Medium-Term Outcomes in COVID-19
Abstract
1. Introduction
2. Method and Materials
2.1. ECG Analysis
2.2. Statistical Analysis
3. Results
Mortality
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zheng, Y.-Y.; Ma, Y.-T.; Zhang, J.-Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus—Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, Z.; Leung, L.W.; Kontogiannis, C.; Zuberi, Z.; Bajpai, A.; Sharma, S.; Chen, Z.; Beeton, I.; Sohal, M.; Gallagher, M.M. Prevalence of bradyarrhythmias needing pacing in COVID-19. Pacing Clin. Electrophysiol. 2021, 44, 1340–1346. [Google Scholar] [CrossRef] [PubMed]
- Romero, J.; Alviz, I.; Parides, M.; Diaz, J.C.; Briceno, D.; Gabr, M.; Gamero, M.; Patel, K.; Braunstein, E.D.; Purkayastha, S.; et al. T-wave inversion as a manifestation of COVID-19 infection: A case series. J. Interv. Card. Electrophysiol. 2020, 59, 485–493. [Google Scholar] [CrossRef]
- Lanza, G.A.; De Vita, A.; Ravenna, S.E.; D’Aiello, A.; Covino, M.; Franceschi, F.; Crea, F. Electrocardiographic findings at presentation and clinical outcome in patients with SARS-CoV-2 infection. EP Eur. 2021, 23, 123–129. [Google Scholar] [CrossRef]
- Farré, N.; Mojón, D.; Llagostera, M.; Belarte-Tornero, L.C.; Calvo-Fernández, A.; Vallés, E.; Negrete, A.; García-Guimaraes, M.; Bartolomé, Y.; Fernández, C.; et al. Prolonged QT Interval in SARS-CoV-2 Infection: Prevalence and Prognosis. J. Clin. Med. 2020, 9, 2712. [Google Scholar] [CrossRef]
- Akhtar, Z.; Gallagher, M.M.; Yap, Y.G.; Leung, L.W.M.; Elbatran, A.I.; Madden, B.; Ewasiuk, V.; Gregory, L.; Breathnach, A.; Chen, Z.; et al. Prolonged QT predicts prognosis in COVID-19. Pacing Clin. Electrophysiol. 2021, 4, 875–882. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Yao, Q.; Gu, X.; Wang, Q.; Ren, L.; Wang, Y.; Hu, P.; Guo, L.; Liu, M.; Xu, J.; et al. 1-year outcomes in hospital survivors with COVID-19: A longitudinal cohort study. Lancet 2021, 398, 747–758. [Google Scholar] [CrossRef]
- Blomberg, B.; Mohn, K.G.-I.; Brokstad, K.A.; Zhou, F.; Linchausen, D.W.; Hansen, B.-A.; Lartey, S.; Onyango, T.B.; Kuwelker, K.; Sævik, M.; et al. Long COVID in a prospective cohort of home-isolated patients. Nat. Med. 2021, 27, 1607–1613. Available online: http://www.nature.com/articles/s41591-021-01433-3 (accessed on 28 August 2021). [CrossRef] [PubMed]
- Aranyó, J.; Bazan, V.; Lladós, G.; Dominguez, M.J.; Bisbal, F.; Massanella, M.; Sarrias, A.; Adeliño, R.; Riverola, A.; Paredes, R.; et al. Inappropriate sinus tachycardia in post-COVID-19 syndrome. Sci. Rep. 2022, 12 (Suppl. S3), euab116.114. [Google Scholar] [CrossRef]
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022, 28, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Okin, P.M.; Devereux, R.B.; Howard, B.V.; Fabsitz, R.R.; Lee, E.T.; Welty, T.K. Assessment of QT Interval and QT Dispersion for Prediction of All-Cause and Cardiovascular Mortality in American Indians: The Strong Heart Study. Circulation 2000, 101, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Camm, F.A.J.; Mb, M.Y.G.Y.; Malik, M. Measurement of the QT Interval and Repolarization Assessment. In Acquired Long QT Syndrome; Blackwell Publishing: Malden, MA, USA, 2004; pp. 24–59. Available online: https://onlinelibrary.wiley.com/doi/10.1002/9780470994771.ch3 (accessed on 13 September 2021).
- Rautaharju, P.M.; Surawicz, B.; Gettes, L.S. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram. J. Am. Coll. Cardiol. 2009, 53, 982–991. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Post, W.S.; Dalal, D.; Blasco-Colmenares, E.; Tomaselli, G.F.; Guallar, E. QT-interval duration and mortality rate: Results from the Third National Health and Nutrition Examination Survey. Arch. Intern. Med. 2011, 171, 1727–1733. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, X.-J.; Barywani, S.B.; Hansson, P.-O.; Thunström, E.; Rosengren, A.; Ergatoudes, C.; Mandalenakis, Z.; Caidahl, K.; Fu, M.L. Impact of changes in heart rate with age on all-cause death and cardiovascular events in 50-year-old men from the general population. Open Heart 2019, 6, e000856. [Google Scholar] [CrossRef] [PubMed]
- Heusch, G. A BEAUTIFUL lesson—Ivabradine protects from ischaemia, but not from heart failure: Through heart rate reduction or more? Eur. Heart J. 2009, 30, 2300–2301. [Google Scholar] [CrossRef][Green Version]
- Gautam, N.; Madathil, S.; Tahani, N.; Bolton, S.; Parekh, D.; Stockley, J.; Goyal, S.; Qureshi, H.; Yasmin, S.; Cooper, B.G.; et al. Medium-Term Outcomes in Severely to Critically Ill Patients with Severe Acute Respiratory Syndrome Coronavirus 2 Infection. Clin. Infect. Dis. 2021, 74, 301–308. [Google Scholar] [CrossRef]
- Ayoubkhani, D.; Khunti, K.; Nafilyan, V.; Maddox, T.; Humberstone, B.; Diamond, I.; Banerjee, A. Post-covid syndrome in individuals admitted to hospital with covid-19: Retrospective cohort study. BMJ 2021, 372, n693. [Google Scholar] [CrossRef]
- Navvas, J.; Varghese, R.; Selvakannan, B.; Narayan, Y.; Newman, O.; Butt, M.; Ragatha, R.; Freer, C.; Kuckreja, S.; Naik, S.; et al. P178 COVID-19 post-discharge mortality rate in a London district general hospital. In The Clinical Experiences of Post-COVID-19 Recovery; [Internet]; BMJ Publishing Group Ltd: London, UK; British Thoracic Society: London, UK, 2021; pp. A186.2–A187. Available online: https://thorax.bmj.com/lookup/doi/10.1136/thorax-2020-BTSabstracts.323 (accessed on 14 September 2021).
- Foy, B.H.; Carlson, J.C.T.; Reinertsen, E.; Padros IValls, R.; Pallares Lopez, R.; Palanques-Tost, E.; Mow, C.; Westover, M.B.; Aguirre, A.D.; Higgins, J.M.; et al. Association of Red Blood Cell Distribution Width with Mortality Risk in Hospitalized Adults With SARS-CoV-2 Infection. JAMA Netw Open. 2020, 3, e2022058. [Google Scholar] [CrossRef]
- Huang, J.; Cheng, A.; Kumar, R.; Fang, Y.; Chen, G.; Zhu, Y.; Lin, S. Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity. J. Med. Virol. 2020, 92, 2152–2158. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Dubois, M.-J.; Navickis, R.J.; Wilkes, M.M. Hypoalbuminemia in acute illness: Is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann. Surg. 2003, 237, 319–334. [Google Scholar] [CrossRef] [PubMed]
- Soni, M.; Gopalakrishnan, R. Significance of RDW in predicting mortality in COVID-19—An analysis of 622 cases. Int. J. Lab. Hematol. 2021. Epub ahead of print. Available online: https://onlinelibrary.wiley.com/doi/10.1111/ijlh.13526 (accessed on 7 September 2021).
- Paris, S.; Inciardi, R.M.; Lombardi, C.M.; Tomasoni, D.; Ameri, P.; Carubelli, V.; Agostoni, P.; Canale, C.; Carugo, S.; Danzi, G.; et al. Implications of atrial fibrillation on the clinical course and outcomes of hospitalized COVID-19 patients: Results of the Cardio-COVID-Italy multicentre study. Europace 2021, 23, 1603–1611. [Google Scholar] [CrossRef]
- Li, J.; Mazzone, P.; Leung, L.W.M.; Lin, W.; D’Angelo, G.; Ma, J.; Li, J.; Akhtar, Z.; Li, Y.; Della Bella, P.; et al. Electrophysiology in the time of coronavirus: Coping with the great wave. Europace 2020, 22, 1841–1847. [Google Scholar] [CrossRef] [PubMed]
- Rattanawong, P.; Shen, W.; El Masry, H.; Sorajja, D.; Srivathsan, K.; Valverde, A.; Scott, L.R. Guidance on Short-Term Management of Atrial Fibrillation in Coronavirus Disease 2019. J. Am. Heart Assoc. 2020, 9, e017529. [Google Scholar] [CrossRef] [PubMed]
- Spini, A.; Giudice, V.; Brancaleone, V.; Morgese, M.G.; De Francia, S.; Filippelli, A.; Ruggieri, A.; Ziche, M.; Ortona, E.; Cignarella, A.; et al. Sex-tailored pharmacology and COVID-19: Next steps towards appropriateness and health equity. Pharmacol. Res. 2021, 173, 105848. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Chinn, J.; De Ferrante, M.; Kirby, K.A.; Hohmann, S.F.; Amin, A. Male gender is a predictor of higher mortality in hospitalized adults with COVID-19. PLoS ONE 2021, 16, e0254066. [Google Scholar] [CrossRef]


| COVID Admission | |
|---|---|
| N= | 159 |
| Age (years) | 70.5 ± 16.5 |
| Male | 94 (59.1%) |
| ITU admission (patients) | 10 (6.3%) |
| Hospital stay (days) | 8.85 ± 7.9 |
| Diabetes | 44 (27.7%) |
| Hypertension | 94 (59.1%) |
| Ischaemic heart disease | 17 (10.7%) |
| Cancer | 21 (13.2%) |
| Dementia | 17 (10.7%) |
| Chronic kidney disease | 23 (14.5%) |
| Left ventricle ejection fraction (%) | 55.5 ± 6.5 |
| Haemoglobin (g/L) | 117.7 ± 20.7 |
| Red cell distribution width (%) | 13.9 ± 1.5 |
| Albumin (g/L) | 36.6 ± 5.1 |
| C-reactive protein (mg/L) | 143.2 ± 101 |
| Troponin (ng/L) | 413.4 ± 2815 |
| Pre-COVID admission QTc (ms) | 435.25 ± 25.6 |
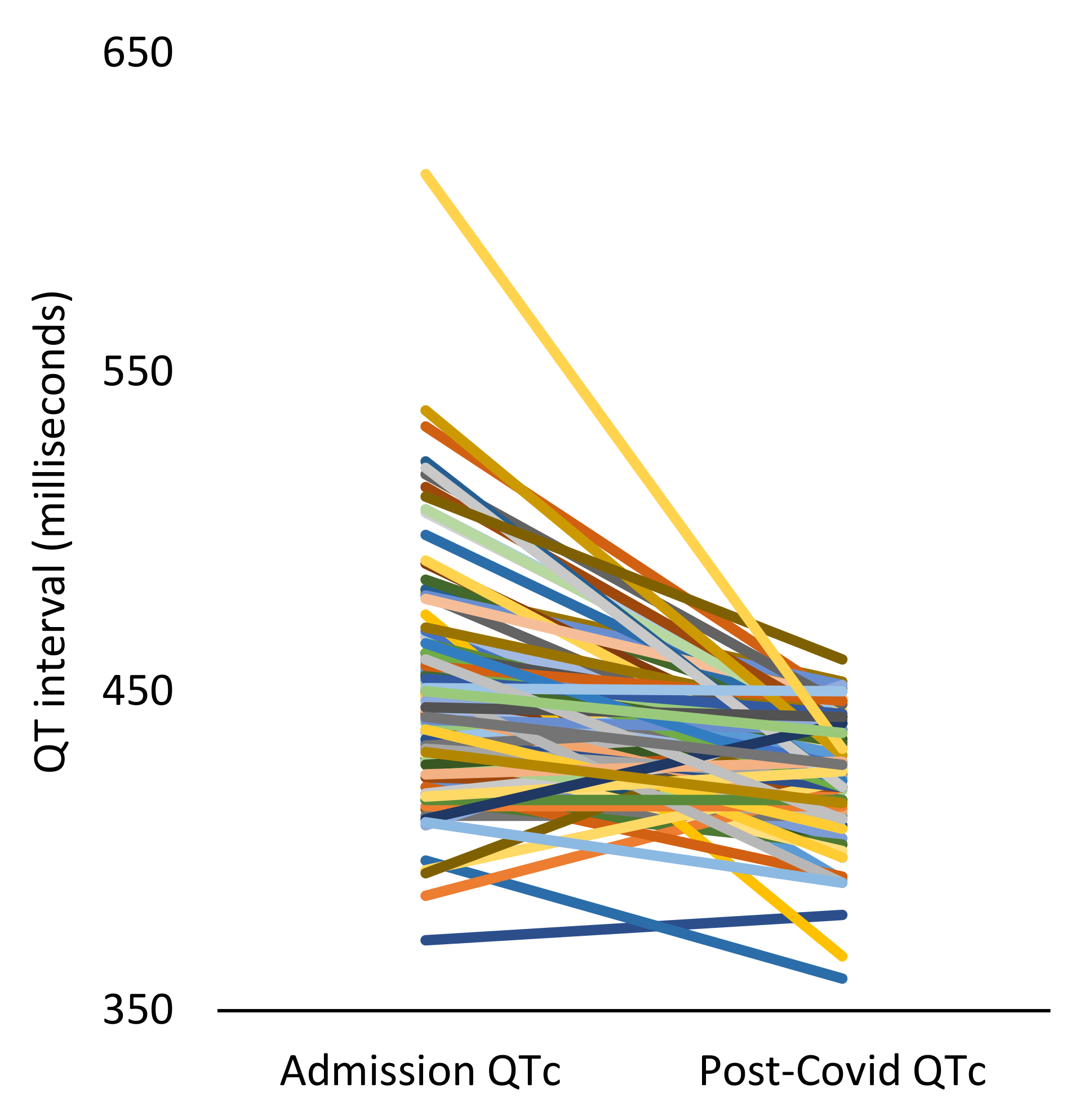
| QTc on COVID admission (ms) | 449.1 ± 33.8 |
| R-R interval on COVID admission (ms) | 696.4 + 136.5 |
| Post-COVID: | |
| Long COVID | 57 (35.8%) |
| Repeat admissions (patients) | 59 (37.1%) |
| New atrial fibrillation in the 1-year follow-up | 25 (15.7%) |
| 1-year mortality | 28 (17.6%) |
| Follow-up to death from admission (days) | 230.6 ± 154.3 |
| Post-COVID QTc (ms) | 425.7 ± 18.2 |
| R-R interval post-COVID (ms) | 811.1 ± 158.9 |
| Alive | Deceased | p-Value | |
|---|---|---|---|
| N= | 131 | 28 | |
| Age (years) | 68 ± 16 | 83 ± 10.7 | <0.001 |
| Female gender | 52 (39.6) | 13 (46.4) | 0.679 |
| COVID ITU admission | 10 (7.6) | 0 (0) | 0.136 |
| COVID hospital stay (days) | 8.9 ± 7.83 | 8.4 ± 8.4 | 0.75 |
| Number of repeat admissions | 0 (0–1) | 2 (0–2) | 0.064 |
| Long COVID (n = 133) | 51 (42.5) | 6 (46.2) | 0.8 |
| New atrial fibrillation | 16 (12.2) | 9 (32.1) | 0.006 |
| Diabetes | 33 (25.2) | 11 (39.2) | 0.096 |
| Hypertension | 78 (59.5) | 16 (57.1) | 0.68 |
| Ischaemic heart disease | 15 (11.5) | 2 (7.1) | 0.544 |
| Cancer | 18 (13.7) | 3 (10.7) | 0.724 |
| Dementia | 12 (9.2) | 5 (17.9) | 0.45 |
| Chronic kidney disease | 16 (12.2) | 7 (25) | 0.21 |
| Left ventricle ejection fraction (%) | 55.9 | 52.3 | 0.33 |
| Lab values: | |||
| Troponin (ng/L) | 581.3 ± 3359.3 | 51.3 ± 79.6 | 0.014 |
| Haemoglobin (g/L) | 118.1 ± 20.1 | 116.4 ± 23.2 | 0.7 |
| Red cell distribution width (%) | 13.8 ± 1.4 | 14.6 ± 1.8 | 0.012 |
| Albumin (g/L) | 37.1 ± 4.9 | 34.1 ± 5.4 | 0.02 |
| C-reactive protein (mg/L) | 146.9 ± 102.5 | 121.9 ± 94.6 | 0.2 |
| ECG: | |||
| QTc pre-admission (ms) | 434.4 ± 25.4 | 439 ± 27.6 | 0.48 |
| QTc on admission (ms) | 449.1 ± 34 | 449.6 ± 27 | 0.93 |
| QTc post-COVID (ms) | 425.7 ±18.2 | 428.9 ± 18.5 | 0.54 |
| Post-COVID QRS duration (ms) | 96.5 ± 18.9 | 94.8 ± 19.8 | 0.75 |
| R-R interval on COVID admission (ms) | 691.1 ± 142.3 | 717.7 ± 190.5 | 0.5 |
| Post-COVID R-R interval (ms) | 818.9 ± 169.3 | 761.1 ± 61.2 | 0.02 |
| QTc change during follow-up (ms) | −26.01 ± 33.5 | −20.6 ± 30.04 | 0.5 |
| Odds Ratio | 95% Confidence Interval | p-Value | |
|---|---|---|---|
| Univariate Analysis | |||
| Age | 1.075 | 1.04–1.113 | <0.001 |
| Diabetes | 1.78 | 0.832–3.8 | 0.137 |
| Chronic kidney disease | 2.09 | 0.89–4.92 | 0.091 |
| Red cell distribution width | 1.29 | 1.091–1.525 | 0.003 |
| Albumin on discharge | 0.897 | 0.827–0.973 | 0.008 |
| C-reactive protein | 0.997 | 0.994–1.001 | 0.2 |
| Post-COVID QTc | 1.02 | 0.991–1.05 | 0.19 |
| Post-COVID R-R interval | 0.995 | 0.993–0.998 | 0.002 |
| Multivariate Cox regression analysis | |||
| Hazard Ratio | 95% Confidence Interval | p-Value | |
| Age | 1.098 | 1.045–1.153 | <0.01 |
| Diabetes | 3.972 | 1.47–10.8 | <0.01 |
| Post-COVID R-R interval | 0.993 | 0.989–0.996 | 0.007 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akhtar, Z.; Sharma, S.; Elbatran, A.I.; Leung, L.W.M.; Kontogiannis, C.; Spartalis, M.; Roberts, A.; Bajpai, A.; Zuberi, Z.; Gallagher, M.M. Medium-Term Outcomes in COVID-19. J. Clin. Med. 2022, 11, 2033. https://doi.org/10.3390/jcm11072033
Akhtar Z, Sharma S, Elbatran AI, Leung LWM, Kontogiannis C, Spartalis M, Roberts A, Bajpai A, Zuberi Z, Gallagher MM. Medium-Term Outcomes in COVID-19. Journal of Clinical Medicine. 2022; 11(7):2033. https://doi.org/10.3390/jcm11072033
Chicago/Turabian StyleAkhtar, Zaki, Sumeet Sharma, Ahmed I. Elbatran, Lisa W. M. Leung, Christos Kontogiannis, Michael Spartalis, Alice Roberts, Abhay Bajpai, Zia Zuberi, and Mark M. Gallagher. 2022. "Medium-Term Outcomes in COVID-19" Journal of Clinical Medicine 11, no. 7: 2033. https://doi.org/10.3390/jcm11072033
APA StyleAkhtar, Z., Sharma, S., Elbatran, A. I., Leung, L. W. M., Kontogiannis, C., Spartalis, M., Roberts, A., Bajpai, A., Zuberi, Z., & Gallagher, M. M. (2022). Medium-Term Outcomes in COVID-19. Journal of Clinical Medicine, 11(7), 2033. https://doi.org/10.3390/jcm11072033







