Outcomes of Nonagenarians with Acute Myocardial Infarction with or without Coronary Intervention
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Definition and Study Endpoints
2.3. Statistical Analysis
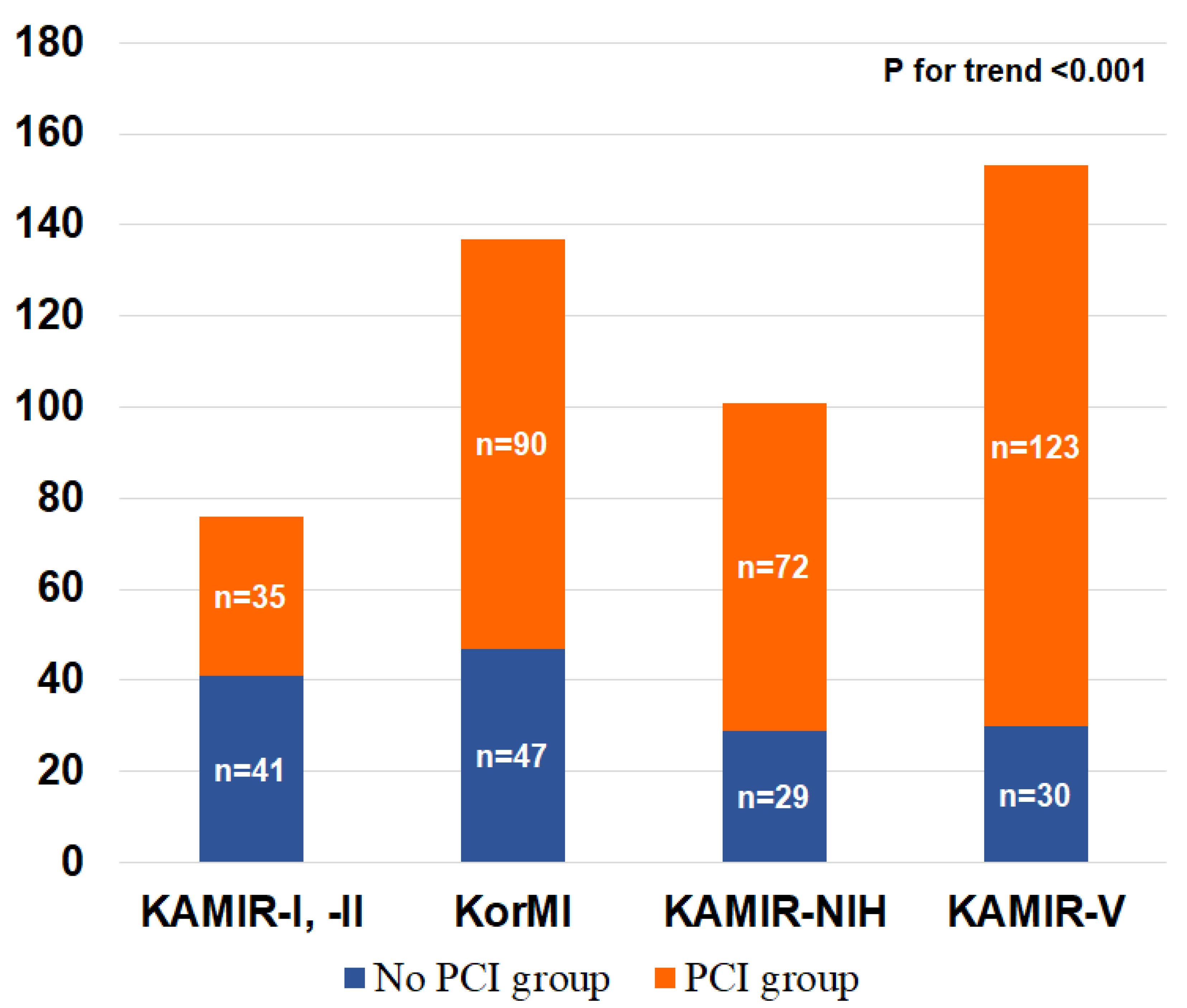
3. Results
4. Discussion
5. Conclusions
- Nonagenarian patients with AMI who underwent PCI appeared to have better clinical outcomes than those who were conservatively treated with no-PCI.
- Nonagenarian patients with AMI who underwent PCI also tended to receive more optimal medical therapy than those who were conservatively treated with no-PCI.
- Nonagenarian patients with AMI received high-quality PCI. Despite dangerous post-PCI clinical situations, in-hospital death was comparable in both groups.
- In routine practice, many clinicians are still reluctant to implement PCI in nonagenarian patients with AMI.
- Whether PCI is truly beneficial in nonagenarian AMI patients remains controversial, and further investigation is needed in the future.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; Elkind, M.S.V.; et al. Heart disease and stroke statistics-2021 update: A report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Jang, I.Y.; Lee, H.Y.; Lee, E. 50th Anniversary Committee of Korean Geriatrics Society. Geriatrics fact sheet in Korea 2018 from national statistics. Ann. Geriatr. Med. Res. 2019, 23, 50–53. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Ahn, Y.; Cho, M.C.; Kim, C.J.; Kim, Y.J.; Jeong, M.H. Current status of acute myocardial infarction in Korea. Korean J. Intern Med. 2019, 34, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.H.; Ahn, Y.; Kim, S.S.; Rhew, S.H.; Jeong, Y.W.; Jang, S.Y.; Cho, J.Y.; Jeong, H.C.; Park, K.H.; Yoon, N.S.; et al. Characteristics, in-hospital and long-term clinical outcomes of nonagenarian compared with octogenarian acute myocardial infarction patients. J. Korean Med. Sci. 2014, 29, 527–535. [Google Scholar] [CrossRef] [Green Version]
- Sung, J.; Hong, K.P. Descriptive study on the Korean status of percutaneous coronary intervention using National Health Insurance Service-National Sample Cohort (NHIS-NSC) database: Focused on temporal trend. Korean Circ. J. 2019, 49, 1155–1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, P.Y.; Alexander, K.P.; Hammill, B.G.; Pasquali, S.K.; Peterson, E.D. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA 2001, 286, 708–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silvain, J.; Cayla, G.; Hulot, J.-S.; Finzi, J.; Kerneis, M.; O’Connor, S.A.; Bellemain-Appaix, A.; Barthélémy, O.; Beygui, F.; Collet, J.-P.; et al. High on-thienopyridine platelet reactivity in elderly coronary patients: The Senior-Platelet study. Eur. Heart J. 2012, 33, 1241–1249. [Google Scholar] [CrossRef] [Green Version]
- Smith, L.G.; Herlitz, J.; Karlsson, T.; Berger, A.K.; Luepker, R.V. International comparison of treatment and long-term outcomes for acute myocardial infarction in the elderly: Minneapolis/St. Paul, MN, USA and Goteborg, Sweden. Eur. Heart J. 2013, 34, 3191–3197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Assali, A.R.; Moustapha, A.; Sdringola, S.; Salloum, J.; Awadalla, H.; Saikia, S.; Ghani, M.; Hale, S.; Schroth, G.; Rosales, O.; et al. The dilemma of success: Percutaneous coronary interventions in patients > or = 75 years of age-successful but associated with higher vascular complications and cardiac mortality. Catheter. Cardiovasc. Interv. 2003, 59, 195–199. [Google Scholar] [CrossRef]
- Galasso, G.; De Servi, S.; Savonitto, S.; Strisciuglio, T.; Piccolo, R.; Morici, N.; Murena, E.; Cavallini, C.; Petronio, A.S.; Piscione, F. Effect of an invasive strategy on outcome in patients ≥ 75 years of age with non-ST-elevation acute coronary syndrome. Am. J. Cardiol. 2015, 115, 576–680. [Google Scholar] [CrossRef]
- Hovanesyan, A.; Rich, M.W. Outcomes of acute myocardial infarction in nonagenarians. Am. J. Cardiol. 2008, 101, 1379–1383. [Google Scholar] [CrossRef] [PubMed]
- Batchelor, W.B.; Anstrom, K.J.; Muhlbaier, L.H.; Grosswald, R.; Weintraub, W.S.; O’Neill, W.W.; Peterson, E.D. Contemporary outcome trends in the elderly undergoing percutaneous coronary interventions: Results in 7472 octogenarians. National Cardiovascular Network Collaboration. J. Am. Coll. Cardiol. 2000, 36, 723–730. [Google Scholar] [CrossRef] [Green Version]
- Skolnick, A.H.; Alexander, K.P.; Chen, A.Y.; Roe, M.T.; Pollack, C.V., Jr.; Ohman, E.M.; Rumsfeld, J.S.; Gibler, W.B.; Peterson, E.D.; Cohen, D.J.; et al. Characteristics, management, and outcomes of 5557 patients age ≥ 90 years with acute coronary syndromes: Results from the CRUSADE Initiative. J. Am. Coll. Cardiol. 2007, 49, 1790–1797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barron, H.V.; Bowlby, L.J.; Breen, T.; Rogers, W.J.; Canto, J.G.; Zhang, Y.; Tiefenbrunn, A.J.; Weaver, W.D. Use of reperfusion therapy for acute myocardial infarction in the United States: Data from the National Registry of Myocardial Infarction 2. Circulation 1998, 97, 1150–1156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biondi-Zoccai, G.; Abbate, A.; D’Ascenzo, F.; Presutti, D.; Peruzzi, M.; Cavarretta, E.; Marullo, A.G.; Lotrionte, M.; Frati, G. Percutaneous coronary intervention in nonagenarians: Pros and cons. J. Geriatr. Cardiol. 2013, 10, 82–90. [Google Scholar]
- Helft, G.; Georges, J.-L.; Mouranche, X.; Loyeau, A.; Spaulding, C.; Caussin, C.; Benamer, H.; Garot, P.; Livarek, B.; Teiger, E.; et al. Outcomes of primary percutaneous coronary interventions in nonagenarians with acute myocardial infarction. Int. J. Cardiol. 2015, 192, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Zimmer, R.; Pessegueiro, A.; Jurewitz, D.; Tobis, J. Outcomes of nonagenarians who undergo percutaneous coronary intervention with drug-eluting stents. Catheter. Cardiovasc. Interv. 2008, 71, 526–530. [Google Scholar] [CrossRef]
- Moreno, R.; Salazar, A.; Bañuelos, C.; Hernández, R.; Alfonso, F.; Sabaté, M.; Escaned, J.; Pérez, M.J.; Azcona, L.; Macaya, C. Effectiveness of percutaneous coronary interventions in nonagenarians. Am. J. Cardiol. 2004, 94, 1058–1060. [Google Scholar] [CrossRef]
- Kang, S.H.; Suh, J.W.; Yoon, C.H.; Cho, M.C.; Kim, Y.J.; Chae, S.C.; Yoon, J.H.; Gwon, H.-C.; Han, K.-R.; Kim, J.H.; et al. Sex differences in management and mortality of patients with ST-elevation myocardial infarction (from the Korean Acute Myocardial Infarction National Registry). Am. J. Cardiol. 2012, 109, 787–793. [Google Scholar] [CrossRef]
- Kim, J.H.; Chae, S.C.; Oh, D.J.; Kim, H.-S.; Kim, Y.J.; Ahn, Y.; Cho, M.C.; Kim, C.J.; Yoon, J.-H.; Park, H.-Y.; et al. Multicenter cohort study of acute myocardial infarction in Korea-interim analysis of the Korea Acute Myocardial Infarction Registry-National Institutes of Health Registry. Circ. J. 2016, 80, 1427–1436. [Google Scholar] [CrossRef] [Green Version]
- Chen, K.-Y.; Rha, S.-W.; Li, Y.-J.; Poddar, K.; Jin, Z.; Minami, Y.; Wang, L.; Kim, E.J.; Park, C.G.; Seo, H.S.; et al. Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation 2009, 119, 3207–3214. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology (ESC); American College of Cardiology (ACC); et al. Fourth universal definition of myocardial infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Simoons, M.L.; Chaitman, B.R.; White, H.D.; Katus, H.A.; Apple, F.S.; Lindahl, B.; Morrow, D.A.; et al. Third universal definition of myocardial infarction. J. Am. Coll. Cardiol. 2012, 60, 1581–1598. [Google Scholar] [CrossRef] [Green Version]
- Thygesen, K.; Alpert, J.S.; White, H.D. Universal definition of myocardial infarction. Eur. Heart J. 2007, 28, 2525–2538. [Google Scholar] [PubMed]
- Avezum, A.; Makdisse, M.; Spencer, F.; Gore, J.M.; Fox, K.; Montalescot, G.; Eagle, K.A.; White, K.; Mehta, R.H.; Knobel, E.; et al. Impact of age on management and outcome of acute coronary syndrome: Observations from the Global Registry of Acute Coronary Events (GRACE). Am. Heart J. 2005, 149, 67–73. [Google Scholar] [CrossRef]
- Kontis, V.; Bennett, J.E.; Mathers, C.D.; Li, G.; Foreman, K.; Ezzati, M. Future life expectancy in 35 industrialised countries: Projections with a Bayesian model ensemble. Lancet 2017, 389, 1323–1335. [Google Scholar] [CrossRef] [Green Version]
- Numasawa, Y.; Inohara, T.; Ishii, H.; Yamaji, K.; Kohsaka, S.; Sawano, M.; Kodaira, M.; Uemura, S.; Kadota, K.; Amano, T.; et al. Comparison of outcomes after percutaneous coronary intervention in elderly patients, including 10,628 nonagenarians: Insights from a Japanese Nationwide Registry (J-PCI Registry). J. Am. Heart Assoc. 2019, 8, e011183. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.W.; Moon, J.S.; Kang, D.R.; Lee, S.J.; Son, J.-W.; Youn, Y.J.; Ahn, S.G.; Ahn, M.-S.; Kim, J.-Y.; Yoo, B.-S.; et al. Clinical impact of atypical chest pain and diabetes mellitus in patients with acute myocardial infarction from prospective KAMIR-NIH registry. J. Clin. Med. 2020, 9, 505. [Google Scholar] [CrossRef] [Green Version]
- Del Buono, M.G.; Montone, R.A.; Rinaldi, R.; Gurgoglione, F.L.; Meucci, M.C.; Camilli, M.; Iannaccone, G.; Sanna, T.; Pedicino, D.; Trani, C.; et al. Clinical predictors and prognostic role of high Killip class in patients with a first episode of anterior ST-segment elevation acute myocardial infarction. J. Cardiovasc. Med. 2021, 22, 530–538. [Google Scholar] [CrossRef]
- El-Menyar, A.; Zubaid, M.; AlMahmeed, W.; Sulaiman, K.; AlNabti, A.; Singh, R.; Al Suwaidi, J. Killip classification in patients with acute coronary syndrome: Insight from a multicenter registry. Am. J. Emerg. Med. 2012, 30, 97–103. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart. J. 2016, 37, 2315–2381. [Google Scholar]
- Stephens, J.W.; Khanolkar, M.P.; Bain, S.C. The biological relevance and measurement of plasma markers of oxidative stress in diabetes and cardiovascular disease. Atherosclerosis 2009, 202, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Antonsen, L.; Jensen, L.O.; Terkelsen, C.J.; Tilsted, H.-H.; Junker, A.; Maeng, M.; Hansen, K.N.; Lassen, J.F.; Thuesen, L.; Thayssen, P. Outcomes after primary percutaneous coronary intervention in octogenarians and nonagenarians with ST-segment elevation myocardial infarction: From the Western Denmark heart registry. Catheter. Cardiovasc. Interv. 2013, 81, 912–919. [Google Scholar] [CrossRef]
- Tokarek, T.; Dziewierz, A.; Plens, K.; Rakowski, T.; Zabojszcz, M.; Dudek, D.; Siudak, Z. Radial approach expertise and clinical outcomes of percutanous coronary interventions performed using femoral approach. J. Clin. Med. 2019, 8, 1484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siudak, Z.; Dziewierz, A.; Rakowski, T.; Żmudka, K.; Legutko, J.; Bartus, S.; Dragan, J.; Zasada, W.; Tokarek, T.; Kułaga, T.; et al. Borderline trend towards long-term mortality benefit from drug eluting stents implantation in ST-elevation myocardial infarction patients in Poland-data from NRDES registry. Catheter. Cardiovasc. Interv. 2014, 83, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Nishihira, K.; Watanabe, N.; Kuriyama, N.; Shibata, Y. Clinical outcomes of nonagenarians with acute myocardial infarction who undergo percutaneous coronary intervention. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 488–495. [Google Scholar] [CrossRef]
- Aubiniere-Robb, L.; Reid, G.; Murphy, A. Primary percutaneous coronary intervention in patients aged 85 years or older: A retrospective analysis of outcomes. J. R. Coll. Physicians Edinb. 2021, 51, 13–18. [Google Scholar] [CrossRef]
- Tokarek, T.; Siudak, Z.; Dziewierz, A.; Rakowski, T.; Krycińska, R.; Siwiec, A.; Dudek, D. Clinical outcomes in nonagenarians undergoing a percutaneous coronary intervention: Data from the ORPKI Polish National Registry 2014–2016. Coron. Artery Dis. 2018, 29, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Jeong, M.H.; Choi, Y.W.; Ahn, Y.K.; Chae, S.C.; Hur, S.H.; Hong, T.J.; Kim, Y.J.; Seong, I.W.; Chae, I.H.; et al. Temporal trends and in-hospital outcomes of primary percutaneous coronary intervention in nonagenarians with ST-segment elevation myocardial infarction. Korean J. Intern. Med. 2015, 30, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Seo, K.-W.; Park, J.-S.; Yang, H.-M.; Lim, H.-S.; Choi, B.-J.; Choi, S.-Y.; Yoon, M.-H.; Hwang, G.-S.; Tahk, S.-J.; et al. Managing nonagenarians with acute myocardial infarction: Invasive versus conservative treatment. Cardiol. Res. Pract. 2020, 2020, 8885518. [Google Scholar] [CrossRef] [PubMed]

| Before IPTW Adjustment | After IPTW Adjustment | |||||
|---|---|---|---|---|---|---|
| Characteristics | PCI Group | No-PCI Group | p-Value | PCI Group | No-PCI Group | p-Value |
| (n = 320) | (n = 147) | (n = 286) | (n = 265) | |||
| Male patients | 134 (41.9) | 48 (32.7) | 0.058 | 121 (42.5) | 108 (40.7) | 0.885 |
| Killip class III-IV | 69 (22.0) | 57 (42.5) | <0.001 | 74 (26.0) | 59 (22.2) | 0.645 |
| BMI ≥ 25 kg/m2 | 41 (15.4) | 22 (21.6) | 0.156 | 45 (15.7) | 33 (12.6) | 0.629 |
| Previous medical history | ||||||
| Hypertension | 208 (65.2) | 82 (56.6) | 0.074 | 189 (66.1) | 197 (74.3) | 0.376 |
| Diabetes mellitus | 49 (15.4) | 29 (19.9) | 0.233 | 49 (17.1) | 56 (21.3) | 0.677 |
| Dyslipidemia | 18 (5.6) | 8 (5.7) | 0.989 | 16 (5.7) | 7 (2.5) | 0.236 |
| Ischemic heart disease | 50 (15.6) | 22 (15.0) | 0.855 | 47 (16.3) | 54 (20.4) | 0.673 |
| Previous heart failure | 14 (4.4) | 14 (9.5) | 0.030 | 12 (4.2) | 12 (4.4) | 0.919 |
| Old CVA | 22 (6.9) | 14 (9.5) | 0.319 | 21 (7.5) | 12 (4.6) | 0.436 |
| Smoking history | 87 (28.2) | 40 (28.0) | 0.952 | 94 (32.9) | 122 (45.9) | 0.282 |
| Family CAD history | 11 (3.7) | 6 (4.9) | 0.569 | 23 (8.1) | 35 (13.2) | 0.589 |
| Prescribed medications | ||||||
| Aspirin | 285 (89.1) | 112 (76.2) | <0.001 | 270 (94.5) | 208 (78.6) | 0.065 |
| P2Y12 inhibitors | 285 (89.1) | 92 (62.6) | <0.001 | 271 (94.8) | 242 (91.4) | 0.339 |
| Beta-blockers | 191 (59.7) | 59 (40.1) | <0.001 | 180 (63.1) | 119 (44.8) | 0.132 |
| ACEIs/ARBs | 201 (62.8) | 65 (44.2) | <0.001 | 184 (64.3) | 114 (42.9) | 0.074 |
| Statins | 240 (75.0) | 73 (49.7) | <0.001 | 218 (76.2) | 162 (61.0) | 0.214 |
| LVEF < 40% | 72 (26.3) | 42 (37.8) | 0.024 | 98 (34.3) | 120 (45.2) | 0.373 |
| STEMI diagnosis | 202 (63.1) | 41 (27.9) | <0.001 | 141 (49.5) | 103 (39.0) | 0.413 |
| Before IPTW Adjustment | After IPTW Adjustment | |||||
|---|---|---|---|---|---|---|
| Characteristics | PCI Group | No-PCI Group | p-Value | PCI Group | No-PCI Group | p-Value |
| (n = 320) | (n = 147) | (n = 286) | (n = 265) | |||
| Cardiogenic shock or cardiac arrest | 48 (15.0) | 18 (12.2) | 0.427 | 32 (11.2) | 10 (3.6) | 0.026 |
| New-onset heart failure | 24 (7.5) | 14 (9.5) | 0.458 | 37 (13.0) | 57 (21.4) | 0.333 |
| Re-occurring MI | 2 (0.6) | 0 (0.0) | 1.000 | 0 (0.0) | 0 (0.0) | 1.000 |
| CVA | 4 (1.3) | 7 (4.8) | 0.042 | 3 (1.1) | 5 (1.8) | 0.539 |
| Atrioventricular block | 11 (3.4) | 3 (2.0) | 0.564 | 6 (2.1) | 0 (0.0) | 0.041 |
| Ventricular tachycardia or fibrillation | 12 (3.8) | 2 (1.4) | 0.243 | 9 (3.3) | 0 (0.0) | 0.023 |
| Atrial fibrillation | 16 (5.0) | 4 (2.7) | 0.330 | 17 (6.1) | 1 (0.5) | 0.003 |
| Acute kidney injury | 6 (1.9) | 6 (4.1) | 0.162 | 10 (3.6) | 4 (1.7) | 0.426 |
| Sepsis | 4 (1.3) | 1 (0.7) | 1.000 | 10 (3.6) | 1 (0.5) | 0.056 |
| Multi-organ failure | 6 (1.9) | 4 (2.7) | 0.515 | 8 (2.7) | 2 (0.9) | 0.254 |
| Temporary pacemaker | 34 (10.6) | 3 (2.0) | 0.001 | 22 (7.7) | 5 (2.0) | 0.059 |
| Cardiopulmonary resuscitation | 35 (10.9) | 10 (6.8) | 0.160 | 33 (11.5) | 8 (3.1) | 0.021 |
| Intra-aortic balloon pump | 15 (4.7) | 1 (0.7) | 0.027 | 11 (3.9) | 0 (0.0) | 0.018 |
| Defibrillation | 8 (2.5) | 0 (0.0) | 0.061 | 5 (1.8) | 0 (0.0) | 0.126 |
| In-hospital death | 50 (15.6) | 29 (19.7) | 0.272 | 28 (9.8) | 15 (5.7) | 0.308 |
| Before IPTW Adjustment | After IPTW Adjustment | |||||
|---|---|---|---|---|---|---|
| Characteristics | PCI Group | No-PCI Group | p-Value | PCI Group | No-PCI Group | p-Value |
| (n = 270) | (n = 118) | (n = 258) | (n = 250) | |||
| MACE | 45 (16.7) | 30 (25.4) | 0.044 | 54 (21.0) | 104 (41.4) | 0.082 |
| All-cause death | 41 (15.2) | 28 (23.7) | 0.043 | 50 (19.6) | 102 (40.8) | 0.068 |
| Cardiac death | 28 (10.4) | 19 (16.1) | 0.111 | 37 (14.4) | 59 (23.8) | 0.363 |
| Non-cardiac death | 13 (4.8) | 9 (7.6) | 0.270 | 13 (5.2) | 43 (17.0) | 0.054 |
| NFMI | 6 (2.2) | 1 (0.8) | 0.680 | 9 (3.6) | 2 (0.6) | 0.093 |
| Any revascularization | 6 (2.2) | 1 (0.8) | 0.680 | 6 (2.3) | 0 (0.0) | 0.036 |
| Univariable Logistic Analysis | Multivariable Logistic Analysis | ||||
|---|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | ||
| Male patients | 1.352 (0.814–2.245) | 0.244 | Male patients | ||
| Killip class III-IV | 1.592 (0.907–2.796) | 0.105 | Killip class III-IV | 1.592 (0.907–2.796) | 0.046 |
| BMI ≥ 25 kg/m2 | 0.868 (0.411–1.834) | 0.711 | BMI ≥ 25 kg/m2 | ||
| Previous medical history | Previous medical history | ||||
| Hypertension | 1.184 (0.699–2.007) | 0.530 | Hypertension | ||
| Diabetes mellitus | 2.050 (1.114–3.711) | 0.021 | Diabetes mellitus | 2.127 (1.045–4.331) | 0.037 |
| Dyslipidemia | 1.718 (0.643–4.590) | 0.281 | Dyslipidemia | ||
| Ischemic heart disease | 1.367 (0.706–2.648) | 0.354 | Ischemic heart disease | ||
| Previous heart failure | 0.872 (0.288–2.642) | 0.808 | Previous heart failure | ||
| Old CVA | 0.960 (0.380–2.423) | 0.931 | Old CVA | ||
| Smoking history | 0.881 (0.498–1.556) | 0.662 | Smoking history | ||
| Family CAD history | 1.213 (0.325–4.529) | 0.774 | Family CAD history | ||
| Prescribed medications | Prescribed medications | ||||
| Aspirin | 1.212 (0.402–3.656) | 0.733 | Aspirin | ||
| P2Y12 inhibitors | 1.542 (0.626–3.800) | 0.347 | P2Y12 inhibitors | ||
| Beta-blockers | 0.769 (0.460–1.287) | 0.318 | Beta-blockers | ||
| ACEIs/ARBs | 0.559 (0.333–0.939) | 0.028 | ACEIs/ARBs | ||
| Statins | 0.846 (0.466–1.535) | 0.582 | Statins | ||
| LVEF < 40% | 1.448 (0.828–2.534) | 0.195 | LVEF < 40% | ||
| STEMI diagnosis | 0.712 (0.428–1.183) | 0.190 | STEMI diagnosis | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, S.; Jeong, M.H.; Cho, K.H.; Kim, M.C.; Sim, D.S.; Hong, Y.J.; Kim, J.H.; Ahn, Y. Outcomes of Nonagenarians with Acute Myocardial Infarction with or without Coronary Intervention. J. Clin. Med. 2022, 11, 1593. https://doi.org/10.3390/jcm11061593
Oh S, Jeong MH, Cho KH, Kim MC, Sim DS, Hong YJ, Kim JH, Ahn Y. Outcomes of Nonagenarians with Acute Myocardial Infarction with or without Coronary Intervention. Journal of Clinical Medicine. 2022; 11(6):1593. https://doi.org/10.3390/jcm11061593
Chicago/Turabian StyleOh, Seok, Myung Ho Jeong, Kyung Hoon Cho, Min Chul Kim, Doo Sun Sim, Young Joon Hong, Ju Han Kim, and Youngkeun Ahn. 2022. "Outcomes of Nonagenarians with Acute Myocardial Infarction with or without Coronary Intervention" Journal of Clinical Medicine 11, no. 6: 1593. https://doi.org/10.3390/jcm11061593
APA StyleOh, S., Jeong, M. H., Cho, K. H., Kim, M. C., Sim, D. S., Hong, Y. J., Kim, J. H., & Ahn, Y. (2022). Outcomes of Nonagenarians with Acute Myocardial Infarction with or without Coronary Intervention. Journal of Clinical Medicine, 11(6), 1593. https://doi.org/10.3390/jcm11061593






