Ambulatory Care in Adult Congenital Heart Disease—Time for Change?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Outpatient Appointments
2.3. Cost to the Patient
2.4. COVID-19
2.5. Patient Public Involvement
2.6. Statistical Analysis
3. Results
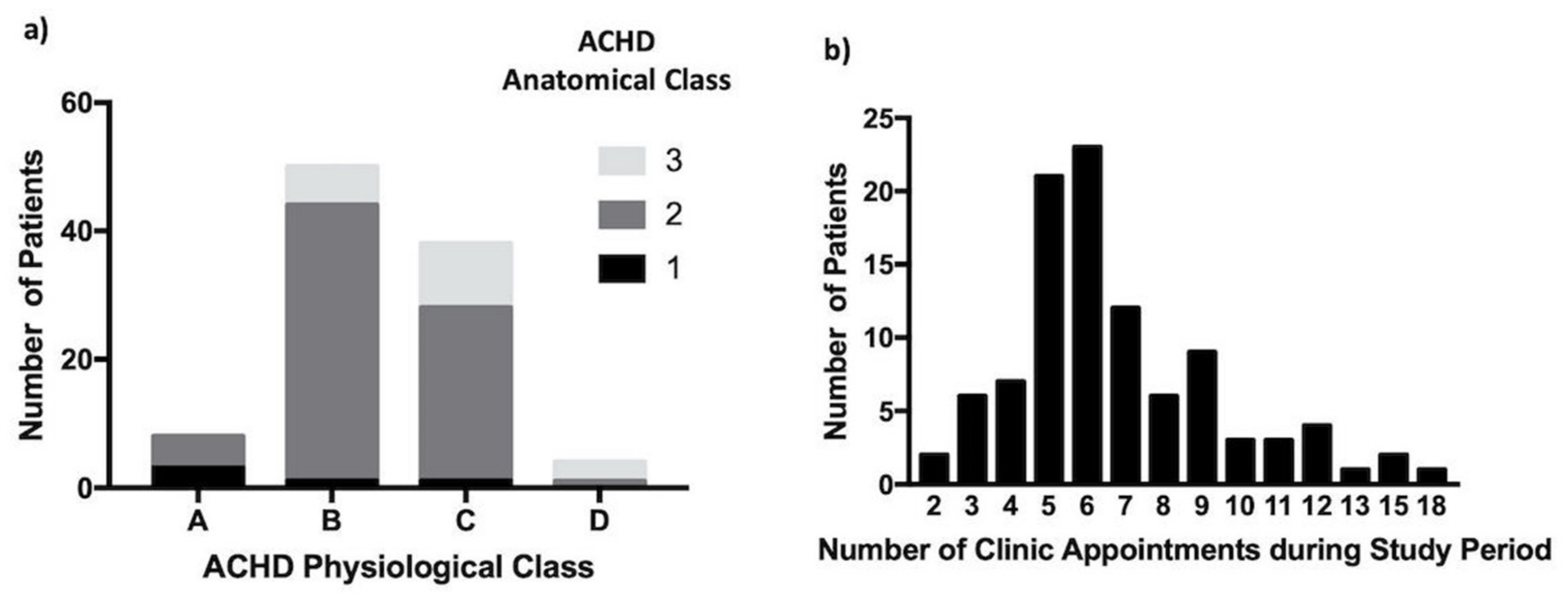
3.1. Study Population (n = 100)
3.2. Attendance at Clinic
3.3. The Outpatient Clinic Visit (n = 575)
3.4. Cost of the ACHD Clinic
3.5. COVID-19 Pandemic
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van der Bom, T.; Bouma, B.J.; Meijboom, F.J.; Zwinderman, A.H.; Mulder, B.J.M. The prevalence of adult congenital heart disease, results from a systematic review and evidence based calculation. Am. Heart J. 2012, 164, 568–575. [Google Scholar] [CrossRef] [PubMed]
- Benziger, C.P.; Stout, K.; Zaragoza-Macias, E.; Bertozzi-Villa, A.; Flaxman, A.D. Projected growth of the adult congenital heart disease population in the United States to 2050: An integrative systems modeling approach. Popul. Health Metr. 2015, 13, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desai, R.; Patel, K.; Dave, H.; Shah, K.; DeWitt, N.; Fong, H.K.; Varma, Y.; Varma, K.; Mansuri, Z.; Sachdeva, R.; et al. Nationwide Frequency, Sequential Trends, and Impact of Co-morbid Mental Health Disorders on Hospitalizations, Outcomes, and Healthcare Resource Utilization in Adult Congenital Heart Disease. Am. J. Cardiol. 2020, 125, 1256–1262. [Google Scholar] [CrossRef] [PubMed]
- Karsenty, C.; Zhao, A.; Marijon, E.; Ladouceur, M. Risk of thromboembolic complications in adult congenital heart disease: A literature review. Arch. Cardiovasc. Dis. 2018, 111, 613–620. [Google Scholar] [CrossRef]
- Reiter, F.P.; Hadjamu, N.J.; Nagdyman, N.; Zachoval, R.; Mayerle, J.; de Toni, E.N.; Kaemmerer, H.; Denk, G. Congenital heart disease-associated liver disease: A narrative review. Cardiovasc. Diagn. Ther. 2021, 11, 577. [Google Scholar] [CrossRef]
- Agarwal, A.; Vittinghoff, E.; Myers, J.J.; Dudley, R.A.; Khan, A.; John, A.; Marcus, G.M. Ambulatory Health Care Service Use and Costs among Commercially Insured US Adults with Congenital Heart Disease. JAMA Netw. Open 2020, 3, e2018752. [Google Scholar] [CrossRef]
- Willems, R.; Werbrouck, A.; de Backer, J.; Annemans, L. Real-world healthcare utilization in adult congenital heart disease: A systematic review of trends and ratios. Cardiol. Young 2019, 29, 553–563. [Google Scholar] [CrossRef]
- Kempny, A.; Diller, G.P.; Dimopoulos, K.; Alonso-Gonzalez, R.; Uebing, A.; Li, W.; Babu-Narayan, S.; Swan, L.; Wort, S.J.; Gatzoulis, M.A. Determinants of outpatient clinic attendance amongst adults with congenital heart disease and outcome. Int. J. Cardiol. 2016, 203, 245–250. [Google Scholar] [CrossRef]
- Wray, J.; Frigiola, A.; Bull, C. Loss to specialist follow-up in congenital heart disease; Out of sight, out of mind. Heart 2013, 99, 485–490. [Google Scholar] [CrossRef] [Green Version]
- Neidenbach, R.; Achenbach, S.; Andonian, C.; Bauer, U.M.; Ewert, P.; Freilinger, S.; Gundlach, U.; Kaemmerer, A.S.; Nagdyman, N.; Nebel, K.; et al. Systematic assessment of health care perception in adults with congenital heart disease in Germany. Cardiovasc. Diagn. Ther. 2021, 11, 481. [Google Scholar] [CrossRef]
- Royal College of Physicians. Outpatients: The Future, Adding Value through Sustainability; RCP: London, UK, 2018. [Google Scholar]
- Office of National Statististics. The English Indices of Deprivation 2019. 2019. Available online: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed on 7 March 2022).
- Stout, K.K.; Daniels, C.J.; Aboulhosn, J.A.; Bozkurt, B.; Broberg, C.S.; Colman, J.M.; Crumb, S.R.; Dearani, J.A.; Fuller, S.; Gurvitz, M.; et al. 2018 AHA/ACC Guideline for the Management of Adults with Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e81–e192. [Google Scholar]
- Diller, G.P.; Kempny, A.; Alonso-Gonzalez, R.; Swan, L.; Uebing, A.; Li, W.; Babu-Narayan, S.; Wort, S.J.; Dimopoulos, K.; Gatzoulis, M.A. Survival Prospects and Circumstances of Death in Contemporary Adult Congenital Heart Disease Patients under Follow-Up at a Large Tertiary Centre. Circulation 2015, 132, 2118–2125. [Google Scholar] [CrossRef] [Green Version]
- Google. Google Maps. Available online: https://www.google.co.uk/maps (accessed on 1 November 2021).
- Awh, K.; Venuti, M.A.; Gleason, L.P.; Rogers, R.; Denduluri, S.; Kim, Y.Y. Clinic nonattendance is associated with increased emergency department visits in adults with congenital heart disease. Congenit. Heart Dis. 2019, 14, 726–734. [Google Scholar] [CrossRef]
- Lyon, J.E. Adults with Congenital Heart Disease: The Patients’ Perspective. Ph.D. Thesis, Bournemouth University, Poole, UK, 2006. [Google Scholar]
- Moons, P.; Skogby, S.; Bratt, E.L.; Zühlke, L.; Marelli, A.; Goossens, E. Discontinuity of cardiac follow-up in young people with congenital heart disease transitioning to adulthood: A systematic review and meta-analysis. J. Am. Heart Assoc. 2021, 10, e019552. [Google Scholar] [CrossRef]
- Goossens, E.; van Deyk, K.; Budts, W.; Moons, P. Are missed appointments in an outpatient clinic for adults with congenital heart disease the harbinger for care gaps? Eur. J. Cardiovasc. Nurs. 2021, 21, 127–134. [Google Scholar] [CrossRef]
- Baumgartner, H.; de Backer, J. The ESC clinical practice guidelines for the management of adult congenital heart disease 2020. Eur. Heart J. 2020, 14, 4153–4154. [Google Scholar] [CrossRef]
- Marelli, A. Trajectories of care in congenital heart disease—The long arm of disease in the womb. J. Intern. Med. 2020, 288, 390–399. [Google Scholar] [CrossRef]
- Davey, B.; Sinha, R.; Lee, J.H.; Gauthier, M.; Flores, G. Social determinants of health and outcomes for children and adults with congenital heart disease: A systematic review. Pediatr. Res. 2021, 89, 275–294. [Google Scholar] [CrossRef]
- World Health Organization. Integrated Care Models: An Overview; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Davy, C.; Bleasel, J.; Liu, H.; Tchan, M.; Ponniah, S.; Brown, A. Effectiveness of chronic care models: Opportunities for improving healthcare practice and health outcomes: A systematic review. BMC Health Serv. Res. 2015, 15, 194. [Google Scholar] [CrossRef] [Green Version]
- Koole, M.A.C.; Kauw, D.; Winter, M.M.; Dohmen, D.A.J.; Tulevski, I.I.; de Haan, R.; Somsen, G.A.; Schijven, M.P.; Robbers-Visser, D.; Mulder, B.J.M.; et al. First real-world experience with mobile health telemonitoring in adult patients with congenital heart disease. Neth. Heart J. 2019, 27, 30–37. [Google Scholar] [CrossRef] [Green Version]
- Baggen, V.J.; Baart, S.J.; van den Bosch, A.E.; Eindhoven, J.A.; Witsenburg, M.; Cuypers, J.A.; Roos-Hesselink, J.W.; Boersma, E. Prognostic value of serial N-terminal pro-B-type natriuretic peptide measurements in adults with congenital heart disease. J. Am. Heart Assoc. 2018, 7, e008349. [Google Scholar] [CrossRef]
- Kauw, D.; Koole, M.A.; Winter, M.M.; Dohmen, D.A.; Tulevski, I.I.; Blok, S.; Somsen, G.A.; Schijven, M.P.; Vriend, J.W.; Robbers-Visser, D.; et al. Advantages of mobile health in the management of adult patients with congenital heart disease. Int. J. Med. Inform. 2019, 132, 104011. [Google Scholar] [CrossRef]
- Singhal, A.; Cowie, M.R. The Role of Wearables in Heart Failure. Curr. Heart Fail. Rep. 2020, 17, 125–132. [Google Scholar] [CrossRef]
- McManus, R.J.; Little, P.; Stuart, B.; Morton, K.; Raftery, J.; Kelly, J.; Bradbury, K.; Zhang, J.; Zhu, S.; Murray, E.; et al. Home and Online Management and Evaluation of Blood Pressure (HOME BP) using a digital intervention in poorly controlled hypertension: Randomised controlled trial. BMJ 2021, 372, m4858. [Google Scholar] [CrossRef]
- Diller, G.P.; Orwat, S.; Lammers, A.E.; Radke, R.M.; De-Torres-Alba, F.; Schmidt, R.; Marschall, U.; Bauer, U.M.; Enders, D.; Bronstein, L.; et al. Lack of specialist care is associated with increased morbidity and mortality in adult congenital heart disease: A population-based study. Eur. Heart J. 2021, 42, 4241–4248. [Google Scholar] [CrossRef]
- Pattenden, J.; Coulton, S.; Spilsbury, K.; Chattoo, S.; Lewin, B.; Cross, B. The Development and the Impact of the British Heart Foundation and Big Lottery Fund Heart Failure Specialist Nurse Service in England; British Heart Foundation: London, UK, 2008. [Google Scholar]
- Diller, G.P.; Kempny, A.; Babu-Narayan, S.V.; Henrichs, M.; Brida, M.; Uebing, A.; Lammers, A.E.; Baumgartner, H.; Li, W.; Wort, S.J.; et al. Machine learning algorithms estimating prognosis and guiding therapy in adult congenital heart disease: Data from a single tertiary centre including 10 019 patients. Eur. Heart J. 2019, 40, 1069–1077. [Google Scholar] [CrossRef] [Green Version]




| Demographic | Median (Range) | N (%) |
|---|---|---|
| Male | 54 (54%) | |
| Age at 2019 Appointment | 40.4 years (29.7–75.8) | |
| White British | 100 (100%) | |
| Index of Multiple Deprivation Decile * [12] | 4 (1–10) | |
| Diagnostic Group [16] | ||
| Tetralogy of Fallot | 27 (27%) | |
| Valvular Disease | 22 (22%) | |
| Aortic Coarctation | 16 (16%) | |
| AVSD | 10 (10%) | |
| Systemic Right Ventricle | 8 (9%) | |
| Fontan | 4 (4%) | |
| Complex Congenital # | 4 (4%) | |
| ASD | 3 (3%) | |
| VSD | 3 (3%) | |
| Ebstein Anomaly | 2 (2%) | |
| TGA Arterial Switch | 1 (1%) |
| Variable | Relative Risk of Decision Being Made | 95% CI | p Value (Fisher’s Exact) |
|---|---|---|---|
| Symptoms | 2.446 | 2.067–2.894 | <0.001 |
| New Symptoms | 4.294 | 3.056–6.032 | <0.001 |
| New Physical Finding | 10.288 | 3.743–28.277 | <0.001 |
| Post-operative/obstetric review | 2.793 | 1.373–5.683 | 0.006 |
| New ECG or Echo Finding | 3.957 | 2.239–6.994 | <0.001 |
| Clinic Attended | Total Appointments | Number of Patients | Appointments per Patient (Median and Range) |
|---|---|---|---|
| Non ACHD cardiology | 36 | 9 | 4 (1–11) |
| Cardiac surgery | 31 | 12 | 2 (1–6) |
| Pre-assessment | 37 | 32 | 1 (1–2) |
| Dental | 70 | 28 | 1 (1–11) |
| Obstetrics or Foetal Medicine | 114 | 9 | 13 (1–25) |
| Other specialities | 436 | 59 | 4 (1–75) |
| Physiotherapy | 9 | 2 | - |
| All | 733 | 77 | 4 (1–82) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coats, L.; Chaudhry, B. Ambulatory Care in Adult Congenital Heart Disease—Time for Change? J. Clin. Med. 2022, 11, 2058. https://doi.org/10.3390/jcm11072058
Coats L, Chaudhry B. Ambulatory Care in Adult Congenital Heart Disease—Time for Change? Journal of Clinical Medicine. 2022; 11(7):2058. https://doi.org/10.3390/jcm11072058
Chicago/Turabian StyleCoats, Louise, and Bill Chaudhry. 2022. "Ambulatory Care in Adult Congenital Heart Disease—Time for Change?" Journal of Clinical Medicine 11, no. 7: 2058. https://doi.org/10.3390/jcm11072058






