Preventive Measures against Pandemics from the Beginning of Civilization to Nowadays—How Everything Has Remained the Same over the Millennia
Abstract
:1. Introduction
- (1)
- Residual symptoms continuing after acute infection recovery;
- (2)
- Organ dysfunction continuing after initial recovery;
- (3)
- New symptoms/syndromes developing after initial asymptomatic or mild infection [6].
Communicable Diseases
- (1)
- The pathogen infects only animals under natural conditions;
- (2)
- The pathogen evolves to be transmitted to humans without continuous human-to-human transmission;
- (3)
- The pathogen undergoes secondary transmission to humans;
- (4)
- The disease exists in animals but different secondary human-to-human transmission occurs without the involvement of animal hosts;
- (5)
- The disease occurs exclusively in humans.
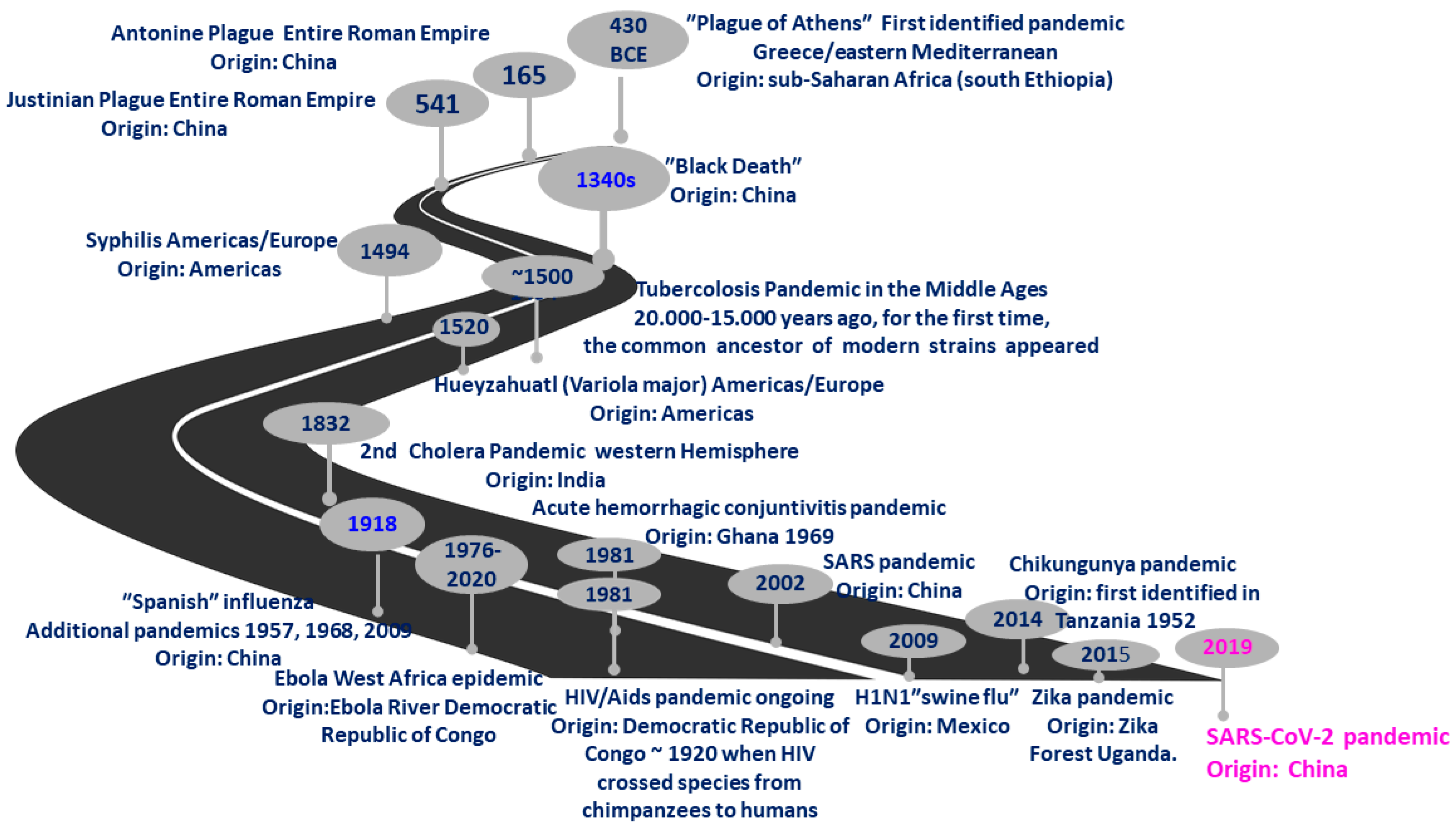
2. History of “Plagues”
| Years | Discovery | References |
|---|---|---|
| 1530 | Girolamo Fracastoro expresses his ideas on the origin of syphilis, explaining that this disease is spread by “seeds” distributed by intimate contact | [43] |
| 1683 | Anton van Leeuwenhoek observes bacteria under the first microscope | [44] |
| 1701–1714 | Giacomo Pilarino and Emmanuel Timoni give the first smallpox inoculations | [45] |
| 1757 | Francis Home demonstrates that measles is caused by an infectious agent in the blood of patients | [46] |
| 1796 | Edward Jenner develops the process of vaccination for smallpox, the first vaccine for any disease | [45] |
| 1842–1847 | Oliver Wendel Holmes describes puerperal fever and Ignaz Semmelweis discovers how to prevent the transmission of puerperal fever | [44] |
| 1857 | Louis Pasteur identifies germs as a cause of disease | [47] |
| 1870 | Robert Koch and Louis Pasteur establish the germ theory of disease | [48] |
| 1879 | First vaccine developed for chicken cholera by Louis Pasteur | [49] |
| 1881 | First vaccine developed for anthrax by Louis Pasteur | [49] |
| 1882 | First vaccine developed for rabies by Louis Pasteur | [49] |
| 1882 | Koch discovers the Tuberculosis bacillus: Mycobacterium tuberculosis | [50] |
| 1890 | Emil von Behring discovers antitoxins and develops tetanus and diphtheria vaccines | [49] |
| 1892 | Dmitri Ivanovsky shows that sap from a diseased tobacco plant remained infectious to healthy tobacco plants despite having been filtered | [51] |
| 1894 | Isolation in culture and microscopic description of causative bacteria | [52,53] |
| 1896/1897 | Almroth Wright and Richard Pfeiffer develop the first vaccine for typhoid fever | [54] |
| 1897 | Waldemar Haffkine tests on himself the first vaccine developed for bubonic plague | [55] |
| 1897 | Paul Ehrlich develops a standardized unit of measure for diphtheria antitoxin that would play an important role in future developmental work on sera and vaccines | [56] |
| 1898 | Martinus Beijerinck is convinced that filtrate contains a new form of infectious agent called a virus | [57] |
| 1913 | Paul Ehrlich develops the first antimicrobial drug, “Salvarsan”, against the bacterium Treponema pallidum, the etiological agent of syphilis | [58] |
| 1918 | Charles Nicolle and Charles Lebailly advance the hypothesis that the causative agent of the “Spanish” flu is a nonfilterable agent of infinitesimal dimensions: possibly a virus | [59,60] |
| 1923 | First vaccine developed for diphtheria by Alexander Thomas Glenny | [49] |
| 1924 | First vaccine developed for tetanus (tetanus toxoid) by Alexander Thomas Glenny | [49] |
| 1914/1926 | First vaccine developed for whooping cough (pertussis) by Leila Denmark | [49] |
| 1927 | First vaccine developed for tuberculosis by Albert Calmette and Camille Guérin | [49] |
| 1928 | Sir Alexander Fleming discovers penicillin | [61] |
| 1931 | German engineers Ernst Ruska and Max Knoll project the electron microscope | [62] |
| 1931 | Live attenuated bacterial vaccine developed and tested | [63,64] |
| 1932 | Gerhard Domagk announces that the red dye prontosil is active against streptococcal infections in humans; afterward, Ernest Fourneau, Jacques and Thérèse Tréfouël, Daniel Bovet, and Fedrico Nitti show that the active antibacterial agent is sulfanilamide | [65] |
| 1935 | First vaccine developed for yellow fever by Max Theiler | [49] |
| 1937 | First vaccine developed for typhus by Rudolf Weigl | [49] |
| 1938 | Jonas Salk and Thomas Francis develop the first vaccine against flu viruses | [66] |
| 1940–1947 | Large concentrations of blood bacteria correlated with mortality | [67] |
| 1944 | Oswald Avery, Colin MacLeod, and Maclyn McCarty report that DNA is the transforming factor in the experiments of Frederick Griffith where an extract of the pathogenic strain of pneumococcus could transform a harmless strain into a pathogenic one | [68] |
| 1944 | Selman Waksman, Albert Schatz, and Elizabeth Bugie announce the discovery of streptomycin and state that it is active against Mycobacterium tuberculosis | [69] |
| 1949 | John Franklin Enders, Thomas Weller, and Frederick Robbins grow poliovirus for the first time in cultured human embryo cells | [70] |
| 1953 | James Watson and Francis Crick describe the structure of DNA | [71] |
| 1955 | Jonas Salk develops the first polio vaccine | [49] |
| 1964 | First vaccine developed for measles by John Franklin Enders | [49] |
| 1967 | Maurice Hilleman develops the first vaccine for mumps virus | [49] |
| 1970 | Maurice Hilleman develops the first vaccine for rubella | [49] |
| 1977 | First approved vaccine developed for pneumonia | [49] |
| 1978 | First approved vaccine developed for meningitis | [49] |
| 1980 | Genetic relatedness of Yersinia pestis and Yersinia pseudotuberculosis | [72] |
| 1981 | First approved vaccine developed for hepatitis B | [49] |
| 1983 | HIV, the virus that causes AIDS, is identified | [73] |
| 1987 | First approval of a drug against AIDS: zidovudine (AZT, ZDV) | [74] |
| 1992 | First approved vaccine developed for hepatitis A | [49] |
| 1995 | First vaccine developed for varicella (chickenpox) and hepatitis A | [49] |
| 1998 | First approved vaccine developed for rotavirus | [49] |
| 2001–2011 | DNA sequence of Yersinia pestis samples | [75] |
| 2006 | First vaccine developed for human papillomavirus and for herpes zoster (shingles) | [49] |
| 2019 | Food and Drug Administration (FDA) approves rVSVΔG-ZEBOV-GP Ebola vaccine | [76] |
| 2020 | First vaccine against COVID-19 | [77] |
| 2022 | First drugs for COVID-19 (molnupiravir and Paxlovid or nirmatrelvir + Paxlovid) | [78,79,80] |
3. Transmission and Measures to Contain SARS-CoV-2 Spread
- Physical distances > 1.5 m;
- Wearing masks and gloves;
- Stay-at-home orders;
- School and workplace closures and activation of distance learning and smart working;
- Closure of museums, commercial parks, gyms, and swimming pools;
- Cancellation of public events;
- Restrictions on size of crowds;
- Seat limitation on public transport to ensure the right distance between passengers;
- Restrictions on internal and international travel;
- Measurements of body temperature at the entrance of closed areas (<37.5 °C);
- Ensuring disinfection rules are followed in public areas such as public transport, shopping areas, schools, and universities;
- Protecting healthcare workers with appropriate personal protection equipment (PPE).
4. Boosting the Immune Response: How Vaccines Changed the Scenario
- (1)
- Speed up vaccine development;
- (2)
- Simplify vaccine production, scale-up, and quality control;
- (3)
- Be produced and scaled up in a predictable and consistent fashion regardless of the antigen;
- (4)
- Have improved safety and efficacy;
- (5)
- Challenge diseases impossible to prevent with other approaches;
- (6)
- Enable precise antigen design;
- (7)
- Generate proteins with a “native-like” presentation;
- (8)
- Express proteins stabilized in a more immunogenic conformation or expose key antigenic sites;
- (9)
- Deliver multiple mRNAs to the same cell;
- (10)
- Allow the generation of multiprotein complexes or protein antigens from different pathogens, thus creating a single vaccine against several targets.
- (11)
- Being noninfectious;
- (12)
- Being nonintegrating;
- (13)
- Being degradable by normal cellular processes soon after injection;
- (14)
- Decreasing the risk of toxicity and long-term side effects;
- (15)
- Not inducing vector-specific immunity;
- (16)
- Not competing with pre-existing or newly raised vector immunity that could interfere with subsequent vaccinations.
5. Conclusions
“And Darkness and Decay and the Red Death held illimitable dominion over all.”(“The Mask of the Red Death: A Fantasy” E. A. Poe, 1842)
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Yin, Y.; Wunderink, R.G. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 2018, 23, 130–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gandhi, V.R.; Shanmugasundaram, S. A Missed Case of Osteoid Osteoma of the Acetabulum Treated with a Novel Computed Tomography-Guided Technique—A Case Report. J. Orthop. Case Rep. 2020, 10, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Li, Y.; Xiao, S.Y. Differential expression of ACE2 in the respiratory tracts and its relationship to COVID-19 pathogenesis. EBioMedicine 2020, 60, 103004. [Google Scholar] [CrossRef] [PubMed]
- Costa, L.B.; Perez, L.G.; Palmeira, V.A.; Macedo e Cordeiro, T.; Ribeiro, V.T.; Lanza, K.; Simoes e Silva, A.C. Insights on SARS-CoV-2 Molecular Interactions with the Renin-Angiotensin System. Front. Cell Dev. Biol. 2020, 8, 559841. [Google Scholar] [CrossRef]
- Muus, C.; Luecken, M.D.; Eraslan, G.; Sikkema, L.; Waghray, A.; Heimberg, G.; Kobayashi, Y.; Vaishnav, E.D.; Subramanian, A.; Smillie, C.; et al. Single-cell meta-analysis of SARS-CoV-2 entry genes across tissues and demographics. Nat. Med. 2021, 27, 546–559. [Google Scholar] [CrossRef]
- Amenta, E.M.; Spallone, A.; Rodriguez-Barradas, M.C.; El Sahly, H.M.; Atmar, R.L.; Kulkarni, P.A. Postacute COVID-19: An Overview and Approach to Classification. Open Forum Infect. Dis. 2020, 7, ofaa509. [Google Scholar] [CrossRef]
- Wolfe, N.D.; Dunavan, C.P.; Diamond, J. Origins of major human infectious diseases. Nature 2007, 447, 279–283. [Google Scholar] [CrossRef]
- Rascovan, N.; Sjogren, K.G.; Kristiansen, K.; Nielsen, R.; Willerslev, E.; Desnues, C.; Rasmussen, S. Emergence and Spread of Basal Lineages of Yersinia pestis during the Neolithic Decline. Cell 2019, 176, 295–305.e10. [Google Scholar] [CrossRef] [Green Version]
- A History of ‘Plague’: Illness as Metaphor. Available online: https://www.merriam-webster.com/words-at-play/plague-word-history-literary-metaphor (accessed on 8 February 2022).
- Nunn, J.F. Ancient Egyptian Medicine; University of Oklahoma Press: Norman, OK, USA, 2002. [Google Scholar]
- Trevisanato, S.I. The ‘Hittite plague’, an epidemic of tularemia and the first record of biological warfare. Med. Hypotheses 2007, 69, 1371–1374. [Google Scholar] [CrossRef] [Green Version]
- Norrie, P. How Disease Affected the End of the Bronze Age. In A History of Disease in Ancient Times; Palgrave Macmillan: Cham, Switzerland, 2016. [Google Scholar] [CrossRef]
- Tsoucalas, G.; Laios, K.; Karamanou, M.; Androutsos, G. Demystifying the epidemic among Achaeans during the Trojan War. Infez. Med. 2014, 22, 342–348. [Google Scholar]
- Russell, J.C. That Earlier Plague; Duke University Press: Durham, NC, USA, 1968; Volume 5, p. 11. [Google Scholar]
- Kousoulis, A.A.; Economopoulos, K.P.; Poulakou-Rebelakou, E.; Androutsos, G.; Tsiodras, S. The plague of Thebes, a historical epidemic in Sophocles’ Oedipus Rex. Emerg. Infect. Dis. 2012, 18, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Littman, R.J. The plague of Athens: Epidemiology and paleopathology. Mt. Sinai J. Med. J. Transl. Pers. Med. 2009, 76, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Cunha, B.A. The cause of the plague of Athens: Plague, typhoid, typhus, smallpox, or measles? Infect. Dis. Clin. N. Am. 2004, 18, 29–43. [Google Scholar] [CrossRef]
- Dirckx, J.H. Pestilence narratives in classical literature: A study in creative imitation: II. Virgil, Ovid, Seneca, and Silius Italicus. Am. J. Dermatopathol. 2000, 22, 459–464. [Google Scholar] [CrossRef]
- Angeletti, L.R.; Gazzaniga, V. The plague of Syracuse (396 B.C.E.) in Diodorus Siculus (XIV, 70). Ann. Ig. Med. Prev. Comunita 2002, 14, 7–13. [Google Scholar]
- Fears, J.R. The plague under Marcus Aurelius and the decline and fall of the Roman Empire. Infect. Dis. Clin. N. Am. 2004, 18, 65–77. [Google Scholar] [CrossRef]
- Iniesta, I. Pandemics in ancient Greek and Roman coinage: Medical memories at the service of hope. Intern. Med. J. 2020, 50, 1574–1578. [Google Scholar] [CrossRef]
- Wagner, D.M.; Klunk, J.; Harbeck, M.; Devault, A.; Waglechner, N.; Sahl, J.W.; Enk, J.; Birdsell, D.N.; Kuch, M.; Lumibao, C.; et al. Yersinia pestis and the plague of Justinian 541–543 AD: A genomic analysis. Lancet Infect. Dis. 2014, 14, 319–326. [Google Scholar] [CrossRef]
- Ryan, J.J.; Klein, K.A.; Neuberger, T.J.; Leftwich, J.A.; Westin, E.H.; Kauma, S.; Fletcher, J.A.; DeVries, G.H.; Huff, T.F. Role for the stem cell factor/KIT complex in Schwann cell neoplasia and mast cell proliferation associated with neurofibromatosis. J. Neurosci. Res. 1994, 37, 415–432. [Google Scholar] [CrossRef]
- Wheelis, M. Biological warfare at the 1346 siege of Caffa. Emerg. Infect. Dis. 2002, 8, 971–975. [Google Scholar] [CrossRef]
- Bowsky, W.M. The impact of the black death upon Sienese government and society. Speculum 1964, 39, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Sgouridou, M. The figure of the doctor and the science of medicine through Boccaccio’s “Decameron”. Infez. Med. 2014, 22, 62–68. [Google Scholar] [PubMed]
- Giovanni Villani (Italian Historian). Available online: https://www.britannica.com/biography/Giovanni-Villani (accessed on 26 February 2022).
- Spyrou, M.A.; Keller, M.; Tukhbatova, R.I.; Scheib, C.L.; Nelson, E.A.; Andrades Valtuena, A.; Neumann, G.U.; Walker, D.; Alterauge, A.; Carty, N.; et al. Phylogeography of the second plague pandemic revealed through analysis of historical Yersinia pestis genomes. Nat. Commun. 2019, 10, 4470. [Google Scholar] [CrossRef]
- Freemon, F.R. Bubonic plague in the Book of Samuel. J. R. Soc. Med. 2005, 98, 436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sampath, S.; Khedr, A.; Qamar, S.; Tekin, A.; Singh, R.; Green, R.; Kashyap, R. Pandemics Throughout the History. Cureus 2021, 13, e18136. [Google Scholar] [CrossRef]
- A Visual History of Pandemics. Available online: https://www.weforum.org/agenda/2020/03/a-visual-history-of-pandemics (accessed on 26 February 2022).
- Papagrigorakis, M.J.; Yapijakis, C.; Synodinos, P.N.; Baziotopoulou-Valavani, E. DNA examination of ancient dental pulp incriminates typhoid fever as a probable cause of the Plague of Athens. Int. J. Infect. Dis. 2006, 10, 206–214. [Google Scholar] [CrossRef] [Green Version]
- Saez, A. The Antonine plague: A global pestilence in the II century d.C. Rev. Chil. Infectol. 2016, 33, 218–221. [Google Scholar] [CrossRef]
- Sabbatani, S.; Manfredi, R.; Fiorino, S. The Justinian plague (part one). Infez. Med. 2012, 20, 125–139. [Google Scholar]
- Stenseth, N.C.; Atshabar, B.B.; Begon, M.; Belmain, S.R.; Bertherat, E.; Carniel, E.; Gage, K.L.; Leirs, H.; Rahalison, L. Plague: Past, present, and future. PLoS Med. 2008, 5, e3. [Google Scholar] [CrossRef] [Green Version]
- Glatter, K.A.; Finkelman, P. History of the Plague: An Ancient Pandemic for the Age of COVID-19. Am. J. Med. 2021, 134, 176–181. [Google Scholar] [CrossRef]
- Haensch, S.; Bianucci, R.; Signoli, M.; Rajerison, M.; Schultz, M.; Kacki, S.; Vermunt, M.; Weston, D.A.; Hurst, D.; Achtman, M.; et al. Distinct clones of Yersinia pestis caused the black death. PLoS Pathog. 2010, 6, e1001134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bramanti, B.; Dean, K.R.; Walloe, L.; Chr. Stenseth, N. The Third Plague Pandemic in Europe. Proc. R. Soc. B 2019, 286, 20182429. [Google Scholar] [CrossRef] [PubMed]
- Spinney, L. Smallpox and other viruses plagued humans much earlier than suspected. Nature 2020, 584, 30–32. [Google Scholar] [CrossRef] [PubMed]
- Behbehani, A.M. The smallpox story: Life and death of an old disease. Microbiol. Rev. 1983, 47, 455–509. [Google Scholar] [CrossRef]
- Eyler, J.M. Smallpox in history: The birth, death, and impact of a dread disease. J. Lab. Clin. Med. 2003, 142, 216–220. [Google Scholar] [CrossRef]
- Becker, A.M. Smallpox in Washington’s Army: Strategic Implications of the Disease during the American Revolutionary War. J. Mil. Hist. 2004, 68, 381–430. [Google Scholar] [CrossRef]
- Lederberg, J. Infectious history. Science 2000, 288, 287–293. [Google Scholar] [CrossRef] [Green Version]
- Ferretti, J.; Kohler, W. History of Streptococcal Research. In Streptococcus pyogenes: Basic Biology to Clinical Manifestations; Ferretti, J.J., Stevens, D.L., Fischetti, V.A., Eds.; University of Oklahoma Health Sciences Center: Oklahoma City, OK, USA, 2016. [Google Scholar]
- Sanchez-Sampedro, L.; Perdiguero, B.; Mejias-Perez, E.; Garcia-Arriaza, J.; Di Pilato, M.; Esteban, M. The evolution of poxvirus vaccines. Viruses 2015, 7, 1726–1803. [Google Scholar] [CrossRef] [Green Version]
- Plotkin, S.A. Vaccination against measles in the 18th century. Clin. Pediatr. 1967, 6, 312–315. [Google Scholar] [CrossRef]
- Smith, K.A. Louis pasteur, the father of immunology? Front. Immunol. 2012, 3, 68. [Google Scholar] [CrossRef] [Green Version]
- Baxter, A.G. Louis Pasteur’s beer of revenge. Nat. Rev. Immunol. 2001, 1, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Hajj Hussein, I.; Chams, N.; Chams, S.; El Sayegh, S.; Badran, R.; Raad, M.; Gerges-Geagea, A.; Leone, A.; Jurjus, A. Vaccines Through Centuries: Major Cornerstones of Global Health. Front. Public Health 2015, 3, 269. [Google Scholar] [CrossRef] [PubMed]
- Migliori, G.B.; Loddenkemper, R.; Blasi, F.; Raviglione, M.C. 125 years after Robert Koch’s discovery of the tubercle bacillus: The new XDR-TB threat. Is “science” enough to tackle the epidemic? Eur. Respir. J. 2007, 29, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Bos, L. Beijerinck’s work on tobacco mosaic virus: Historical context and legacy. Philos. Trans. R. Soc. Lond. B Biol. Sci. 1999, 354, 675–685. [Google Scholar] [CrossRef] [Green Version]
- Solomon, T. Alexandre Yersin and the plague bacillus. J. Trop. Med. Hyg. 1995, 98, 209–212. [Google Scholar]
- Hawgood, B.J. Alexandre Yersin (1863–1943): Discoverer of the plague bacillus, explorer and agronomist. J. Med. Biogr. 2008, 16, 167–172. [Google Scholar] [CrossRef]
- Williamson, J.D.; Gould, K.G.; Brown, K. Richard Pfeiffer’s typhoid vaccine and Almroth Wright’s claim to priority. Vaccine 2021, 39, 2074–2079. [Google Scholar] [CrossRef]
- Hawgood, B.J. Waldemar Mordecai Haffkine, CIE (1860–1930): Prophylactic vaccination against cholera and bubonic plague in British India. J. Med. Biogr. 2007, 15, 9–19. [Google Scholar] [CrossRef]
- Browning, C.H. Emil Behring and Paul Ehrlich: Their contributions to science. Nature 1955, 175, 570–575. [Google Scholar] [CrossRef]
- Dimmock, N.J.; Easton, A.; Leppard, K. Introduction to Modern Virology, 7th ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2015. [Google Scholar]
- Gelpi, A.; Gilbertson, A.; Tucker, J.D. Magic bullet: Paul Ehrlich, Salvarsan and the birth of venereology. Sex. Transm. Infect. 2015, 91, 68–69. [Google Scholar] [CrossRef] [Green Version]
- Francis, T. Transmission of Influenza by a Filterable Virus. Science 1934, 80, 457–459. [Google Scholar] [CrossRef] [PubMed]
- Is Influenza Due To A Filtrable Virus? J. Am. Med. Assoc. 1918, 71, 2154–2155. [CrossRef]
- Bennett, J.W.; Chung, K.T. Alexander Fleming and the discovery of penicillin. Adv. Appl. Microbiol. 2001, 49, 163–184. [Google Scholar] [CrossRef] [PubMed]
- Freundlich, M.M. Origin of the Electron Microscope. Science 1963, 142, 185–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demeure, C.E. Chapter 10. Live Vaccines against Plague and Pseudotuberculosis; Carniel, E., Hinnebusch, B.J., Eds.; Caister Academic Press: Norfolk, UK, 2012. [Google Scholar]
- Coulanges, P. 50th anniversary of the EV antiplague vaccine (Girard and Robic). Bull. Soc. Pathol. Exot. Fil. 1983, 76, 114–120. [Google Scholar]
- Chung, K.T. Azo dyes and human health: A review. J. Environ. Sci. Health Part C 2016, 34, 233–261. [Google Scholar] [CrossRef]
- Barberis, I.; Martini, M.; Iavarone, F.; Orsi, A. Available influenza vaccines: Immunization strategies, history and new tools for fighting the disease. J. Prev. Med. Hyg. 2016, 57, E41–E46. [Google Scholar]
- Wagle, P.M. Recent advances in the treatment of bubonic plague. Ind. J. Med. Sci. 1948, 2, 489–494. [Google Scholar]
- Avery, O.T.; Macleod, C.M.; McCarty, M. Studies on the Chemical Nature of the Substance Inducing Transformation of Pneumococcal Types: Induction of Transformation by a Desoxyribonucleic Acid Fraction Isolated from Pneumococcus Type III. J. Exp. Med. 1944, 79, 137–158. [Google Scholar] [CrossRef]
- Schatz, A.; Bugie, E.; Waksman, S.A. Streptomycin, a substance exhibiting antibiotic activity against gram-positive and gram-negative bacteria. Proc. Soc. Exp. Biol. Med. 1944, 55, 66–69. [Google Scholar] [CrossRef]
- Rosen, F.S. Isolation of poliovirus—John Enders and the Nobel Prize. N. Engl. J. Med. 2004, 351, 1481–1483. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.D.; Crick, F.H. Molecular structure of nucleic acids: A structure for deoxyribose nucleic acid. Nature 1953, 171, 737–738. [Google Scholar] [CrossRef] [PubMed]
- Achtman, M.; Zurth, K.; Morelli, G.; Torrea, G.; Guiyoule, A.; Carniel, E. Yersinia pestis, the cause of plague, is a recently emerged clone of Yersinia pseudotuberculosis. Proc. Natl. Acad. Sci. USA 1999, 96, 14043–14048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barre-Sinoussi, F.; Ross, A.L.; Delfraissy, J.F. Past, present and future: 30 years of HIV research. Nat. Rev. Microbiol. 2013, 11, 877–883. [Google Scholar] [CrossRef]
- Maeda, K.; Das, D.; Kobayakawa, T.; Tamamura, H.; Takeuchi, H. Discovery and Development of Anti-HIV Therapeutic Agents: Progress Towards Improved HIV Medication. Curr. Top. Med. Chem. 2019, 19, 1621–1649. [Google Scholar] [CrossRef]
- Parkhill, J.; Wren, B.W.; Thomson, N.R.; Titball, R.W.; Holden, M.T.; Prentice, M.B.; Sebaihia, M.; James, K.D.; Churcher, C.; Mungall, K.L.; et al. Genome sequence of Yersinia pestis, the causative agent of plague. Nature 2001, 413, 523–527. [Google Scholar] [CrossRef] [Green Version]
- Malenfant, J.H.; Joyce, A.; Choi, M.J.; Cossaboom, C.M.; Whitesell, A.N.; Harcourt, B.H.; Atmar, R.L.; Villanueva, J.M.; Bell, B.P.; Hahn, C.; et al. Use of Ebola Vaccine: Expansion of Recommendations of the Advisory Committee on Immunization Practices To Include Two Additional Populations—United States, 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 290–292. [Google Scholar] [CrossRef]
- Lamb, Y.N. BNT162b2 mRNA COVID-19 Vaccine: First Approval. Drugs 2021, 81, 495–501. [Google Scholar] [CrossRef]
- Syed, Y.Y. Molnupiravir: First Approval. Drugs 2022, 82, 455–460. [Google Scholar] [CrossRef]
- Mahase, E. COVID-19: Pfizer’s paxlovid is 89% effective in patients at risk of serious illness, company reports. BMJ 2021, 375, n2713. [Google Scholar] [CrossRef]
- Lamb, Y.N. Nirmatrelvir Plus Ritonavir: First Approval. Drugs 2022, 19, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Zink, A.R.; Reischl, U.; Wolf, H.; Nerlich, A.G. Molecular analysis of ancient microbial infections. FEMS Microbiol. Lett. 2002, 213, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Donoghue, H.D. Paleomicrobiology of Human Tuberculosis. Microbiol. Spectr. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Donoghue, H.D. Insights into ancient leprosy and tuberculosis using metagenomics. Trends Microbiol. 2013, 21, 448–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brier, B. Infectious diseases in ancient Egypt. Infect. Dis. Clin. N. Am. 2004, 18, 17–27. [Google Scholar] [CrossRef]
- McNeill, W.H. Plagues and Peoples; Anchor Books Doubleday: New York, NY, USA, 1998. [Google Scholar]
- Diamond, J. Guns, Germs, and Steel: The Fates of Human Societies; W. W. Norton & Company Inc.: New York, NY, USA, 1999. [Google Scholar]
- Spyrou, M.A.; Bos, K.I.; Herbig, A.; Krause, J. Ancient pathogen genomics as an emerging tool for infectious disease research. Nat. Rev. Genet. 2019, 20, 323–340. [Google Scholar] [CrossRef]
- Andrades Valtuena, A.; Mittnik, A.; Key, F.M.; Haak, W.; Allmae, R.; Belinskij, A.; Daubaras, M.; Feldman, M.; Jankauskas, R.; Jankovic, I.; et al. The Stone Age Plague and Its Persistence in Eurasia. Curr. Biol. 2017, 27, 3683–3691.e8. [Google Scholar] [CrossRef] [Green Version]
- Neukamm, J.; Pfrengle, S.; Molak, M.; Seitz, A.; Francken, M.; Eppenberger, P.; Avanzi, C.; Reiter, E.; Urban, C.; Welte, B.; et al. 2000-year-old pathogen genomes reconstructed from metagenomic analysis of Egyptian mummified individuals. BMC Biol. 2020, 18, 108. [Google Scholar] [CrossRef]
- Lalremruata, A.; Ball, M.; Bianucci, R.; Welte, B.; Nerlich, A.G.; Kun, J.F.; Pusch, C.M. Molecular identification of falciparum malaria and human tuberculosis co-infections in mummies from the Fayum depression (Lower Egypt). PLoS ONE 2013, 8, e60307. [Google Scholar] [CrossRef] [Green Version]
- Nerlich, A.G.; Schraut, B.; Dittrich, S.; Jelinek, T.; Zink, A.R. Plasmodium falciparum in ancient Egypt. Emerg. Infect. Dis. 2008, 14, 1317–1319. [Google Scholar] [CrossRef]
- Zink, A.R.; Grabner, W.; Reischl, U.; Wolf, H.; Nerlich, A.G. Molecular study on human tuberculosis in three geographically distinct and time delineated populations from ancient Egypt. Epidemiol. Infect. 2003, 130, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Raele, D.A.; Panzarino, G.; Sarcinelli, G.; Cafiero, M.A.; Maria Tunzi, A.; Dellu, E. Genetic Evidence of the Black Death in the Abbey of San Leonardo (Apulia Region, Italy): Tracing the Cause of Death in Two Individuals Buried with Coins. Pathogens 2021, 10, 1354. [Google Scholar] [CrossRef] [PubMed]
- Bramanti, B.; Wu, Y.; Yang, R.; Cui, Y.; Stenseth, N.C. Assessing the origins of the European Plagues following the Black Death: A synthesis of genomic, historical, and ecological information. Proc. Natl. Acad. Sci. USA 2021, 118, e2101940118. [Google Scholar] [CrossRef]
- Guellil, M.; Kersten, O.; Namouchi, A.; Luciani, S.; Marota, I.; Arcini, C.A.; Iregren, E.; Lindemann, R.A.; Warfvinge, G.; Bakanidze, L.; et al. A genomic and historical synthesis of plague in 18th century Eurasia. Proc. Natl. Acad. Sci. USA 2020, 117, 28328–28335. [Google Scholar] [CrossRef] [PubMed]
- Bos, K.I.; Schuenemann, V.J.; Golding, G.B.; Burbano, H.A.; Waglechner, N.; Coombes, B.K.; McPhee, J.B.; DeWitte, S.N.; Meyer, M.; Schmedes, S.; et al. A draft genome of Yersinia pestis from victims of the Black Death. Nature 2011, 478, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Guellil, M.; Rinaldo, N.; Zedda, N.; Kersten, O.; Gonzalez Muro, X.; Stenseth, N.C.; Gualdi-Russo, E.; Bramanti, B. Bioarchaeological insights into the last plague of Imola (1630–1632). Sci. Rep. 2021, 11, 22253. [Google Scholar] [CrossRef]
- Fornaciari, G.; Marchetti, A. Intact Smallpox Virus Particles in an Italian Mummy of Sixteenth Century. Lancet 1986, 328, 625. [Google Scholar] [CrossRef]
- Duggan, A.T.; Perdomo, M.F.; Piombino-Mascali, D.; Marciniak, S.; Poinar, D.; Emery, M.V.; Buchmann, J.P.; Duchene, S.; Jankauskas, R.; Humphreys, M.; et al. 17th Century Variola Virus Reveals the Recent History of Smallpox. Curr. Biol. 2016, 26, 3407–3412. [Google Scholar] [CrossRef] [Green Version]
- Muhlemann, B.; Vinner, L.; Margaryan, A.; Wilhelmson, H.; de la Fuente Castro, C.; Allentoft, M.E.; de Barros Damgaard, P.; Hansen, A.J.; Holtsmark Nielsen, S.; Strand, L.M.; et al. Diverse variola virus (smallpox) strains were widespread in northern Europe in the Viking Age. Science 2020, 369, eaaw8977. [Google Scholar] [CrossRef]
- Johnson, N.P.; Mueller, J. Updating the accounts: Global mortality of the 1918–1920 “Spanish” influenza pandemic. Bull. Hist. Med. 2002, 76, 105–115. [Google Scholar] [CrossRef]
- Tumpey, T.M.; Basler, C.F.; Aguilar, P.V.; Zeng, H.; Solorzano, A.; Swayne, D.E.; Cox, N.J.; Katz, J.M.; Taubenberger, J.K.; Palese, P.; et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science 2005, 310, 77–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taubenberger, J.K.; Morens, D.M. 1918 Influenza: The mother of all pandemics. Emerg. Infect. Dis. 2006, 12, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Morens, D.M.; Taubenberger, J.K.; Fauci, A.S. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: Implications for pandemic influenza preparedness. J. Infect. Dis. 2008, 198, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Hatchett, R.J.; Mecher, C.E.; Lipsitch, M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc. Natl. Acad. Sci. USA 2007, 104, 7582–7587. [Google Scholar] [CrossRef] [Green Version]
- Merson, M.H.; O’Malley, J.; Serwadda, D.; Apisuk, C. The history and challenge of HIV prevention. Lancet 2008, 372, 475–488. [Google Scholar] [CrossRef]
- WHO. Available online: https://covid19.who.int/ (accessed on 6 February 2022).
- Reno, E.; Quan, N.G.; Franco-Paredes, C.; Chastain, D.B.; Chauhan, L.; Rodriguez-Morales, A.J.; Henao-Martinez, A.F. Prevention of yellow fever in travellers: An update. Lancet Infect. Dis. 2020, 20, e129–e137. [Google Scholar] [CrossRef]
- Chen, L.H.; Wilson, M.E. Yellow fever control: Current epidemiology and vaccination strategies. Trop. Dis. Travel Med. Vaccines 2020, 6, 1. [Google Scholar] [CrossRef]
- Otter, J.A.; Donskey, C.; Yezli, S.; Douthwaite, S.; Goldenberg, S.D.; Weber, D.J. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: The possible role of dry surface contamination. J. Hosp. Infect. 2016, 92, 235–250. [Google Scholar] [CrossRef] [Green Version]
- Zhang, C.Q.; Chung, P.K.; Liu, J.D.; Chan, D.K.C.; Hagger, M.S.; Hamilton, K. Health Beliefs of Wearing Facemasks for Influenza A/H1N1 Prevention: A Qualitative Investigation of Hong Kong Older Adults. Asia Pac. J. Public Health 2019, 31, 246–256. [Google Scholar] [CrossRef] [Green Version]
- Cauchemez, S.; Ferguson, N.M.; Wachtel, C.; Tegnell, A.; Saour, G.; Duncan, B.; Nicoll, A. Closure of schools during an influenza pandemic. Lancet Infect. Dis. 2009, 9, 473–481. [Google Scholar] [CrossRef]
- Delgado, R.; Simon, F. Transmission, Human Population, and Pathogenicity: The Ebola Case in Point. Microbiol. Spectr. 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Undurraga, E.A.; Carias, C.; Meltzer, M.I.; Kahn, E.B. Potential for broad-scale transmission of Ebola virus disease during the West Africa crisis: Lessons for the Global Health security agenda. Infect. Dis. Poverty 2017, 6, 159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, V.K.; Firmal, P.; Alam, A.; Ganguly, D.; Chattopadhyay, S. Overview of Immune Response During SARS-CoV-2 Infection: Lessons From the Past. Front. Immunol. 2020, 11, 1949. [Google Scholar] [CrossRef] [PubMed]
- Kampf, G.; Bruggemann, Y.; Kaba, H.E.J.; Steinmann, J.; Pfaender, S.; Scheithauer, S.; Steinmann, E. Potential sources, modes of transmission and effectiveness of prevention measures against SARS-CoV-2. J. Hosp. Infect. 2020, 106, 678–697. [Google Scholar] [CrossRef] [PubMed]
- International Outbreak of Novel SARS-CoV-2 Coronavirus Infection. Available online: https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-international-outbreak (accessed on 26 February 2022).
- Castaldi, S.; Romano, L.; Pariani, E.; Garbelli, C.; Biganzoli, E. COVID-19: The end of lockdown what next? Acta Biomed. 2020, 91, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Afari, F. A Brief International History of Pandemics. Available online: https://www.graduateinstitute.ch/communications/news/brief-international-history-pandemics (accessed on 26 February 2022).
- Grmek, M.D.; Buchet, C. The beginnings of maritime quarantine. In Man, Health and the Sea; Honoré Champion: Paris, France, 1997; pp. 39–60. (In French) [Google Scholar]
- Tognotti, E. Lessons from the history of quarantine, from plague to influenza A. Emerg. Infect. Dis. 2013, 19, 254–259. [Google Scholar] [CrossRef]
- Defoe, D. A Journal of the Plague Year. Int. J. Epidemiol. 2006, 35, 1066. [Google Scholar] [CrossRef]
- Bassareo, P.P.; Melis, M.R.; Marras, S.; Calcaterra, G. Learning from the past in the COVID-19 era: Rediscovery of quarantine, previous pandemics, origin of hospitals and national healthcare systems, and ethics in medicine. Postgrad. Med. J. 2020, 96, 633–638. [Google Scholar] [CrossRef]
- Gensini, G.F.; Yacoub, M.H.; Conti, A.A. The concept of quarantine in history: From plague to SARS. J. Infect. 2004, 49, 257–261. [Google Scholar] [CrossRef]
- Savona-Ventura, C. The Order of St Lazarus in the Kingdom of Jerusalem. J. Monast. Mil. Orders 2008, 1, 55–64. [Google Scholar]
- Sehdev, P.S. The origin of quarantine. Clin. Infect. Dis. 2002, 35, 1071–1072. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barquet, N.; Domingo, P. Smallpox: The triumph over the most terrible of the ministers of death. Ann. Intern. Med. 1997, 127, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Pead, P.J. Benjamin Jesty: New light in the dawn of vaccination. Lancet 2003, 362, 2104–2109. [Google Scholar] [CrossRef]
- Jenson, A.B.; Ghim, S.J.; Sundberg, J.P. An inquiry into the causes and effects of the variolae (or Cow-pox. 1798). Exp. Dermatol. 2016, 25, 178–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plotkin, S. History of vaccination. Proc. Natl. Acad. Sci. USA 2014, 111, 12283–12287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plotkin, S.A. Vaccines: Past, present and future. Nat. Med. 2005, 11, S5–S11. [Google Scholar] [CrossRef] [PubMed]
- Underhill, D.M.; Gordon, S.; Imhof, B.A.; Nunez, G.; Bousso, P. Elie Metchnikoff (1845–1916): Celebrating 100 years of cellular immunology and beyond. Nat. Rev. Immunol. 2016, 16, 651–656. [Google Scholar] [CrossRef]
- De Jesus, N.H. Epidemics to eradication: The modern history of poliomyelitis. Virol. J. 2007, 4, 70. [Google Scholar] [CrossRef] [Green Version]
- Sadarangani, M.; Marchant, A.; Kollmann, T.R. Immunological mechanisms of vaccine-induced protection against COVID-19 in humans. Nat. Rev. Immunol. 2021, 21, 475–484. [Google Scholar] [CrossRef]

| Years | Infectious Disease | Literary Documents | Origin | Possible Pathogen | Peer-Reviewed Source |
|---|---|---|---|---|---|
| 1500 BCE | Different diseases | Ebers Papyrus | Egipt | Unknown | [10] |
| 1335 BCE | Hittite plague | The Amarna Letter EA 96; The Amarna Letter EA 137; The Amarna Letter EA 224. | Mesopotamia via Canaanite harbors | Francisella tularensis | [11] |
| The story of the plague is handed down in literature in the Hittite plague prayers (KUB XIV 10 and KUB XXVI 86) | |||||
| 1190 or 1141 BCE | Plague of the Philistines, also known as the Plague of Ashdod | Bible, Book of Samuel according to 1 Samuel 5:9 | Ashdod (now Israel) | Y. pestis, Francisella tularensis, smallpox, or variola | [12] |
| 800–781 BCE | Plague of the Achaean soldiers’ camp | Homer’s Iliad Book 1:50–56 | Troy or Ilion located at Hisarlik in present-day Turkey | Equine encephalomyelitis? | [13] |
| 463 to 462 BCE | Rome when Lucius Aebutius and Publius Servilius were elected consuls | Quintus Livius Titus, popularly known as Livy, in his Early History of Rome | Rome, Italy | Unknown | [14] |
| 430–420 BCE | Plague of Thebes | Oedipus Rex by Sophocles (original Greek title Oιδίπους τύραννος) | Thebes, Greece | Leishmania spp., Leptospira spp., Brucella abortus, Orthopoxviridae, and Francisella tularensis in cattle. | [15] |
| Humans could have been affected by a different pathogen such as Salmonella enterica serovar Typhi | |||||
| 430–429 BCE | Plague of Athens | History of the Peloponnesian War by Thucydides | Ethiopia, then all the Mediterranean | Salmonella enterica serovar Typhi | [16,17] |
| 430–429 BCE | Plague of Athens | Titus Lucretius Carus 99–55 BCE De Rerum Natura with the Plague of Athens | Athens, Greece | Unknown | [18] |
| 433–432 BCE | Rome when Gaius Julius and Lucius Verginius were consuls | Quintus Livius Titus, popularly known as Livy, in his Early History of Rome Ab Urbe Condita 4.20–21, 4.25.3–4, and 4.30.8–10) | Rome, Italy | Anthrax? | [14] |
| 396 BCE | Plague at Syracuse | Punica by Tiberius Catius Asconius Silius Italicus | Syracuse, Italy | Typhoid or smallpox | [19] |
| Mythological plague | 70–19 BCE | Publius Vergilius Maro Third book of Georgics | Unknown | Unknown | [18] |
| Mythological plague | Plague at Aegina | Publius Ovidius Naso 43 BCE–18 CE Metamorphoses, Book 7 523–613 | Unknown | Unknown | [18] |
| Mythological plague | Lucius Annaeus Seneca Between 8 and 1 BCE–65 CE | Oedipus is a fabula crepidata (Roman tragic play with Greek subject) | Unknown | Unknown | [18] |
| 293 BCE | Plague of Rome | The construction of a hospital on Tiber Island in honor of Asclepius, the God of Medicine | Rome, Italy | Unknown | [14] |
| 165 CE, first wave | The Antonine Plague, Marcus Aurelius Antoninus (161–180 CE) | Plague of Galen, Methodus Medendi | Rome, Italy | Smallpox (Variola major and Variola minor) | [20,21] |
| 251–266 CE second wave | Cyprian Plague | Documented by Saint Cyprian, the Assyrian | Ethiopia | Small-pox | [21] |
| 541–543 CE and subsequent outbreaks 750–1000 CE | Justinian Plague Justinian I (r. 527–565 CE) | Symptoms described by Procopius of Cesarea (500–565 CE) in his History of the Wars, Book II, are very similar to those later reported during the second pandemic of the 14th to 17th centuries (the Black Death) | Pelusium, near Suez in Egypt | Y. pestis, distinct from the lineage that caused the second pandemic (including the Black Death) 800 years later in human populations | [22] |
| 590 CE | Roman Plague | The plague was described by the bishop and chronicler Gregory of Tours and later chronicler Paul the Deacon | Rome, Italy | Y. pestis | [14] |
| 1347–1351 | Black Death | China and Inner Asia | Y. pestis | ||
| Thomas Walsingham—Norfolk, 1422 | Thomas Walsingham “Towns once packed with people were emptied of their inhabitants, and the plague spread so thickly that the living were hardly able to bury the dead” | Y. pestis | [23] | ||
| Gabriele de Mussi (1280–1356) | Gabriele de Mussi Historia de Morbo | Y. pestis | [24] | ||
| Francesco Petrarch (1304–1374) | Francesco Petrarch chronicles the plague at Parma and bewails the magnitude of the destruction that seems to threaten the very existence of the human race | Y. pestis | [23] | ||
| Agnolo di Tura (14th century) | Agnolo di Tura, in his Crunica Senese, gives a shocking account of the raging plague in Siena | Y. pestis | [25] | ||
| Simon de Covino (1320–1367) | At Marseilles, the Black Death entered France, and Simon de Covino, the French poet–physician, describes the symptoms of the disease in Latin hexameter verse | Y. pestis | [25] | ||
| Giovanni Boccaccio 1313–1375 | Boccaccio acknowledges the Florentine plague of 1348 to be the prime mover of The Decameron, and in the introduction to that work he says “between March and the following July” | Y. pestis | [26] | ||
| Matteo Villani 1275–1363 | Matteo Villani attributes to the Black Death the social, moral, and political anarchy that were rampant in Florence in succeeding years | Y. pestis | [27] | ||
| The second plague pandemic, caused by Yersinia pestis, devastated Europe and the nearby regions between the 14th and 18th centuries 1360–1363; 1374; 1400; 1438–1439; 1456–1457; 1464–1466; 1481–1485; 1500–1503; 1518–1531; 1544–1548; 1563–1566; 1573–1588; 1596–1599; 1602–1611; 1623–1640; 1644–1654; 1664–1667; 1679 | Second outbreak of Black Death | Giovanni Baldinucci’s diary | Y. pestis | [28] | |
| Italian Plague of 1629–1631 or the Great Plague of Milan and the Great Plague of Seville (1647–1652), | Francesco Rondinelli | ||||
| the Great Plague of London (1665–1666), | Plague of Florence 1632–1633 | ||||
| and the Great Plague of Vienna (1679) | Alessandro Manzoni’s The Betrothed | ||||
| 1720–today | Third outbreak of Black Death. There is some controversy over the identity of the disease, but in its virulent form, it was responsible for the Great Plague of Marseille in 1720–1722, the Great Plague of 1738 (which hit Eastern Europe), and the Russian plague of 1770–1772 | Yunnan Province, Southwest China | Y. pestis | [23] |
| Time Frame of Disease Appearance | Archaeological Discovery and Pathogen Identification | Method of Retrieval | References |
|---|---|---|---|
| 4900 BCE | Different individuals at Fralsegarden in Gokhem parish, Falbygden, western Sweden. Identification of the presence of Y. pestis DNA | Genotyping of Y. pestis strain, phylogenetic and molecular clock analyses, heatmaps and functional classification of variants, and admixture analyses of human genomes | [8] |
| 4800 to 3700 | 563 tooth and bone samples from Russia, Hungary, Croatia, Lithuania, Estonia | Shotgun screening sequencing, in silico screening, deep shotgun sequencing, Y. pestis in-solution capture, genome reconstruction and authentication, individual sample treatment due to laboratory preparation and sequencing strategies, SNP calling, heterozygosity and phylogenetic analysis, dating analysis, SNP effect analysis, virulence factor analysis, and indel analysis | [88] |
| Latvia, and Germany. | |||
| Identification of the presence of extinct clade in the Y. pestis phylogeny | |||
| 3250 BCE to 700 CE | Different individuals from Abusir el-Meleq, located in Middle Egypt. | Metagenomic screening and SNP typing | [89] |
| Identification of Mycobacterium leprae strain and a 2000-year-old human hepatitis B virus | |||
| 3500 BCE to 300 CE | Mummies from Upper and Lower Egypt. | PCR amplification and sequencing | [90,91,92] |
| Identification of Falciparum malaria (Plasmodium Falciparum) and human tuberculosis (Mycobacterium tuberculosis) | |||
| 430 BCE | Dental pulp in Kerameikos mass burial of putative victims of the plague. | PCR amplification and sequencing | [32] |
| Identification of Salmonella enterica serovar Typhi | |||
| 541–543 CE | Radiocarbon dating of individuals to 533 AD (plus or minus 98 years) from the Aschheim-Bajuwarenring, Bavaria, Germany. | PCR amplification and sequencing reconstructed draft genomes of the infectious Y. pestis strains, comparing them with a database of genomes from 131 Y. pestis strains from the second and third pandemics, and constructing a maximum likelihood phylogenetic tree. | [22] |
| Identification of Y. pestis | |||
| 13th and beginning of the 14th century to 19th century | Different subjects from different places in Europe. Identification of Y. pestis | PCR and sequencing SNP calling and evaluation | [93,94,95,96] |
| 1630–1632 | Different subjects from Imola Northern Italy. Identification of Y. pestis | Genomic and metagenomic analysis of sequencing data | [97] |
| 16th century | Italian mummy from the 16th century. | Genomic and metagenomic analysis of sequencing data | [98] |
| Identification of intact smallpox virus particles | |||
| 1580–1630 VARV | Different subjects from Vilnius, Lithuania. | PCR and sequencing | [99,100] |
| Identification of smallpox |
| Pandemic | Years | Source | Main Actions | Current Prevention | References |
|---|---|---|---|---|---|
| Yellow fever | 1900 | Mosquito | Travel limitation in areas affected by yellow fever. Yellow fever control strategies include insecticide spraying, larval control including larvicide spraying, and bacterial toxins | Vaccine valid for 10 years | [108,109] |
| SARS-CoV | 2002–2004 | Bats, palm civets | During the viral incubation period (4–5 days), which is important for the prevention and control of the disease, there are no clinical symptoms | One of the treatment modalities used to reduce the replication of the virus and its spread is passive immunization with monoclonal antibodies | [110] |
| MERS-CoV | 2012 | Dromedary camels | Prevention includes washing hands often, cleaning surfaces regularly with an alcohol-based cleaner, | Interferons (IFNs). Different vaccines targeting SARS-CoV and MERS-CoV have been developed and tested in preclinical models. However, only a few of them have gone into clinical trials, and none of them have been approved by the FDA. | |
| covering mouth and nose with a tissue when coughing or sneezing | The different vaccines include protein subunit vaccines (RBD-based vaccine), virus-like particle vaccines, DNA vaccines, viral vector vaccines, inactivated vaccines, and live attenuated vaccines | ||||
| A/H1N1 | 2009 | Pigs | Reducing the risk of human-to-human transmission: isolation and quarantine of infected patients. Use of the surgical template. Hand hygiene is the most important measure to reduce the risk of transmission. Hands should be washed frequently with soap and water, alcohol-based cloths, or antiseptic. Cleaning of contaminated surfaces or equipment should be performed with phenolic disinfectants, ammonia compounds, or alcohol | Antiviral drugs, including adamantanes (amantadine, rimantadine) and neuraminidase inhibitors (zanamivir, oseltamivir, peramivir, and laninamivir) are used to treat cases of influenza, even if they have side effects; antibiotics for the treatment or prevention of secondary bacterial pneumonia; parenteral nutrition; oxygen therapy or ventilatory support and vasopressors for shock. Vaccines: for subjects between the ages of 3 and 77. The immunization schedule consisted of two vaccinations, 21 days apart | [111,112] |
| Ebola | 2013–2016 | Bats, NHPs, and small terrestrial mammals | Reducing the risk of wildlife-to-human: avoiding contact with infected fruit bats or monkeys/apes and the consumption of their raw meat. | Combination of three mono-clonal antibodies directed against the envelope glycoprotein (GP) of EBOV, liposomal-formulated interfering RNA, and inhibitors of RNA polymerase. | [113,114] |
| Reducing the risk of human-to-human transmission: avoiding direct or close contact with people with Ebola symptoms, particularly with their bodily fluids. Gloves and appropriate personal protective equipment should be worn when taking care of ill patients at home. Regular hand washing is required after visiting patients in hospital, as well as after taking care of patients at home | Two main vaccines have proved efficacious in preventing Ebola infection. Both vaccines express GP as the single EBOV component and are virally vectored in chimpanzee adenovirus and vesicular stomatitis virus (rVSV), respectively | ||||
| Outbreak containment measure: prompt and safe burial of the dead, identifying people who may have been in contact with someone infected with Ebola, monitoring the health of contacts for 21 days, the importance of separating the healthy from the sick to prevent further spread, the importance of good hygiene and maintaining a clean environment | |||||
| SARS-CoV-2 | 2019 | Probably from bats | Several practices are recommended with the aim to limit further transmission; they include handwashing, hand disinfection, wearing of face masks and gloves, disinfection of surfaces, and physical distance | Conservative fluid therapy and broad-spectrum antibiotics are given to patients as a protective measure to avoid opportunistic bacterial infections. However, ventilator support for respiration is provided to patients under extreme conditions. | [115,116] |
| Numerous FDA-approved antiviral drugs, plasma therapy, vaccines (live attenuated vaccine (LAV), inactivated virus, subunit vaccines, monoclonal antibody vaccine, virus vectors, protein vaccines, and DNA/RNA-based vaccines), and immunotherapies |
| Years | Source | Measurements | References |
|---|---|---|---|
| 430–428 BCE | Plague of Athens | The containment strategies used included the application of purifications and incantations and the enforcement of abstinence from baths and many food items then considered noxious to diseased people | [119] |
| 541–755 | Plague of Justinian | The containment strategies included unspecified traditional public health measures and quarantine | [119] |
| Giovanni Boccaccio (1313–1375), in his book The Decameron | Written in Tuscan vernacular (Italian). The book is a collection of short stories told by a group of seven young women and three young men sheltering in a villa just outside Florence to escape the black death that afflicted that city. Boccaccio probably conceived his masterpiece of classical Italian Renaissance prose after the plague epidemic of 1348, which came to a standstill by 1353 | ||
| 1377, 1397 | “De ordinibus contra eos qui veniunt de loc ispestiferis anno 1397 factis” | Quarantine was first introduced in Dubrovnik on Croatia’s Dalmatian Coast | [120] |
| Orders made against those who come to the place of the pestiferous in 1397 | The Great Council of Ragusa specified again the 30-day duration of quarantine and determined the place | ||
| 1423, 1448 | Venetian Senate | First permanent plague hospital (lazaretto) was opened by the Republic of Venice in 1423 on the small island of Santa Maria di Nazareth.Prolonged the waiting period to 40 days, thus giving birth to the term “quarantine” | [121] |
| 1467 | Genoa adopted the Venetian system | [119] | |
| 1476 | In Marseille, France, a hospital for persons with leprosy was converted into a lazaretto | [121] | |
| 1480 | Marsilio Ficino, “Consilio contro la pestilentia” | When you converse, stay away from your partner at least two arms, and in the open place, and when it is suspicious, let us stay at least six fathoms longer, and out in the open, and let the wind not be reversed by him | |
| 1589 | Viceroy of Peru | Lima physicians advised the use of quarantine among all native communities to prevent further spread of the disease | [119] |
| 1663 | English quarantine regulations provided for the confinement (in the Thames estuary) of ships with suspected plague-infected passengers or crew | [121] | |
| 1665 | A journal of the plague year by Daniel Defoe | It was a rule with those who had thus two houses in their keeping or care, that if anybody was taken sick in a family, before the master of the family let the examiners or any other officer know of it, he immediately would send all the rest of his family, whether children or servants, as it fell out to be, to such other house which he had so in charge, and then giving notice of the sick person to the examiner, have a nurse or nurses appointed, and have another person to be shut up in the house with them (which many for money would do), so to take charge of the house in case the person should die | [122] |
| 1688 and 1691 | Quarantine to control yellow fever which first appeared in New York and Boston | [121] | |
| 1796 | United States introduced quarantine legislation in port cities threatened by yellow fever from the West Indies | [123] | |
| 1799 | In the harbor of Philadelphia, the first quarantine station was built after a previous yellow fever outbreak in 1793 | [123] | |
| 1878 | Release of the National Quarantine Act, which shifted quarantine power from single states to the federal government | [123] | |
| 1944 | The federal government quarantine authority was set up | [123] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vitiello, L.; Ilari, S.; Sansone, L.; Belli, M.; Cristina, M.; Marcolongo, F.; Tomino, C.; Gatta, L.; Mollace, V.; Bonassi, S.; et al. Preventive Measures against Pandemics from the Beginning of Civilization to Nowadays—How Everything Has Remained the Same over the Millennia. J. Clin. Med. 2022, 11, 1960. https://doi.org/10.3390/jcm11071960
Vitiello L, Ilari S, Sansone L, Belli M, Cristina M, Marcolongo F, Tomino C, Gatta L, Mollace V, Bonassi S, et al. Preventive Measures against Pandemics from the Beginning of Civilization to Nowadays—How Everything Has Remained the Same over the Millennia. Journal of Clinical Medicine. 2022; 11(7):1960. https://doi.org/10.3390/jcm11071960
Chicago/Turabian StyleVitiello, Laura, Sara Ilari, Luigi Sansone, Manuel Belli, Mario Cristina, Federica Marcolongo, Carlo Tomino, Lucia Gatta, Vincenzo Mollace, Stefano Bonassi, and et al. 2022. "Preventive Measures against Pandemics from the Beginning of Civilization to Nowadays—How Everything Has Remained the Same over the Millennia" Journal of Clinical Medicine 11, no. 7: 1960. https://doi.org/10.3390/jcm11071960
APA StyleVitiello, L., Ilari, S., Sansone, L., Belli, M., Cristina, M., Marcolongo, F., Tomino, C., Gatta, L., Mollace, V., Bonassi, S., Muscoli, C., & Russo, P. (2022). Preventive Measures against Pandemics from the Beginning of Civilization to Nowadays—How Everything Has Remained the Same over the Millennia. Journal of Clinical Medicine, 11(7), 1960. https://doi.org/10.3390/jcm11071960










