Abstract
In recent years, an increase in the problem of polypharmacotherapy in psychiatric patients has been observed, including the widespread problem of groups of people taking new psychoactive substances. One reason for this problem may be the poor knowledge of pharmacological interactions in psychiatry. The aim of this study was to explore the opinions and knowledge of psychiatrists from around the world on various aspects related to polypharmacotherapy. A total of 1335 psychiatrists from six continents were included in the study. The respondents’ opinion on the problem of hepatotoxicity in psychiatry was also examined. The greatest discrepancy among psychiatrists from different continents in the answers given concerned the definition of polypharmacotherapy (p < 0.001) and the approach to hepatotoxicity (p < 0.001). It is noteworthy that only about 20% of the psychiatrists surveyed (p < 0.001) believe that polypharmacotherapy is associated with a higher rate of patients’ hospitalisations. The most commonly used type of polypharmacy by psychiatrists was antidepressants and antipsychotics. Most of them also stated that polypharmacy was associated with reduced patient compliance with the doctor’s recommendations related to taking medications due to the increased complexity of the therapy. The continent that diversified the analysed questions to the greatest extent was Africa. Future educational activities for trainee psychiatrists should include more discussion of polypharmacotherapy in psychiatry.
1. Introduction
One of the major problems of modern pharmacotherapy in psychiatry is related to selecting the right combination of drugs for patients suffering from different conditions and requiring multidrug therapy. These patients constitute a group of people with a high risk of drug interactions. These interactions may result in a reduction of the therapeutic effect, the appearance of adverse reactions, and, in some situations, very seriously endanger the health and life of the patient. Post-drug complications increase the morbidity of the population, and, consequently, affect the costs borne by health systems, mainly due to an increase in the frequency of medical visits and hospitalisations. Polypharmacotherapy is commonly defined as the use of five or more medications daily by an individual, but is still debated, and it can vary from 2 to 11 concurrent medications. There is a diversity of definitions of polypharmacotherapy [1,2]. Polypharmacotherapy is particularly dangerous when the patient is treated by multiple specialists who are not necessarily informed which drugs the patient is currently taking [3].
Up to a third of outpatient psychiatric patients in the United States were receiving three or more psychotropic drugs at the same time. Over time, polypharmacotherapy has been used in an increasing proportion of patients [1]. According to data published in 2021, in a group of 14,418 hospitalised cases, 31% received at least five drugs simultaneously. Less than half of all patients received a combination of different antidepressants, or had antidepressant treatment supported by antipsychotics. The risk of any potential drug-drug interaction (pDDI) and potentially inappropriate medication (PIM) increased with each additional medication [4]. In a group of 47,071 inpatient hospital admissions, one-third of cases received an average of at least five different medications per day during their hospital stay. Fifty-one per cent of patients were receiving more than one psychotropic drug at a time [5]. According to data from 2021, the use of three or more psychotropic drugs in paediatrics increased significantly in the United States between 2000 and 2020. A higher number of side-effects were associated with drug regimens. Factors contributing to this include incorrect assumptions about the efficacy of combinations, as well as limited professional awareness of the metabolic and neurological side-effects of drugs [6]. The latest results of other studies carried out in a group of 448 psychiatric patients indicated that polypharmacotherapy was a risk factor for single and multiple drug-related adverse reactions [7].
The problem of polypharmacotherapy in patients taking various types of new psychoactive substances (NPS), such as mephedrone, has attracted attention in recent years. Ninety-nine per cent of the patients who were taking mephedrone combined it with other psychoactive substances, which resulted in the need for polypharmacotherapy. It increases the risk of subsequent hospitalisation of the same patients. This practice leads to a vicious circle effect resulting in numerous interactions not only between the drugs used, but also between abused psychoactive substances [8,9].
No data are observed in the literature regarding the knowledge of psychiatrists from all over the world on different aspects related to the topic of polypharmacotherapy. A single study, i.e., in a group of 347 psychiatrists from 34 countries, showed that their decision-making regarding polypharmacotherapy is policy-dependent. Another antipsychotic polytherapy survey conducted in a group of 44 prescribers showed that it was mainly assigned by those with more clinical experience and fewer concerns about it [10]. In Japan, in a group of 217 psychiatrists, the use of antipsychotic polypharmacotherapy was associated with, among other things, practice in a psychiatric hospital, as well as concern about potential drug–drug interactions [11]. In a group of Nigerian psychiatrists, polypharmacotherapy was mainly associated with the use of first-generation antipsychotics, as well as a desire to reduce the number of non-psychotic drugs [12].
The aim of our study was to investigate the attitudes of psychiatrists from six continents on various aspects related to polypharmacotherapy, including its definition, type of risks and benefits, and reasons for use. One of the main factors indicating the need for this type of study was the growing problem of polypharmacotherapy in patients taking new psychoactive substances in recent years. Studies conducted in the last 2 years have shown that only about 14% of psychiatrists know the names of and use pharmacological interaction databases in their daily work [13]. The attitudes towards the problem of hepatotoxicity associated with medications used in psychiatry were further investigated in the study group of psychiatrists. Polypharmacotherapy results in patients taking more and more medicinal products, which, by interacting pharmacokinetically and pharmacodynamically, induce symptoms of drug-related diseases, of which drug-related hepatopathies are one of the most clinically relevant [14]. An example of this would be patients taking a new psychoactive substance such as mephedrone, which is combined by most patients with other psychoactive substances, resulting, very often, in the need for polypharmacotherapy. The severity of the hepatotoxicity problem associated with the ingestion of psychoactive substances, combined with a range of potentially hepatotoxic drugs, can only make it more difficult to achieve a therapeutic effect [9]. For this reason, the authors decided to further investigate the opinion and knowledge of psychiatrists on hepatotoxicity in psychiatry.
2. Methods
2.1. Studied Group and Procedure
A total of 1335 psychiatrists from six continents were included in the analysis. Contact with psychiatrists was mainly through the LinkedIn Recruiter portal. Each person taking part in the study was made aware of the purpose of the survey before agreeing to complete it. Participation in the study was voluntary. The first questions concerned sociodemographic data, as well as daily medical practice. The next questions addressed several aspects related to the polypharmacotherapy used, i.e., its definition, reasons/types of use, possible ways of its reduction, factors influencing the occurrence, and risks/benefits associated with it (Appendix A). The questionnaire also included two questions on the appropriateness of polypharmacotherapy in schizophrenia and bipolar affective disorder. In line with the aim of the study outlined in the introduction, the question on hepatotoxicity in psychiatry, including the one associated with the use of psychotropic drugs, was also included in the study.
2.2. Statistical Analysis
In order to check whether there are statistically significant differences between psychiatrists from different continents in terms of the variable measured on the ordinal scale, the Kruskal–Wallis test was used. Selection was based on homogeneity of variance in the groups of individuals being compared. Effect size was measured by the epsilon-squared coefficient. For questions measured on a nominal scale, the chi-squared test and the Fi–Cramer coefficient were used. A p value < 0.05 was taken as the statistically significant level.
3. Results
3.1. Characteristics of the Studied Group of Psychiatrists
The study involved 1335 psychiatrists from six continents. The largest part of the study group was made up of psychiatrists of European origin, aged less than 40 years, with work experience ranging from 1 to 10 years, as well as men (Table 1).

Table 1.
Sociodemographic data of the surveyed group of psychiatrists.
3.2. Definition of Polypharmacotherapy
The definition of polypharmacotherapy was evaluated differently by the study group of psychiatrists, i.e., from different continents. This is indicated, among other things, by the result of Cramer’s V-factor. The largest number of psychiatrists stated that polypharmacotherapy involves a patient taking two or more drugs as part of the treatment of a disease or disorder for a period of time sufficient to overlap the effect of these drugs. The exception here are psychiatrists of African descent, who indicated as the most frequently selected answer the simultaneous use of two or more drugs by the patient as part of the treatment of a disease or disorder (Table 2).

Table 2.
Psychiatrists’ answers on the definition of polypharmacotherapy.
3.3. Reasons for Using Polypharmacotherapy
A greater proportion of the psychiatrists surveyed believe that monotherapy for a given disease does not have the expected effect according to clinical trials. Most of them expressed an affirmative view that the high complexity of the disorder or its severe course makes it difficult to choose an appropriate monotherapy. There are no statistically significant differences between continents in terms of individual reasons (Table 3).

Table 3.
Reasons for using polypharmacotherapy by the surveyed group of psychiatrists.
3.4. Type of Polypharmacotherapy
Among the types of polypharmacotherapy used by the surveyed group of psychiatrists, the most frequently chosen answer was the use of antidepressants with antipsychotics. Slightly more psychiatrists from Africa, compared to other continents, said they use two or more antipsychotic medications. In relation to the other continents, fewer respondents chose the answer of using antidepressants with sedative–sleep medication (Table 4).

Table 4.
Types of polypharmacotherapy used by the surveyed group of psychiatrists.
3.5. Clozapine Pharmacotherapy in the Treatment of Schizophrenia
Among the statements concerning the pharmacotherapy with clozapine in the treatment of schizophrenia, the most frequently chosen answer concerned the opinion that the use of clozapine monotherapy may be associated with less frequent hospitalisation than in the case of antipsychotic polypharmacotherapy during the treatment of schizophrenia. The other statements listed in the table below (Table 5) were selected by a small percentage of the psychiatrists surveyed. Monitoring of liver enzyme levels during clozapine pharmacotherapy has been indicated mainly by psychiatrists from Australia and South America. The greatest variation in the answers given concerns the knowledge that clozapine monotherapy has no confirmed and described side-effects associated with hepatotoxicity.

Table 5.
Psychiatrists’ answers on the clozapine pharmacotherapy in the treatment of schizophrenia.
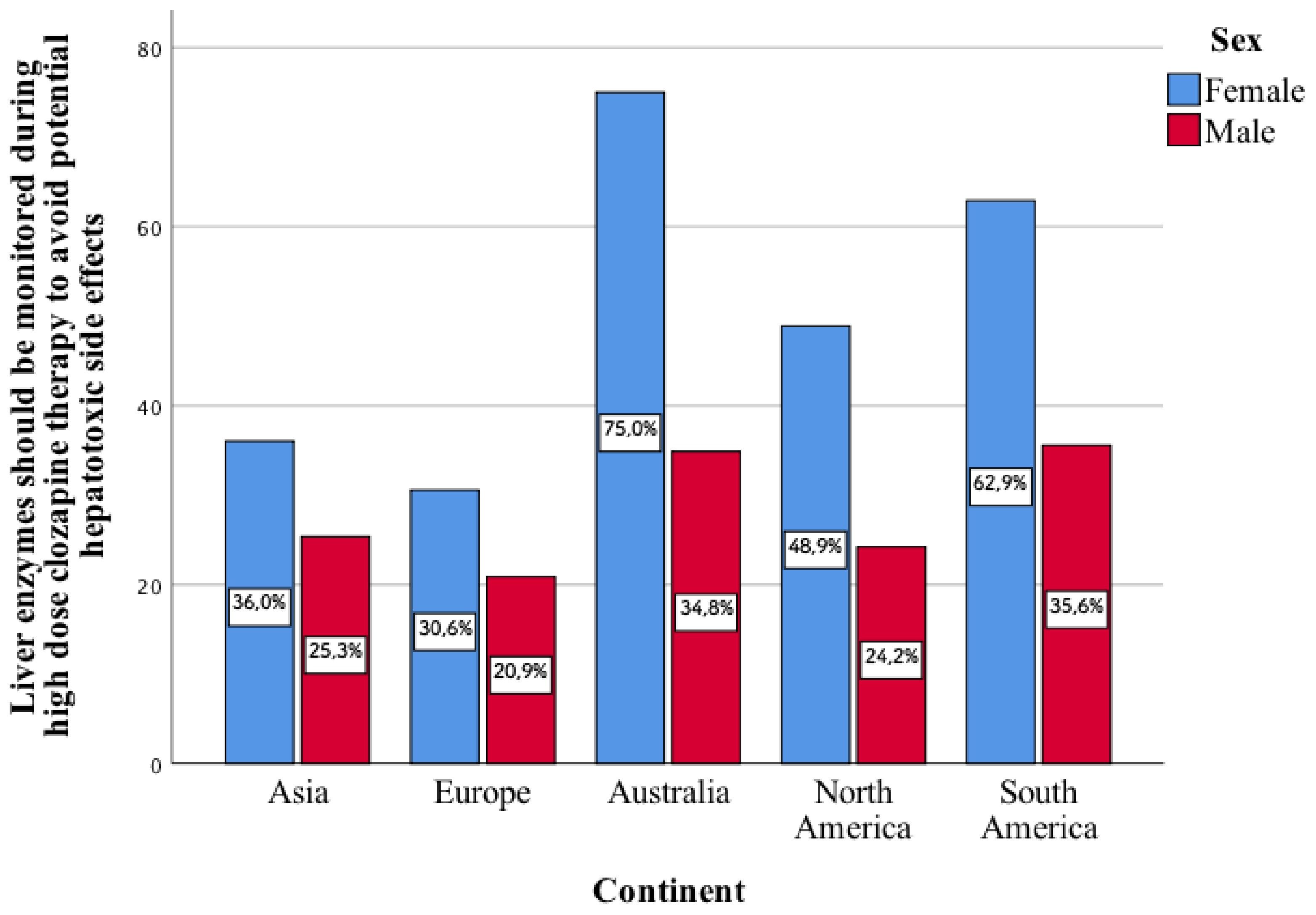
Only 31.6% of the psychiatrists surveyed believe that while taking high-dose clozapine, liver enzyme levels should be monitored to avoid potential side-effects related to hepatotoxicity. This type of statement enters into a statistically significant relationship with the gender of psychiatrists from individual continents. The greater part of the surveyed women, compared to men, indicated that they agree with this type of aspect (Figure 1). This concerns North America (p < 0.001) and South America (p < 0.001).
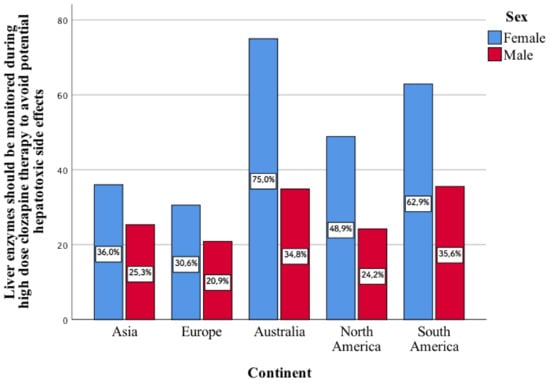
Figure 1.
Opinion of the women and men surveyed on whether, in their opinion, the level of liver enzymes should be monitored during high-dose clozapine therapy in order to avoid potential side-effects related to hepatotoxicity.
3.6. Polypharmacotherapy in the Treatment of Bipolar Disorder
A majority of psychiatrists have stated that for depressive states in bipolar disorder, it is acceptable to combine two or even three drugs with different mechanisms of action or those that have synergistic effects. The remaining answers related to bipolar disorder were chosen by a small percentage of the surveyed group. A smaller percentage of psychiatrists from Europe compared to other continents stated that patients undergoing monotherapy in the treatment of bipolar disorder were more likely to have recurrent acute manic episodes than patients on polypharmacotherapy. The greatest variation in the answers given concerns the first two statements listed in the table below (Table 6).

Table 6.
Psychiatrists’ answers on the polypharmacotherapy in the treatment of bipolar disorder.
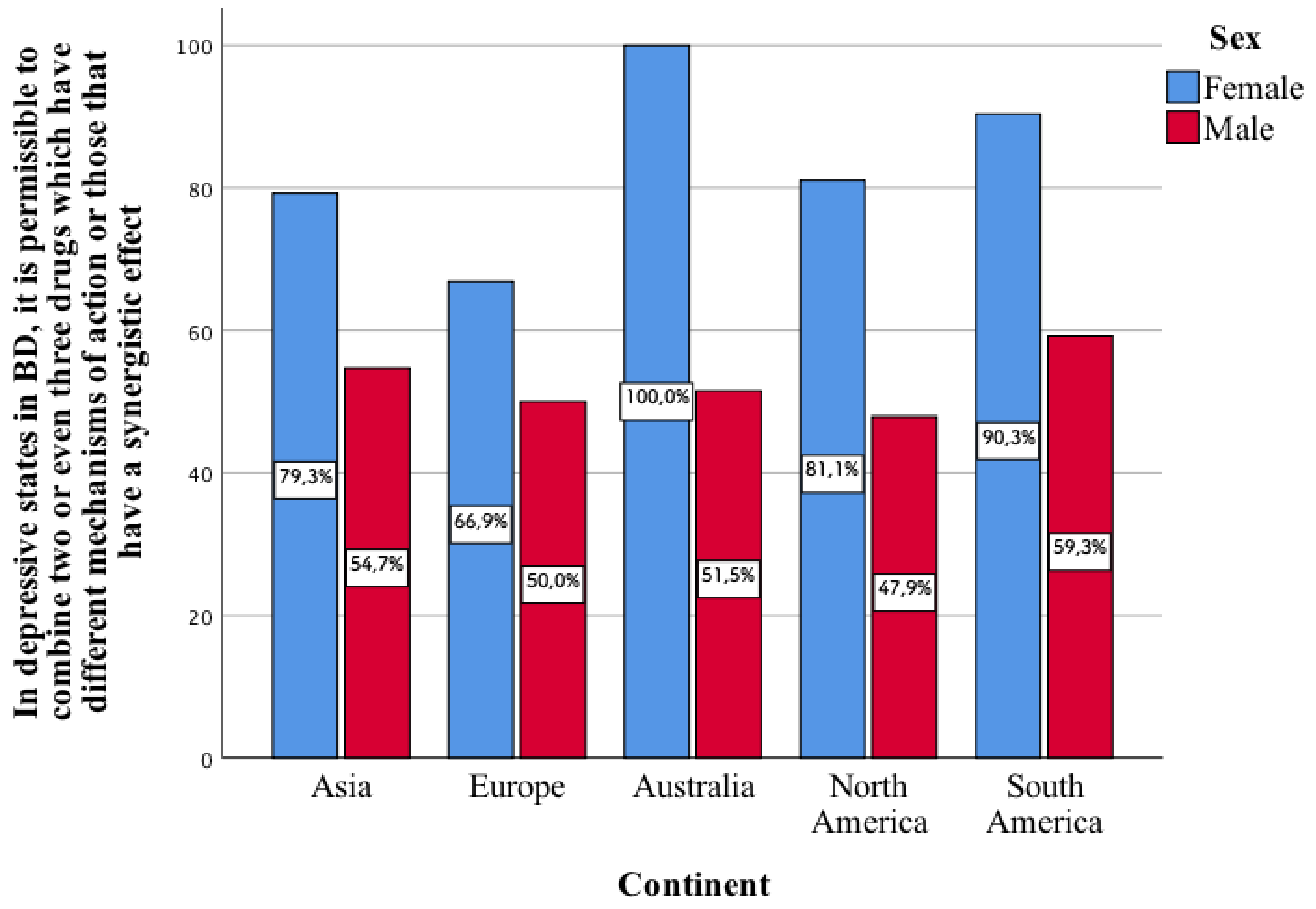
One of the aspects mentioned in the above table enters into a statistically significant correlation in all continents. It concerns whether, in depressive states in bipolar disorder, it is permissible to combine two or even three drugs with different mechanisms of action or those that have a synergistic effect. In each of the individual continents, a greater percentage of the surveyed women chose this type of response as compared to men (p < 0.001, Figure 2).
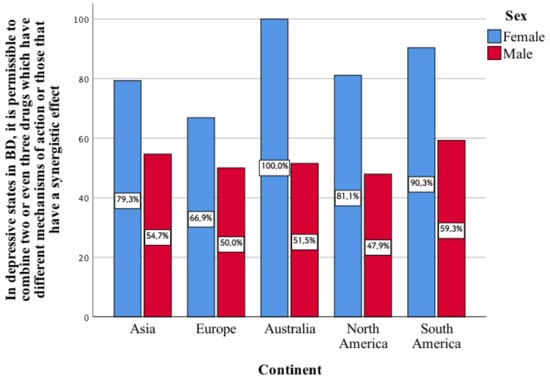
Figure 2.
Opinion of the surveyed women and men on whether, in depressive states in bipolar disorder, it is permissible to combine two or even three drugs with different mechanisms of action or those that have a synergistic effect.
3.7. Hepatotoxicity and the Effects of Psychiatric Drugs on Liver Function
A greater proportion of psychiatrists from across the continents said that knowledge of the influence of drugs on the functioning of the liver is useful in planning therapy in psychiatric patients taking more than one drug. This applies above all to European psychiatrists. More than 90% of psychiatrists chose the last aspects listed in Table 5 related to the hepatotoxicity of psychotropic drugs, although this applies to a slightly lesser extent to the subjects of African origin. Of note is the fact that a significant proportion of psychiatrists, mainly from Asia, believe that hepatotoxicity is well-studied, and described side-effect of many drugs used in psychiatric practice. The greatest variation in the study group of psychiatrists concerns the first and third aspects listed in the table below related to hepatotoxicity (Table 7).

Table 7.
Psychiatrists’ answers on the hepatotoxicity and the effects of psychiatric drugs on liver function.
3.8. Prevent and/or Reduce Excessive Polypharmacotherapy in Psychiatric Patients
Among the various methods associated with preventing and/or reducing excessive polypharmacotherapy among psychiatric patients, the psychiatrists surveyed from each continent indicated all the methods listed in Table 8 as effective (1–5 from ineffective to effective).

Table 8.
Psychiatrists’ answers on preventing and/or reducing excessive polypharmacotherapy in psychiatric patients.
We also observed statistically significant differences between women and men in terms of the factor of cooperation with specialists in the field of pharmacology or pharmacists in order to review the list of drugs taken by patients with polypharmacy. This applies to continents such as Asia, Europe, and North and South America. In these continents, women have expressed a greater view that this factor may prevent and/or reduce excessive polypharmacy in psychiatric patients. In men from these continents, the median of the answers given was four, and in women it was higher, i.e., equal to five. In other words, women from these continents believe, to a greater extent, that the analysed factor may contribute to the prevention and/or reduction of excessive polypharmacy among psychiatric patients:
- −
- Asia, U = 4493; p < 0.001
- −
- Europe, U = 13,256; p < 0.001
- −
- North America, U = 4668.5; p < 0.001
- −
- South America, U = 11,697.5; p < 0.001
3.9. Possible Risks/Benefits Associated with the Use of Polypharmacotherapy
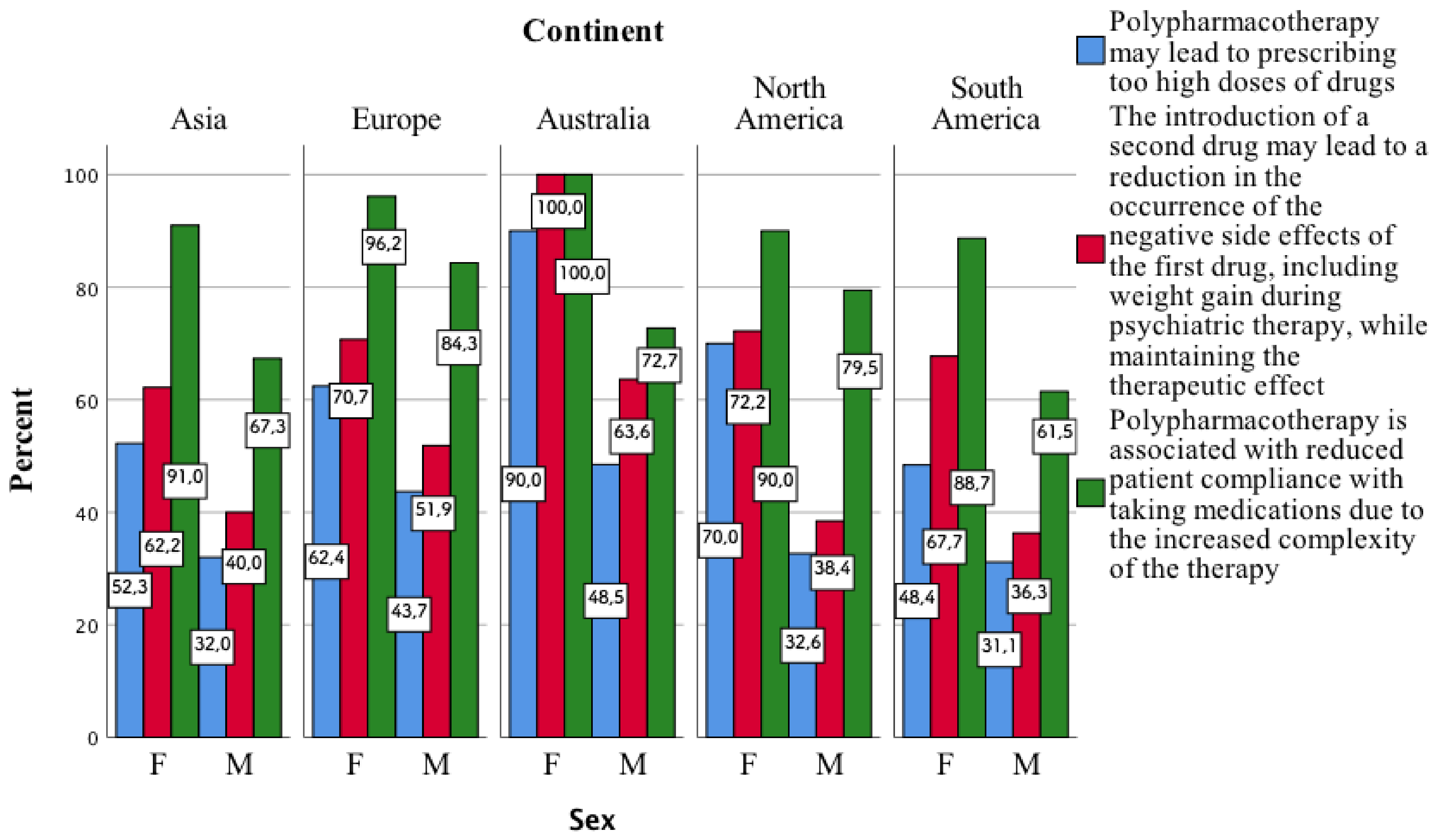
Among the possible risks/benefits associated with the use of polypharmacotherapy, the largest number of psychiatrists surveyed stated that polypharmacotherapy is associated with reduced patient compliance with the doctor’s recommendations related to taking medications due to the increase in the complexity of the therapy. This type of sentence was mainly indicated by psychiatrists coming from Europe. The same applies to their view that the introduction of a second drug can lead to a reduction in the occurrence of the negative side-effects of the first drug, e.g., weight gain during psychiatric treatment, while maintaining the therapeutic effect. The largest number of Australian-origin psychiatrists in relation to other psychiatrist groups believe that polypharmacotherapy may lead to prescribing too high doses of drugs. A small percentage of psychiatrists from each continent believe that polypharmacotherapy may be associated with higher rates of patient hospitalisation. The same applies to their view that, for some patients treated with antipsychotics, the therapeutic effect of polypharmacotherapy is better than that of monotherapy, particularly when analysing therapy with clozapine. The greatest variation in the answers given relates to the opinion that polypharmacotherapy is associated with a decrease in patient compliance with the doctor’s instructions related to taking medication due to an increase in the complexity of the therapy (Table 9).

Table 9.
Psychiatrists’ answers on the risk/benefits of polypharmacotherapy.
It is noteworthy that in individual continents, the greater part of the surveyed women, compared to men, indicated the second, third, and fifth aspects related to polypharmacotherapy mentioned in the above table (Figure 3).
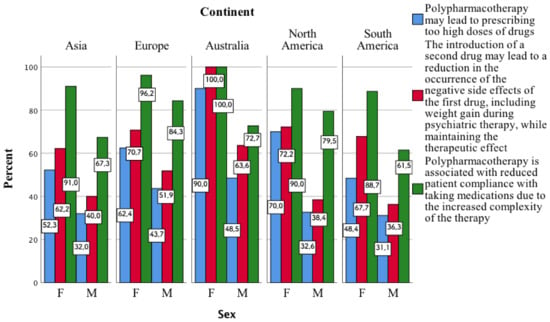
Figure 3.
Opinion of the surveyed women and men on three aspects related to the risks and benefits of using polypharmacy.
3.10. The Factors Influencing the Occurrence of the Phenomenon of Polypharmacotherapy
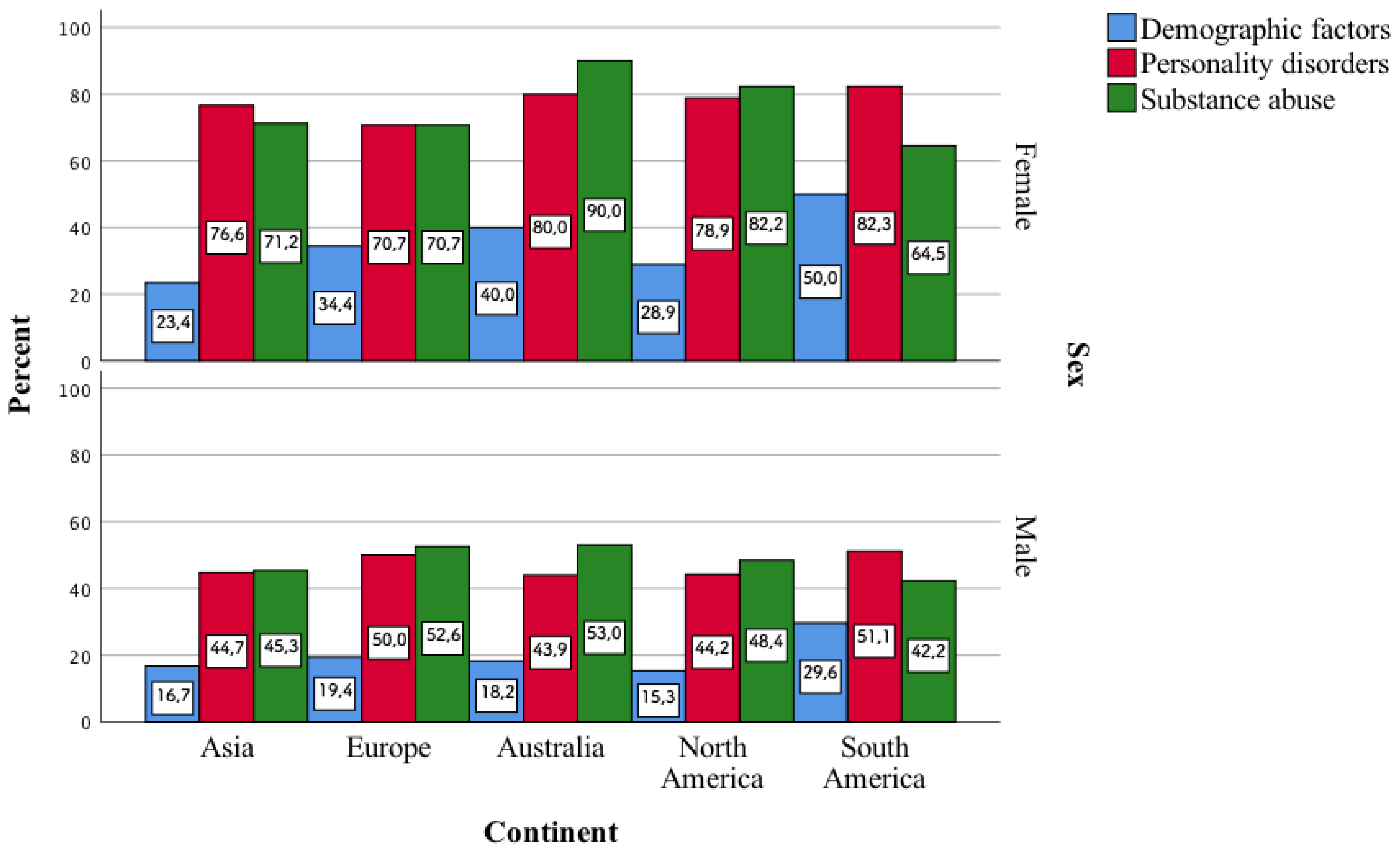
Among the factors influencing the occurrence of the phenomenon of polypharmacotherapy, the greatest number of psychiatrists indicated the presence of comorbidities, the severity of the disease, and resistance to treatment. This is particularly true of European psychiatrists. A small percentage of psychiatrists, mainly from Europe, identified demographic factors as the answer. Individuals indicated socioeconomic status. The divergence of responses for the other factors is noteworthy. Among the psychiatrists, 50–60% believe that personality disorders and substance abuse may be such factors. The factor that differentiated the groups of psychiatrists to the greatest extent was comorbidities (Table 10).

Table 10.
Psychiatrists’ answers on the factors influencing the occurrence of the phenomenon of polypharmacotherapy.
One of the least frequently indicated factors, i.e., demographic ones, draws attention. They were indicated by a small percentage of psychiatrists, and, as it turns out, they enter into a statistically significant correlation with their gender in individual continents. It turns out that more women than men stated that these demographic factors influence the occurrence of polypharmacotherapy. The largest differences in terms of sex are characteristic of demographic factors in Europe (p < 0.001). More women than men on continents also indicated factors such as personality disorders and substance abuse. The biggest differences in this case are in North America (p < 0.001) (Figure 4).
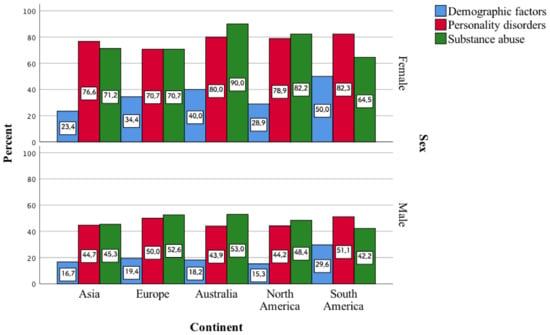
Figure 4.
Demographic factors, personality disorders, and substance abuse as variables influencing, according to the surveyed women and men, the occurrence of the phenomenon of polypharmacotherapy.
4. Discussion
To our knowledge, the study we conducted is the first to address the views of psychiatrists from six continents on the broad topic of polypharmacotherapy. In the first step, we assessed its definition, which was interpreted in a different way. Polypharmacotherapy is defined as the taking of two or more drugs by a patient as part of the treatment of a disease or disorder for a period of time sufficient to overlap the effect of these drugs [15,16]. Unfortunately, this type of answer was indicated by less than half of the psychiatrists surveyed. The initial answers listed in the first question are not correct due to the fact that they do not take into account any timeframe related to polypharmacotherapy, i.e., they do not provide any reference to the health of patients in whom each of the drugs taken is necessary. Some drugs may only be taken, e.g., in the hospital setting intermittently (so the overlap effect may not be observed), and some have to be taken due to chronic diseases, and hence, drug interactions become a significant problem.
The next aspect analysed in the study group of psychiatrists concerned their opinion on the reasons for using polypharmacotherapy in psychiatric patients. As the psychiatric diagnosis is based on the medical history, and the medical history is based on the doctor’s experience, it is often possible that the polypharmacotherapy applied is based more on the personal treatment methods of the professional concerned than on EBM (evidence-based medicine). An example is the situation of relying on the assumption that certain drugs work better taken in combination because it has worked for another patient, rather than on making sure that it is the safe and best form of therapy for that patient.
The same applies, for example, to the belief that a patient’s symptoms are so complex that a number of drugs should be used at once rather than starting with single drugs in low doses. This question also aimed to find out whether doctors refer more to the literature and research or to their own experience in medical practice when making a final decision about the type of therapy. The median of the answers given indicates that a larger proportion of psychiatrists believe that monotherapy in a given disease does not bring the expected results according to clinical trials. The highest agreement was for the sentence indicating that the high complexity of the disorder or its severe course makes it difficult to choose an appropriate monotherapy.
The psychiatrists surveyed stated that the most common type of polypharmacotherapy they used was a combination of antidepressants and antipsychotics. The number of visits with two or more drugs prescribed increased from 42.6% in 1996–1997 to 59.8% in 2005–2006. For the number of visits with three or more drugs, the increase ranged from 16.9% to 33.2%. Combinations of antidepressants with sedative–sleep medications (23.1%), antipsychotics (12.9%), and other antidepressants (12.6%) were the first, second, and third most commonly prescribed psychotropic drug combinations in the years when this type of study was conducted [1].
The next two questions analysed concerned clozapine pharmacotherapy for schizophrenia and pharmacotherapy for bipolar affective disorder. The largest number of psychiatrists surveyed chose the correct answer, namely that the use of clozapine monotherapy may be associated with less frequent hospitalisation than in the case of using antipsychotic polypharmacotherapy during the treatment of schizophrenia. While comparing patients diagnosed with schizophrenia and receiving Medicaid, in a 12-month study, Velligan et al. noted that clozapine monotherapy was associated with lower rates of disease-related hospital visits. The Medicaid cost difference was 40–45% compared with patients receiving polypharmacotherapy, most commonly a combination of risperidone and quetiapine, or risperidone and ariprazole [17]. The other two correct answers listed in Table 4, i.e., third and fourth, were indicated by a small percentage of the psychiatrists surveyed. This is especially true since clozapine is a monotherapy drug that can cause serious liver damage. The studies conducted so far indicate that hepatotoxicity should be monitored when using clozapine [18]. For example, in a 30-year-old man, the level of liver enzymes during the 4-week monotherapy with clozapine increased significantly after 3 weeks, so as not to allow further use of the drug [19]. Some differences in therapeutic doses of antipsychotics are known to be due to ethnicity (i.e., allele frequencies of pharmacogenes associated to psychotropic medications) [20,21]. More than half of the psychiatrists surveyed also chose the correct answer, indicating that for depressive states in bipolar disorder, it is acceptable to combine two or even three drugs with different mechanisms of action or those that have a synergistic effect. It is acceptable to combine two or three drugs for the treatment of depressive states in ChAD, and these drugs may have the same or different mechanisms of action [22]. A small percentage of psychiatrists from individual continents stated that the addition of lamotrigine to the quetiapine used reverses the pro-inflammatory effect of quetiapine in microglia cells. Quetiapine has strong pro-inflammatory effects in microglia cells, but these can be reversed when quetiapine is used together with lamotrigine or with other drug combinations that contain lamotrigine [23].
In our study, we also examined the approach of the subjects to the problem of hepatotoxicity in psychiatry. The majority of the psychiatrists surveyed indicated four correct answers regarding the aspects studied. It is noteworthy, however, that a smaller percentage of psychiatrists from individual continents indicated one of these correct answers. It indicates that drug-related hepatotoxicity can be unequivocally established when symptoms associated with liver damage occur after starting the drug, disappear after stopping the drug, and reappear after subsequent administration of the same drug [24]. For example, antidepressants can cause varying degrees of liver damage, including fatal damage. They are most often idiopathic and dose-dependent. They can develop within a few days to up to six months after starting treatment. For this reason, among others, it is very important in psychiatry to monitor the level of liver enzymes, including in psychiatric patients taking more than one drug [25].
According to the psychiatrists surveyed, all of the factors listed in Table 6 are the main methods of reducing excessive polypharmacotherapy. A study by Mary Brunette et al. showed that providing clinical staff with educational courses and audits, combined with feedback on the accuracy of prescribed medications, reduced the phenomenon of polypharmacotherapy in psychiatry. According to the authors of the study, thanks to these practices, the phenomenon of antipsychotic polypharmacotherapy decreased from 13.1% to 10.9% [26]. Another study showed that patient-directed education is a very important tool in reducing excessive polypharmacotherapy. Patients (65–95 years) taking benzodiazepines were studied. Of the recipients who received adequate knowledge, 62% had a conversation with their doctor and/or pharmacist about stopping treatment with benzodiazepines. After 6 months, 27% of patients in this group had stopped using benzodiazepines, compared with 5% in the control group [27].
In other studies, in order to select the best possible pharmacological treatment for patients residing in nursing homes, an online platform was introduced which allows participants to access relevant information regardless of time and place, and facilitates medical records and information exchange between doctors, nurses, and pharmacists. Pharmacists in this study tested the validity of pharmacotherapy by analysing the drugs that were prescribed to patients. After applying the intervention proposed in the study, the improvement in the adequacy of the drugs used was most evident in the residents with an inadequate Medication Appropriateness Index (MAI) baseline. The authors of the study and articles conclude that the study they propose can realistically improve the appropriateness of treatment for nursing home patients [28,29]. In 2003, a programme was set up in New York to speed up the recovery of psychiatric patients by simplifying their treatment. The software that was developed allowed doctors to visualise the treatment history of their patients, as well as those of their colleagues. The system allowed doctors to make better decisions in treating patients, and thus, contributed to a reduction in antipsychotic polypharmacotherapy [30].
The penultimate topic analysed was connected with the risks and benefits of using polypharmacotherapy. Of the five correct answers, most psychiatrists indicated the fifth one. It indicates that polypharmacotherapy is associated with a reduction in patient compliance with the doctor’s recommendations related to taking medications due to the increase in the complexity of the therapy [16]. The remaining correct answers were chosen by a significantly smaller percentage of psychiatrists from individual continents. According to the literature, polypharmacotherapy may be a rational choice when monotherapy does not have the desired effect or when a drug is needed to reduce the side-effects of other substances used, but it is associated with a number of disadvantages and additional health risks and costs for patients, as well as the risk of burdening the health system [2,16,31]. For this reason, additional educational activities related to the aspects studied should be carried out in the future. This mainly concerns the fact that polypharmacotherapy may lead to prescribing too high doses of drugs, and may be associated with a higher percentage of patients hospitalisation.
One of the ways to reduce the problem of side-effects associated with drug interactions may be to involve pharmacists in educating psychiatrists on this subject [32]. Most of the data related to teaching psychopharmacology is contained in the American Society for Psychopharmacology Model Psychopharmacology Curriculum (ASCP). Educators present their suggestions related to teaching psychopharmacology [33]. Accordingly, one of the recommendations that could be made is to increase the emphasis in class on drug interactions in psychiatry. This applies, inter alia, to the use of databases in which you can check if there are side-effects associated with drug interactions. Another option for broadening the working knowledge of drug interactions among those educating psychiatry is by studying case reports, as well as reviewing the literature on psychotropic drugs [33,34,35].
Finally, we examined the aethiologic factors that may influence the occurrence of polypharmacotherapy. All of the factors listed in Table 7 play an important role here; however, two of them, i.e., socio-economic status and socio-demographics, were indicated by a smaller percentage of psychiatrists coming from each continent. It is also noteworthy that about 50% of psychiatrists identified personality disorders and substance abuse as factors. Lelliott et al. showed that in a group of patients aged 18–65 years, the risk of being prescribed more than one antipsychotic decreased by about 12% every ten years. The risk for men was about 1.4 times higher than for women [36].
The studies conducted by Haider et al. showed that people with the lowest level of education took the highest number of medications, and were most likely to experience polypharmacotherapy and excessive pharmacotherapy. The risk of polypharmacotherapy increased by an average of 11% as the level of education decreased. Women with low education had a slightly higher risk than men with low education. The researchers point out that this may be related to the fact that people with higher education have better access to knowledge related to their treatment and medication, and thus, communicate more actively with the specialist, and influence the prescribing process [37]. Kuno and Rothbard found that people of African American descent were less likely to receive antidepressants, but were more likely to receive higher doses of antipsychotics than Caucasians, despite similar severity of depressive symptoms. The overall conclusion of the researchers was that there are differences depending on the patient’s race that affect the treatment, perhaps due to the beliefs of doctors who expect lower compliance with medical recommendations by people of African American origin [38]. In a study by Lin and Smith, the authors note that black patients were more likely to be prescribed additional antipsychotics during treatment with olanzapine. Patients of African American descent were also more likely to receive higher doses of medication. The authors postulate that this is related to an overestimation of the risk of aggressive behaviour in these patients [39]. Burcu et al. found that, when considering visits to psychiatrists and non-psychiatrists, psychiatrists tended to prescribe antipsychotics more frequently to children and adolescents (24.2% vs. 4.6%). Rarely are these drugs prescribed as monotherapy, i.e., in only 10.2% of cases [40]. In their studies, Suzuki et al. found that some patients with drug-resistant schizophrenia (TRS) benefited from polypharmacotherapy with OLZ (olanzapine) and RIS (risperidone), which could not be achieved by monotherapy with either drug, albeit at the cost of side-effects, i.e., elevated blood prolactin levels, total cholesterol, and weight gain. They concluded that polypharmacotherapy may be beneficial for some patients difficult to treat, but not all, hence the need for further research and clarification of which patients may benefit from polypharmacotherapy and which may not [41]. In the elderly group (75 years and older), the number of medicines taken, and therefore, the frequency of polypharmacotherapy increases with the presence of comorbidities. Most of the subjects had five or more comorbidities, putting them at high risk of excessive polypharmacotherapy, with the greatest number of patients being prescribed antidepressants. The authors noted that there is a trend towards polypharmacotherapy in elderly patients with comorbidities such as hypertension, history of myocardial infarction, diabetes, heart failure, or dementia [42]. In monolingual Hispanics and African Americans, adherence to treatment recommendations was lower (77 and 68%) than in Caucasians (90%). The researchers additionally point out that diet affects the pharmacokinetic properties of drugs, and dietary habits vary among ethnic groups, which may affect the effects of drugs. In addition, ethnic minorities are often in the habit of using traditional herbal medicines, which may affect the effectiveness of the therapy [43]. As for the factor of other psychoactive substances, Barnes et al. point out that there is often a tendency to abuse them in patients with schizophrenia, which probably makes it difficult to adhere to prescribed pharmacotherapy. Patients who were additionally prescribed benzodiazepines, and who had a history of addiction and comorbidities, had a higher risk of benzodiazepine dependence and reported a lower quality of life standard [44,45].
5. Conclusions
Polypharmacotherapy might have bad consequences if being inappropriate, which should be further explored. Future education should place more emphasis on the topic of polypharmacotherapy in psychiatric patients. The diverse definitions of polypharmacotherapy, and the low awareness of its impact on the risk of subsequent hospitalizations of psychiatric patients, prove the need to strengthen the teaching of the medical community in this field. Attention should also be paid to the problem of hepatotoxicity in psychiatry, namely by making the medical community aware of the need to monitor laboratory parameters related to liver function. Further studies are required to assess to which extent the polypharmacy practice was rational and appropriate.
6. Limitations
A limitation of the study we conducted is remote contact with psychiatrists (it was an online survey), which has to do with the prevailing COVID-19 pandemic resulting in difficulties in doing inpatient work or attending psychiatric conferences. The sample usually consists of younger population when it is an online survey. However, research to date has shown that it is an effective portal for conducting this type of research. Another limitation of the study is the lack of the study conducted through other forms of contact with psychiatrists, such as through the website of the World Psychiatric Association (www.wpanet.org, accessed on 1 April 2022). Future research should consider an even larger group of psychiatrists, so as to be able to check whether there are statistically significant differences between women and men in terms of the examined aspect.
Author Contributions
All authors made substantial, direct, and intellectual contributions to the work, and approved it for publication. M.O. conceived the idea for this study. M.O., D.T. and A.G. conducted a survey. M.O., D.T., A.G. and M.B.-Z. performed the literature search. T.N. was responsible for the clinical aspect of the research. M.O. analysed the data. M.O., T.N. and M.B.-Z. drafted the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, considering it was conducted anonymised. This study did not require the consent of the Bioethics Committee. The psychiatrists who were selected to participate in the surveys were informed that anonymity was guaranteed, and that the data would be used for research. By responding to the surveys, the respondents gave their consent to participate. Each psychiatrist was informed of the study aim before he or she agreed to participate. Participation in the study was voluntary.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Please contact the corresponding author with any data availability requests.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Questionnaire
Question 1. Please Select the Definition of Polypharmacotherapy you Consider to be the Most Correct/Complete and that You Use in Your Daily Practice:
- a.
- A patient taking two or more drugs simultaneously to treat a disease or disorder
- b.
- A patient taking two or more drugs from the same category simultaneously to treat a disease or disorder
- c.
- A patient taking two or more drugs from different categories simultaneously to treat a disease or disorder
- d.
- A patient taking two or more drugs to treat a disease or disorder for a period sufficient for the effects of these drugs to overlap
- e.
- A patient taking two or more drugs from any drug groups, including drugs unrelated to the therapy of the disease or disorder (such as NSAIDs).
Question 2. Please Indicate to What Extent You Agree with the Reasons for Using Polypharmacotherapy for Psychiatric Patients (5—I Completely Agree, 3—It is Difficult to Say, 1—I Do Not Agree at All).
- a.
- Monotherapy for a given disease does not bring the expected results according to clinical trials:
- b.
- Monotherapy for a given disease does not bring the expected results in the history of a given patient:
- c.
- Polypharmacotherapy was successful in other patients with similar symptoms or disorders:
- d.
- The high complexity of the disorder or its severe course makes it difficult to select an appropriate monotherapy:
- e.
- The use of combined drugs gives a better therapeutic effect than the use of one drug in other patients with a similar disorder/symptoms:
Question 3. Which Type of Polypharmacotherapy Do You Use in Your Medical Practice:
- a.
- Two or more antidepressant drugs
- b.
- Two or more antipsychotic drugs
- c.
- Antidepressants with sedative–hypnotic drugs
- d.
- Antidepressants with antipsychotics
- e.
- Antipsychotics with sedative–hypnotic drugs
Question 4. The Following Sentences Apply to Clozapine Pharmacotherapy in the Treatment of Schizophrenia. Please Tick the Sentences Which you Think are True or with Which You Agree the Most.
- a.
- The use of clozapine monotherapy may be associated with a reduced need for hospitalisation than in the case of antipsychotic polypharmacy in the treatment of schizophrenia.
- b.
- Polypharmacotherapy with sulpiride and clozapine does not show increased efficacy compared to clozapine monotherapy in the treatment of schizophrenia in patients who are refractory to treatment with atypical antipsychotics.
- c.
- Clozapine is a drug which can cause severe liver damage when used in monotherapy.
- d.
- Liver enzymes should be monitored during high-dose clozapine therapy to avoid potential hepatotoxic side-effects.
- e.
- Clozapine monotherapy has no confirmed and described hepatotoxic side-effects.
Question 5. The Following Sentences Concern the Phenomenon of Polypharmacotherapy in the Treatment of Bipolar Disorder (BD). Please Tick the Sentences Which You Think are True or with Which You Agree the Most.
- a.
- In the treatment of depression symptoms in BD, the addition of lamotrigine to quetiapine does not increase the efficacy of the pharmacotherapy.
- b.
- The addition of lamotrigine when using quetiapine reverses the pro-inflammatory effects of quetiapine in microglia cells.
- c.
- Patients undergoing monotherapy for the treatment of BD more often have relapses of acute manic episodes than patients undergoing polypharmacotherapy.
- d.
- Women with BD during pregnancy and in the puerperium period should undergo prophylactic polypharmacotherapy in order to avoid episodes of the disease during this period.
- e.
- In depressive states in BD, it is permissible to combine two or even three drugs which have different mechanisms of action or those that have a synergistic effect.
Question 6. The Following Claims Concern Hepatotoxicity and the Effects of Psychiatric Drugs on Liver Function. Please Tick the Sentences which you Think are True or with which You Agree the Most.
- a.
- Knowledge of the effects of drugs on liver function is useful when planning therapy for psychiatric patients taking more than one drug.
- b.
- Hepatotoxicity is a well-studied and reported side-effect of many drugs used in psychiatric practice.
- c.
- Drug-related hepatotoxicity can be unequivocally determined when the symptoms of liver damage occur after a patient starts taking a drug, and disappear when the drug is discontinued.
- d.
- Drug-related hepatotoxicity can be unequivocally determined when the symptoms of liver damage occur after a patient starts taking a drug, disappear when the drug is discontinued, and reappear after the next administration of the same drug.
- e.
- When prescribing drugs, in particular, potentially hepatotoxic drugs, the patient should be required to test and monitor the level of liver enzymes.
- f.
- Minimising polypharmacotherapy, in particular, with potentially hepatotoxic drugs, may lower the risk of liver damage in psychiatric patients.
Question 7. In Your Opinion, How Effective Would It Be to Use the Following Methods to Prevent And/or Reduce Excessive Polypharmacotherapy in Psychiatric Patients? (On a Scale of 1–5 from Very Effective to Ineffective)
- a.
- Education and training of hospital staff (doctors, nurses):
- b.
- Conducting internal audits and controls:
- c.
- Educating patients and improving their understanding of the disease, the drug used, and its side-effects:
- d.
- Collaborating with specialists in the field of pharmacology or with pharmacists to review the list of drugs taken by patients in polypharmacotherapy:
- e.
- Introducing new programmes or applications into medical practice to help doctors show the medications taken previously by patients and their effectiveness:
Question 8. Various Statements Regarding the Risks and Benefits of Polypharmacotherapy Are Presented Below. Please Tick the Sentences Which You Think Are True or with Which You Agree the Most.
- a.
- For some patients treated with antipsychotics, the therapeutic effect of polypharmacotherapy is better than in the case of monotherapy, in particular, for clozapine therapy.
- b.
- Polypharmacotherapy may lead to prescribing too high doses of drugs.
- c.
- The introduction of a second drug may lead to a reduction in the occurrence of the negative side-effects of the first drug, including weight gain during psychiatric therapy, while maintaining the therapeutic effect.
- d.
- By ensuring faster and better therapeutic effects, polypharmacotherapy leads to better patient compliance with the doctor’s recommendations.
- e.
- Polypharmacotherapy is associated with reduced patient compliance with taking medications due to the increased complexity of the therapy.
- f.
- Thanks to better therapeutic effectiveness, polypharmacotherapy leads to lower therapy costs and less frequent medical consultations/hospitalisation.
- g.
- Polypharmacotherapy may be associated with a higher rate of hospitalisation.
Question 9. Which of the Etiological Factors Listed Below, in Your Opinion, Influence the Occurrence of Polypharmacotherapy?
- a.
- Demographic factors (age, gender, race, patient’s level of education)
- b.
- Personality disorders
- c.
- The presence of comorbidities
- d.
- The severity of the disease
- e.
- Resistance to treatment
- f.
- Socio-economic status
- g.
- Substance abuse
References
- Mojtabai, R.; Olfson, M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch. Gen. Psychiatry 2010, 67, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Kukreja, S.; Kalra, G.; Shah, N.; Shrivastava, A. Polypharmacy In Psychiatry: A Review. Mens Sana Monogr. 2013, 11, 82–99. [Google Scholar] [PubMed]
- Kinoshita, H.; Kobayashi, Y.; Fukuda, T. Duplicative medications in patients who visit multiple medical institutions among the insured of a corporate health insurance society in Japan. Health Policy 2008, 85, 114–123. [Google Scholar] [CrossRef]
- Wolff, J.; Reißner, P.; Hefner, G.; Normann, C.; Kaier, K.; Binder, H.; Hiemke, C.; Toto, S.; Domschke, K.; Marschollek, M.; et al. Pharmacotherapy, drug-drug interactions and potentially inappropriate medication in depressive disorders. PLoS ONE 2021, 16, e0255192. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.; Hefner, G.; Normann, C.; Kaier, K.; Binder, H.; Hiemke, C.; Toto, S.; Domschke, K.; Marschollek, M.; Klimke, A. Polypharmacy and the risk of drug-drug interactions and potentially inappropriate medications in hospital psychiatry. Pharmacoepidemiol. Drug Saf. 2021, 30, 1258–1268. [Google Scholar] [CrossRef]
- Zito, J.M.; Zhu, Y.; Safer, D.J. Psychotropic Polypharmacy in the US Pediatric Population: A Methodologic Critique and Commentary. Front. Psychiatry 2021, 12, 644741. [Google Scholar] [CrossRef]
- Ayani, N.; Morimoto, T.; Sakuma, M.; Kikuchi, T.; Watanabe, K.; Narumoto, J. Antipsychotic Polypharmacy Is Associated With Adverse Drug Events in Psychiatric Inpatients: The Japan Adverse Drug Events Study. J. Clin. Psychopharmacol. 2021, 41, 397–402. [Google Scholar] [CrossRef]
- Ordak, M.; Nasierowski, T.; Muszynska, E. The growing problem of mephedrone use in Warsaw, Poland, 2010–2018. Lancet Psychiatry 2018, 5, 787. [Google Scholar] [CrossRef] [Green Version]
- Ordak, M.; Nasierowski, T.; Muszynska, E. The problem of poly-pharmacotherapy in patients on a mephedrone binge. Pharmacol. Res. 2019, 143, 204. [Google Scholar] [CrossRef]
- Correll, C.U.; Shaikh, L.; Gallego, J.A.; Nachbar, J.; Olshanskiy, V.; Kishimoto, T.; Kane, J.M. Antipsychotic polypharmacy: A survey study of prescriber attitudes, knowledge and behavior. Schizophr. Res. 2011, 131, 58–62. [Google Scholar] [CrossRef] [Green Version]
- Kishimoto, T.; Watanabe, K.; Uchida, H.; Mimura, M.; Kane, J.M.; Correll, C.U. Antipsychotic polypharmacy: A Japanese survey of prescribers’ attitudes and rationales. Psychiatry Res. 2013, 209, 406–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- James, B.O.; Omoaregba, J.O.; Raji, S.O.; Imishue, O.E.; Okonoda, K.M.; Nyamali, Y.I.; Famuyiwa, P.A.; Correll, C.U. Attitudes towards and rationale for antipsychotic polypharmacy among psychiatrists in Nigeria: Characteristics associated with high reported antipsychotic polypharmacy. Psychiatry Res. 2017, 248, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Ordak, M.; Nasierowski, T.; Muszynska, E.; Bujalska-Zadrozny, M. Increasing the Effectiveness of Pharmacotherapy in Psychiatry by Using a Pharmacological Interaction Database. J. Clin. Med. 2021, 10, 2185. [Google Scholar] [CrossRef] [PubMed]
- Kullak-Ublick, G.A.; Andrade, R.J.; Merz, M.; End, P.; Benesic, A.; Gerbes, A.L.; Aithal, G.P. Drug-induced liver injury: Recent advances in diagnosis and risk assessment. Gut 2017, 66, 1154–1164. [Google Scholar] [CrossRef] [Green Version]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef] [Green Version]
- Olashore, A.A.; Rukewe, A. Polypharmacy among children and adolescents with psychiatric disorders in a mental referral hospital in Botswana. BMC Psychiatry 2017, 17, 174. [Google Scholar] [CrossRef] [Green Version]
- Velligan, D.I.; Carroll, C.; Lage, M.J.; Fairman, K. Outcomes of medicaid beneficiaries with schizophrenia receiving clozapine only or antipsychotic combinations. Psychiatr. Serv. 2015, 66, 127–133. [Google Scholar] [CrossRef]
- Todorović Vukotić, N.; Đorđević, J.; Pejić, S.; Đorđević, N.; Pajović, S.B. Antidepressants- and antipsychotics-induced hepatotoxicity. Arch. Toxicol. 2021, 95, 767–789. [Google Scholar] [CrossRef]
- Panagiotis, B. Grand mal seizures with liver toxicity in a case of clozapine treatment. J. Neuropsychiatry Clin. Neurosci. 1999, 11, 117–118. [Google Scholar] [CrossRef]
- de Leon, J. Precision psychiatry: The complexity of personalizing antipsychotic dosing. Eur. Neuropsychopharmacol. 2022, 58, 80–85. [Google Scholar] [CrossRef]
- de Leon, J.; Schoretsanitis, G.; Smith, R.L.; Molden, E.; Solismaa, A.; Seppälä, N.; Kopeček, M.; Švancer, P.; Olmos, I.; Ricciardi, C.; et al. An International Adult Guideline for Making Clozapine Titration Safer by Using Six Ancestry-Based Personalized Dosing Titrations, CRP, and Clozapine Levels. Pharmacopsychiatry 2022, 55, 73–86. [Google Scholar] [PubMed]
- Sarkar, S. Psychiatric Polypharmacy, Etiology and Potential Consequences. Curr. Psychopharmacol. 2017, 6, 12. [Google Scholar] [CrossRef]
- Bortolasci, C.C.; Spolding, B.; Callaly, E.; Martin, S.; Panizzutti, B.; Kidnapillai, S.; Connor, T.; Hasebe, K.; Mohebbi, M.; Dean, O.M.; et al. Mechanisms Underpinning the Polypharmacy Effects of Medications in Psychiatry. Int. J. Neuropsychopharmacol. 2018, 21, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Sedky, K.; Nazir, R.; Joshi, A.; Kaur, G.; Lippmann, S. Which psychotropic medications induce hepatotoxicity? Gen. Hosp. Psychiatry 2012, 34, 53–61. [Google Scholar] [CrossRef]
- Voican, C.S.; Corruble, E.; Naveau, S.; Perlemuter, G. Antidepressant-induced liver injury: A review for clinicians. Am. J. Psychiatry 2014, 171, 404–415. [Google Scholar] [CrossRef] [Green Version]
- Brunette, M.F.; Cotes, R.O.; de Nesnera, A.; McHugo, G.; Dzebisashvili, N.; Xie, H.; Bartels, S.J. Use of Academic Detailing With Audit and Feedback to Improve Antipsychotic Pharmacotherapy. Psychiatr. Serv. 2018, 69, 1021–1028. [Google Scholar] [CrossRef]
- Tannenbaum, C.; Martin, P.; Tamblyn, R.; Benedetti, A.; Ahmed, S. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: The EMPOWER cluster randomized trial. JAMA Intern. Med. 2014, 174, 890–898. [Google Scholar] [CrossRef] [Green Version]
- Schaffler-Schaden, D.; Pitzer, S.; Schreier, M.; Dellinger, J.; Brandauer-Stickler, B.; Lainer, M.; Flamm, M.; Osterbrink, J. Improving medication appropriateness in nursing home residents by enhancing interprofessional cooperation: A study protocol. J. Interprof. Care 2018, 32, 517–520. [Google Scholar] [CrossRef]
- Dellinger, J.K.; Pitzer, S.; Schaffler-Schaden, D.; Schreier, M.M.; Fährmann, L.S.; Hempel, G.; Likar, R.; Osterbrink, J.; Flamm, M. Improving medication appropriateness in nursing homes via structured interprofessional medication-review supported by health information technology: A non-randomized controlled study. BMC Geriatr. 2020, 20, 506. [Google Scholar] [CrossRef]
- Tucker, W.M. When less is more: Reducing the incidence of antipsychotic polypharmacy. J. Psychiatr. Pract. 2007, 13, 202–204. [Google Scholar] [CrossRef]
- Kojima, G.; Bell, C.; Tamura, B.; Inaba, M.; Lubimir, K.; Blanchette, P.L.; Iwasaki, W.; Masaki, K. Reducing cost by reducing polypharmacy: The polypharmacy outcomes project. J. Am. Med. Dir. Assoc. 2012, 13, 818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- AlRuthia, Y.; Alkofide, H.; Alosaimi, F.D.; Sales, I.; Alnasser, A.; Aldahash, A.; Almutairi, L.; AlHusayni, M.M.; Alanazi, M.A. Drug-drug interactions and pharmacists’ interventions among psychiatric patients in outpatient clinics of a teaching hospital in Saudi Arabia. Saudi Pharm. J. 2019, 27, 798–802. [Google Scholar] [CrossRef] [PubMed]
- Rakofsky, J. Innovations in Psychopharmacology Education in U.S. Psychiatric Residency Programs. Focus 2021, 19, 46–49. [Google Scholar] [PubMed]
- Zisook, S.; Benjamin, S.; Balon, R.; Glick, I.; Louie, A.; Moutier, C.; Moyer, T.; Santos, C.; Servis, M. Alternate methods of teaching psychopharmacology. Acad Psychiatry 2005, 29, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Osser, D.N.; Patterson, R.D.; Levitt, J.J. Guidelines, algorithms, and evidence-based psychopharmacology training for psychiatric residents. Acad. Psychiatry 2005, 29, 180–186. [Google Scholar] [CrossRef]
- Lelliott, P.; Paton, C.; Harrington, M.; Konsolaki, M.; Sensky, T.; Okocha, C. The influence of patient variables on polypharmacy and combined high dose of antipsychotic drugs prescribed for in-patients. Psychiatr. Bull. 2002, 26, 41114. [Google Scholar] [CrossRef] [Green Version]
- Haider, S.I.; Johnell, K.; Weitoft, G.R.; Thorslund, M.; Fastbom, J. The Influence of educational level on polypharmacy and in- appropriate drug use: A register-based study of more than 600,000 older people. J. Am. Geriatr. Soc. 2009, 57, 62–69. [Google Scholar] [CrossRef]
- Kuno, E.; Rothbard, A.B. Racial disparities in antipsychotic prescription patterns for patients with schizophrenia. Am. J. Psychiatry 2002, 159, 567–572. [Google Scholar] [CrossRef]
- Lin, K.M.; Smith, M.W. Psychopharmacotherapy in the con- text of culture and ethnicity. Ethn. Psychopharmacol. 2000, 19, 1–36. [Google Scholar]
- Burcu, M.; Safer, D.J.; Zito, J.M. Antipsychotic prescribing for behavioral disorders in US youth: Physician specialty, in- surance coverage, and complex regimens. Pharmacoepidemiol. Drug Saf. 2016, 25, 26–34. [Google Scholar] [CrossRef]
- Suzuki, T.; Uchida, H.; Watanabe, K.; Nakajima, S.; Nomura, K.; Takeuchi, H.; Tanabe, A.; Yagi, G.; Kashima, H. Effectiveness of antipsychotic polypharmacy for patients with treatment refractory schizophrenia: An open-label trial of olanzapine plus risperidone for those who failed to respond to a sequential treatment with olanzapine, quetiapine and risperidone. Hum. Psychopharmacol. 2008, 23, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Mizokami, F.; Koide, Y.; Noro, T.; Furuta, K. Polypharmacy with common diseases in hospitalized elderly patients. Am. J. Geriatr. Pharmacother. 2012, 10, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, I.; Neelam, K.; Duddu, V.; Husain, N. Ethnicity and psychopharmacology. J. Psychopharmacol. 2008, 22, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Barnes, T.R.; Mutsatsa, S.H.; Hutton, S.B.; Watt, H.C.; Joyce, E.M. Comorbid substance use and age at onset of schizophrenia. Br. J. Psychiat. 2006, 188, 237–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunette, M.F.; Noordsy, D.L.; Xie, H.; Drake, R.E. Benzodiazepine use and abuse among patients with severe mental illness and co-occurring substance use disorders. Psychiatr. Serv. 2003, 54, 1395–1401. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).