Understanding the Impact of Child, Intervention, and Family Factors on Developmental Trajectories of Children with Hearing Loss at Preschool Age: Design of the AChild Study
Abstract
:1. Introduction
1.1. Language and Psycho-Social and Family Outcomes
1.2. Child, Family and Intervention Factors That Affect Developmental Outcomes
1.3. Rationale
1.4. Objectives and Hypotheses
- Objective 1
- Hypothesis 1
- Objective 2
- Hypothesis 2
- audiological factors (access to spoken language by means of early optimal fitting and constant use of hearing technology)
- access to signed language
- family factors (parental stress, family–child interaction, media use, and parental self-efficacy)
- family-centred intervention (mediated by family factors)
- e.
- child HL (degree of HL)
- f.
- child nonverbal cognition and additional disabilities/comorbidities
- g.
- aetiology of HL (including genotype)
- h.
- family factors (SES, parental education)
- Objective 3
- Hypothesis 3
- (a)
- child linguistic and social communication development
- (b)
- child behavioural problems
- (c)
- child emotional problems
- (d)
- child health
- (e)
- quality of parent–child interaction (e.g., facilitative language strategies, and parental responsiveness)
- (f)
- family-centred early intervention services
- (g)
- non-malleable family resources (e.g., SES, and parental education)
- Objective 4
1.5. Data Resource Areas
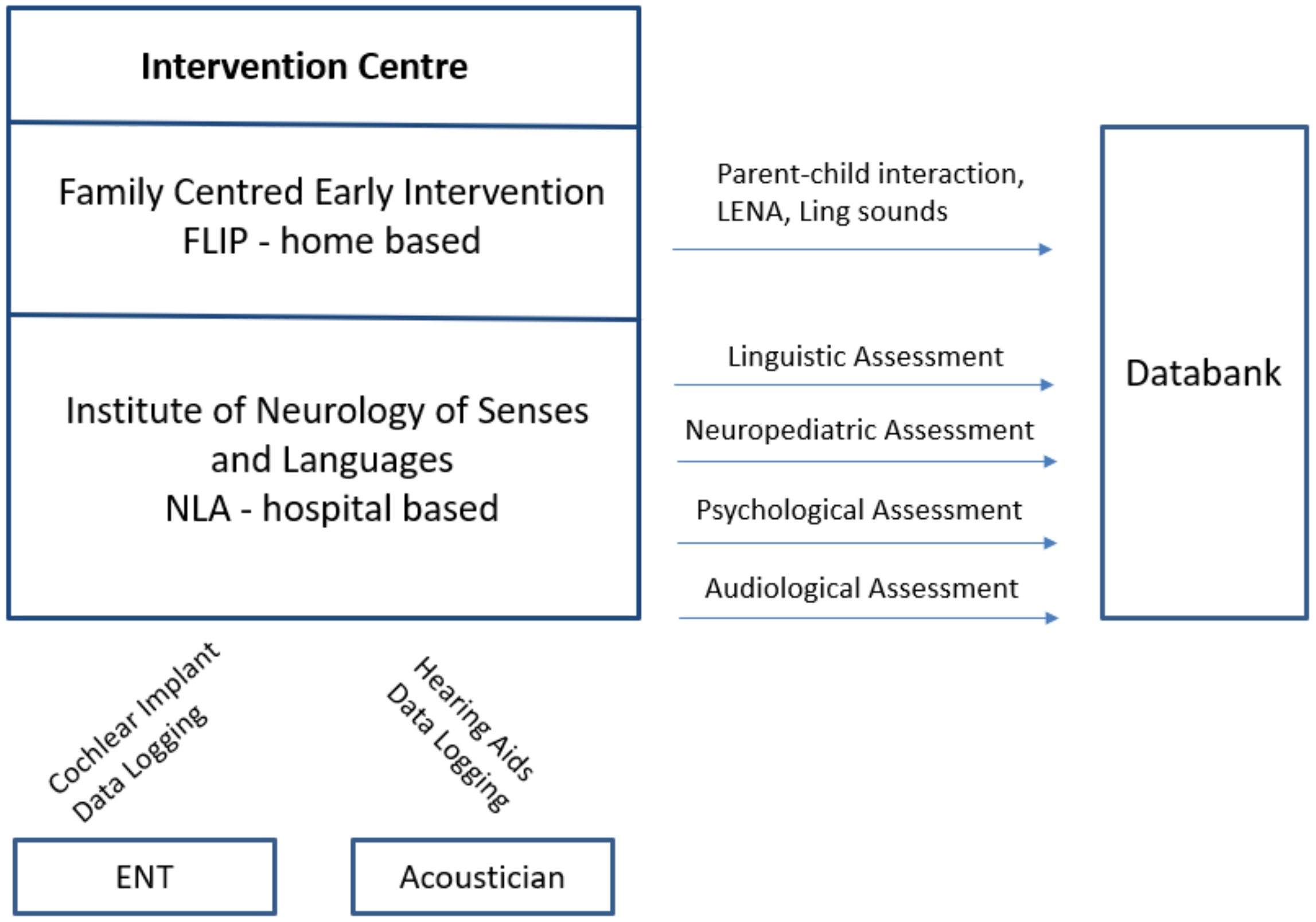
1.5.1. Upper Austria
1.5.2. Lower Austria
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection
2.4. Measures
2.5. Data Organization
2.6. Statistics
2.7. Strengths of the AChild Study
3. Discussion
Challenges and Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Childhood Hearing Loss: Strategies for Prevention and Care. Available online: https://www.who.int/publications-detail/childhood-hearing-loss-strategies-for-prevention-and-care (accessed on 4 June 2021).
- Butcher, E.; Dezateux, C.; Cortina-Borja, M.; Knowles, R.L. Prevalence of permanent childhood hearing loss detected at the universal newborn hearing screen: Systematic review and meta-analysis. PLoS ONE 2019, 14, e0219600. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Global Estimates on Prevalence of Hearing Loss: Prevention of Deafness. Available online: https://www.who.int/pbd/deafness/estimates/en/ (accessed on 4 June 2021).
- Shearer, A.; Hildebrand, M.; Smith, R. Hereditary Hearing Loss and Deafness Overview. Available online: https://www.ncbi.nlm.nih.gov/sites/books/NBK1434/ (accessed on 4 June 2021).
- Gallaudet Research Institute. Regional and National Summary Report of Data from the 2009-10 Annual Survey of Deaf and Hard of Hearing Children and Youth. Available online: https://research.gallaudet.edu/Demographics/2010_National_Summary.pdf (accessed on 20 April 2020).
- Van Naarden Braun, K.; Christensen, D.; Doernberg, N.; Schieve, L.; Rice, C.; Wiggins, L.; Schendel, D.; Yeargin-Allsopp, M. Trends in the prevalence of autism spectrum disorder, cerebral palsy, hearing loss, intellectual disability, and vision impairment, metropolitan atlanta, 1991–2010. PLoS ONE 2015, 10, e0124120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallaudet Research Institute. 2013-14 Regional and National Summary. Available online: https://www.gallaudet.edu/documents/Research-Support-and-International-Affairs/Intl%20Affairs/Demographics/AS14_RegNat.pdf (accessed on 4 June 2021).
- Holzinger, D.; Weishaupt, A.; Fellinger, P.; Beitel, C.; Fellinger, J. Prevalence of 2.2 per mille of significant hearing loss at school age suggests rescreening after NHS. Int. J. Pediatr. Otorhinolaryngol. 2016, 87, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Appachi, S.; Specht, J.L.; Raol, N.; Lieu, J.E.C.; Cohen, M.S.; Dedhia, K.; Anne, S. Auditory outcomes with hearing rehabilitation in children with unilateral hearing loss: A systematic review. Otolaryngol. Head Neck Surg. 2017, 157, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Lieu, J.E.C.; Kenna, M.; Anne, S.; Davidson, L. Hearing loss in children: A review. JAMA 2020, 324, 2195–2205. [Google Scholar] [CrossRef] [PubMed]
- Fellinger, J.; Holzinger, D.; Pollard, R. Mental health of deaf people. Lancet 2012, 379, 1037–1044. [Google Scholar] [CrossRef]
- Holzinger, D.; Hofer, J.; Dall, M. Frühe Prädiktoren der Sprachentwicklung von Kindern mit permanenter Hörstörung. Kindh. Entwickl. 2021, 30, 25–36. [Google Scholar] [CrossRef]
- Sarant, J.Z.; Holt, C.M.; Dowell, R.C.; Rickards, F.W.; Blamey, P.J. Spoken language development in oral preschool children with permanent childhood deafness. J. Deaf Stud. Deaf Educ. 2009, 14, 205–217. [Google Scholar] [CrossRef] [Green Version]
- Ching, T.Y.C.; Dillon, H.; Marnane, V.; Hou, S.; Day, J.; Seeto, M.; Crowe, K.; Street, L.; Thomson, J.; van Buynder, P.; et al. Outcomes of early- and late-identified children at 3 years of age: Findings from a prospective population-based study. Ear Hear. 2013, 34, 535–552. [Google Scholar] [CrossRef] [Green Version]
- Boons, T.; Brokx, J.P.L.; Dhooge, I.; Frijns, J.H.M.; Peeraer, L.; Vermeulen, A.; Wouters, J.; van Wieringen, A. Predictors of spoken language development following pediatric cochlear implantation. Ear Hear. 2012, 33, 617–639. [Google Scholar] [CrossRef] [Green Version]
- Cupples, L.; Ching, T.Y.; Button, L.; Seeto, M.; Zhang, V.; Whitfield, J.; Gunnourie, M.; Martin, L.; Marnane, V. Spoken language and everyday functioning in 5-year-old children using hearing aids or cochlear implants. Int. J. Audiol. 2018, 57, S55–S69. [Google Scholar] [CrossRef] [PubMed]
- Yoshinaga-Itano, C.; Sedey, A.L.; Wiggin, M.; Chung, W. Early hearing detection and vocabulary of children with hearing loss. Pediatrics 2017, 140, e20162964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomblin, J.B.; Harrison, M.; Ambrose, S.E.; Walker, E.A.; Oleson, J.J.; Moeller, M.P. Language Outcomes in Young Children with Mild to Severe Hearing Loss. Ear Hear. 2015, 36 (Suppl. 1), 76S–91S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomblin, J.B.; Oleson, J.; Ambrose, S.E.; Walker, E.A.; McCreery, R.W.; Moeller, M.P. Aided hearing moderates the academic outcomes of children with mild to severe hearing loss. Ear Hear. 2020, 41, 775–789. [Google Scholar] [CrossRef]
- Stika, C.J.; Eisenberg, L.S.; Carter, A.S.; Johnson, K.C.; Hammes Ganguly, D.M.; Henning, S.C.; Des Jardin, J.L. Developmental outcomes in early-identified children who are hard of hearing at 2 to 3 years of age. Ear Hear. 2021, 42, 1238–1252. [Google Scholar] [CrossRef]
- Theunissen, S.C.P.M.; Rieffe, C.; Kouwenberg, M.; de Raeve, L.J.I.; Soede, W.; Briaire, J.J.; Frijns, J.H.M. Behavioral problems in school-aged hearing-impaired children: The influence of sociodemographic, linguistic, and medical factors. Eur. Child Adolesc. Psychiatry 2014, 23, 187–196. [Google Scholar] [CrossRef]
- Dammeyer, J. Psychosocial development in a Danish population of children with cochlear implants and deaf and hard-of-hearing children. J. Deaf Stud. Deaf Educ. 2010, 15, 50–58. [Google Scholar] [CrossRef] [Green Version]
- Leigh, G.; Ching, T.Y.C.; Crowe, K.; Cupples, L.; Marnane, V.; Seeto, M. Factors affecting psychosocial and motor development in 3-year-old children who are deaf or hard of hearing. J. Deaf Stud. Deaf Educ. 2015, 20, 331–342. [Google Scholar] [CrossRef] [Green Version]
- Dirks, E.; Uilenburg, N.; Rieffe, C. Parental stress among parents of toddlers with moderate hearing loss. Res. Dev. Disabil. 2016, 55, 27–36. [Google Scholar] [CrossRef]
- Stika, C.J.; Eisenberg, L.S.; Johnson, K.C.; Henning, S.C.; Colson, B.G.; Ganguly, D.H.; DesJardin, J.L. Developmental outcomes of early-identified children who are hard of hearing at 12 to 18 months of age. Early Hum. Dev. 2015, 91, 47–55. [Google Scholar] [CrossRef] [Green Version]
- Vohr, B.; Jodoin-Krauzyk, J.; Tucker, R.; Johnson, M.J.; Topol, D.; Ahlgren, M. Early language outcomes of early-identified infants with permanent hearing loss at 12 to 16 months of age. Pediatrics 2008, 122, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Hintermair, M. Parental resources, parental stress, and socioemotional development of deaf and hard of hearing children. J. Deaf Stud. Deaf Educ. 2006, 11, 493–513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomblin, J.B.; Oleson, J.J.; Ambrose, S.E.; Walker, E.; Moeller, M.P. The influence of hearing aids on the speech and language development of children with hearing loss. JAMA Otolaryngol. Head Neck Surg. 2014, 140, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Walker, E.A.; Holte, L.; McCreery, R.W.; Spratford, M.; Page, T.; Moeller, M.P. The influence of hearing aid use on outcomes of children with mild hearing loss. J. Speech Lang. Hear Res. 2015, 58, 1611–1625. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cupples, L.; Ching, T.Y.C.; Crowe, K.; Seeto, M.; Leigh, G.; Street, L.; Day, J.; Marnane, V.; Thomson, J. Outcomes of 3-year-old children with hearing loss and different types of additional disabilities. J. Deaf Stud. Deaf Educ. 2014, 19, 20–39. [Google Scholar] [CrossRef] [Green Version]
- Netten, A.P.; Rieffe, C.; Theunissen, S.C.P.M.; Soede, W.; Dirks, E.; Korver, A.M.H.; Konings, S.; Oudesluys-Murphy, A.M.; Dekker, F.W.; Frijns, J.H.M. Early identification: Language skills and social functioning in deaf and hard of hearing preschool children. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 2221–2226. [Google Scholar] [CrossRef]
- DesJardin, J.L.; Eisenberg, L.S. Maternal contributions: Supporting language development in young children with cochlear implants. Ear Hear. 2007, 28, 456–469. [Google Scholar] [CrossRef]
- Zaidman-Zait, A.; Most, T.; Tarrasch, R.; Haddadeid, E.; Brand, D. The impact of childhood hearing loss on the family: Mothers’ and fathers’ stress and coping resources. DEAFED 2016, 21, 23–33. [Google Scholar] [CrossRef] [Green Version]
- Blank, A.; Frush Holt, R.; Pisoni, D.B.; Kronenberger, W.G. Associations between parenting stress, language comprehension, and inhibitory control in children with hearing loss. J. Speech Lang. Hear. Res. 2020, 63, 321–333. [Google Scholar] [CrossRef]
- Vohr, B.; Pierre, L.S.; Topol, D.; Jodoin-Krauzyk, J.; Bloome, J.; Tucker, R. Association of maternal communicative behavior with child vocabulary at 18–24 months for children with congenital hearing loss. Early Hum. Dev. 2010, 86, 255–260. [Google Scholar] [CrossRef]
- Yoshinaga-Itano, C.; Sedey, A.L.; Mason, C.A.; Wiggin, M.; Chung, W. Early intervention, parent talk, and pragmatic language in children with hearing loss. Pediatrics 2020, 146, S270–S277. [Google Scholar] [CrossRef] [PubMed]
- Yoshinaga-Itano, C. Benefits of early intervention for children with hearing loss. Otolaryngol. Clin. N. Am. 1999, 32, 1089–1102. [Google Scholar] [CrossRef]
- Wiggin, M.; Sedey, A.L.; Yoshinaga-Itano, C.; Mason, C.A.; Gaffney, M.; Chung, W. Frequency of early intervention sessions and vocabulary skills in children with hearing loss. J. Clin. Med. 2021, 10, 5025. [Google Scholar] [CrossRef] [PubMed]
- Moeller, M.P.; Carr, G.; Seaver, L.; Stredler-Brown, A.; Holzinger, D. Best practices in family-centered early intervention for children who are deaf or hard of hearing: An international consensus statement. J. Deaf Stud. Deaf Educ. 2013, 18, 429–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ching, T.Y.C.; Leigh, G.; Dillon, H. Introduction to the longitudinal outcomes of children with hearing impairment (LOCHI) study: Background, design, sample characteristics. Int. J. Audiol. 2013, 52 (Suppl. 2), S4–S9. [Google Scholar] [CrossRef] [PubMed]
- Moeller, M.P.; Tomblin, J.B. An introduction to the outcomes of children with hearing loss study. Ear Hear. 2015, 36 (Suppl. 1), 4S–13S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fink, N.E.; Wang, N.-Y.; Visaya, J.; Niparko, J.K.; Quittner, A.; Eisenberg, L.S.; Tobey, E.A. Childhood development after cochlear implantation (CDaCI) study: Design and baseline characteristics. Cochlear Implants Int. 2007, 8, 92–116. [Google Scholar] [CrossRef]
- Holzinger, D.; Binder, D.; Raus, D.; Palmisano, G.; Fellinger, J. Development and implementation of a low-cost tracking system after newborn hearing screening in upper Austria: Lessons learned from the perspective of an early intervention provider. Children 2021, 8, 743. [Google Scholar] [CrossRef]
- Statistik Austria. Natürliche Bevölkerungsbewegung, Eheschließungen, Ehescheidungen sowie Begründungen und Auflösungen eingetragener Partnerschaften 2020 nach Politischen Bezirken—Vorläufige Ergebnisse. Available online: https://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/bevoelkerung/geborene/index.html (accessed on 26 April 2021).
- Journal of Early Hearing Detection and Intervention. JCIH 2019. 2019. Available online: http://www.jcih.org/JCIH_2019_Executive_Summary.pdf (accessed on 18 March 2021).
- Thompson, W.K.; Hallmayer, J.; O’Hara, R. Design considerations for characterizing psychiatric trajectories across the lifespan: Application to effects of APOE-ε4 on cerebral cortical thickness in Alzheimer’s disease. Am. J. Psychiatry 2011, 168, 894–903. [Google Scholar] [CrossRef] [Green Version]
- Neumann, K.; Chadha, S.; Tavartkiladze, G.; Bu, X.; White, K. Newborn and infant hearing screening facing globally growing numbers of people suffering from disabling hearing loss. Int. J. Neonatal Screen. 2019, 5, 7. [Google Scholar] [CrossRef] [Green Version]
- Walker, E.A.; Spratford, M.; Moeller, M.P.; Oleson, J.; Ou, H.; Roush, P.; Jacobs, S. Predictors of hearing aid use time in children with mild-to-severe hearing loss. LSHSS 2013, 44, 73–88. [Google Scholar] [CrossRef] [Green Version]
- MED-EL. Little Ears Hör-Fragebogen. Elternfragebogen zur Erfassung auditiven Verhaltens; MED-EL: Innsbruck, Austria, 2003. [Google Scholar]
- Ching, T.Y.C.; Hill, M. The parents’ evaluation of aural/oral performance of children (PEACH) scale: Normative data. J. Am. Acad. Audiol. 2007, 18, 220–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biesalski, P.; Leitner, H.; Leitner, E.; Gangel, D. Der Mainzer Kindersprachtest. Sprachaudiometrie im Vorschulalter. HNO 1974, 22, 160–161. [Google Scholar] [PubMed]
- Chilla, R. Der Göttinger Kindersprachverständnistest I. HNO 1976, 24, 342–346. [Google Scholar]
- Hahlbrock, K.-H. Über Sprachaudiometrie und neue Wörterteste. Arch. Ohren- Nasen- Kehlkopfheilkd. 1953, 162, 394–431. [Google Scholar] [CrossRef]
- McLeod, S.; Harrison, L.J.; McCormack, J. Skala zur Verständlichkeit im Kontext [Intelligibility in Context Scale: Deutsch]: (S. Neumann, Trans.); Charles Sturt University: Bathurst, Australia, 2012. [Google Scholar]
- Wachtlin, B.; Brachmaier, J.; Amman, E.; Hoffmann, V.; Keilmann, A. Development and Evaluation of the LittlEARS® Early Speech Production Questionnaire—LEESPQ. Int. J. Pediatr. Otorhinolaryngol. 2017, 94, 23–29. [Google Scholar] [CrossRef]
- Marschick, P.; Vollmann, R.; Einspieler, C. ACDI (Austrian Communicative Development Inventory) Aufgaben und Gesten; Karl-Franzens-Universität Graz: Graz, Austria, 2004. [Google Scholar]
- Prizant, B.M. CSBS Developmental Profile Forms; Paul, H., Ed.; Brookes Publishing Company: Baltimore, MD, USA, 2002. [Google Scholar]
- Szagun, G.; Stumper, B.; Schramm, S.A. FRAKIS Fragebogen zur Frühkindlichen Sprachentwicklung, 2nd ed.; Pearson Deutschland GmbH: Frankfurt am Main, Germany, 2009. [Google Scholar]
- Grimm, H. SETK-2 Sprachentwicklungstest für Zweijährige Kinder, 2nd ed.; Hogrefe: Göttingen, Germany, 2016. [Google Scholar]
- Petermann, F. Sprachstandserhebungstest für Kinder im Alter zwischen 3 und 5 Jahren; Hogrefe: Göttingen, Germany, 2016. [Google Scholar]
- Dunn, L.; Dunn, D.M. Peabody Picture Vocabulary Test; Pearson: London, UK, 2015. [Google Scholar]
- Holzinger, D.; Diendorfer, B.; Beitel, C.; Heitz, R.; Bernegger, M.; Ebner, I.; Kraxberger, B. LOGiK-S Logopädie im Kindergarten—Screening: Handbuch; Land Oberösterreich and Konventhospital Barmherzige Brüder Linz: Linz, Austria, 2016. [Google Scholar]
- Zimmerman, I.; Steiner, V.; Pond, R.E. Preschool Language Scale, 5th ed.; Pearson: London, UK, 2011. [Google Scholar]
- Fox-Boyer, A.V. Test zur Überprüfung des Grammatikverständnisses; Schulz-Kirchner Verlag: Idstein, Germany, 2020. [Google Scholar]
- Schreiber, K.; Dobner, C.; Stalzer, B.; Stalzer, C.; Holzinger, D. Entwicklung praktikabler und zuverlässiger Verfahren zur Ermittlung des Sprachverstehens in der Österreichischen Gebärdensprache im Vorschulalter—Eine Pilotstudie. Hörgeschädigtenpädagogik 2020, 3, 147–156. [Google Scholar]
- O’Neill, D. LUI Manual Language Use Inventory: An Assessment of Young Children’s Pragmatic Language Development; Knowledge in Development: Waterloo, ON, Canada, 2009. [Google Scholar]
- Bishop, D.V. Development of the children’s communication checklist (CCC): A method for assessing qualitative aspects of communicative impairment in children. J. Child Psychol. Psychiatry 1998, 39, 879–891. [Google Scholar] [CrossRef]
- Thomas-Stonell, N.L.; Oddson, B.; Robertson, B.; Rosenbaum, P.L. Development of the FOCUS (Focus on the Outcomes of Communication Under Six), a communication outcome measure for preschool children. Dev. Med. Child Neurol. 2010, 52, 47–53. [Google Scholar] [CrossRef]
- Bayley, N. Bayley Scales of Infant and Toddler Development—Deutsche Fassung, 3rd ed.; Pearson Deutschland GmbH: Frankfurt am Main, Germany, 2015. [Google Scholar]
- Tellegen, P.J.; Laros, J.A.; Petermann, F. SON-R 2½-7 Non-Verbaler Intelligenztest; Hogrefe: Göttingen, Germany, 2007. [Google Scholar]
- Daseking, M.; Petermann, F. Verhaltensinventar zur Beurteilung exekutiver Funktionen für das Kindergartenalter: Deutschsprachige Adaptation des Behavior Rating Inventory of Executive Function®—Preschool Version (BRIEF®-P) von Gerard A. Gioia, Kimberly Andrews Espy und Peter K. Isquith; Huber: Atlanta, GA, USA, 2013. [Google Scholar]
- Sparrow, S.; Cicchetti, D.; Saulnier, C. Vineland Adaptive Behavior Scales—Third Edition: Deutsche Fassung in Zusammenarbeit mit A. von Gontard, C. Wagner, J. Hussong und H. Mattheus, 3rd ed.; Pearson Deutschland GmbH: Frankfurt am Main, Germany, 2021. [Google Scholar]
- Stone, M. KNOX’S CUBE Test Revised (KCT-R): A Manual for Clinical and Experimental Uses; Stoelting: Wood Dale, IL, USA, 2002. [Google Scholar]
- Mottier, G. Mottier-Test. Über Untersuchungen der Sprache lesegestörter Kinder. Folia Phoniatr. 1951, 3, 170–177. [Google Scholar] [CrossRef]
- Varni, J.W. PedsQL™ Infant Scales 1–12 Months. 1998. Available online: https://eprovide.mapi-trust.org/instruments/pediatric-quality-of-life-inventory-infant-scales (accessed on 20 June 2021).
- Varni, J.W. PedsQL™ Infant Scales 13–24 Months: Parent Report for Infants (Ages 13–24 Months). 1998. Available online: https://eprovide.mapi-trust.org/instruments/pediatric-quality-of-life-inventory-infant-scales (accessed on 20 June 2021).
- Varni, J.W. PedsQL™ Paediatric Quality of Life Inventory: Parent Report for Toddlers (Ages 2–4); 1998. Available online: https://eprovide.mapi-trust.org/instruments/pediatric-quality-of-life-inventory (accessed on 20 June 2021).
- Dazord, A.; Manificat, S. Evaluation of the child’s quality of life: Validation of a questionnaire and first results. Expans. Sci. Française 1997, 45, 106–114. (In French) [Google Scholar]
- Achenbach, T.M. Arbeitsgruppe deutsche child behavior checklist. In Child Behavior Checklist 1 ½–5 Deutsche Fassung: Elternfragebogen für Klein- und Vorschulkinder, 1st ed.; Hogrefe: Göttingen, Germany, 2000. [Google Scholar]
- Goodman, R. Fragebogen zu Stärken und Schwächen (SDQ-Deu). Abgerufen Am 2005, 1, 2019. [Google Scholar]
- Nachshen, J.S.; Woodford, L.; Minnes, P. The Family Stress and Coping Interview for families of individuals with developmental disabilities: A lifespan perspective on family adjustment. J. Intellect. Disabil. Res. 2003, 47, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Tröster, H. Eltern-Belastungs-Inventar: Deutsche Version des Parenting Stress Index (PSI) von R. R. Abidin; Hogrefe: Göttingen, Germany, 2010. [Google Scholar]
- Varni, J.W.; Sherman, S.A.; Burwinkle, T.M.; Dickinson, P.E.; Dixon, P. The PedsQL Family Impact Module: Preliminary reliability and validity. Health Qual. Life Outcomes 2004, 2, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ambrose, S.; Appenzeller, M.; DesJardin, J. Scale of Parental Involvement and Self-Efficacy—Revised; Boys Town National Research Hospital: Omaha, NE, USA, 2019. [Google Scholar]
- LENA. LENA—Building Brains Through Early Talk. Available online: https://www.lena.org/ (accessed on 22 February 2022).
- Sommer, A.; Mann, D. Qualität Elterlichen Interaktionsverhaltens. Erfassung von Interaktionen mit Hilfe der Eltern-Kind-Interaktions Einschätzskala im Nationalen Bildungspanel; NEPS Working Paper Number 56; Leibniz Institute for Educational Trajectories: Bamberg, Germany, 2015; Available online: https://www.neps-data.de/Portals/0/Working%20Papers/WP_LVI.pdf (accessed on 7 June 2021).
- Education Group. 7. OÖ Kinder-Medien-Studie. 2020. Available online: https://www.edugroup.at/innovation/forschung/kinder-medien-studie/detail/themenbloecke-der-7-ooe-kinder-medien-studie.html (accessed on 7 June 2021).
- Ceh, K.M.; Bervinchak, D.M.; Francis, H.W. Early literacy gains in children with cochlear implants. Otol. Neurotol. 2013, 34, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Curtin, M.; Dirks, E.; Cruice, M.; Herman, R.; Newman, L.; Rodgers, L.; Morgan, G. Assessing parent behaviours in parent-child interactions with deaf and hard of hearing infants aged 0–3 years: A systematic review. J. Clin. Med. 2021, 10, 3345. [Google Scholar] [CrossRef]
- Linberg, A.; Mann, D.; Attig, M.; Vogel, F.; Weinert, S.; Roßbach, H.-G. Quality of Parent-Child-Interactions—Assessment of Interac-tion with the Parent-Child-Interaction Rating System in the National Educational Panel Study at the Child’s Age of 7, 17 and 26 Months; NEPS Survey Paper No. 51; Leibniz-Institut für Bildungsverläufe, Nationales Bildungspanel: Bamberg, Germany, 2019. [Google Scholar]
- Vogel, F.; Freund, J.-D.; Weinert, S. Vergleichbarkeit von Interaktionsmaßen über verschiedene Vergleichbarkeit von Interaktionsmaßen über verschiedene Situationen bei Säuglingen: Ergebnisse des Projekts ViVA; Poster Presentation; Tagung der Fachgruppe Entwicklungspsychologie der Deutschen Gesellschaft für Psychologie: Frankfurt am Main, Germany, 2015. [Google Scholar]
- Gilkerson, J.; Richards, J.A.; Warren, S.F.; Oller, D.K.; Russo, R.; Vohr, B. Language experience in the second year of life and language outcomes in late childhood. Pediatrics 2018, 142, e20174276. [Google Scholar] [CrossRef] [Green Version]
- Gómez, E.; Strasser, K. Language and socioemotional development in early childhood: The role of conversational turns. Dev. Sci. 2021, 24, e13109. [Google Scholar] [CrossRef]
- Ambrose, S.E.; VanDam, M.; Moeller, M.P. Linguistic input, electronic media, and communication outcomes of toddlers with hearing loss. Ear Hear. 2014, 35, 139–147. [Google Scholar] [CrossRef] [Green Version]
- Fenson, L.; Marchman, V.; Thal, D.; Dale, P.; Reznick, J.S.; Bates, E. MacArthur-Bates Communicative Development Inventories, 2nd ed.; Brookes: Baltimore, MD, USA, 2007. [Google Scholar]
- Ireton, H. Child Development Inventory; Behavior Science Systems, Inc.: Minneapolis, MN, USA, 1992. [Google Scholar]
- Holzinger, D.; Dall, M.; Sanduvete-Chaves, S.; Saldaña, D.; Chacón-Moscoso, S.; Fellinger, J. The impact of family environment on language development of children with cochlear implants: A systematic review and meta-analysis. Ear Hear. 2020, 41, 1077–1091. [Google Scholar] [CrossRef]
- Dale, P.S.; Tosto, M.G.; Hayiou-Thomas, M.E.; Plomin, R. Why does parental language input style predict child language development? A twin study of gene-environment correlation. J. Commun. Disord. 2015, 57, 106–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ambrose, S.E.; Appenzeller, M.; Mai, A.; DesJardin, J.L. Beliefs and self-efficacy of parents of young children with hearing loss. J. Early Hear. Detect. Interv. 2020, 5, 73–85. [Google Scholar] [PubMed]
- EUROCAT Network. European Network of Population-Based Registries for the Epidemiological Surveillance of Congenital Anomalies. Available online: https://eu-rd-platform.jrc.ec.europa.eu/eurocat/eurocat-network/eurocat-network-overview_en (accessed on 28 December 2021).
- Vanderbilt University. REDCap—Research Electronic Data Capture. Available online: https://www.project-redcap.org/ (accessed on 28 September 2021).
- Grimm, K.J.; Ram, N.; Estabrook, N. Growth Modeling: Structural Equation and Multilevel Modeling Approaches; The Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- McArdle, J.J. Latent variable modeling of differences and changes with longitudinal data. Ann. Rev. Psychol. 2009, 60, 577–605. [Google Scholar] [CrossRef]
- Little, T.D. Longitudinal Structural Equation Modeling; The Guilford Press: New York, NY, USA, 2013; ISBN 9781462510238. [Google Scholar]
- Muthen, B.; Muthen, L.K. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism Clin. Exp. Res. 2000, 24, 882–891. [Google Scholar] [CrossRef]
- Roth, D.L.; MacKinnon, D.P. Mediation analysis with longitudinal data. In Longitudinal Data Analysis: A Practical Guide for Researchers in Aging, Health, and Social Sciences; Newsom, J.T., Jones, R.N., Hofer, S.M., Eds.; Routledge/Taylor & Francis Group: Oxforsshire, UK, 2012; pp. 181–216. [Google Scholar]
- McArdle, J.J.; Grimm, K.J.; Hamagami, F.; Bowles, R.P.; Meredith, W. Modeling life-span growth curves of cognition using longitudinal data with multiple samples and changing scales of measurement. Psychol. Methods 2009, 14, 126–149. [Google Scholar] [CrossRef] [Green Version]
- Enders, C.K. Applied Missing Data Analysis; The Guilford Press: New York, NY, USA, 2010. [Google Scholar]
| Age at Enrollment | Collection Wave | |||||
|---|---|---|---|---|---|---|
| 9 Months | 18 Months | 27 Months | 36 Months | 48 Months | 66 Months | |
| 9 Months | 40 (220) | 11 | ||||
| 18 Months | 9 | 4 | ||||
| 27 Months | 21 | 9 | ||||
| 36 Months | 28 | 4 | ||||
| 48 Months | 15 | |||||
| 66 Months | 14 | |||||
| Total at Each Age Level | 40 | 20 | 25 | 37 | 19 | 14 |
| N = 126 | ||
|---|---|---|
| Family Characteristics | ||
| Hearing status parent, DHH parent, n (%) | 15 (11.9) | |
| Maternal education, n (%) | ||
| Compulsory school, n (%) | 8 (6.3) | |
| Apprenticeship, n (%) | 14 (11.1) | |
| Technical school with diploma, n (%) | 14 (11.1) | |
| University, n (%) | 15 (11.9) | |
| Multilingual yes, n (%) | 39 (31) | |
| Family-Centred Early Intervention | ||
| Age at entry into early intervention, m (SD) | 12.63 (15.91) | |
| Age at entry into early intervention, median (range) | 5.50 (0–64) | |
| Child characteristics | ||
| Sex female, n (%) | 49 (38.9) | |
| Clinical classification | ||
| Syndromic, n (%) | 33 (26.2) | |
| Non-syndromic, n (%) | 73 (57.9) | |
| Genetic testing | ||
| Available, n (%) | 66 (52.4) | |
| Waiting for final report, n (%) | 22 (17.5) | |
| Confirmed etiologies | ||
| CMV, n (%) | 4 (3.2) | |
| Non-syndromic | ||
| Connexin, n (%) | 18 (14.3) | |
| Further non-syndromic | pending | |
| Non-syndromic mimics, n (%) | 3 (2.4) | |
| Syndromic etiologies | ||
| Trisomie 21, n (%) | 4 (3.2) | |
| Other (CHARGE syndrome, Cornelia-de-Lange syndrome, Goldenhar syndrome, micro deletion syndrome 6q12, syndromal tegmental cap dysplasia, Leopard syndrome, Waardenburg syndrome type 2A), n (%) | 8 (6.4) | |
| Uncertain after genetic testing, n (%) | 21 (16.7) | |
| Additional diagnoses, n (%) | 40 (31.7) | |
| Autism Spectrum Disorder, n (%) | 2 (1.6) | |
| Visual impairment, n (%) | 15 (11.9) | |
| Inborn errors of metabolism, n (%) | 1 (0.8) | |
| Cognitive development below average (≥1 SD below mean), n (%) | 15 (12.4) | |
| Global developmental delay (>2 SD below mean), n (%) | 15 (12.4) | |
| Hearing loss characteristics | ||
| Age at hearing loss diagnosis in months, mean (SD) | 8.94 (13.3) | |
| Age at hearing loss diagnosis in months, median (range) | 4 (0–64) | |
| Hearing loss laterality, n (%) | ||
| Bilateral | 101 (80.2) | |
| Unilateral | 25 (19.8) | |
| No Hearing loss right/left | 10 (7.9)/15 (11.9) | |
| Hearing Aid | ||
| Age of first fitting in months, mean (SD) | 12.03 (14.2) | |
| Age of first fitting in months, median (range) | 6.00 (1–73) | |
| Current use bilateral, n (%) | 81 (64.3) | |
| Current use unilateral, n (%) | 21 (16.7) | |
| Cochlear Implant | ||
| Bilateral, n (%) | 22 (17.5) | |
| Age of 1st implant in months, mean (SD) | 18.23 (7.75) | |
| Age of 1st implant in months, median (range) | 14.5 (10–37) | |
| Age of 2nd implant in months, mean (SD) | 18.23 (7.75) | |
| Age of 2nd implant in months, median (range) | 14.5 (10–37) | |
| Unilateral, n (%) | 4 (3.2) | |
| Age of implant in months, mean (SD) | 29 (15.8) | |
| Age of implant in months, median (range) | 26.5 (15–48) | |
| Concurrent hearing aid and cochlear implant use, n (%) | 3 (2.4) | |
| Type of Hearing loss, n (%) | ||
| Sensorineural | 102 (81) | |
| Auditory Neuropathy Spectrum disorder | 3 (2.4) | |
| Atresia | 11 (8.7) | |
| Permanent conductive | 1 (0.8) | |
| Other | 6 (4.8) | |
| Degree of hearing loss in the better ear (bilateral), n (%) | ||
| Mild (26–40 dB) | 7 (5.6) | |
| Moderate (41–70) | 49 (38.9) | |
| Severe (71–90) | 18 (14.3) | |
| Profound (>91) | 24 (19) | |
| Degree of hearing loss (unilateral), n (%) | ||
| Mild (26–40 dB) | 2 (8.0) | |
| Moderate (41–70) | 5 (20.0) | |
| Severe (71–90) | 7 (28.0) | |
| Profound (>91) | 4 (16.0) | |
| Unknown (Atresia) | 7 (28.0) |
| Baseline | 9 Months | 18 Months | 27 Months | 36 Months | 48 Months | 66 Months | |
|---|---|---|---|---|---|---|---|
| Parents at home | 6 min | 35 min | 75 min | 60 min | 70 min | 40 min | 75 min |
| Clinical assessment child | 85 min | 85 min | 85 min | 80 min | 105 min | 95 min | 120 min |
| Interview parents | 10 min | 30 min | 20 min | 20 min | 20 min | 5 min | 25 min |
| Months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Construct | C | F | Measure | Baseline | 9 | 18 | 27 | 36 | 48 | 66 |
| Hearing | ||||||||||
| Objective hearing threshold | x | ABR, ASSR | ● | |||||||
| Hearing threshold | x | PTA (0.5, 1, 2, 4 kHz) | ● | ● | ● | ● | ● | ● | ● | |
| Aided hearing threshold | x | PTA (0.5, 1, 2, 4 kHz) | ● | ● | ● | ● | ● | ● | ● | |
| Hearing aid/CI use | x | Walker [48] | ● | ● | ● | ● | ● | ● | ||
| Data logging | ● | ● | ● | ● | ● | ● | ||||
| Speech perception | ||||||||||
| Hearing performance | x | Little Ears [49] | ● | ● | ||||||
| PEACH [50] | ● | ● | ||||||||
| Audibility | x | Speech intelligibility index (SII) | ● | ● | ● | ● | ||||
| Sound identification | x | Ling-sounds | ● | ● | ● | |||||
| Word identification | x | Mainzer Kindersprachtest [51] | ● | ● | ||||||
| Göttinger Kindersprachtest [52] | ● | ● | ||||||||
| Freiburger Sprachverständnistest [53] | ● | |||||||||
| Speech production | ||||||||||
| Intelligibility | x | Intelligibility in Context Scale (ICS) [54] | ● | ● | ||||||
| Vocal Development | x | Little Ears Speech Production [55] | ● | ● | ||||||
| Language/Communication | ||||||||||
| Use of gestures | x | ACDI Early Gestures [56] | ● | |||||||
| Symbolic behavior | x | CSBS [57] | ● | ● | ||||||
| Vocabulary expressive | x | FRAKIS [58] | ● | ● | ||||||
| SETK-2 subtest word production [59] | ● | ● | ||||||||
| SET 3-5 picture naming [60] | ● | ● | ● | |||||||
| Vocabulary receptive | x | SETK-2 word comprehension [59] | ● | |||||||
| PPVT-4 [61] | ● | |||||||||
| Grammar expressive | x | Subject-Verb agreement and Verb 2nd-word order | ● | ● | ||||||
| LogikS Grammar expressive [62] | ● | ● | ||||||||
| Language receptive | x | PLS-5 [63] | ● | ● | ||||||
| SETK-2 sentence comprehension [59] | ● | ● | ||||||||
| TROG-D [64] | ● | ● | ● | |||||||
| RDLS sign language use [65] | ● | ● | ● | |||||||
| CDI for language other than German | ● | ● | ● | |||||||
| CDI for sign language [65] | ● | ● | ||||||||
| Social communication | x | LUI [66] | ● | ● | ● | |||||
| CCC-2 [67] | ● | |||||||||
| FOCUS [68] | ● | ● | ||||||||
| Cognition | ||||||||||
| Non-verbal development | x | Bayley [69] | ● | ● | ● | |||||
| SON-R 2 ½-7 [70] | ● | ● | ● | |||||||
| Executive functioning | x | BRIEF-preschool [71] | ● | ● | ||||||
| Adaptive skills | x | Vineland-3 [72] | ● | ● | ● | ● | ● | ● | ||
| Visual successive memory and attention | x | KNOX cube test [73] | ● | ● | ● | |||||
| Phonological working memory | x | Mottier test [74] | ● | ● | ● | |||||
| Psychosocial | ||||||||||
| Quality of life | x | PedsQL 1–12 months [75] | ● | |||||||
| PedsQL 13–24 months [76] | ● | |||||||||
| PedsQL 2–4 years [77] | ● | ● | ● | |||||||
| AUQUEI [78] | ● | |||||||||
| Emotional and behavioral problems | x | CBCL [79] | ● | ● | ||||||
| Mental health | x | SDQ [80] | ● | ● | ● | ● | ||||
| Coping | x | Family Stress and Coping Interview [81] | ● | ● | ||||||
| Medical | ||||||||||
| Genetics | x | |||||||||
| Motor skills | x | Neurological Status | ● | ● | ● | ● | ● | ● | ● | |
| Health status | x | Neurological Status | ● | ● | ● | ● | ● | ● | ● | |
| Intervention | ||||||||||
| Family | ||||||||||
| Socio-economic data | x | SES questionnaire | ● | ● | ||||||
| Parental stress | x | Parental Stress Index [82] | ● | ● | ||||||
| Family quality of life | x | PedsQL Family [83] | ● | ● | ● | |||||
| Family involvement and self-efficacy | x | SPISE-R [84] | ● | ● | ● | |||||
| Parent-child communication | x | LENA [85] | ● | ● | ● | |||||
| Parent-child interaction | x | EKIE [86] | ● | ● | ● | |||||
| Media use | x | Media use questionnaire [87] | ● | ● | ||||||
| Reading time | x | Dialogic book reading questionnaire [88] | ● | ● | ● | ● | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dall, M.; Kiblböck, S.; Müllegger, D.; Fellinger, J.; Hofer, J.; Kapplmüller, R.; Breitwieser, S.; Schossleitner, K.; Weber, C.; Zöhrer, R.; et al. Understanding the Impact of Child, Intervention, and Family Factors on Developmental Trajectories of Children with Hearing Loss at Preschool Age: Design of the AChild Study. J. Clin. Med. 2022, 11, 1508. https://doi.org/10.3390/jcm11061508
Dall M, Kiblböck S, Müllegger D, Fellinger J, Hofer J, Kapplmüller R, Breitwieser S, Schossleitner K, Weber C, Zöhrer R, et al. Understanding the Impact of Child, Intervention, and Family Factors on Developmental Trajectories of Children with Hearing Loss at Preschool Age: Design of the AChild Study. Journal of Clinical Medicine. 2022; 11(6):1508. https://doi.org/10.3390/jcm11061508
Chicago/Turabian StyleDall, Magdalena, Sandra Kiblböck, Daiva Müllegger, Johannes Fellinger, Johannes Hofer, Ruth Kapplmüller, Sandra Breitwieser, Katharina Schossleitner, Christoph Weber, Ruth Zöhrer, and et al. 2022. "Understanding the Impact of Child, Intervention, and Family Factors on Developmental Trajectories of Children with Hearing Loss at Preschool Age: Design of the AChild Study" Journal of Clinical Medicine 11, no. 6: 1508. https://doi.org/10.3390/jcm11061508
APA StyleDall, M., Kiblböck, S., Müllegger, D., Fellinger, J., Hofer, J., Kapplmüller, R., Breitwieser, S., Schossleitner, K., Weber, C., Zöhrer, R., & Holzinger, D. (2022). Understanding the Impact of Child, Intervention, and Family Factors on Developmental Trajectories of Children with Hearing Loss at Preschool Age: Design of the AChild Study. Journal of Clinical Medicine, 11(6), 1508. https://doi.org/10.3390/jcm11061508






