Abstract
The objective of this in vitro study was to evaluate and compare the accuracy of zygomatic dental implant (ZI) placement carried out using a dynamic navigation system. Materials and Methods: Forty (40) ZIs were randomly distributed into one of two study groups: (A) ZI placement via a computer-aided dynamic navigation system (n = 20) (navigation implant (NI)); and (B) ZI placement using a conventional free-hand technique (n = 20) (free-hand implant (FHI)). A cone-beam computed tomography (CBCT) scan of the existing situation was performed preoperatively to plan the surgical approach for the computer-aided study group. Four zygomatic dental implants were placed in anatomically based polyurethane models (n = 10) manufactured by stereolithography, and a postoperative CBCT scan was performed. Subsequently, the preoperative planning and postoperative CBCT scans were added to dental implant software to analyze the coronal entry point, apical end point, and angular deviations. Results were analyzed using the Student’s t-test. Results: The results showed statistically significant differences in the apical end-point deviations between FHI and NI (p = 0.0018); however, no statistically significant differences were shown in the coronal entry point (p = 0.2617) or in the angular deviations (p = 0.3132). Furthermore, ZIs placed in the posterior region showed more deviations than the anterior region at the coronal entry point, apical end point, and angular level. Conclusions: The conventional free-hand technique enabled more accurate placement of ZIs than the computer-assisted surgical technique. In addition, placement of ZIs in the anterior region was more accurate than that in the posterior region.
1. Introduction
Zygomatic implants (ZIs) have proven to be a suitable treatment option in the restoration of the extremely atrophic, totally edentulous maxillae usually caused by maxillary resection in patients with oncological pathologies, congenital deformities, or metabolic disorders—patients undergoing radiotherapy—or immunosuppressed patients [1]. ZIs are especially indicated for use in patients with compromised vascularization, which can affect the outcome of bone grafts used to regenerate maxillary defects; they are also indicated in cases of incompatibility of the donor area [2]. Specifically, ZIs provide a predictable treatment option that prevents long waiting times before prosthetic rehabilitation when compared with alternative techniques for conventional implant placement using grafting materials [3]. Additionally, a recent meta-analysis reported a failure rate of 2.89% (CI-95% 1.83–3.96%) associated with conventional-length dental implants (n = 3549), while the failed implantation of ZIs (n = 1895) had an estimated incidence rate of 0.69% (CI-95% 0.21–1.16%) over a follow-up period ranging from 3 to 163 months [4].
In 1988, Branemark first described using an intrasinusal placement approach for ZIs; however, this technique can lead to sinusitis, dental implant failure, oroantral fistula, periorbital and conjunctival hematoma or edema, paresthesia, difficulty speaking, pain, and edema [5]. Alternative placement approaches that depend on bone availability have subsequently emerged, such as the extrasinusal, extramaxillary, or slot techniques [6]; however, these are not devoid of intraoperative complications, which are primarily linked to operator experience. Therefore, preoperative planning techniques using cone-beam computed tomography (CBCT) scans [7] have been recommended to enable accurate computer-aided surgery with both static and dynamic navigation systems [8]. These increase the accuracy of dental implant placement, thereby reducing the risk of intraoperative complications and maintaining high survival rates of patients receiving dental implants [9]. Computer-aided surgery using static navigation systems has been widely used for the placement of conventional-length dental implants, showing a high success rate; furthermore, static navigation techniques have shown a mean horizontal deviation of 1.2 mm at the coronal entry point, 1.4 mm at the apical end point, and an angular deviation of 3.5° [10]. Computer-aided surgery using dynamic navigation systems has shown lower mean horizontal deviations at the coronal entry point (0.71 ± 0.40 mm), apical end point (1.00 ± 0.49 mm), and angular deviation (2.26 ± 1.62°) [11]. Therefore, image-guided surgery approaches have been recommended to help increase the accuracy of ZI placement, preventing intraoperative and postoperative complications, as the length of ZIs is almost five times greater than a conventional-length dental implant; therefore, an entry-point or angular deviation of the dental implant bur may increase the apical-point deviation [12]. In addition, computer-aided surgery using dynamic navigation systems allows for free-hand implant navigation using high-precision motion tracking technology, preventing anatomical injuries [13]. Image-guided navigation systems also increase the accuracy of dental implant placement using artificial fiducial markers, which provide a virtual coordinate system linked to the surgical field or coordinate system of the patient [14]. However, computer-aided navigation systems are more expensive than surgical templates, and their accuracy depends on the learning curve and experience of the operator [15].
The objective of the present study was to evaluate the accuracy of placing ZIs using a dynamic navigation system. The null hypothesis (H0) stated that accuracy rates do not differ when comparing placement of ZIs using a dynamic navigation system versus a free-hand approach.
2. Materials and Methods
2.1. Study Design
This in vitro study was carried out between January and March 2021 at the Dental Center of Innovation and Advanced Specialties at Alfonso X El Sabio University in Madrid, Spain. The Ethical Committee of the Faculty of Health Sciences at Alfonso X El Sabio University approved the study in December 2020 (Process No. 25/2020). The patient gave their informed consent for the researchers to use their preoperative cone-beam computed tomography (CBCT) scan for the purposes of this study.
2.2. Experimental Procedure
Forty (40) ZIs (Galimplant, Sarria, Lugo, Spain) were planned and placed in teeth in positions 2.4 (4.3 mm × 30 mm, internal taper and conical wall), 2.2 (4.3 mm × 50 mm, internal taper and conical wall), 1.2 (4.3 mm × 52.5 mm, internal taper and conical wall), and 1.4 (4.3 mm × 35 mm, internal taper and conical wall). Researchers used an ANOVA to establish the sample size, achieving 80% power with a confidence level of 5%, with a variability between groups of 0.6 and an intragroup variability of 4, to identify differences in comparison with the null hypothesis H0: μ1 = μ2 = μ3 = μ4. Ten (10) anatomically based, standardized polyurethane models of a completely edentulous, atrophic, upper jaw maxilla were manufactured using a three-dimensional impression procedure (Sawbones Europe AB, Malmo, Sweden) based on a preoperative CBCT scan (WhiteFox, Satelec, Merignac, France). The scan was taken from a patient using the following exposure parameters: 8.0 mA, 105.0 kV peak, 7.20 s, with a 15 mm × 13 mm field of view (Figure 1). The anatomically based models were manufactured respecting the size and shape of the patient.
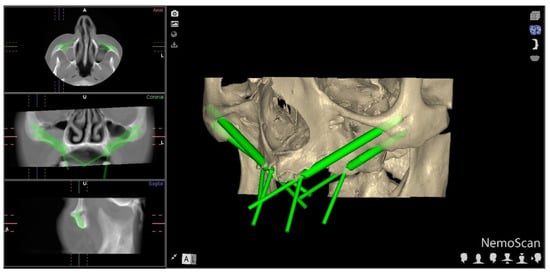
Figure 1.
Preoperative planning of ZI placement based on the CBCT scan taken of the patient. Detail of the coronal, sagittal, and axial views, and three-dimensional reconstruction.
Afterwards, the models were fixed onto an artificial head to simulate the clinical conditions (Figure 2).
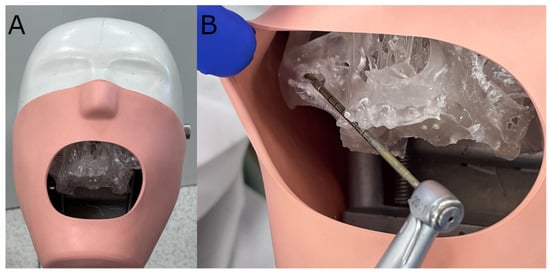
Figure 2.
(A) Polyurethane model fixed onto an artificial head and (B) drilling procedure.
Researchers randomized the ZIs (Epidat 4.1, Galicia, Spain), which were assigned to one of two study groups: (A) ZI (Galimplant, Sarria, Lugo, Spain) placement using a computer-aided dynamic navigation system (Navident, ClaroNav, Toronto, ON, Canada) (n = 20) (navigation implant (NI)); and (B) manual ZI (Galimplant, Sarria, Lugo, Spain) placement using a free-hand technique (n = 20) (freehand implant (FHI)). The order of placement of the ZIs (Galimplant, Sarria, Lugo, Spain) was randomized across the study groups (Epidat 4.1, Galicia, Spain), beginning with the NI study group and followed by the FHI control group.
A preoperative CBCT scan was taken of the NI anatomically based standardized polyurethane models (WhiteFox, Satelec, Merignac, France) prior to placing a jaw tag; the use of polyurethane was based on the American Society for Testing and Materials’ (ASTM F-1839-08) approval of the use of polyurethane for testing instruments and dental implants (“Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Test Orthopedic Devices for Instruments”) [16]. This black-and-white tag was affixed to the dental surface of the anatomically based, standardized polyurethane models using a photopolymerized composite resin (Navistent, ClaroNav, Toronto, ON, Canada). The datasets obtained from the CBCT scan were uploaded to treatment-planning software (Navident, ClaroNav, Toronto, ON, Canada) on a laptop computer mounted onto a mobile unit to simulate placement of the ZIs in accordance with the prior surgical planning (Figure 3A). An additional black-and-white drill tag was affixed to the handpiece (W & H, Bürmoos, Austria). The researchers calibrated and identified both of the optical reference markers with an optical triangulation tracking system using stereoscopic motion-tracking cameras, orienting the drilling process in real time to ensure that the planned angle, pathway, and depth were achieved. A ZI system (Galimplant, Sarria, Lugo, Spain) was used to perform the drilling, with this procedure being monitored using the computer-aided dynamic navigation system installed onto the laptop computer (Figure 3B).
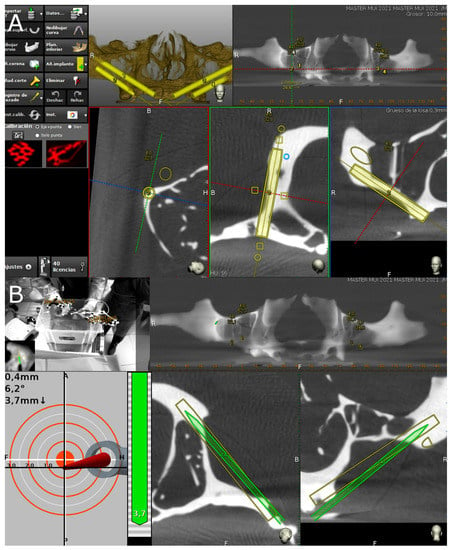
Figure 3.
(A) Preoperative planning of placement of ZIs with the dynamic navigation appliance using treatment-planning software, and (B) tracking procedure during ZI placement.
The conventional free-hand technique was used to place all ZIs (Galimplant, Sarria, Lugo, Spain) that had been randomly assigned to the FHI control group, with the operator having access to the preoperative planning and CBCT scan. All ZIs (Galimplant, Sarria, Lugo, Spain) were placed by a unique operator with prior surgical experience.
2.3. Measurement Procedure
Following placement of the ZIs, the researchers conducted postoperative CBCT scans (WhiteFox, Satelec, Merignac, France) using the aforementioned exposure parameters. The planning and postoperative CBCT scans (WhiteFox, Satelec, Merignac, France) of the different study groups were subsequently imported into 3D implant-planning software (NemoScan, Nemotec, Madrid, Spain). The scans were then overlaid in order to assess the apical deviation, measured at the coronal entry point (mm), apical end point (mm), and angular deviation (°), with the latter measured at the center of the cylinder. Any deviations that were noted in any of the implants were subsequently analyzed and compared between the axial, sagittal, and coronal views (Figure 4A–C) by an independent operator. In addition, deviations in the positions of the zygomatic dental implants were also recorded and analyzed.
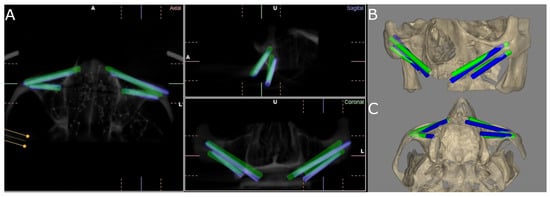
Figure 4.
(A) CBCT images of the coronal, sagittal, and axial views; and (B) front and (C) bottom views of the three-dimensional reconstruction of the measurement procedure contrasted against the preoperative planning (green cylinders) and postoperative ZI placement (blue cylinders) of the ZIs placed on the experimental model.
2.4. Statistical Analysis
For each of the response variables, tables were produced with summaries of the following statistics according to group, position and group, and position: number of observations, mean, standard deviation, median, and the minimum and maximum values. These were represented graphically by box plots. Linear regression models with repeated measures were adjusted to analyze the differences according to group, according to position, and the interaction between both variables. Where statistically significant differences were detected, two-to-two comparisons were made between groups/positions. The p-values were adjusted using the Tukey method to correct the type I error. The statistical analysis was carried out using the software SAS v.9.4 (SAS Institute Inc., Cary, NC, USA). Statistical decisions were made using a significance level of 0.05.
3. Results
Table 1 shows the mean, median, and SD values with 95% confidence intervals for the coronal entry point (mm), apical end point (mm), and angular deviations (°) of the NI study group and the FHI control group.

Table 1.
Descriptive values of deviations at the coronal entry point (mm), apical end point (mm), and angular (°) deviations of the computer-aided dynamic navigation technique (NI) and the free-hand approach.
The paired Student’s t-test did not find any statistically significant differences in the coronal entry-point deviations between the study groups (p = 0.2617), nor in the ZI positions (p = 0.1649). However, statistically significant deviations were observed between the computer-aided dynamic navigation technique (NI) and the free-hand approach at the ZI position 2.4 (p = 0.0155) (Figure 5).
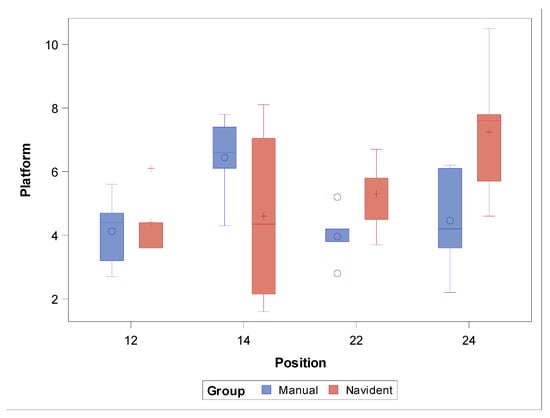
Figure 5.
Box plot of deviations at the coronal entry point observed in the study groups and ZI positions. Median values are represented by the horizontal lines within each box. The symbols represent extreme values.
The paired Student’s t-test revealed statistically significant differences in the apical end-point deviations between the FHI control group and the NI study group (p = 0.0018). On the other hand, no statistically significant differences were observed between the zygomatic dental implant positions (p = 0.1856), except at the ZI position 2.4 (p = 0.0005) (Figure 6).
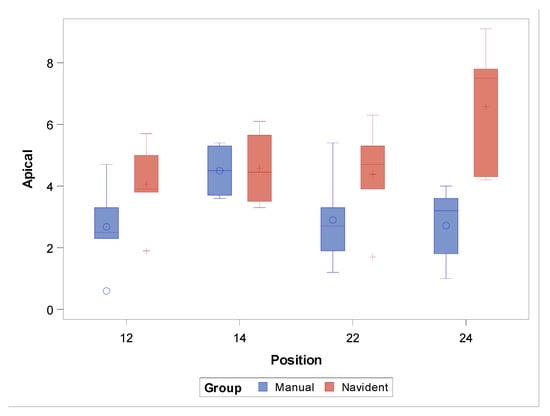
Figure 6.
Box plot of apical end-point deviations recorded in the study groups and ZI positions. Median values are represented by the horizontal lines within each box. The symbols represent extreme values.
The paired Student’s t-test found no statistically significant differences between the angular deviations of the study groups (p = 0.3132); on the other hand, statistically significant differences were shown for the zygomatic dental implant positions (p = 0.0008), especially at the ZI position 1.4 (p = 0.0040) (Figure 7).
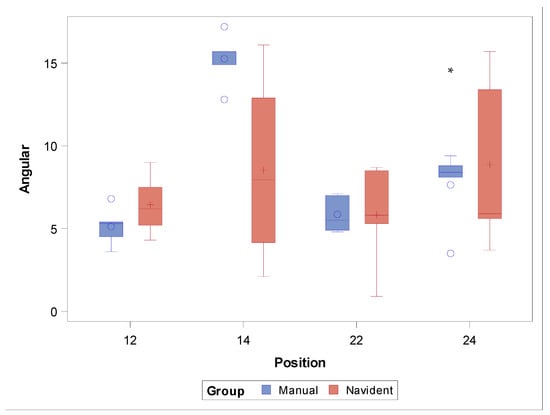
Figure 7.
Box plot of angular deviations found in the study groups and ZI positions. Median values are represented by the horizontal lines within each box. The symbols represent extreme values.
In summary, the FHI approach showed lower deviation values at the coronal entry point and the apical end point. This may be because the ZIs assigned to the FHI control group were the last to be placed, enabling the operator to learn and to memorize the correct position of the ZI. Furthermore, ZIs placed in posterior regions showed higher levels of deviation at the coronal entry point, apical end point, and angular level.
One ZI was withdrawn from the NI study group because the osteotomy site preparations did not provide sufficient stability for the ZI.
4. Discussion
The results of the present study reject the null hypothesis (H0), which states that there is no difference in accuracy when comparing placement of ZIs using a dynamic navigation system versus a free-hand approach.
The primary findings of the present study indicate that the free-hand conventional technique for ZI placement was more accurate than the computer-aided dynamic navigation technique at the coronal and apical levels; however, the computer-aided dynamic navigation technique showed more accuracy than the free-hand conventional technique at the angular level.
Hung et al. [17], Xiaojun et al. [18], Chen et al. [19], Hung et al. [20], Zhu et al. [8], and Jorba-García et al. [21] found computer-aided dynamic navigation to have greater accuracy than the free-hand conventional approach for the placement of conventional-length dental implants. Nevertheless, Brief et al. found that, although computer-aided navigation techniques are significantly more accurate than free-hand conventional techniques, the level of accuracy provided by the free-hand conventional technique is sufficient for most clinical situations [22]. However, Aydemir et al. reported that the conventional free-hand technique provides greater accuracy at the coronal entry-point and apical end-point levels than the computer-assisted dynamic navigation technique in the placement of ZIs, although the computer-aided dynamic navigation technique resulted in lower angular deviation than the free-hand conventional technique [23]. Moreover, Jung et al. found similar safety levels, outcomes, morbidity, and efficiency between computer-aided navigation techniques and free-hand conventional techniques for placement of conventional-length dental implants [24]. These results corroborate those of the present study, and the learning curve required for the use of computer-aided dynamic navigation systems may explain the discrepancies observed between the dynamic navigation system and the free-hand conventional technique [11]. Additionally, Mediavilla Guzmán et al. warned of low methodological quality in the studies related to ZIs, which makes it difficult to compare the results of the different studies [13]. Gunkel et al. also found that studies conducted under laboratory or in vitro conditions showed higher accuracy rates than clinical studies [25]. Likewise, Kim et al. [26] and Tahmaseb et al. [27] reported variability in the accuracy of computer-aided surgery using static navigation systems, depending on the study design.
Otherwise, Jorba-García et al. showed a mean angular deviation of 2.1° and a mean horizontal deviation of 0.46 mm at the coronal entry point for computer-aided surgery using dynamic navigation systems [28]. Xiaojun et al. showed a mean horizontal deviation of 1.36 ± 0.59 mm at the coronal entry point of conventional-length dental implants [18]; Chen et al., 1.12 ± 0.29 mm [14]; Hung et al., 1.07 ± 0.15 mm [20]; Hung et al., 1.35 ± 0.75 mm [17]; Block et al., 0.4 mm [29]; Kaewsiri et al., 1.05 ± 0.44 mm [30]; and Zhou et al., 1.56 ± 0.54 mm [8]. However, the present study showed a higher mean horizontal deviation at the coronal entry point (5.43 ± 2.13 mm), possibly due to the learning curve and operator experience. Kaewsiri et al. reported a mean horizontal deviation of 1.29 ± 0.50 mm at the apical end point, directly correlated with the length of the dental implant (8, 10, and 12 mm) [30]. Consequently, the horizontal deviation at the apical end point would be higher in ZIs than in conventional-length dental implants. In addition, Chrcanovic et al. reported an anteroposterior angular deviation of 8.06 ± 6.40° and craniocaudal of 11.20 ± 9.75°, which led to the invasion of the infratemporal fossa and the orbit by the ZIs [31]. Moreover, Vrielinck et al. found a mean angular deviation of 5.1° (ranging from 0.8 to 9.0° [32]; Xiaojun et al., 4.1 ± 0.9° [18]; Zhou et al., 2.52 ± 0.84° [8]; Hung et al., 1.37 ± 0.21° [17]; Hung et al., 2.05 ± 1.02° [20]; and Chen et al., 0.19 ± 0.92° [14]. These results are slightly lower than those obtained in the present study (7.36 ± 4.12°). These deviation values may lead to clinical and/or prosthetic complications in 36.4% of ZI placements, primarily due to a lack of primary stability [33]. In the present study, one ZI randomly placed using the dynamic navigation system was also removed due to insufficient stability at the prepared osteotomy site. In addition, Lan et al. described all complications related to the ZI placement procedure, reporting a malposition rate of 12% (95% confidence interval [CI]: 4 to 23%), surgical guiding failure rate of 11% (95% CI: 3 to 21%), and local infection/injury rate of 10% (95% CI: 3 to 18%) [34]. Additionally, Gutiérrez et al. reported that the prosthetic rehabilitations of ZIs have shown a low incidence of prosthetic complications (4.9% (95% CI: 2.7–7.3%)), regardless of the prosthetic treatment. The present study also found that the ZI placed in position 2.4 showed statistically significant deviations at the coronal entry point, and the ZI placed in position 1.4 showed statistically significant deviations in angular deviation. In summary, the ZIs placed in the anterior region showed lower deviations than the ZIs placed in the posterior region, likely due to better accessibility and visibility of the operative field.
The findings of the present study can be useful to clinicians in selecting the more accurate technique for ZI placement in patients with atrophied maxilla who must undergo full-arch rehabilitation by means of ZIs. The authors recommend improving the methodological quality of studies and increasing the body of evidence by way of additional randomized studies implementing new computer-assisted navigation techniques.
5. Conclusions
Within the limitations of the present study, the results indicated that the free-hand conventional technique provided greater accuracy in the placement of ZIs than the computer-assisted surgical technique. In addition, placement of ZIs in the anterior region was more accurate than that in the posterior region.
Author Contributions
Conceptualization, J.R.G.R., I.G.Á. and Á.Z.-M.; design, V.M.d.P.H.; data acquisition, E.R.D.; formal analysis, J.P.M.; statistical analyses, Á.Z.-M. and S.H.M.; review and editing, J.M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available on request, pursuant to any applicable restrictions (e.g., ethical or privacy considerations).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bidra, A.S.; Jacob, R.F.; Taylor, T.D. Classification of maxillectomy defects: A systematic review and criteria necessary for a universal description. J. Prosthet. Dent. 2012, 107, 261–270. [Google Scholar] [CrossRef]
- Rosenstein, J.; Dym, H. Zygomatic Implants: A Solution for the Atrophic Maxilla. Dent. Clin. N. Am. 2020, 64, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Davó, R.; Felice, P.; Pistilli, R.; Barausse, C.; Marti-Pages, C.; Ferrer-Fuertes, A.; Ippolito, D.R.; Esposito, M. Immediately loaded zygomatic implants vs. conventional dental implants in augmented atrophic maxillae: 1-year post-loading results from a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 145–161. [Google Scholar] [PubMed]
- Gutiérrez Muñoz, D.; Obrador Aldover, C.; Zubizarreta-Macho, Á.; González Menéndez, H.; Lorrio Castro, J.; Peñarrocha-Oltra, D.; Montiel-Company, J.M.; Hernández Montero, S. Survival Rate and Prosthetic and Sinus Complications of Zygomatic Dental Implants for the Rehabilitation of the Atrophic Edentulous Maxilla: A Systematic Review and Meta-Analysis. Biology 2021, 10, 601. [Google Scholar] [CrossRef] [PubMed]
- Brånemark, P.I.; Gröndahl, K.; Ohrnell, L.O.; Nilsson, P.; Petruson, B.; Svensson, B.; Engstrand, P.; Nannmark, U. Zygoma fixture in the management of advanced atrophy of the maxilla: Technique and long-term results. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2004, 38, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; Nobre Mde, A.; Lopes, I. A new approach to rehabilitate the severely atrophic maxilla using extramaxillary anchored implants in immediate function: A pilot study. J. Prosthet. Dent. 2008, 100, 354–366. [Google Scholar] [CrossRef]
- Omami, G.; Al Yafi, F. Should Cone Beam Computed Tomography Be Routinely Obtained in Implant Planning? Dent. Clin. N. Am. 2019, 63, 363–379. [Google Scholar] [CrossRef]
- Zhou, W.; Fan, S.; Wang, F.; Huang, W.; Jamjoom, F.Z.; Wu, Y. A novel extraoral registration method for a dynamic navigation system guiding zygomatic implant placement in patients with maxillectomy defects. Int. J. Oral Maxillofac. Surg. 2021, 50, 116–120. [Google Scholar] [CrossRef]
- Chana, H.; Smith, G.; Bansal, H.; Zahra, D. A Retrospective Cohort Study of the Survival Rate of 88 Zygomatic Implants Placed Over an 18-year Period. Int. J. Oral Maxillofac. Implants 2019, 34, 461–470. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 16, 416–435. [Google Scholar] [CrossRef] [Green Version]
- Stefanelli, L.V.; DeGroot, B.S.; Lipton, D.I.; Mandelaris, G.A. Accuracy of a Dynamic Dental Implant Navigation System in a Private Practice. Int. J. Oral Maxillofac. Implants 2019, 34, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, F.; Huang, W.; Fan, S. Real-Time Navigation in Zygomatic Implant Placement: Workflow. Oral Maxillofac. Surg. Clin. N. Am. 2019, 31, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Mediavilla Guzmán, A.; Riad Deglow, E.; Zubizarreta-Macho, Á.; Agustín-Panadero, R.; Hernández Montero, S. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Navigation for Dental Implant Placement: An In Vitro Study. J. Clin. Med. 2019, 8, 2123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.K.; Yuh, D.Y.; Huang, R.Y.; Fu, E.; Tsai, C.F.; Chiang, C.Y. Accuracy of Implant Placement with a Navigation System, a Laboratory Guide, and Freehand Drilling. Int. J. Oral Maxillofac. Implants 2018, 33, 1213–1218. [Google Scholar] [CrossRef]
- Gargallo-Albiol, J.; Barootchi, S.; Salomó-Coll, O.; Wang, H.L. Advantages and disadvantages of implant navigation surgery. A systematic review. Ann. Anat. 2019, 225, 1–10. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; Pontes, A.E.; Piattelli, A.; Iezzi, G. Primary Stability of Dental Implants in Low-Density (10 and 20 pcf) Polyurethane Foam Blocks: Conical vs. Cylindrical Implants. Int. J. Environ. Res. Public Health 2020, 17, 2617. [Google Scholar] [CrossRef] [Green Version]
- Hung, K.F.; Wang, F.; Wang, H.W.; Zhou, W.J.; Huang, W.; Wu, Y.Q. Accuracy of a real-time surgical navigation system for the placement of quad zygomatic implants in the severe atrophic maxilla: A pilot clinical study. Clin. Implant Dent. Relat. Res. 2017, 19, 458–465. [Google Scholar] [CrossRef]
- Xiaojun, C.; Ming, Y.; Yanping, L.; Yiqun, W.; Chengtao, W. Image guided oral implantology and its application in the placement of zygoma implants. Comput. Methods Programs Biomed. 2009, 93, 162–173. [Google Scholar] [CrossRef]
- Chen, X.; Wu, Y.; Wang, C. Application of a surgical navigation system in the rehabilitation of maxillary defects using zygoma implants: Report of one case. Int. J. Oral Maxillofac. Implants 2011, 26, e29–e34. [Google Scholar]
- Hung, K.; Huang, W.; Wang, F.; Wu, Y. Real-Time Surgical Navigation System for the Placement of Zygomatic Implants with Severe Bone Deficiency. Int. J. Oral Maxillofac. Implants 2016, 31, 1444–1449. [Google Scholar] [CrossRef] [Green Version]
- Jorba-García, A.; Figueiredo, R.; González-Barnadas, A.; Camps-Font, O.; Valmaseda-Castellón, E. Accuracy and the role of experience in dynamic computer guided dental implant surgery: An in-vitro study. Med. Oral Patol. Oral Cir. Bucal. 2019, 24, e76–e83. [Google Scholar] [CrossRef] [PubMed]
- Brief, J.; Edinger, D.; Hassfeld, S.; Eggers, G. Accuracy of image-guided implantology. Clin. Oral Implants Res. 2005, 16, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Aydemir, C.A.; Arısan, V. Accuracy of dental implant placement via dynamic navigation or the freehand method: A split-mouth randomized controlled clinical trial. Clin. Oral Implants Res. 2020, 31, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Schneider, D.; Ganeles, J.; Wismeijer, D.; Zwahlen, M.; Hämmerle, C.H.; Tahmaseb, A. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implants 2009, 24, 92–109. [Google Scholar]
- Gunkel, A.R.; Freysinger, W.; Thumfart, W.F. Experience with various 3-dimensional navigation systems in head and neck surgery. Arch. Otolaryngol. Head Neck Surg. 2000, 126, 390–395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.G.; Lee, W.J.; Lee, S.S.; Heo, M.S.; Huh, K.H.; Choi, S.C.; Kim, T.I.; Yi, W.J. An advanced navigational surgery system for dental implants completed in a single visit: An in vitro study. J. Craniomaxillofac. Surg. 2015, 43, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 25–42. [Google Scholar] [CrossRef] [Green Version]
- Jorba-García, A.; González-Barnadas, A.; Camps-Font, O.; Figueiredo, R.; Valmaseda-Castellón, E. Accuracy assessment of dynamic computer-aided implant placement: A systematic review and meta-analysis. Clin Oral Investig. 2021, 25, 2479–2494. [Google Scholar] [CrossRef]
- Block, M.S.; Emery, R.W.; Lank, K.; Ryan, J. Implant Placement Accuracy Using Dynamic Navigation. Int. J. Oral Maxillofac. Implants 2017, 32, 92–99. [Google Scholar] [CrossRef]
- Kaewsiri, D.; Panmekiate, S.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of static vs. dynamic computer-assisted implant surgery in single tooth space: A randomized controlled trial. Clin. Oral Implants Res. 2019, 30, 505–514. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Oliveira, D.R.; Custódio, A.L. Accuracy evaluation of computed tomography-derived stereolithographic surgical guides in zygomatic implant placement in human cadavers. J. Oral Implantol. 2010, 36, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Vrielinck, L.; Politis, C.; Schepers, S.; Pauwels, M.; Naert, I. Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe bone atrophy using customized drill guides. Preliminary results from a prospective clinical follow-up study. Int. J. Oral Maxillofac. Surg. 2003, 32, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Ramezanzade, S.; Yates, J.; Tuminelli, F.J.; Keyhan, S.O.; Yousefi, P.; Lopez-Lopez, J. Zygomatic implants placed in atrophic maxilla: An overview of current systematic reviews and meta-analysis. Maxillofac. Plast. Reconstr. Surg. 2021, 43, 1. [Google Scholar] [CrossRef] [PubMed]
- Lan, K.; Wang, F.; Huang, W.; Davó, R.; Wu, Y. Quad Zygomatic Implants: A Systematic Review and Meta-analysis on Survival and Complications. Int. J. Oral Maxillofac. Implants 2021, 36, 21–29. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).