Metallic versus Non-Metallic Cerclage Cables System in Periprosthetic Hip Fracture Treatment: Single-Institution Experience at a Minimum 1-Year Follow-Up
Abstract
:1. Introduction
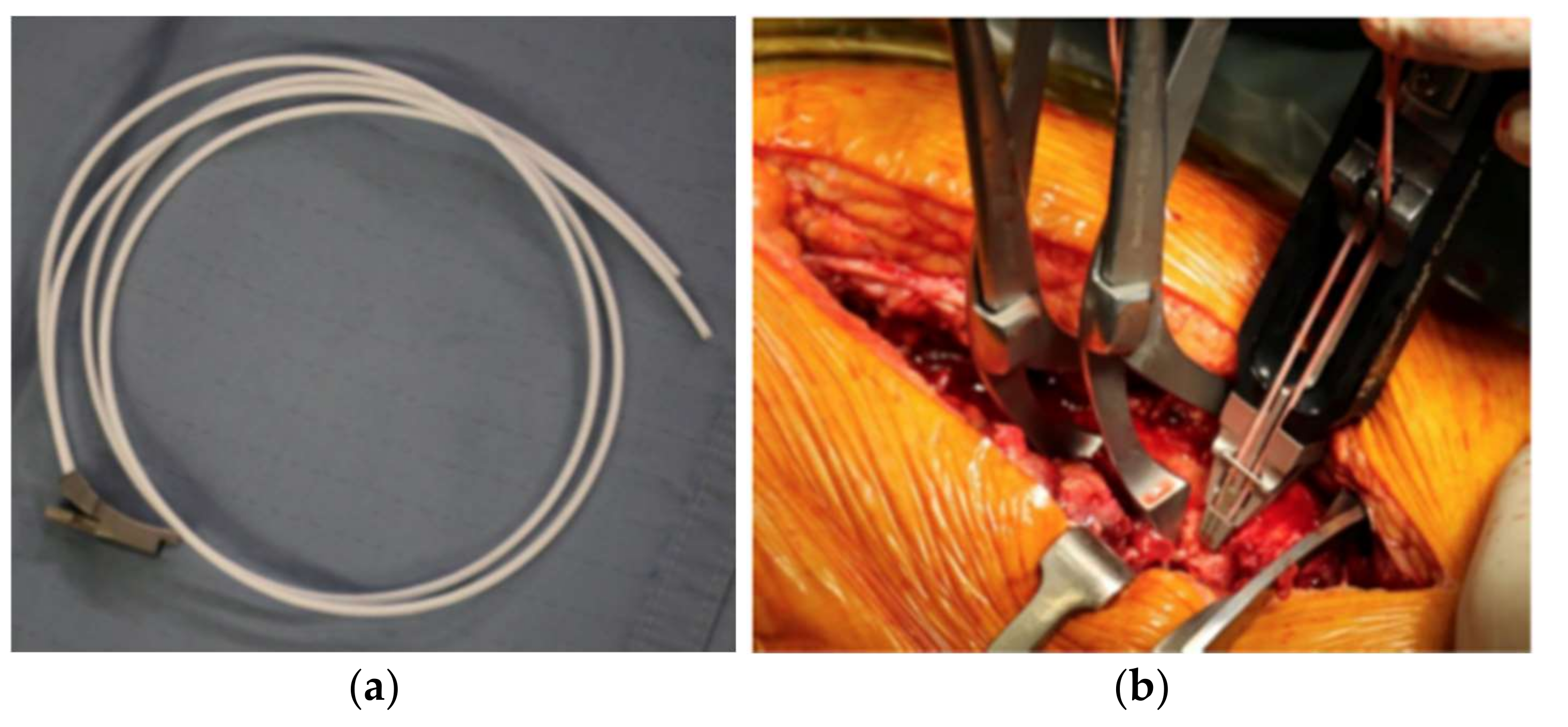
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2017 Revision, Key Findings and Advance Tables; ESA/P/WP/248; United Nations: New York, NY, USA, 2017. [Google Scholar]
- Hernlund, E.; Svedbom, A.; Ivergård, M.; Compston, J.; Cooper, C.; Stenmark, J.; McCloskey, E.V.; Jönsson, B.; Kanis, J.A. Osteoporosis in the European Union: Medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch. Osteoporos. 2013, 8, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurtz, S.; Mowat, F.; Ong, K.; Chan, N.; Lau, E.; Halpern, M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J. Bone Jt. Surg. Am. 2005, 87, 1487–1497. [Google Scholar] [CrossRef]
- Birrell, F.; Johnell, O.; Silman, A. Projecting the need for hip replacement over the next three decades: Influence of changing demography and threshold for surgery. Ann. Rheum. Dis. 1999, 58, 569–572. [Google Scholar] [CrossRef] [Green Version]
- Khan, T.; Grindlay, D.; Ollivere, B.J.; Scammell, B.E.; Manktelow, A.R.; Pearson, R.G. A systematic review of Vancouver B2 and B3 periprosthetic femoral fractures. Bone Jt. J. 2017, 99-B, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Lindahl, H.; Garellick, G.; Regnér, H.; Herberts, P.; Malchau, H. Three hundred and twenty-one periprosthetic femoral fractures. J. Bone Jt. Surg. Am. 2006, 88, 1215–1222. [Google Scholar] [CrossRef]
- Masri, B.A.; Meek, R.M.; Duncan, C.P. Periprosthetic fractures evaluation and treatment. Clin. Orthop. Relat. Res. 2004, 420, 80–95. [Google Scholar] [CrossRef] [PubMed]
- Quah, C.; Porteous, M.; Stephen, A. Principles of managing Vancouver type B periprosthetic fractures around cemented polished tapered femoral stems. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 477–482. [Google Scholar] [CrossRef]
- Stoffel, K.; Blauth, M.; Joeris, A.; Blumenthal, A.; Rometsch, E. Fracture fixation versus revision arthroplasty in Vancouver type B2 and B3 periprosthetic femoral fractures: A systematic review. Arch. Orthop. Trauma Surg. 2020, 140, 1381–1394. [Google Scholar] [CrossRef] [Green Version]
- Peeters, I.; Depover, A.; Van Tongel, A.; De Wilde, L. A review of metallic and non-metallic cerclage in orthopaedic surgery: Is there still a place for metallic cerclage? Injury 2019, 50, 1627–1633. [Google Scholar] [CrossRef]
- Silverton, C.D.; Jacobs, J.J.; Rosenberg, A.G.; Kull, L.; Conley, A.; Galante, J.O. Complications of a cable grip system. J. Arthroplast. 1996, 11, 400–404. [Google Scholar] [CrossRef]
- Fleischer, J.; Schleyer, A.; Nassutt, R.; Grittner, U.; Ojodu, I.; Hopp, S.J. Biomechanical strength and failure mechanism of different tubercula refixation methods within the framework of an arthroplasty for shoulder fracture. Orthop. Traumatol. Surg. Res. 2017, 103, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Nwankwo, C.D.; Parrish, R.; Leasure, J.; McGann, W.A. Prophylactic Cerclage With Braided Polyblend Suture During Femoral Broaching. Orthopedics 2016, 39, e1183–e1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renner, N.; Wieser, K.; Lajtai, G.; Morrey, M.E.; Meyer, D.C. Stainless steel wire versus FiberWire suture cerclage fixation to stabilize the humerus in total shoulder arthroplasty. J. Shoulder Elb. Surg. 2014, 23, 1568–1574. [Google Scholar] [CrossRef] [PubMed]
- Ting, N.T.; Wera, G.D.; Levine, B.R.; Della Valle, C.J. Early experience with a novel nonmetallic cable in reconstructive hip surgery. Clin. Orthop. Relat. Res. 2010, 468, 2382–2386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perren, S.M.; Fernandez Dell’Oca, A.; Lenz, M.; Windolf, M. Cerclage, evolution and potential of a Cinderella technology. An overview with reference to periprosthetic fractures. Acta Chir. Orthop. Traumatol. Cech. 2011, 78, 190–199. [Google Scholar] [PubMed]
- Rayan, F.; Haddad, F. Periprosthetic femoral fractures in total hip arthroplasty—A review. Hip Int. 2010, 20, 418–426. [Google Scholar] [CrossRef]
- Fleischman, A.N.; Chen, A.F. Periprosthetic fractures around the femoral stem: Overcoming challenges and avoiding pitfalls. Ann. Transl. Med. 2015, 3, 234. [Google Scholar] [CrossRef]
- Graham, S.M.; Moazen, M.; Leonidou, A.; Tsiridis, E. Locking plate fixation for Vancouver B1 periprosthetic femoral fractures: A critical analysis of 135 cases. J. Orthop. Sci. 2013, 18, 426–436. [Google Scholar] [CrossRef]
- Dennis, M.G.; Simon, J.A.; Kummer, F.J.; Koval, K.J.; DiCesare, P.E. Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: A biomechanical study of 5 techniques. J. Arthroplast. 2000, 15, 523–528. [Google Scholar] [CrossRef]
- Knierzinger, D.; Heinrichs, C.H.; Hengg, C.; Konschake, M.; Kralinger, F.; Schmoelz, W. Biomechanical evaluation of cable and suture cerclages for tuberosity reattachment in a 4-part proximal humeral fracture model treated with reverse shoulder arthroplasty. J. Shoulder Elb. Surg. 2018, 27, 1816–1823. [Google Scholar] [CrossRef]
- Camarda, L.; Morello, S.; Balistreri, F.; D’Arienzo, A.; D’Arienzo, M. Non-metallic implant for patellar fracture fixation: A systematic review. Injury 2016, 47, 1613–1617. [Google Scholar] [CrossRef] [PubMed]
- Jarit, G.J.; Sathappan, S.S.; Panchal, A.; Strauss, E.; Di Cesare, P.E. Fixation systems of greater trochanteric osteotomies: Biomechanical and clinical outcomes. J. Am. Acad. Orthop. Surg. 2007, 15, 614–624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altenburg, A.J.; Callaghan, J.J.; Yehyawi, T.M.; Pedersen, D.R.; Liu, S.S.; Leinen, J.A.; Dahl, K.A.; Goetz, D.D.; Brown, T.D.; Johnston, R.C. Cemented total hip replacement cable debris and acetabular construct durability. J. Bone Jt. Surg. Am. 2009, 91, 1664–1670. [Google Scholar] [CrossRef]
- Bauer, T.W.; Ming, J.; D’Antonio, J.A.; Morawa, L.G. Abrasive threebody wear of polyethylene caused by broken multifilament cables of a total hip prosthesis: A report of these cases. J. Bone Jt. Surg. Am. 1996, 78, 1244–1247. [Google Scholar] [CrossRef]
- Sarin, V.K.; Mattchen, T.M.; Pratt, W.R.; Hack, B. Novel isoelastic cerclage cable for fracture. Orthop. Proc. 2008, 90B (Suppl. 1), 189. [Google Scholar]
- Clarke, R.P.; Shea, W.D.; Bierbaum, B.E. Trochanteric osteotomy. Analysis of pattern of wire fixation failure and complications. Clin. Orthop. Relat. Res. 1979, 141, 102–110. [Google Scholar]
- Chen, W.M.; McAuley, J.P.; Engh, C.A., Jr.; Hopper, R.H., Jr.; Engh, C.A. Extended slide trochanteric osteotomy for revision total hip arthroplasty. J. Bone Jt. Surg. Am. 2000, 82, 1215–1219. [Google Scholar] [CrossRef]
- Ritter, M.A.; Eizember, L.E.; Keating, E.M.; Faris, P.M. Trochanteric fixation by cable grip in hip replacement. J. Bone Jt. Surg. Br. 1991, 73, 580–581. [Google Scholar] [CrossRef] [Green Version]
- Steinberg, E.L.; Shavit, R. Braided cerclage wires: A biomechanical study. Injury 2011, 42, 347–351. [Google Scholar] [CrossRef]
- Phadnis, J.; Watts, A.C. Tension band suture fixation for olecranon fractures. Shoulder Elb. 2017, 9, 299–303. [Google Scholar] [CrossRef]
- Huang, S.L.; Xue, J.L.; Gao, Z.Q.; Lan, B.S. Management of patellar fracture with titanium cable cerclage. Medicine 2017, 96, e8525. [Google Scholar] [CrossRef] [PubMed]

| Group A (n = 32) | Group B (n = 30) | |
|---|---|---|
| Age (years) | 75.1 ± 8.1 | 77.3 ± 4.1 |
| Sex (M; F) | 13; 19 | 9; 21 |
| BMI (body mass index) | 25.3 ± 4.2 | 26.1 ± 3.7 |
| Fracture | ||
| 22 | 21 |
| 10 | 9 |
| Follow-up (months) | 16.1 ± 3.2 | 14.8 ± 2.9 |
| Type | Subtype | Fracture Description |
|---|---|---|
| A | Fracture in trochanteric region | |
| AG | Fractures of the greater trochanter | |
| AL | Fractures of the lesser trochanter | |
| B | Fracture around stem or just below it | |
| B1 | Well-fixed stem | |
| B2 | Loose stem with good proximal bone stock | |
| B3 | Loose stem with poor-quality bone stock | |
| C | Fracture occurring well below the tip of the stem |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Speranza, A.; Massafra, C.; Pecchia, S.; Di Niccolo, R.; Iorio, R.; Ferretti, A. Metallic versus Non-Metallic Cerclage Cables System in Periprosthetic Hip Fracture Treatment: Single-Institution Experience at a Minimum 1-Year Follow-Up. J. Clin. Med. 2022, 11, 1608. https://doi.org/10.3390/jcm11061608
Speranza A, Massafra C, Pecchia S, Di Niccolo R, Iorio R, Ferretti A. Metallic versus Non-Metallic Cerclage Cables System in Periprosthetic Hip Fracture Treatment: Single-Institution Experience at a Minimum 1-Year Follow-Up. Journal of Clinical Medicine. 2022; 11(6):1608. https://doi.org/10.3390/jcm11061608
Chicago/Turabian StyleSperanza, Attilio, Carlo Massafra, Stefano Pecchia, Riccardo Di Niccolo, Raffaele Iorio, and Andrea Ferretti. 2022. "Metallic versus Non-Metallic Cerclage Cables System in Periprosthetic Hip Fracture Treatment: Single-Institution Experience at a Minimum 1-Year Follow-Up" Journal of Clinical Medicine 11, no. 6: 1608. https://doi.org/10.3390/jcm11061608






