Pelvic Floor Dysfunctions and Their Rehabilitation in Multiple Sclerosis
Abstract
1. Introduction
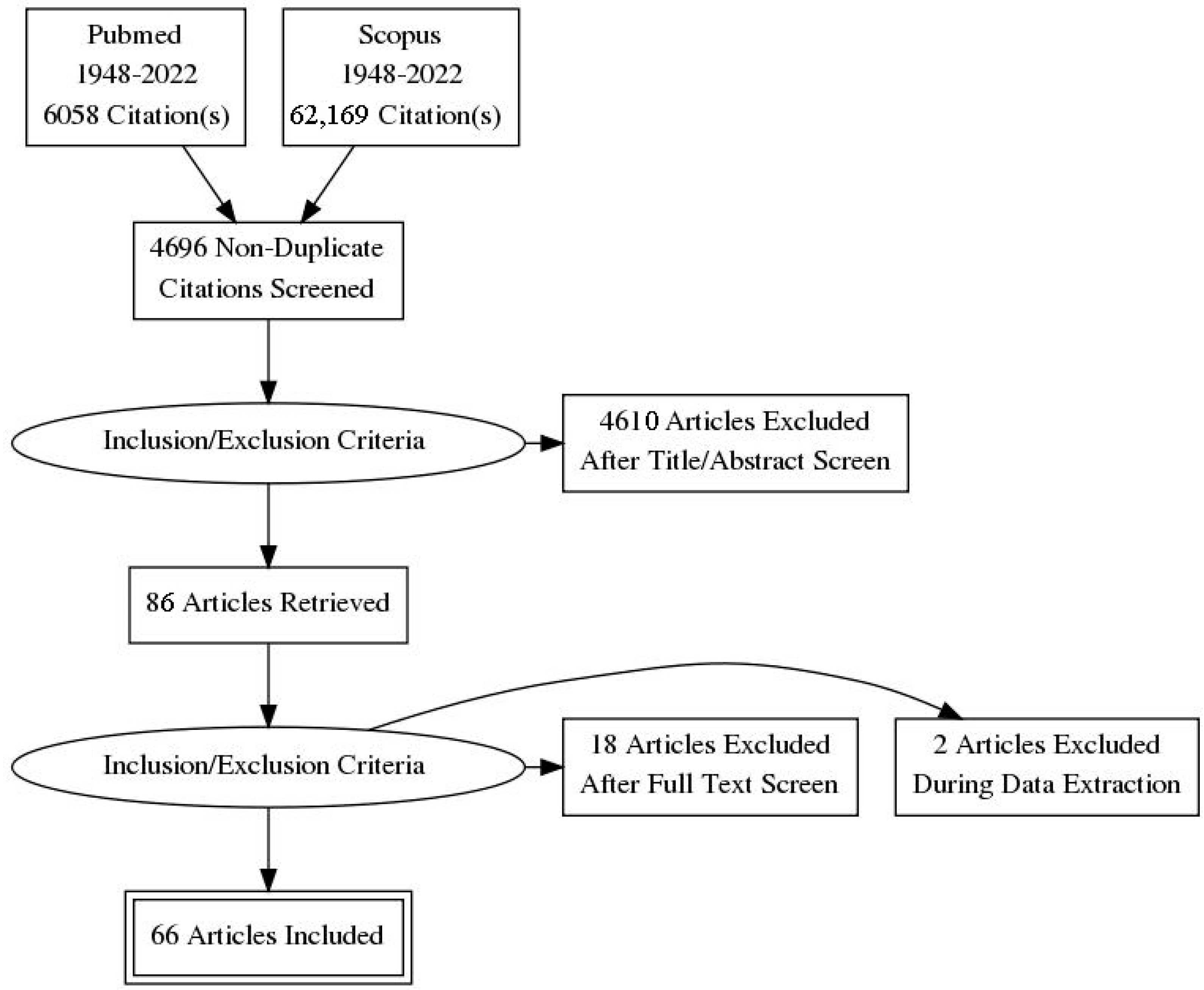
2. Materials and Methods
Search Strategy and Selection Criteria
- (a)
- Population of interest: adults with MS with bladder, bowel, or sexual dysfunctions;
- (b)
- Intervention: rehabilitation program, including physical exercise and/or instrumental techniques;
- (c)
- Outcomes: symptoms, impact on quality of life, improvement in self-reported questionnaires, pad test, urodynamic evaluation;
- (d)
- Design: prospective and retrospective studies, randomized controlled trials;
3. Pelvic Floor Dysfunctions in MS
3.1. Urinary Dysfunctions in MS
3.2. Anorectal Dysfunctions in MS
3.3. Sexual Dysfunctions in MS
- -
- primary causes, related to direct neurological damage due to demyelinating lesions (i.e., impaired genital sensation), decreased sexual desire, and orgasmic dysfunctions;
- -
- secondary causes, as a consequence of MS-related physical changes, such as spasticity, pain, fatigue.
- -
- tertiary causes, linked to psychosocial and cultural aspects, which interfere with sexual satisfaction, such as mood disorders or impaired partner relationships [20].
4. Sphincteric Patient-Reported Outcomes
4.1. Urinary Dysfunctions
- Actionable Bladder Symptom Screening Tool (ABSST) [26] (specifically designed for pwMS with urinary incontinence, to help identify who may need and benefit from assessment and treatment).
- Neurogenic Bladder Symptom Score (NBSS) [27] (designed to assess bladder symptoms and consequences among patients with neurogenic bladder due to neurological disease or lesions, such as MS, spinal cord injuries, or spina bifida). The authors validated each domain as an independent subscale, so to use them not only in combination but also separately [28].
- International Prostate Symptom Score (IPSS) [31].
4.2. Anorectal Dysfunctions
4.3. Sexual Dysfunctions
- The Sexual Dysfunction Management and Expectations Assessment in Multiple Sclerosis Female (SEA-MS-F) [37] (developed to ascertain women’s expectations concerning the treatment of sexual dysfunction),
- The Female sexual function questionnaire (SFQ-28) [40], organized into seven domains of female sexual function: desire, physical arousal–sensation, physical arousal–lubrication, enjoyment, orgasm, pain, and partner relationship. Scores for Desire, Arousal, Orgasm, Pain, and Enjoyment are subdivided into three categories that include a high probability of sexual dysfunctions, borderline sexual function, and high probability of normal sexual function. Partner domain and total score are not subdivided into categories, but higher scores indicate better relationships and so less sexual dysfunctions.
- The Female Sexual Function Index (FSFI) [41].
5. Pelvic Floor Rehabilitation in MS
- (a)
- a behavioral construct, to learn how to consciously pre-contract the PF muscles before and during increases in abdominal pressure to prevent leakage and
- (b)
- two constructs based on changing the neuromuscular function and morphology:
- strength training builds up long-lasting muscle volume and thus provides structural support;
- abdominal muscle training indirectly strengthens the PF muscles.
6. Limitations
- a high coexistence of bowel and bladder dysfunctions;
- a coexistence of mixed sphincter dysfunctions (retention plus urgency or incontinence);
- absence of correlation between the pattern of bowel symptoms and urinary disturbance.
- absence of a consensus on the protocol to use to manage PF dysfunction,
- absence of a uniform approach to PF exercises,
- different devices or methods used in addition to PF training,
- different evaluation of PF dyssynergia in pwMS (clinical parameters, patient-reported outcomes, EMG activity, manometry),
- a shortage of studies on anorectal dysfunctions treatment,
- absence of data on the long-term benefit of PFMT.
7. Discussion and Conclusions
- The first diagnostic step is screening for PF disorders, also in a- or paucisymptomatic pwMS, using a self-administered scale (PROs) considering bladder, bowel, and sexual functions.
- The second diagnostic step is a specific assessment, based on the results of PROs, considering urine testing (if pwMS presented UTI symptoms), abdominal ultrasound, and, in the second line, urodynamics and manometric exams. We highlight, at this step, the importance of a correct assessment of PF contractions with a digital technique, based on the PERFECT scheme: P meaning power (or pressure), E, endurance, R, repetitions, F, fast contractions, and finally, ECT, every contraction timed. The use of a perineometer could help in this assessment [73].
- (1)
- The first therapeutic step is based on a conservative approach: adequate diet and lifestyle and/or a pharmacologic approach (for example, with alpha-blockers, antimuscarinic anti-diarrheic agents, prokinetics), psychological assessment, and physiotherapeutic evaluation to perform a correct PFMT (in particular, in pwMS with mild disability), with or without biofeedback, NMES, TTNS.
- (2)
- The second therapeutic step is based on a progressively more invasive approach: from intermittent self-catheterization and/or anal irrigation to detrusor injection of botulinum toxin A or sacral neuromodulation.
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Neurostatus. Available online: http://www.neurostatus.net (accessed on 16 January 2022).
- Mahajan, S.T.; James, R.; Frasure, H. Pelvic floor disorders and multiple sclerosis: Are patients satisfied with their care? Int. J. MS Care 2014, 16, 20–25. [Google Scholar] [CrossRef]
- Aguilar-Zafra, S.; Del Corral, T.; Vidal-Quevedo, C.; Rodríguez-Durán, P.; López-de-Uralde-Villanueva, I. Pelvic floor dysfunction negatively impacts general functional performance in patients with multiple sclerosis. Neurourol. Urodyn. 2020, 39, 978–986. [Google Scholar] [CrossRef] [PubMed]
- DasGupta, R.; Fowler, C.J. Bladder, bowel and sexual dysfunction in multiple sclerosis: Management strategies. Drugs 2003, 63, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Litwiller, S.E.; Frohman, E.M.; Zimmern, P.E. Multiple sclerosis and the urologist. J. Urol. 1999, 161, 743–757. [Google Scholar] [CrossRef]
- Fowler, C.J.; Panicker, J.N.; Drake, M.; Harris, C.; Harrison, S.C.W.; Kirby, M.; Lucas, M.; Macleod, N.; Mangnall, J.; North, A.; et al. A UK consensus of the management of the bladder in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2009, 80, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Lensch, E.; Jost, W.H. Autonomic disorders in multiple sclerosis. Autoimmune Dis. 2011, 80, 470–477. [Google Scholar] [CrossRef]
- Ghezzi, A.; Mutta, E.; Bianchi, F.; Bonavita, S.; Buttari, F.; Caramma, A.; Cavarretta, R.; Centonze, D.; Coghe, G.C.; Coniglio, G.; et al. Diagnostic tools for assessment of urinary dysfunction in MS patients without urinary disturbances. Neurol. Sci. 2016, 37, 437–442. [Google Scholar] [CrossRef]
- Amarenco, G.; de Sèze, M.; Ruffion, A.; Sheikh Ismael, S. Clinical and urodynamic evaluations of urinary disorders in multiple sclerosis. Ann. Phys. Rehabil. Med. 2014, 57, 277–287. [Google Scholar] [CrossRef]
- Esposito, S.; Bonavita, S.; Sparaco, M.; Gallo, A.; Tedeschi, G. The role of diet in multiple sclerosis: A review. Nutr. Neurosci. 2018, 21, 377–390. [Google Scholar] [CrossRef]
- Kaplan, S.A.; Dmochowski, R.; Cash, B.D.; Kopp, Z.S.; Berriman, S.J.; Khullar, V. Systematic review of the relationship between bladder and bowel function: Implications for patient management. Int. J. Clin. Pract. 2013, 67, 205–216. [Google Scholar] [CrossRef]
- Chia, Y.W.; Gill, K.P.; Jameson, J.S.; Forti, A.D.; Henry, M.M.; Swash, M.; Shorvon, P.J. Paradoxical puborectalis contraction is a feature of constipation in patients with multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 1996, 60, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Marola, S.; Ferrarese, A.; Gibin, E.; Capobianco, M.; Bertolotto, A.; Enrico, S.; Solej, M.; Martino, V.; Destefano, I.; Nano, M. Anal sphincter dysfunction in multiple sclerosis: An observation manometric study. Open Med. 2016, 11, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Munteis, E.; Andreu, M.; Martinez-Rodriguez, J.E.; Ois, A.; Bory, F.; Roquer, J. Manometric correlations of anorectal dysfunction and biofeedback outcome in patients with multiple sclerosis. Mult. Scler. 2008, 14, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.S.; Rogers, J.; Chia, Y.W.; Misiewicz, J.J.; Henry, M.M.; Swash, M. Pelvic floor function in multiple sclerosis. Gut 1994, 35, 388–390. [Google Scholar] [CrossRef][Green Version]
- Preziosi, G.; Raptis, D.A.; Raeburn, A.; Panicker, J.; Emmanuel, A. Autonomic rectal dysfunction in patients with multiple sclerosis and bowel symptoms is secondary to spinal cord disease. Dis. Colon Rectum 2014, 57, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Nusrat, S.; Gulick, E.; Levinthal, D.; Bielefeldt, K. Anorectal Dysfunction in Multiple Sclerosis: A Systematic Review. ISRN Neurol. 2012, 2012, 376023. [Google Scholar] [CrossRef]
- Drulovic, J.; Kisic-Tepavcevic, D.; Pekmezovic, T. Epidemiology, diagnosis and management of sexual dysfunction in multiple sclerosis. Acta Neurol. Belg. 2020, 120, 791–797. [Google Scholar] [CrossRef]
- Sadeghi-Bahmani, D.; Motl, R.W. Rate, burden, and treatment of sexual dysfunction in multiple sclerosis: The case for exercise training as a new treatment approach. Mult. Scler. Relat. Disord. 2021, 51, 102878. [Google Scholar] [CrossRef]
- Abrams, P.; Avery, K.; Gardener, N.; Donovan, J.; ICIQ Advisory Board. The International Consultation on Incontinence Modular Questionnaire. J. Urol. 2006, 175, 1063–1066. Available online: http://www.iciq.net (accessed on 27 December 2021). [CrossRef]
- Coyne, K.; Revicki, D.; Hunt, T.; Corey, R.; Stewart, W.; Bentkover, J.; Kurth, H.; Abrams, P. Psychometric validation of an overactive bladder symptom and health-related quality of life questionnaire: The OAB-q. Qual. Life Res. 2002, 11, 563–574. [Google Scholar] [CrossRef]
- Coyne, K.; Thompson, C.L.; Lai, J.S.; Sexton, C.C. An overactive bladder symptom and health-related quality of life short-form: Validation of the OAB-q SF. Neurourol. Urodyn. 2015, 34, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Coyne, K.S.; Zyczynski, T.; Margolis, M.K.; Elinoff, V.; Roberts, R. Validation of an overactive bladder awareness tool for use in primary care settings. Adv. Ther. 2005, 22, 381–394. [Google Scholar] [CrossRef] [PubMed]
- Burks, J.; Chancellor, M.; Bates, D.; Denys, P.; Macdiarmid, S.; Nitti, V.; Globe, D.; Signori, M.; Hudgens, S.; Odderson, I.; et al. Development and validation of the actionable bladder symptom screening tool for multiple sclerosis patients. Int. J. MS Care 2013, 15, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Welk, B.; Morrow, S.A.; Madarasz, W.; Potter, P.; Sequeira, K. The conceptualization and development of a patient-reported neurogenic bladder symptom score. Res. Rep. Urol. 2013, 5, 129–137. [Google Scholar] [CrossRef]
- Cintra, L.K.L.; de Bessa Júnior, J.; Kawahara, V.I.; Ferreira, T.P.A.; Srougi, M.; Battistella, L.R.; de Souza, D.R.; Bruschini, H.; Gomes, C.M. Cross-cultural adaptation and validation of the neurogenic bladder symptom score questionnaire for Brazilian Portuguese. Int. Braz. J. Urol. 2019, 45, 605–614. [Google Scholar] [CrossRef]
- Bonniaud, V.; Parratte, B.; Amarenco, G.; Jackowski, D.; Didier, J.P.; Guyatt, G. Measuring quality of life in multiple sclerosis patients with urinary disorders using the Qualiveen questionnaire. Arch. Phys. Med. Rehabil. 2004, 85, 1317–1323. [Google Scholar] [CrossRef]
- Bonniaud, V.; Bryant, D.; Parratte, B.; Guyatt, G. Development and validation of the short form of a urinary quality of life questionnaire: SF-Qualiveen. J. Urol. 2008, 180, 2592–2598. [Google Scholar] [CrossRef]
- Barry, M.J.; Fowler, F.J., Jr.; O’leary, M.P.; Bruskewitz, R.C.; Holtgrewe, H.L.; Mebust, W.K.; Cockett, A.T.K.; The Measurement Committee of the American Urological Association. American Urological Association symptom index for benign prostatic hyperplasia. J. Urol. 1992, 148, 1549–1557. [Google Scholar] [CrossRef]
- Preziosi, G.; Raptis, D.A.; Storrie, J.; Raeburn, A.; Fowler, C.J.; Emmanuel, A. Bowel biofeedback treatment in patients with multiple sclerosis and bowel symptoms. Dis. Colon Rectum 2011, 54, 1114–1121. [Google Scholar] [CrossRef]
- Krogh, K.; Christensen, P.; Sabroe, S.; Laurberg, S. Neurogenic bowel dysfunction score. Spinal Cord 2006, 44, 625–631. [Google Scholar] [CrossRef]
- Passananti, V.; Wilton, A.; Preziosi, G.; Storrie, J.B.; Emmanuel, A. Long-term efficacy and safety of transanal irrigation in multiple sclerosis. Neurogastroenterol. Motil. 2016, 28, 1349–1355. [Google Scholar] [CrossRef] [PubMed]
- Agachan, F.; Chen, T.; Pfeifer, J.; Reissman, P.; Wexner, S.D. A constipation scoring system to simplify evaluation and management of constipated patients. Dis. Colon Rectum 1996, 39, 681–685. [Google Scholar] [CrossRef] [PubMed]
- Jorge, J.M.; Wexner, S.D. Etiology and management of fecal incon-tinence. Dis. Colon Rectum 1993, 36, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Bisseriex, H.; Guinet-Lacoste, A.; Chevret-Measson, M.; Costa, P.; Sheikh Ismael, S.; Rousseau, A.; Amarenco, G. Sexual Dysfunction Management and Expectations Assessment in Multiple Sclerosis-Female (SEA-MS-F): Creation and Validation of a Specific Questionnaire. J. Sex. Med. 2014, 11, 2955–2965. [Google Scholar] [CrossRef]
- Sanders, A.S.; Foley, F.W.; LaRocca, N.G.; Nicholas, G.; Zemon, V. The multiple sclerosis intimacy and sexuality questionnaire-19 (MSISQ-19). Sex. Disabil. 2000, 18, 3–24. [Google Scholar] [CrossRef]
- Foley, F.W.; Zemon, V.; Campagnolo, D.; Marrie, R.A.; Cutter, G.; Tyry, T.; Beier, M.; Farrell, E.; Vollmer, T.; Schairer, L. The multiple sclerosis intimacy and sexuality questionnaire: Re-validation and development of a 15-item version with a large US sample. Mult. Scler. 2013, 19, 1197–1203. [Google Scholar] [CrossRef]
- Quirk, F.H.; Heiman, J.R.; Rosen, R.C.; Laan, E.; Smith, M.D.; Boolell, M.D. Development of the sexual function questionnaire for clinical trials of female sexual dysfunction. J. Women’s Health Gend.-Based Med. 2012, 11, 277–289. [Google Scholar] [CrossRef]
- Rosen, R.; Brown, C.; Heiman, J.; Leiblum, S.; Meston, C.; Shabsigh, R.; Ferguson, D.; D’Agostino, R., Jr. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J. Sex Marital Ther. 2000, 26, 191–208. [Google Scholar] [CrossRef]
- Kegel, A. Progressive resistance exercise in the functional restoration of the perineal muscles. Am. J. Obstet. Gynecol. 1948, 56, 238–248. [Google Scholar] [CrossRef]
- Bø, K. Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work? Int. Urogynecol. J. Pelvic Floor Dysfunct. 2004, 15, 76–84. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, D.; Vermeulen, C.; Ketelaer, P.; Van Poppel, H.; Baert, L. Pelvic floor rehabilitation in multiple sclerosis. Acta Neurol. Belg. 1999, 99, 61–64. [Google Scholar]
- Lúcio, A.C.; Perissinoto, M.C.; Natalin, R.A.; Prudente, A.; Damasceno, B.P.; D’ancona, C.A. A comparative study of pelvic floor muscle training in women with multiple sclerosis: Its impact on lower urinary tract symptoms and quality of life. Clinics 2011, 66, 1563–1568. [Google Scholar] [CrossRef]
- Pérez, D.C.; Chao, C.W.; Jiménez, L.L.; Fernández, I.M.; de la Llave Rincón, A.I. Pelvic floor muscle training adapted for urinary incontinence in multiple sclerosis: A randomized clinical trial. Int. Urogynecol. J. 2020, 31, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Lúcio, A.; D’ancona, C.A.; Perissinotto, M.C.; McLean, L.; Damasceno, B.P.; de Moraes Lopes, M.H. Pelvic Floor Muscle Training with and without Electrical Stimulation in the Treatment of Lower Urinary Tract Symptoms in Women with Multiple Sclerosis. J. Wound Ostomy Cont. Nurs. 2016, 43, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Lúcio, A.C.; Campos, R.M.; Perissinotto, M.C.; Miyaoka, R.; Damasceno, B.P.; D’ancona, C.A. Pelvic floor muscle training in the treatment of lower urinary tract dysfunction in women with multiple sclerosis. Neurourol. Urodyn. 2010, 29, 1410–1413. [Google Scholar] [CrossRef]
- Polat Dunya, C.; Tulek, Z.; Kürtüncü, M.; Panicker, J.N.; Eraksoy, M. Effectiveness of the transcutaneous tibial nerve stimulation and pelvic floor muscle training with biofeedback in women with multiple sclerosis for the management of overactive bladder. Mult. Scler. 2020, 27, 621–629. [Google Scholar] [CrossRef] [PubMed]
- McClurg, D.; Ashe, R.G.; Marshall, K.; Lowe-Strong, A.S. Comparison of pelvic floor muscle training, electromyography biofeedback, and neuromuscular electrical stimulation for bladder dysfunction in people with multiple sclerosis: A randomized pilot study. Neurourol. Urodyn. 2006, 25, 337–348. [Google Scholar] [CrossRef]
- McClurg, D.; Ashe, R.G.; Lowe-Strong, A.S. Neuromuscular electrical stimulation and the treatment of lower urinary tract dysfunction in multiple sclerosis–A double blind, placebo controlled, randomised clinical trial. Neurourol. Urodyn. 2008, 27, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.P.; Pegorare, A.B.; Salgado, P.R.; Casafus, F.S.; Christofoletti, G. Impact of a Pelvic Floor Training Program among Women with Multiple Sclerosis: A Controlled Clinical Trial. Am. J. Phys. Med. Rehabil. 2016, 95, 1–8. [Google Scholar] [CrossRef]
- Silva Ferreira, A.P.; de Souza Pegorare, A.B.G.; Miotto Junior, A.; Salgado, P.R.; Medola, F.O.; Christofoletti, G. A Controlled Clinical Trial on the Effects of Exercise on Lower Urinary Tract Symptoms in Women with Multiple Sclerosis. Am. J. Phys. Med. Rehabil. 2019, 98, 777–782. [Google Scholar] [CrossRef]
- Lúcio, A.C.; D’Ancona, C.A.; Lopes, M.H.; Perissinotto, M.C.; Damasceno, B.P. The effect of pelvic floor muscle training alone or in combination with electrostimulation in the treatment of sexual dysfunction in women with multiple sclerosis. Mult. Scler. 2014, 20, 1761–1768. [Google Scholar] [CrossRef]
- Polat Dunya, C.; Tülek, Z.; Kürtüncü, M.; Gündüz, T.; Panicker, J.N.; Eraksoy, M. Evaluating the effects of transcutaneous tibial nerve stimulation or pelvic floor muscle training on sexual dysfunction in female multiple sclerosis patients reporting overactive bladder. Neurourol. Urodyn. 2021, 40, 1661–1669. [Google Scholar] [CrossRef]
- Altunan, B.; Gundogdu, A.A.; Ozcaglayan, T.I.K.; Unal, A.; Turgut, N. The effect of pelvic floor exercise program on incontinence and sexual dysfunction in multiple sclerosis patients. Int. Urol. Nephrol. 2021, 53, 1059–1065. [Google Scholar] [CrossRef]
- Primus, G. Maximal electrical stimulation in neurogenic detrusor hyperactivity: Experiences in multiple sclerosis. Eur. J. Med. 1992, 1, 80–82. [Google Scholar] [PubMed]
- Lavorgna, L.; Sparaco, M.; Esposito, S.; Motl, R.W.; Gallo, A.; Bisecco, A.; Tedeschi, G.; Bonavita, S. Validity and reproducibility of the Italian version of the patient determined disease steps scale in people with multiple sclerosis. Mult. Scler. Relat. Disord. 2017, 18, 173–176. [Google Scholar] [CrossRef]
- Norton, C.; Chelvanayagam, S.; Wilson-Barnett, J.; Redfern, S.; Kamm, M.A. Randomized controlled trial of biofeedback for fecal incontinence. Gastroenterology 2003, 125, 1320–1329. [Google Scholar] [CrossRef]
- Schott, A.M.; Damon, H.; Mion, F.; Siproudhis, L. A randomized controlled trial of biofeedback that does not have the power to conclude. Gastroenterology 2004, 126, 1496–1497. [Google Scholar] [CrossRef]
- Parodi, B.; de Rosbo, N.K. The Gut-Brain Axis in Multiple Sclerosis. Is Its Dysfunction a Pathological Trigger or a Consequence of the Disease? Front. Immunol. 2021, 12, 34621267. [Google Scholar] [CrossRef] [PubMed]
- Cantarel, B.L.; Waubant, E.; Chehoud, C.; Kuczynski, J.; DeSantis, T.Z.; Warrington, J.; Venkatesan, A.; Fraser, C.M.; Mowry, E.M. Gut microbiota in multiple sclerosis: Possible influence of immunomodulators. J. Investig. Med. 2015, 63, 729–734. [Google Scholar] [CrossRef]
- Tremlett, H.; Fadrosh, D.W.; Faruqi, A.A.; Hart, J.; Roalstad, S.; Graves, J.; Lynch, S.; Waubant, E.; US Network of Pediatric MS Centers. Gut microbiota composition and relapse risk in pediatric MS: A pilot study. J. Neurol. Sci. 2016, 363, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Adamczyk-Sowa, M.; Medrek, A.; Madej, P.; Michlicka, W.; Dobrakowski, P. Does the Gut Microbiota Influence Immunity and Inflammation in Multiple Sclerosis Pathophysiology? J. Immunol. Res. 2017, 2017, 7904821. [Google Scholar] [CrossRef]
- Miyake, S.; Kim, S.; Suda, W.; Oshima, K.; Nakamura, M.; Matsuoka, T.; Chihara, N.; Tomita, A.; Sato, W.; Kim, S.W.; et al. Dysbiosis in the Gut Microbiota of Patients with Multiple Sclerosis, with a Striking Depletion of Species Belonging to Clostridia XIVa and IV Clusters. PLoS ONE 2015, 10, e0137429. [Google Scholar] [CrossRef]
- Wiesel, P.H.; Norton, C.; Roy, A.J.; Storrie, J.B.; Bowers, J.; Kamm, M.A. Gut focused behavioural treatment (biofeedback) for constipation and faecal incontinence in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2000, 69, 240–243. [Google Scholar] [CrossRef]
- Chia, J.W.; Fowler, C.J.; Kamm, M.A.; Henry, M.M.; Lemieux, M.C.; Swash, M. Prevalence of bowel dysfunction in patients with multiple sclerosis and bladder dysfunction. J. Neurol. 1995, 242, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Tavazzi, E.; Bergsland, N.; Cattaneo, D.; Gervasoni, E.; Lagana, M.M.; Dipasquale, O.; Grosso, C.; Saibene, F.L.; Baglio, F.; Rovaris, M. Effects of motor rehabilitation on mobility and brain plasticity in multiple sclerosis: A structural and functional MRI study. J. Neurol. 2018, 265, 1393–1401. [Google Scholar] [CrossRef] [PubMed]
- Bonavita, S.; Sacco, R.; Della Corte, M.; Esposito, S.; Sparaco, M.; d’Ambrosio, A.; Docimo, R.; Bisecco, A.; Lavorgna, L.; Corbo, D.; et al. Computer-aided cognitive rehabilitation improves cognitive performances and induces brain functional connectivity changes in relapsing remitting multiple sclerosis patients: An exploratory study. J. Neurol. 2015, 262, 91–100. [Google Scholar] [CrossRef]
- Prosperini, L.; Di Filippo, M. Beyond clinical changes: Rehabilitation-induced neuroplasticity in MS. Mult. Scler. 2019, 25, 1348–1362. [Google Scholar] [CrossRef]
- Amatya, B.; Khan, F.; Galea, M. Rehabilitation for people with multiple sclerosis: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2019, 1, CD012732. [Google Scholar] [CrossRef]
- Dumoulin, C.; Cacciari, L.P.; Hay-Smith, E.J.C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst. Rev. 2018, 10, CD005654. [Google Scholar] [CrossRef] [PubMed]
- Laycock, J.; Jerwood, D. Pelvic Floor Muscle Assessment: The PERFECT Scheme. Physiotherapy 2001, 87, 631–642. [Google Scholar] [CrossRef]
| Questionnaire | Items | Score | Signification | Notes |
|---|---|---|---|---|
| URINARY DYSFUNCTIONS | ||||
| ICI-Q UI SF | 4 | 0 to 21 | higher scores: greater severity of symptoms | |
| OAB-q | 33 | 0 to 100 | higher scores: greater severity of symptoms and lower QoL | Two short forms: OABq-SF and OAB-V8 |
| ABSST | 8 | ≥3 need for further urogynecological evaluation and treatment | ||
| NBSS | 25 | 0 to 74 | higher scores: greater severity of symptoms | Three domains: Incontinence, Storage and Voiding, and Consequences (used not only in combination but also separately) |
| Qualiveen | 30 | for each domain 0: no effect of urinary problems on QoL 4: high impact on QoL | higher scores: higher QoL | Short form: 8 items |
| IPSS | 7 | 0–7—mild 8–19—moderate 20–35—severe | measure of frequency and severity of symptoms | An additional item measures the impact on QoL |
| ANORECTAL DYSFUNCTIONS | ||||
| NBD | 10 | 0 to 47 | higher score: higher severity of dysfunction | |
| Wexner incontinence score | 5 | 0 to 20 | 0: absence of symptoms, 20: highest severity of symptoms | |
| Wexner constipation score | 8 | 0 to 30 | 0: absence of symptoms, 30: highest severity of symptoms | |
| SEXUAL DYSFUNCTIONS | ||||
| SEA-MS-F | 8 | 0 to 32 | organized into 3 parts: general expectations (sexuality); specific expectations (sexual symptoms); ultimate goals for treatment of sexual dysfunction | |
| MSISQ-19 | 19 | 19 to 95 | higher scores: greater impact of MS symptoms on sexual life | Specific subscale (used also separately) for the primary, secondary, and tertiary aspects of sexual dysfunctions in MS |
| MSISQ-15 | 15 | 15 to 75 | higher scores: greater impact of MS symptoms on sexual life | Specific subscale (used also separately) for the primary, secondary, and tertiary aspects of sexual dysfunctions in MS |
| SFQ-28 | 28 | each of the 7 domains has a different score range, indicating (from the lower to the higher scores) high probability of sexual dysfunction, borderline status, and normal sexual function | ||
| FSFI | 19 | 2 to 36 | Higher scores indicate better sexual functioning | Six domains: sexual desire, sexual arousal, lubrication, orgasm, satisfaction, and pain |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sparaco, M.; Bonavita, S. Pelvic Floor Dysfunctions and Their Rehabilitation in Multiple Sclerosis. J. Clin. Med. 2022, 11, 1941. https://doi.org/10.3390/jcm11071941
Sparaco M, Bonavita S. Pelvic Floor Dysfunctions and Their Rehabilitation in Multiple Sclerosis. Journal of Clinical Medicine. 2022; 11(7):1941. https://doi.org/10.3390/jcm11071941
Chicago/Turabian StyleSparaco, Maddalena, and Simona Bonavita. 2022. "Pelvic Floor Dysfunctions and Their Rehabilitation in Multiple Sclerosis" Journal of Clinical Medicine 11, no. 7: 1941. https://doi.org/10.3390/jcm11071941
APA StyleSparaco, M., & Bonavita, S. (2022). Pelvic Floor Dysfunctions and Their Rehabilitation in Multiple Sclerosis. Journal of Clinical Medicine, 11(7), 1941. https://doi.org/10.3390/jcm11071941







