Cognitive and Adaptive Effects of Early Growth Hormone Treatment in Prader–Willi Syndrome Patients: A Cohort Study
Abstract
:1. Introduction
1.1. GH Treatment Effects
1.2. GH Treatment and Cognition in Childhood
1.3. GH Treatment and Cognition in Adults
2. Materials and Methods
2.1. Participants
2.2. Instruments: Cognitive Functioning and Adaptive Behavior
2.3. Statistical Analysis
3. Results
3.1. Descriptive Data
3.2. Cognition and Adaptive Behavior of the Total Simple
3.3. Comparison of Cognition and Adaptive Behavior in the Two Groups
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gabau, E.; Aguilera, C.; Baena, N.; Ruiz, A.; Guitart, M. Enfermedades por alteración de la impronta genética. Síndrome Prader-Willi y de Angelman. Pediatr. Integral. 2019, XXIII, 249–257. [Google Scholar]
- Rice, L.; Einfeld, S.L. Cognitive and behavioural aspects of Prader–Willi syndrome. Curr. Opin. Psychiatry 2015, 28, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Dimitropoulos, A.; Ferranti, A.; Lemler, M. Expressive and receptive language in Prader–Willi syndrome: Report on genetic subtype differences. J. Commun. Disord. 2013, 46, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Famelart, N.; Diene, G.; Çabal-Berthoumieu, S.; Glattard, M.; Molinas, C.; Guidetti, M.; Tauber, M. Equivocal expression of emotions in children with Prader-Willi syndrome: What are the consequences for emotional abilities and social adjustment? Orphanet J. Rare Dis. 2020, 15, 55. [Google Scholar] [CrossRef]
- Dykens, E.M.; Roof, E.; Hunt-Hawkins, H.; Daniell, C.; Jurgensmeyer, S. Profiles and trajectories of impaired social cognition in people with Prader-Willi syndrome. PLoS ONE 2019, 14, e0223162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whittington, J.; Holland, A. Cognition in people with Prader-Willi syndrome: Insights into genetic influences on cognitive and social development. Neurosci. Biobehav. Rev. 2017, 72, 153–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deal, C.L.; Rogol, A.D. Growth hormone treatments and cognitive functioning in children with Prader–Willi syndrome. Eur. J. Endocrinol. 2020, 182, C21–C25. [Google Scholar] [CrossRef]
- Martínez-Moreno, C.G.; Calderón-Vallejo, D.; Harvey, S.; Arámburo, C.; Quintanar, J.L. Growth Hormone (GH) and Gonadotropin-Releasing Hormone (GnRH) in the Central Nervous System: A Potential Neurological Combinatory Therapy? Int. J. Mol. Sci. 2018, 19, 375. [Google Scholar] [CrossRef] [Green Version]
- Böhm, B.; Ritzén, E.M.; Lindgren, A.C. Growth hormone treatment improves vitality and behavioural issues in children with Prader-Willi syndrome. Acta Paediatr. 2015, 104, 59–67. [Google Scholar] [CrossRef]
- Whitman, B.Y.; Myers, S.; Carrel, A.; Allen, D. The Behavioral Impact of Growth Hormone Treatment for Children and Adolescents with Prader-Willi Syndrome: A 2-Year, Controlled Study. Pediatrics 2002, 109, e35. [Google Scholar] [CrossRef] [Green Version]
- Bertella, L.; Mori, I.; Grugni, G.; Pignatti, R.; Ceriani, F.; Molinari, E.; Ceccarelli, A.; Sartorio, A.; Vettor, R.; Semenza, C. Quality of life and psychological well-being in GH-treated, adult PWS patients: A longitudinal study. J. Intellect. Disabil. Res. 2007, 51, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Gil, E.M.; Giménez-Palop, O.; Caixàs, A. Treatment with growth hormone in the prader-willi syndrome. Endocrinol. Diabetes Nutr. 2018, 65, 229–236. [Google Scholar] [CrossRef]
- Lo, S.T.; Siemensma, E.P.C.; Festen, D.A.M.; Collin, P.J.L.; Hokken-Koelega, A.C.S. Behavior in children with Prader–Willi syndrome before and during growth hormone treatment: A randomized controlled trial and 8-year longitudinal study. Eur. Child Adolesc. Psychiatry 2014, 24, 1091–1101. [Google Scholar] [CrossRef] [PubMed]
- Alfaro, D.L.P.; Lemoine, P.; Ehlinger, V.; Molinas, C.; Diene, G.; Valette, M.; Pinto, G.; Coupaye, M.; Poitou-Bernert, C.; Thuilleaux, D.; et al. Causes of death in Prader-Willi syndrome: Lessons from 11 years’ experience of a national reference center. Orphanet J. Rare Dis. 2019, 14, 238. [Google Scholar] [CrossRef] [Green Version]
- Siemensma, E.; Tummers-de Lind van Wijngaarden, R.; Festen, D.; Troeman, Z.; van Alfen-van der Velden, A.; Otten, B.; Rotteveel, J.; Odink, R.; Bindels-de Heus, G.; van Leeuwen, M.; et al. Beneficial Effects of Growth Hormone Treatment on Cognition in Children with Prader-Willi Syndrome: A Randomized Controlled Trial and Longitudinal Study. J. Clin. Endocrinol. Metab. 2012, 97, 2307–2314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donze, S.H.; Damen, L.; Mahabier, E.F.; Hokken-Koelega, A.C. Cognitive functioning in children with Prader–Willi syndrome during 8 years of growth hormone treatment. Eur. J. Endocrinol. 2020, 182, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Kuppens, R.J.; Mahabier, E.F.; Bakker, N.E.; Siemensma, E.P.C.; Donze, S.H.; Hokken-Koelega, A.C.S. Effect of cessation of GH treatment on cognition during transition phase in Prader-Willi syndrome: Results of a 2-year crossover GH trial. Orphanet J. Rare Dis. 2016, 11, 153. [Google Scholar] [CrossRef] [Green Version]
- Höybye, C.; Thoren, M.; Böhm, B. Cognitive, emotional, physical and social effects of growth hormone treatment in adults with Prader-Willi syndrome. J. Intellect. Disabil. Res. 2005, 49, 245–252. [Google Scholar] [CrossRef]
- Luo, Y.; Zheng, Z.; Yang, Y.; Bai, X.; Yang, H.; Zhu, H.; Pan, H.; Chen, S. Effects of growth hormone on cognitive, motor, and behavioral development in Prader-Willi syndrome children: A meta-analysis of randomized controlled trials. Endocrine 2021, 71, 321–330. [Google Scholar] [CrossRef]
- Corripio, R.; Tubau, C.; Calvo, L.; Brun, C.; Capdevila, N.; Larramona, H.; Gabau, E. Safety and effectiveness of growth hormone therapy in infants with Prader-Willi syndrome younger than 2 years: A prospective study. J. Pediatr. Endocrinol. Metab. 2019, 32, 879–884. [Google Scholar] [CrossRef]
- Copet, P.; Jauregi, J.; Laurier, V.; Ehlinger, V.; Arnaud, C.; Cobo, A.-M.; Molinas, C.; Tauber, M.; Thuilleaux, D. Cognitive profile in a large french cohort of adults with Prader-Willi syndrome: Differences between genotypes. J. Intellect. Disabil. Res. 2010, 54, 204–215. [Google Scholar] [CrossRef] [PubMed]
| KERRYPNX | n | % |
|---|---|---|
| Group 1 | 10 | 32.3% |
| Group 2 | 21 | 67.7% |
| Socioeconomic status | ||
| High | 1 | 3.2% |
| Upper-middle | 13 | 41.9% |
| Middle | 8 | 25.8% |
| Low-middle | 4 | 12.9% |
| Low | 5 | 16.1% |
| Group 1 | Group 2 | p-Value | |||
|---|---|---|---|---|---|
| Median | Lower and Limit Values | Median | Lower and Limit Values | ||
| Age | 6 | (5.17–8.63) | 18 | (17.06–25.89) | <0.001 * |
| Age of starting treatment with GH | 0.77 | (0.76–1.25) | 4.41 | (3.33–11.79) | <0.001 * |
| GH treatment duration | 5.90 | (4.76–8.15) | 12.33 | (9.96–14.82) | 0.001 * |
| Mean (sd) | Minimum and Maximum Values | |
|---|---|---|
| TIQ | 60 (12.30) | 40–81 |
| GAI | 66 (13.97) | 40–94 |
| VCI | 70.65 (15.02) | 45–98 |
| PS | 70 (9.71) | 55–85 |
| GAB | 64.32 (20.95) | 11–115 |
| Group 1 | Group 2 | p-Value | |||
|---|---|---|---|---|---|
| Median | Lower and Upper Limits 95% of Confidence | Median | Lower and Upper Limits 95% of Confidence | ||
| TIQ | 74 | (63.04–75.76) | 58 | (51.59–62.32) | p = 0.009 * |
| GAI | 77 | (67.50–80.10) | 62 | (56.91–70.52) | p = 0.043 * |
| CVI | 76.5 | (67.77–82.43) | 67 | (60.95–76.10) | p = 0.186 |
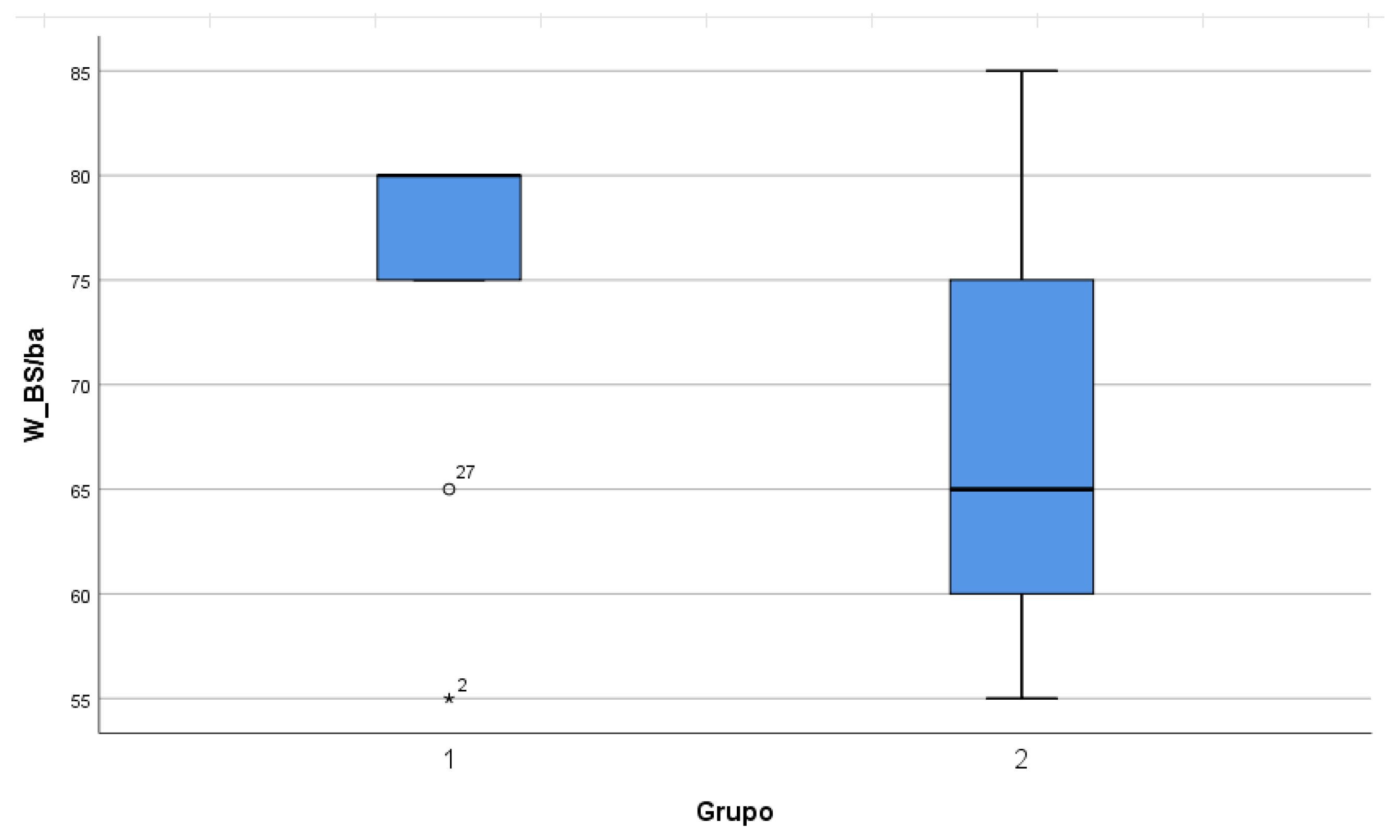
| PS | 80 | (68.07–81.93) | 65 | (63.13–72.13) | p = 0.068 |
| GAB | 87.5 | (70.49–97.11) | 53 | (48.25–61.84 | p < 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayet-Roger, A.; Joga-Elvira, L.; Caixàs, A.; Corripio, R. Cognitive and Adaptive Effects of Early Growth Hormone Treatment in Prader–Willi Syndrome Patients: A Cohort Study. J. Clin. Med. 2022, 11, 1592. https://doi.org/10.3390/jcm11061592
Ayet-Roger A, Joga-Elvira L, Caixàs A, Corripio R. Cognitive and Adaptive Effects of Early Growth Hormone Treatment in Prader–Willi Syndrome Patients: A Cohort Study. Journal of Clinical Medicine. 2022; 11(6):1592. https://doi.org/10.3390/jcm11061592
Chicago/Turabian StyleAyet-Roger, Aitana, Lorena Joga-Elvira, Assumpta Caixàs, and Raquel Corripio. 2022. "Cognitive and Adaptive Effects of Early Growth Hormone Treatment in Prader–Willi Syndrome Patients: A Cohort Study" Journal of Clinical Medicine 11, no. 6: 1592. https://doi.org/10.3390/jcm11061592
APA StyleAyet-Roger, A., Joga-Elvira, L., Caixàs, A., & Corripio, R. (2022). Cognitive and Adaptive Effects of Early Growth Hormone Treatment in Prader–Willi Syndrome Patients: A Cohort Study. Journal of Clinical Medicine, 11(6), 1592. https://doi.org/10.3390/jcm11061592






