Determinants of Quality of Life in Adult Patients with Chronic Non-Bacterial Osteomyelitis (CNO) of the Sternocostoclavicular Region (SCCH): A Dutch Single Center Study
Abstract
:1. Introduction
2. Material and Methods
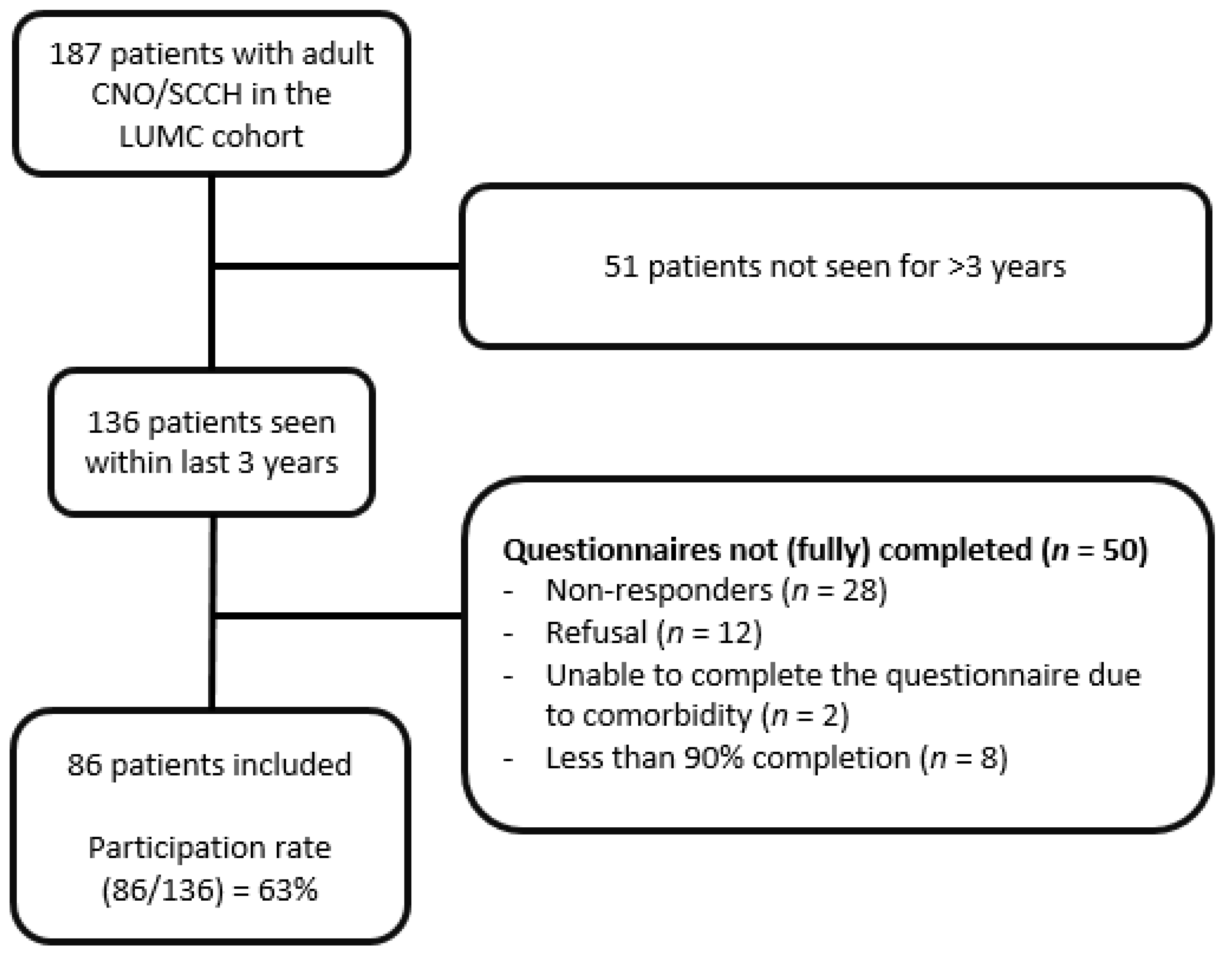
2.1. Material
2.2. Methods
3. Questionnaires
3.1. Quality of Life
3.2. Illness Perceptions
3.3. Coping Strategies
3.4. Shoulder Function
3.5. Reference Groups
3.6. Statistical Analysis
4. Results
4.1. Patients Characteristics
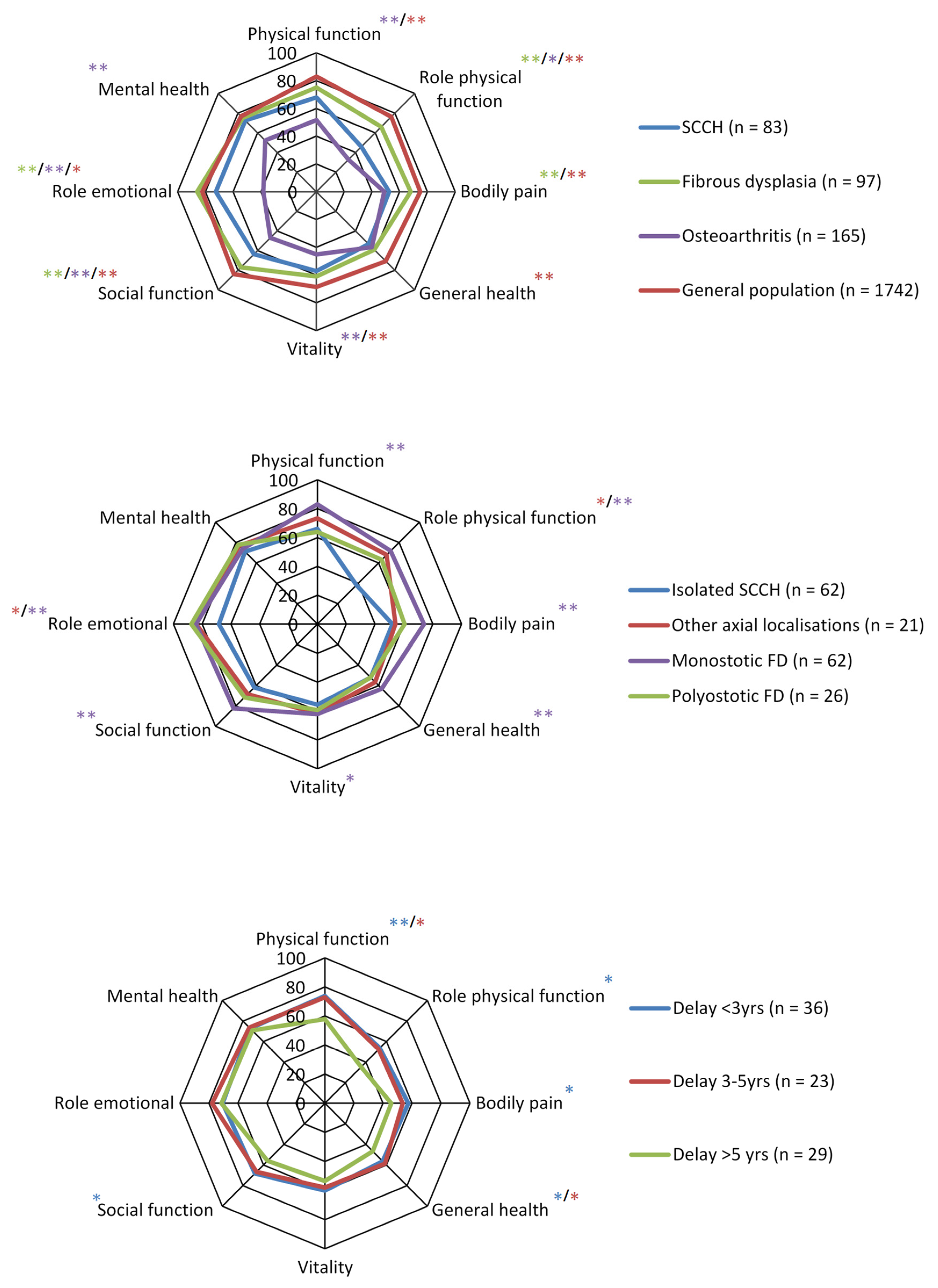
4.2. Outcomes and Determinants of Quality of Life
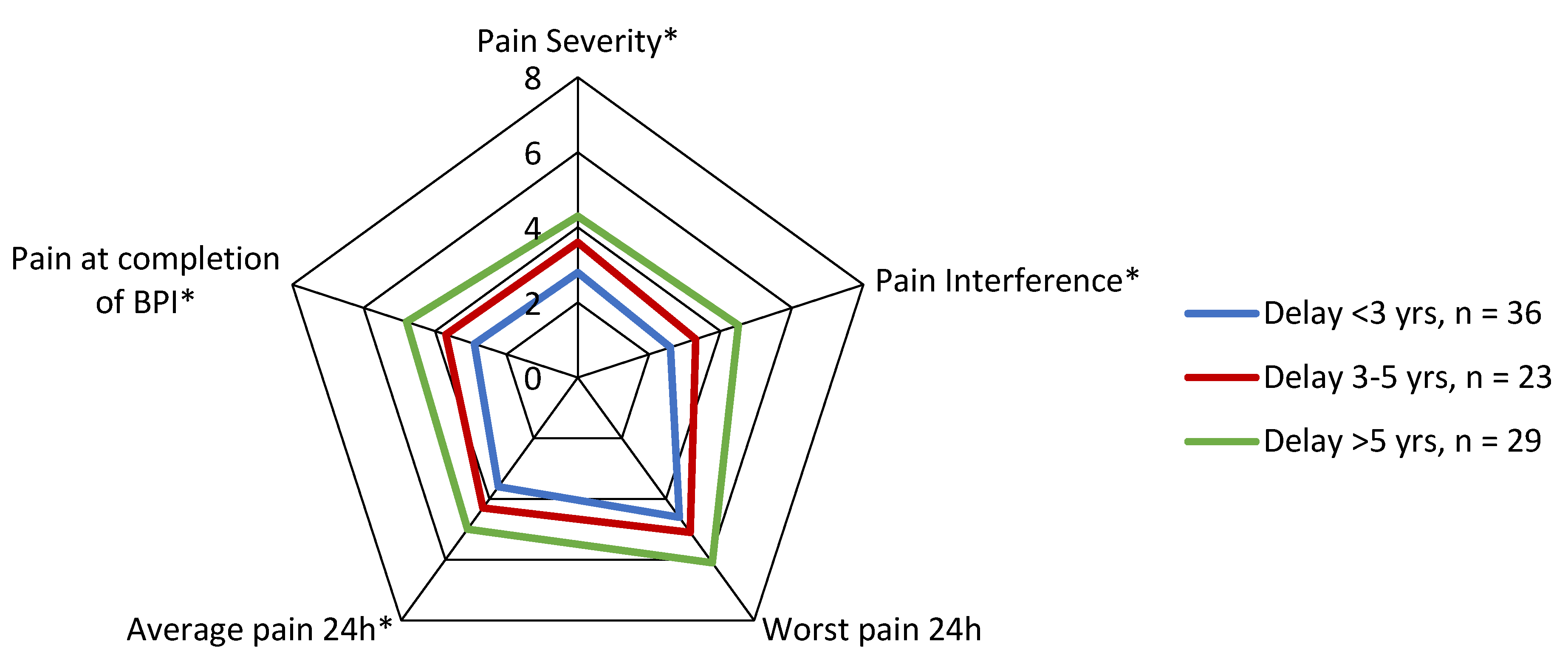
4.3. Shoulder Girdle Function Scores
4.4. Relationship between BPI Scores and SF-36 Scores
4.5. Correlation between Shoulder Function and SF-36 Scores
4.6. Illness Perceptions
4.7. Relationship between Illness Perceptions and SF-36 Scores
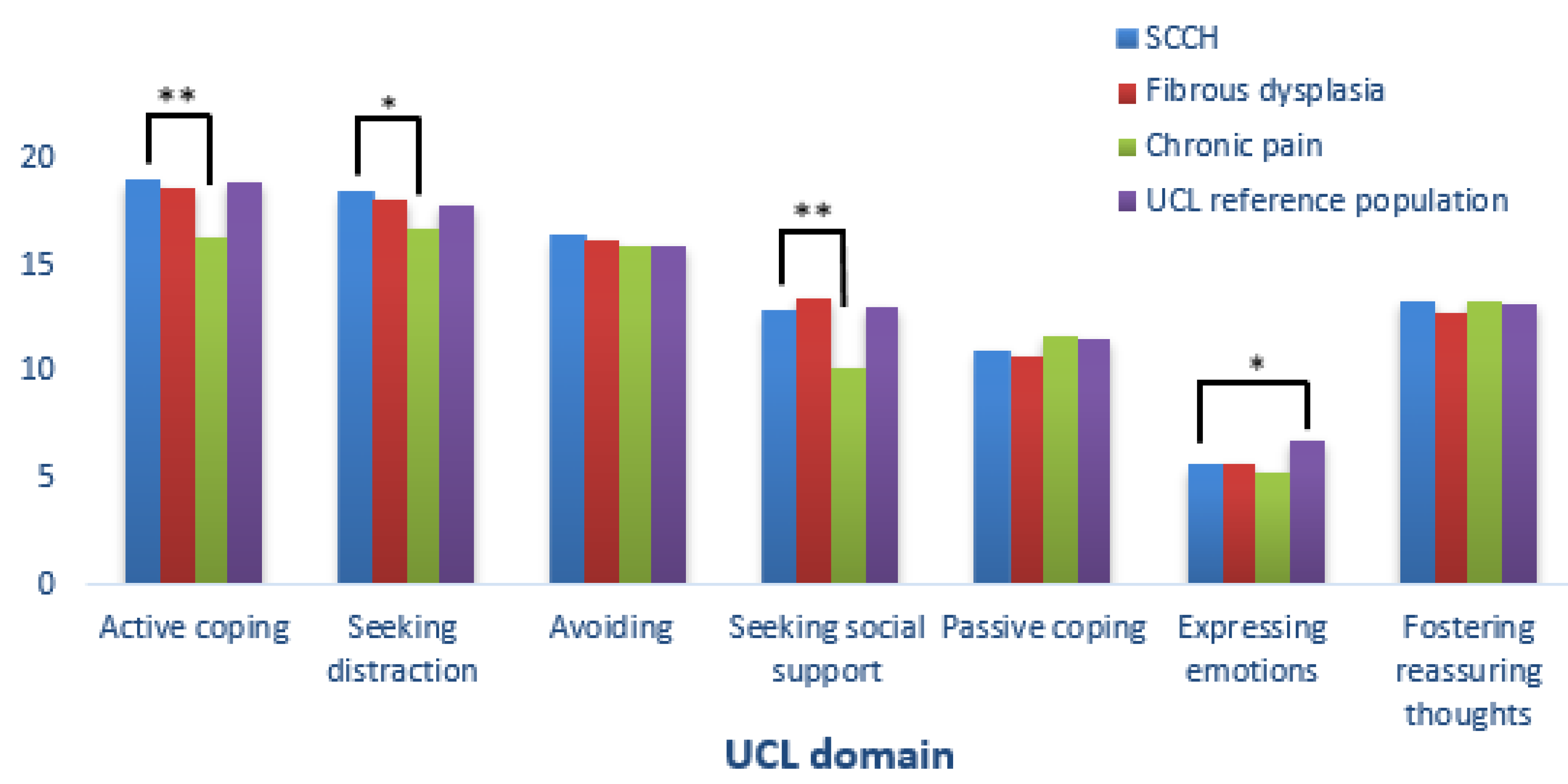
4.8. Coping Strategies
4.9. Relationship between Coping Strategies and BPI and SF-36 Scores
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ramautar, A.I.; Appelman-Dijkstra, N.M.; Lakerveld, S.; Schroijen, M.A.; Snel, M.; Winter, E.M.; Hamdy, N.A.T. Chronic Nonbacterial Osteomyelitis of the Sternocostoclavicular Region in Adults: A Single-Center Dutch Cohort Study. JBMR Plus 2021, 5, e10490. [Google Scholar] [CrossRef] [PubMed]
- van der Kloot, W.A.; Chotkan, S.A.; Kaptein, A.A.; Hamdy, N.A. Diagnostic delay in sternocostoclavicular hyperostosis: Impact on various aspects of quality of life. Arthritis Care Res. 2010, 62, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Schipper, H.; Clinch, J.; Powell, V. Definition and conceptual issues. In Quality of Life Assessments in Clinical Trials; Lippincot-Raven: Philadelphia, PA, USA, 1996; pp. 11–24. [Google Scholar]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef] [PubMed]
- McAndrew, L.M.; Musumeci-Szabó, T.J.; Mora, P.A.; Vileikyte, L.; Burns, E.; Halm, E.A.; Leventhal, H. Using the common sense model to design interventions for the prevention and management of chronic illness threats: From description to process. Br. J. Health Psychol. 2008, 13 Pt 2, 195–204. [Google Scholar] [CrossRef]
- Skinner, E.A.; Zimmer-Gembeck, M.J. Challenges to the developmental study of coping. New Dir. Child. Adolesc. Dev. 2009, 2009, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S. Psychological stress and coping in adaptation and illness. Int. J. Psychiatry Med. 1974, 5, 321–333. [Google Scholar] [CrossRef] [PubMed]
- Tiemensma, J.; Gaab, E.; Voorhaar, M.; Asijee, G.; Kaptein, A.A. Illness perceptions and coping determine quality of life in COPD patients. Int. J. Chron. Obs. Pulmon. Dis. 2016, 11, 2001–2007. [Google Scholar] [CrossRef] [Green Version]
- van Erp, S.J.; Brakenhoff, L.K.; Vollmann, M.; van der Heijde, D.; Veenendaal, R.A.; Fidder, H.H.; Hommes, D.W.; Kaptein, A.A.; van der Meulen-de Jong, A.E.; Scharloo, M. Illness Perceptions and Outcomes in Patients with Inflammatory Bowel Disease: Is Coping a Mediator? Int. J. Behav. Med. 2017, 24, 205–214. [Google Scholar] [CrossRef] [Green Version]
- Lorefice, L.; Fenu, G.; Frau, J.; Coghe, G.; Marrosu, M.G.; Cocco, E. The burden of multiple sclerosis and patients’ coping strategies. BMJ Support. Palliat. Care 2018, 8, 38–40. [Google Scholar] [CrossRef]
- Rotman, M.; Andela, C.D.; Majoor, B.C.J.; Dijkstra, P.D.S.; Hamdy, N.A.T.; Kaptein, A.A.; Appelman-Dijkstra, N.M. Passive Coping Strategies Are Associated With More Impairment In Quality Of Life In Patients With Fibrous Dysplasia. Calcif. Tissue Int. 2018, 103, 469–475. [Google Scholar]
- van der Kloot, W.A.; Hamdy, N.A.; Hafkemeijer, L.C.; den Dulk, F.M.; Chotkan, S.A.; van Emmerik, A.A.; Kaptein, A.A. The psychological burden of an initially unexplained illness: Patients with sternocostoclavicular hyperostosis before and after delayed diagnosis. Health Qual. Life Outcomes 2010, 8, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Cleeland, C.S.; Ryan, K.M. Pain assessment: Global use of the Brief Pain Inventory. Ann. Acad. Med. Singap. 1994, 23, 129–138. [Google Scholar] [PubMed]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef]
- Mendoza, T.; Mayne, T.; Rublee, D.; Cleeland, C. Reliability and validity of a modified Brief Pain Inventory short form in patients with osteoarthritis. Eur. J. Pain 2006, 10, 353–361. [Google Scholar] [CrossRef]
- Song, C.Y.; Lin, S.F.; Huang, C.Y.; Wu, H.C.; Chen, C.H.; Hsieh, C.L. Validation of the Brief Pain Inventory in Patients with Low Back Pain. Spine 2016, 41, E937–E942. [Google Scholar] [CrossRef] [Green Version]
- Broadbent, E.; Petrie, K.J.; Main, J.; Weinman, J. The brief illness perception questionnaire. J. Psychosom. Res. 2006, 60, 631–637. [Google Scholar] [CrossRef]
- Turner, H.; Bryant-Waugh, R.; Peveler, R.; Bucks, R.S. A psychometric evaluation of an English version of the Utrecht Coping List. Eur. Eat. Disord. Rev. 2012, 20, 339–342. [Google Scholar] [CrossRef]
- Schreurs, P.J.G. De Utrechtse Coping Lijst: UCL: Omgaan met Problemen en Gebeurtenissen; Harcourt Test Publ: Amsterdam, The Nederlands, 1993. [Google Scholar]
- L’Insalata, J.C.; Warren, R.F.; Cohen, S.B.; Altchek, D.W.; Peterson, M.G. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J. Bone Joint Surg. Am. 1997, 79, 738–748. [Google Scholar] [CrossRef]
- Paul, A.; Lewis, M.; Shadforth, M.F.; Croft, P.R.; Van Der Windt, D.A.; Hay, E.M. A comparison of four shoulder-specific questionnaires in primary care. Ann. Rheum. Dis. 2004, 63, 1293–1299. [Google Scholar] [CrossRef]
- Kirkley, A.; Griffin, S.; Dainty, K. Scoring systems for the functional assessment of the shoulder. Arthroscopy 2003, 19, 1109–1120. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Muller, M.; Cohen, P.D.; Essink-Bot, M.L.; Fekkes, M.; Sanderman, R.; Sprangers, M.A.; te Velde, A.; Verrips, E. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J. Clin. Epidemiol. 1998, 51, 1055–1068. [Google Scholar] [CrossRef]
- Ataoğlu, S.; Ankaralı, H.; Ankaralı, S.; Ataoğlu, B.B.; Ölmez, S.B. Quality of life in fibromyalgia, osteoarthritis and rheumatoid arthritis patients: Comparison of different scales. Egypt. Rheumatol. 2018, 40, 203–208. [Google Scholar] [CrossRef]
- Majoor, B.C.J.; Andela, C.D.; Bruggemann, J.; van de Sande, M.A.J.; Kaptein, A.A.; Hamdy, N.A.T.; Sander Dijkstra, P.D.; Appelman-Dijkstra, N.M. Determinants of impaired quality of life in patients with fibrous dysplasia. Orphanet J. Rare Dis. 2017, 12, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hopman-Rock, M.; Kraaimaat, F.W.; Bijlsma, J.W. Quality of life in elderly subjects with pain in the hip or knee. Qual. Life Res. 1997, 6, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Majoor, B.C.J.; Papapoulos, S.E.; Dijkstra, P.D.S.; Fiocco, M.; Hamdy, N.A.T.; Appelman-Dijkstra, N.M. Denosumab in Patients With Fibrous Dysplasia Previously Treated With Bisphosphonates. J. Clin. Endocrinol. Metab. 2019, 104, 6069–6078. [Google Scholar] [CrossRef]
| n = 86 | |
|---|---|
| Gender (male/female) | 13/73 (15/85%) |
| Age (yrs) Age at diagnosis (yrs) | 52 (range 23–79) 43 (range 22–69) |
| Delay in diagnosis (yrs) | 3.0 (±5.5 SD) |
| <3 | 36 (41%) |
| 3–5 | 23 (26%) |
| >5 | 29 (33%) |
| Educational Level | |
| Low | 19 (20%) |
| Medium | 37 (42%) |
| High | 29 (33%) |
| Unknown | 4 (5%) |
| Follow-up (yrs) | 5 (range 0–26) |
| Subtypes of CNO/SCCH | |
| Isolated CNO/SCCH | 64 (75%) |
| Additional axial localizations | 22 (25%) |
| Spine | 12 (14%) |
| Mandible | 7 (8%) |
| Both | 3 (3%) |
| Extraskeletal manifestations | 27 (30%) |
| Limitation of Shoulder Function | During Daily Personal and Household Activities | During Recreational or Athletic Activities |
|---|---|---|
| (Very) severe limitation | 32 (36.4) | 39 (46.6) |
| Moderate | 25 (28.4) | 25 (28.4) |
| Mild | 17 (19.3) | 13 (14.8) |
| No | 14 (15.9) | 9 (10.2) |
| B-IPQ | SCCH n = 86 | Asthma n = 309 | Diabetes 2 n = 119 |
|---|---|---|---|
| Consequences | 5.1 (2.8) | 3.5 (2.3) α | 4.7 (2.9) |
| Timeline | 8.9 (2.0) | 8.8 (2.2) | 9.2 (1.9) |
| Personal control | 4.8 (2.7) | 6.7 (2.4) α | 6.7 (2.3) α |
| Treatment control | 6.1 (2.5) | 7.9 (2.0) α | 8.0 (2.3) α |
| Identity | 5.9 (2.6) | 4.5 (2.3) α | 4.6 (2.8) α |
| Illness concern | 4.7 (2.7) | 4.6 (2.8) | 7.0 (3.1) α |
| Coherence | 5.8 (2.6) | 6.5 (2.6) | 7.9 (2.3) α |
| Emotional response | 4.2 (2.9) | 3.3 (2.9) | 4.3 (3.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramautar, A.I.E.; Andela, C.D.; Hamdy, N.A.T.; Winter, E.M.; Appelman-Dijkstra, N.M. Determinants of Quality of Life in Adult Patients with Chronic Non-Bacterial Osteomyelitis (CNO) of the Sternocostoclavicular Region (SCCH): A Dutch Single Center Study. J. Clin. Med. 2022, 11, 1852. https://doi.org/10.3390/jcm11071852
Ramautar AIE, Andela CD, Hamdy NAT, Winter EM, Appelman-Dijkstra NM. Determinants of Quality of Life in Adult Patients with Chronic Non-Bacterial Osteomyelitis (CNO) of the Sternocostoclavicular Region (SCCH): A Dutch Single Center Study. Journal of Clinical Medicine. 2022; 11(7):1852. https://doi.org/10.3390/jcm11071852
Chicago/Turabian StyleRamautar, Ashna I. E., Cornelie D. Andela, Neveen A. T. Hamdy, Elizabeth M. Winter, and Natasha M. Appelman-Dijkstra. 2022. "Determinants of Quality of Life in Adult Patients with Chronic Non-Bacterial Osteomyelitis (CNO) of the Sternocostoclavicular Region (SCCH): A Dutch Single Center Study" Journal of Clinical Medicine 11, no. 7: 1852. https://doi.org/10.3390/jcm11071852
APA StyleRamautar, A. I. E., Andela, C. D., Hamdy, N. A. T., Winter, E. M., & Appelman-Dijkstra, N. M. (2022). Determinants of Quality of Life in Adult Patients with Chronic Non-Bacterial Osteomyelitis (CNO) of the Sternocostoclavicular Region (SCCH): A Dutch Single Center Study. Journal of Clinical Medicine, 11(7), 1852. https://doi.org/10.3390/jcm11071852






