects. J. Gastroenterol. Hepatol. 2006, 21, 1575–1580. [Google Scholar] [CrossRef]
- Sumanac, K.; Zealley, I.; Fox, B.M.; Rawlinson, J.; Salena, B.; Marshall, J.K.; Stevenson, G.W.; Hunt, R.H. Minimizing postcolonoscopy abdominal pain by using CO2 insufflation: A prospective, randomized, double blind, controlled trial evaluating a new commercially available CO2 delivery system. Gastrointest. Endosc. 2002, 56, 190–194. [Google Scholar] [CrossRef]
| Variable | EGD First (n = 100) | Colonoscopy First (n = 100) | p Value |
|---|---|---|---|
| Male, n (%) | 38 (38) | 43 (43) | 0.471 † |
| Age, median (IQR), years | 59.5 (54.0–67.8) | 61.0 (53.0–67.0) | 0.883 § |
| Body-mass index, median (IQR), kg/m2 | 24.1 (21.7–25.9) | 24.3 (22.0–26.6) | 0.235 * |
| Smoking, n (%) | 2 (2) | 6 (6) | 0.279 ‡ |
| Alcoholism, n (%) | 6 (6) | 12 (12) | 0.138 † |
| Constipation, n (%) | 18 (18) | 17 (17) | 0.852 † |
| Chronic laxative use, n (%) | 5 (5) | 4 (4) | >0.999 ‡ |
| Previous abdominal/pelvic surgery, n (%) | 44 (44) | 39 (39) | 0.473 † |
| Indications for colonoscopy | |||
| Screening | 14 (14) | 23 (23) | 0.144 † |
| Surveillance | 86 (86) | 77 (77) | 0.144 † |
| Variable | EGD-First (n = 100) | Colonoscopy-First (n = 100) | p Value |
|---|---|---|---|
| Procedure time of bidirectional endoscopy, median (IQR), min | 33.1 (27.9–36.7) | 30.6 (27.2–33.5) | 0.005 * |
| Outcomes of colonoscopy | |||
| Cecal-intubation success, n (%) | 100 (100) | 100 (100) | >0.999 † |
| Cecal-intubation time, median (IQR) | 16.0 (12.1–19.1) | 13.7 (11.3–16.2) | <0.001 * |
| Difficult colonoscopy, n (%) | 30 (30) | 10 (10) | 0.001 |
| Colonoscopy withdrawal time, median (IQR) | 9.3 (7.7–11.4) | 10.2 (8.5–11.7) | 0.163 § |
| Cleaning time, median (IQR), min | 1.4 (1.0–1.9) | 1.4 (0.9–1.8) | 0.512 § |
| Inspection time, median (IQR), min | 6.7 (6.0–8.0) | 7.5 (6.1–8.5) | 0.060 § |
| Polypectomy time, median (IQR), min | 0.8 (0–1.7) | 0.9 (0.3–1.9) | 0.425 § |
| Colonoscopy procedure time, median (IQR) | 26.5 (20.4–27.0) | 24.0 (20.4–27.1) | 0.003 * |
| Volume of water infused during insertion (mL), median (IQR) | 1040 (750–1272) | 945 (750–1115) | 0.038 § |
| Volume of water aspirated during insertion (mL), median (IQR) | 1100 (900–1500) | 1000 (705–1300) | 0.021 § |
| Boston Bowel Preparation Scale, median (IQR) | |||
| Right colon | 3 (2–3) | 3 (3–3) | 0.105 § |
| Transverse colon | 3 (3–3) | 3 (3–3) | 0.684 § |
| Left colon | 3 (2–3) | 3 (3–3) | 0.013 § |
| Total score | 8.5 (8–9) | 9 (8–9) | 0.030 § |
| Adenoma-detection rate, n (%) | 45 (45) | 49 (49) | 0.571 † |
| Polyp-detection rate, n (%) | 71 (71) | 77 (77) | 0.333 † |
| Number of cases requiring abdominal compression, n (%) | 55 (55) | 57 (57) | 0.776 † |
| Number of cases requiring change of position, n (%) | 10 (10) | 7 (7) | 0.447 † |
| Outcomes of EGD | |||
| EGD procedure time, median (IQR) | 3.2 (2.7–3.8) | 3.1 (2.6–3.9) | 0.360 § |
| Patient tolerance during the EGD, median (IQR) | |||
| Counts of gag | 0 (0–0) | 0 (0–0) | 0.788 § |
| Counts of cough | 0 (0–0) | 0 (0–0) | 0.873 § |
| EGD technical adequacy, median (IQR) | 4 (4–4) | 4 (4–4) | 0.195 § |
| EGD findings, n (%) | |||
| Reflux esophagitis | 23 (23) | 29 (29) | 0.333 † |
| Gastritis | 32 (32) | 40 (40) | 0.239 † |
| Gastric ulcer | 19 (19) | 14 (14) | 0.446 † |
| Gastric polyp | 26 (26) | 27 (27) | 0.873 † |
| Gastric erosion | 11 (11) | 6 (6) | 0.205 † |
| Duodenal ulcer | 6 (6) | 4 (4) | 0.516 † |
| Variable | EGD-First (n = 100) | Colonoscopy-First (n = 100) | p Value |
|---|---|---|---|
| Propofol dose, median (IQR), mg | |||
| Initial dose | 100 (88–120) | 100 (90–110) | 0.176 § |
| Dose used during EGD | 0 (0–20) | 0 (0–50) | 0.049 § |
| Loading dose before the second procedure | 0 (0–20) | 50 (0–77.8) | <0.001 § |
| Dose used during colonoscopy | 80 (50–110) | 85 (50–120) | 0.636 § |
| Total dose | 200 (180–250) | 250 (200–300) | <0.001 § |
| Recovery time, median (IQR), min | 7.0 (4.0–10.7) | 13.5 (10.0–17.0) | <0.001 § |
| Turnover time of endoscopic room, median (IQR) | 39.5 (34.7–45.5) | 42.6 (38.3–49.3) | 0.004 |
| Sedation-related adverse events, n (%) | |||
| Bradycardia | 27 (27) | 31 (31) | 0.533 † |
| Tachycardia | 1 (1) | 1 (1) | >0.999 † |
| Oxygen desaturation | 2 (2) | 0 (0) | 0.497 ‡ |
| Hypertension | 19 (19) | 11 (11) | 0.113 † |
| Hypotension | 6 (6) | 2 (2) | 0.279 ‡ |
| Patients’ assessment of discomfort and satisfaction | |||
| Pain ^, median (IQR) | 0 (0–1) | 0 (0–0) | 0.004 § |
| Bloating ^, median (IQR) | 0 (0–2) | 0 (0–0) | 0.006 § |
| Nausea ^, median (IQR) | 0 (0–0) | 0 (0–0) | 0.951 § |
| Dizziness ^, median (IQR) | 0 (0–0) | 0 (0–0) | 0.830 § |
| Sore throat ^, median (IQR) | 0 (0–0) | 0 (0–0) | 0.325 § |
| Patient satisfaction #, median (IQR) | 10 (10–10) | 10 (9.7–10) | 0.322 § |
| Willingness to repeat, n (%) | 95 (95) | 89 (89) | 0.248 ‡ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, Y.-H.; Koo, M.; Tseng, C.-W. Comparison of Procedural Sequences in Sedated Same-Day Bidirectional Endoscopy with Water-Exchange Colonoscopy: A Randomized Controlled Trial. J. Clin. Med. 2022, 11, 1365. https://doi.org/10.3390/jcm11051365
Hsieh Y-H, Koo M, Tseng C-W. Comparison of Procedural Sequences in Sedated Same-Day Bidirectional Endoscopy with Water-Exchange Colonoscopy: A Randomized Controlled Trial. Journal of Clinical Medicine. 2022; 11(5):1365. https://doi.org/10.3390/jcm11051365
Chicago/Turabian StyleHsieh, Yu-Hsi, Malcolm Koo, and Chih-Wei Tseng. 2022. "Comparison of Procedural Sequences in Sedated Same-Day Bidirectional Endoscopy with Water-Exchange Colonoscopy: A Randomized Controlled Trial" Journal of Clinical Medicine 11, no. 5: 1365. https://doi.org/10.3390/jcm11051365
APA StyleHsieh, Y.-H., Koo, M., & Tseng, C.-W. (2022). Comparison of Procedural Sequences in Sedated Same-Day Bidirectional Endoscopy with Water-Exchange Colonoscopy: A Randomized Controlled Trial. Journal of Clinical Medicine, 11(5), 1365. https://doi.org/10.3390/jcm11051365







