A New Grading System for Migrated Lumbar Disc Herniation on Sagittal Magnetic Resonance Imaging: An Agreement Study
Abstract
:1. Introduction
2. Materials and Methods
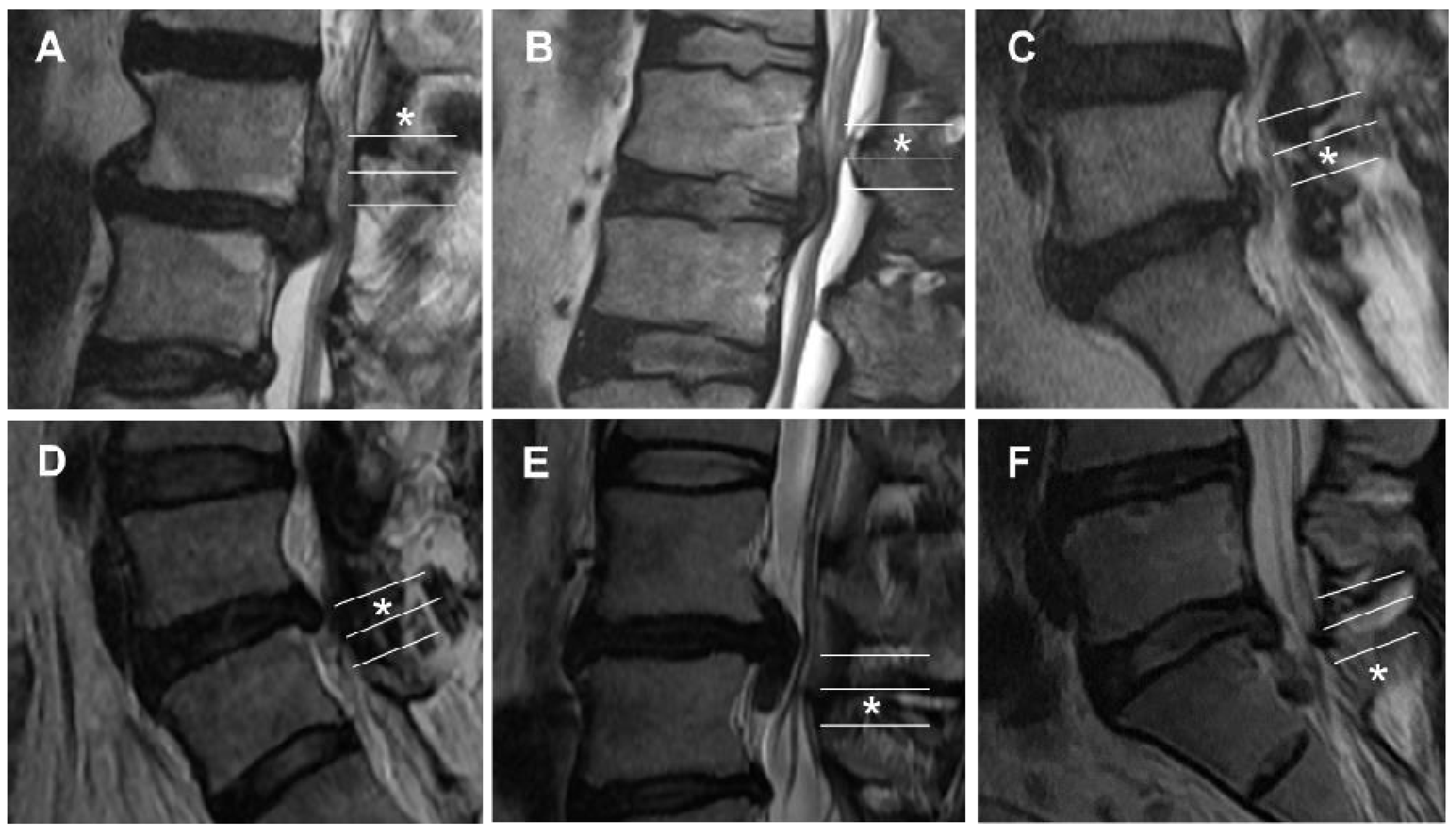
2.1. New Magnetic Resonance Imaging Grading System for Migrated Lumbar Disc Herniation
2.2. Study Population
2.3. Image Measurement and Analysis
2.4. Statistical Analysis
3. Results
3.1. Demographics
3.2. Distribution
3.3. Interobserver and Intraobserver Agreements
3.4. Inter-Grading System Agreement
4. Discussion
4.1. Comparison of the Grading Systems
4.2. Distribution
4.3. Clinical Usefulness of the Grading System of Migrated Lumbar Disc Herniation
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Apostolides, P.J.; Jacobowitz, R.; Sonntag, V.K. Lumbar discectomy microdiscectomy: “The gold standard”. Clin. Neurosurg. 1996, 43, 228–238. [Google Scholar]
- Li, X.; Hu, Z.; Cui, J.; Han, Y.; Pan, J.; Yang, M.; Tan, J.; Sun, G.; Li, L. Percutaneous endoscopic lumbar discectomy for recurrent lumbar disc herniation. Int. J. Surg. 2016, 27, 8–16. [Google Scholar] [CrossRef]
- Ruan, W.; Feng, F.; Liu, Z.; Xie, J.; Cai, L.; Ping, A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: A meta-analysis. Int. J. Surg. 2016, 31, 86–92. [Google Scholar] [CrossRef]
- Qin, R.; Liu, B.; Hao, J.; Zhou, P.; Yao, Y.; Zhang, F.; Chen, X. Percutaneous Endoscopic Lumbar Discectomy Versus Posterior Open Lumbar Microdiscectomy for the Treatment of Symptomatic Lumbar Disc Herniation: A Systemic Review and Meta-Analysis. World Neurosurg. 2018, 120, 352–362. [Google Scholar] [CrossRef]
- Shi, R.; Wang, F.; Hong, X.; Wang, Y.T.; Bao, J.P.; Liu, L.; Wang, X.H.; Xie, Z.Y.; Wu, X.T. Comparison of percutaneous endoscopic lumbar discectomy versus microendoscopic discectomy for the treatment of lumbar disc herniation: A meta-analysis. Int. Orthop. 2019, 43, 923–937. [Google Scholar] [CrossRef]
- Fardon, D.F.; Milette, P.C. Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine 2001, 26, E93–E113. [Google Scholar] [PubMed]
- Schellinger, D.; Manz, H.J.; Vidic, B.; Patronas, N.J.; Deveikis, J.P.; Muraki, A.S.; Abdullah, D.C. Disk fragment migration. Radiology 1990, 175, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Saruhashi, Y.; Omura, K.; Miyamoto, K.; Katsuura, A.; Hukuda, S. A migrated lumbar disc herniation simulating a dumbbell tumor. J. Spinal Disord. 1999, 12, 307–309. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Kang, B.U.; Ahn, Y.; Choi, G.; Choi, Y.G.; Ahn, K.U.; Shin, S.W.; Kang, H.Y. Operative failure of percutaneous endoscopic lumbar discectomy: A radiologic analysis of 55 cases. Spine 2006, 31, E285–E290. [Google Scholar] [CrossRef]
- Lee, S.; Kim, S.K.; Lee, S.H.; Kim, W.J.; Choi, W.C.; Choi, G.; Shin, S.W. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: Classification of disc migration and surgical approaches. Eur. Spine J. 2007, 16, 431–437. [Google Scholar] [CrossRef] [Green Version]
- Mobbs, R.J.; Steel, T.R. Migration of lumbar disc herniation: An unusual case. J. Clin. Neurosci. 2007, 14, 581–584. [Google Scholar] [CrossRef] [PubMed]
- Brayda-Bruno, M.; Cinnella, P. Posterior endoscopic discectomy (and other procedures). Eur. Spine J. 2000, 9 (Suppl. S1), S24–S29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeung, A.T.; Tsou, P.M. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine 2002, 27, 722–731. [Google Scholar] [CrossRef]
- Ahn, Y. Transforaminal percutaneous endoscopic lumbar discectomy: Technical tips to prevent complications. Expert. Rev. Med. Devices 2012, 9, 361–366. [Google Scholar] [CrossRef]
- Choi, G.; Lee, S.H.; Lokhande, P.; Kong, B.J.; Shim, C.S.; Jung, B.; Kim, J.S. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine 2008, 33, E508–E515. [Google Scholar] [CrossRef]
- Choi, G.; Prada, N.; Modi, H.N.; Vasavada, N.B.; Kim, J.S.; Lee, S.H. Percutaneous endoscopic lumbar herniectomy for high-grade down-migrated L4-L5 disc through an L5-S1 interlaminar approach: A technical note. Minim. Invasive Neurosurg. 2010, 53, 147–152. [Google Scholar] [CrossRef] [Green Version]
- Kim, C.H.; Chung, C.K.; Woo, J.W. Surgical Outcome of Percutaneous Endoscopic Interlaminar Lumbar Discectomy for Highly Migrated Disk Herniation. Clin. Spine Surg. 2016, 29, E259–E266. [Google Scholar] [CrossRef]
- Ahn, Y.; Jang, I.T.; Kim, W.K. Transforaminal percutaneous endoscopic lumbar discectomy for very high-grade migrated disc herniation. Clin. Neurol. Neurosurg. 2016, 147, 11–17. [Google Scholar] [CrossRef] [Green Version]
- Ahn, Y.; Jeong, T.S.; Lim, T.; Jeon, J.Y. Grading system for migrated lumbar disc herniation on sagittal magnetic resonance imaging: An agreement study. Neuroradiology 2018, 60, 101–107. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Daghighi, M.H.; Pouriesa, M.; Maleki, M.; Fouladi, D.F.; Pezeshki, M.Z.; Mazaheri Khameneh, R.; Bazzazi, A.M. Migration patterns of herniated disc fragments: A study on 1,020 patients with extruded lumbar disc herniation. Spine J. 2014, 14, 1970–1977. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, T.; Hirabayashi, Y.; Shimizu, R.; Saitoh, K.; Fukuda, H.; Mitsuhata, H. The lumbar extradural structure changes with increasing age. Br. J. Anaesth. 1997, 78, 149–152. [Google Scholar] [CrossRef] [PubMed]



| Grade | Direction and Degree | Range of Migration Distance |
|---|---|---|
| 1 | Superior very high | Beyond the inferior margin of the upper pedicle |
| 2 | Superior high | From the inferior margin of the upper pedicle to the midpoint between the inferior margin of the upper pedicle and superior disc margin |
| 3 | Superior low | From the midpoint between the inferior margin of the upper pedicle and superior disc margin to the superior disc margin |
| 4 | Inferior low | From the inferior disc margin to the midpoint between the inferior margin of the lower pedicle and inferior disc margin |
| 5 | Inferior high | From the midpoint between the inferior margin of the lower pedicle and inferior disc margin to the inferior margin of the lower pedicle |
| 6 | Inferior very high | Beyond the inferior margin of the lower pedicle |
| Characteristic | No. |
|---|---|
| Patients | 101 |
| Sex | |
| Female | 43 (42.57%) |
| Male | 58 (57.43%) |
| Age (years) | 45.91 ± 14.64 |
| Age group (years) | |
| ≤29 | 9 (8.91%) |
| 30–39 | 26 (25.74%) |
| 40–49 | 25 (24.75%) |
| 50–59 | 24 (23.76%) |
| 60–69 | 9 (8.91%) |
| ≥70 | 8 (7.92%) |
| Level of migrated LDH | |
| L1–L2 | 1 (0.99%) |
| L2–L3 | 3 (2.97%) |
| L3–L4 | 17 (16.83%) |
| L4–L5 | 51 (50.50%) |
| L5–S1 | 29 (28.71%) |
| Direction of disc migration | |
| Upward (superior) | 47 (46.53%) |
| Downward (inferior) | 54 (53.47%) |
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 | Grade 6 | Total | |
|---|---|---|---|---|---|---|---|
| Reader 1 (first) | 17 | 13 | 17 | 27 | 16 | 11 | 101 |
| Reader 1 (second) | 18 | 16 | 13 | 28 | 19 | 7 | 101 |
| Reader 2 (first) | 14 | 14 | 18 | 26 | 23 | 6 | 101 |
| Reader 2 (second) | 17 | 17 | 13 | 24 | 24 | 6 | 101 |
| Total | 66 | 60 | 61 | 105 | 82 | 30 | 404 |
| % | 16.34 | 14.85 | 15.10 | 25.99 | 20.30 | 7.43 |
| Observer | Grading System | k (95% CI) | Agreement |
|---|---|---|---|
| Reader 1 vs. 2 (first) | New | 0.753 (0.658–0.848) | Substantial |
| Lee–Kim | 0.714 (0.614–0.814) | Substantial | |
| Reader 1 vs. 2 (second) | New | 0.756 (0.660–0.852) | Substantial |
| Lee–Kim | 0.742 (0.645–0.840) | Substantial |
| Observer | Grading System | k (95% CI) | Agreement |
|---|---|---|---|
| Reader 1 | New | 0.733 (0.636–0.831) | Substantial |
| Lee–Kim | 0.729 (0.630–0.828) | Substantial | |
| Reader 2 | New | 0.829 (0.747–0.912) | Almost perfect |
| Lee–Kim | 0.668 (0.564–0.773) | Substantial |
| Observer | Grading System | k (95% CI) | Agreement |
|---|---|---|---|
| Reader 1 | New vs. Lee–Kim (first) | 0.878 (0.807–0.950) | Almost perfect |
| New vs. Lee–Kim (second) | 0.779 (0.686–0.872) | Substantial | |
| Reader 2 | New vs. Lee–Kim (first) | 0.828 (0.744–0.911) | Almost perfect |
| New vs. Lee–Kim (second) | 0.841(0.760–0.921) | Almost perfect |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahn, Y.; Kim, J.-E.; Yoo, B.-R.; Jeong, Y.-M. A New Grading System for Migrated Lumbar Disc Herniation on Sagittal Magnetic Resonance Imaging: An Agreement Study. J. Clin. Med. 2022, 11, 1750. https://doi.org/10.3390/jcm11071750
Ahn Y, Kim J-E, Yoo B-R, Jeong Y-M. A New Grading System for Migrated Lumbar Disc Herniation on Sagittal Magnetic Resonance Imaging: An Agreement Study. Journal of Clinical Medicine. 2022; 11(7):1750. https://doi.org/10.3390/jcm11071750
Chicago/Turabian StyleAhn, Yong, Ji-Eun Kim, Byung-Rhae Yoo, and Yu-Mi Jeong. 2022. "A New Grading System for Migrated Lumbar Disc Herniation on Sagittal Magnetic Resonance Imaging: An Agreement Study" Journal of Clinical Medicine 11, no. 7: 1750. https://doi.org/10.3390/jcm11071750
APA StyleAhn, Y., Kim, J.-E., Yoo, B.-R., & Jeong, Y.-M. (2022). A New Grading System for Migrated Lumbar Disc Herniation on Sagittal Magnetic Resonance Imaging: An Agreement Study. Journal of Clinical Medicine, 11(7), 1750. https://doi.org/10.3390/jcm11071750






