Noise Levels and Sleep in a Surgical ICU
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
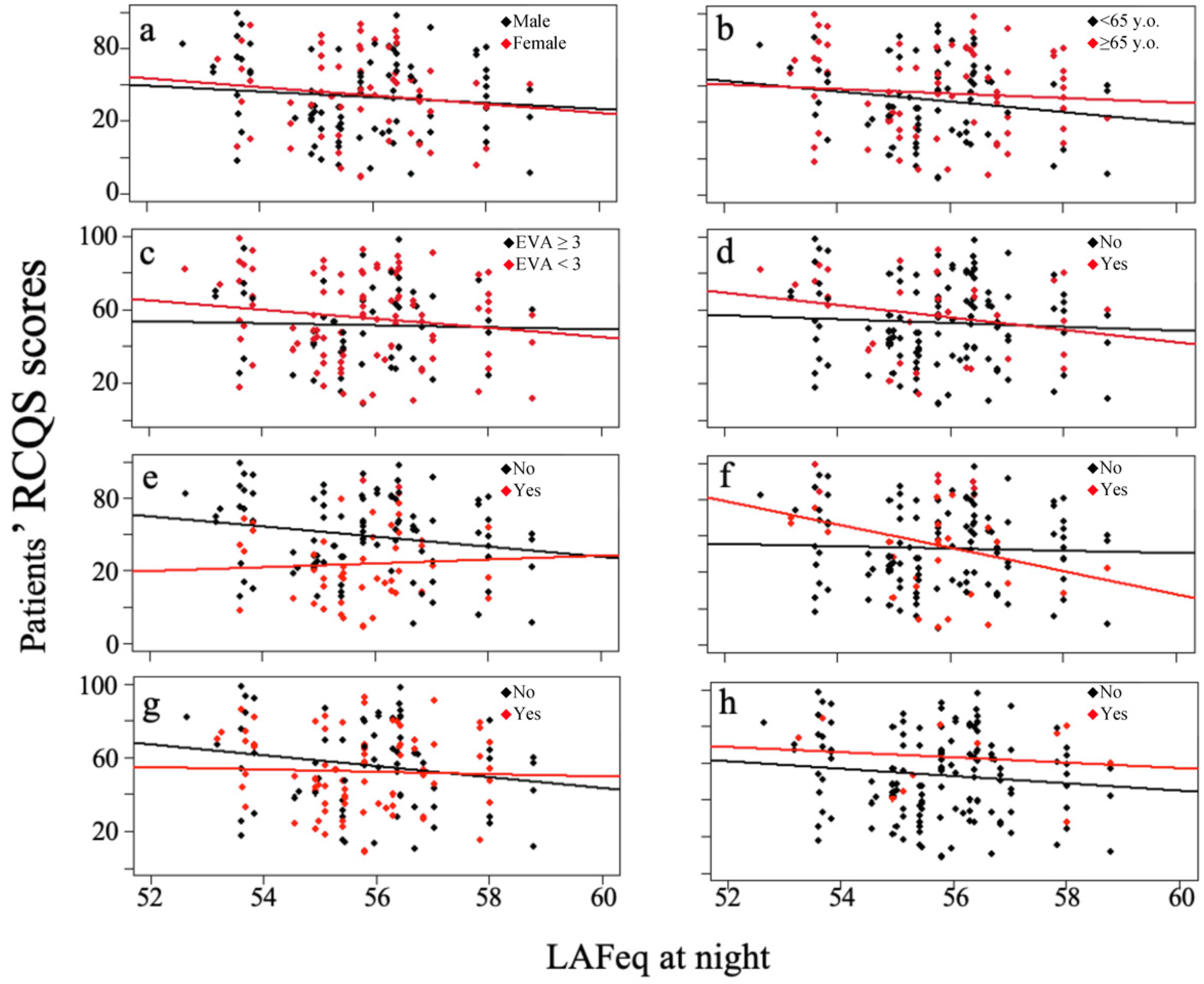
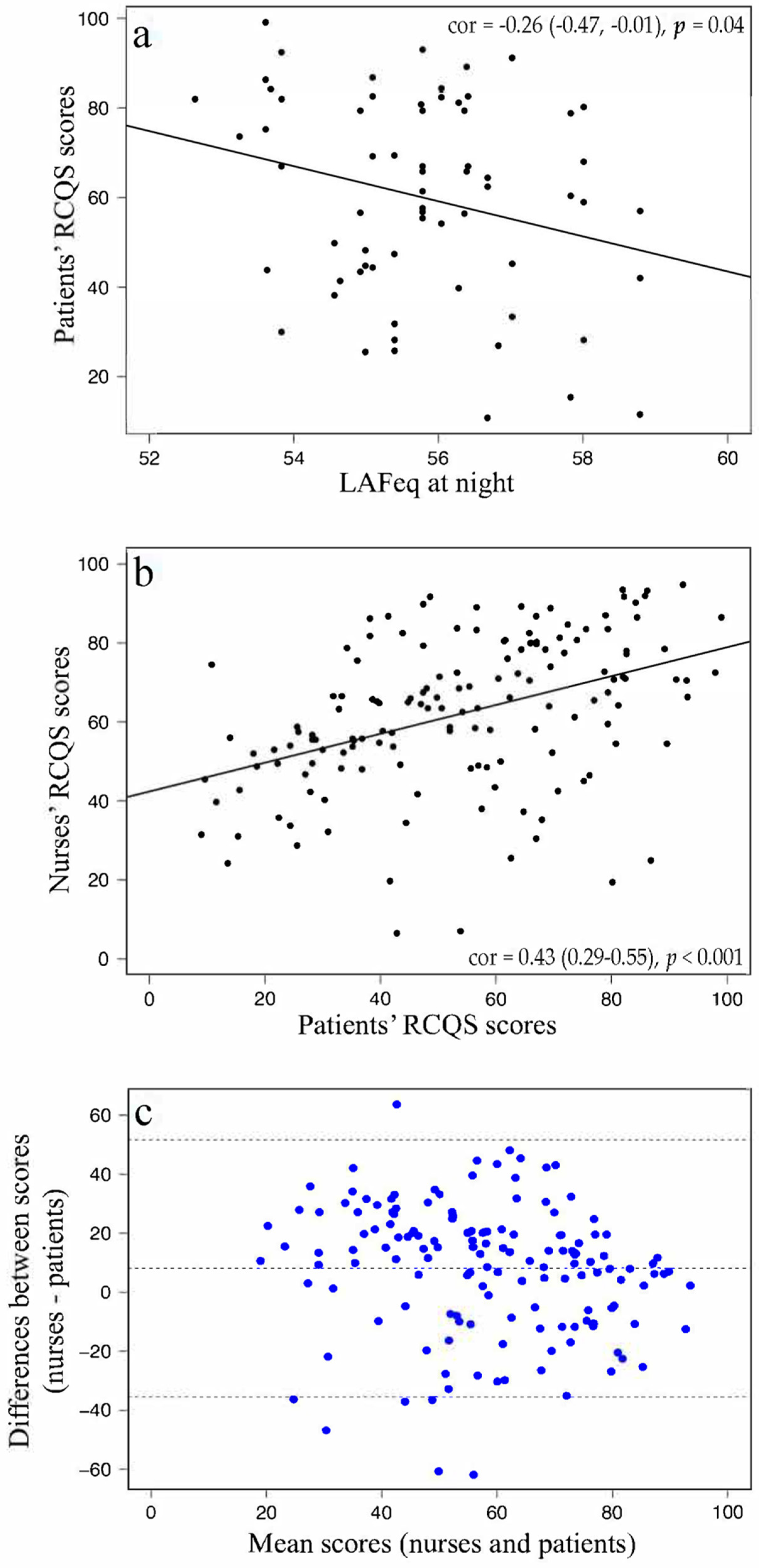
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
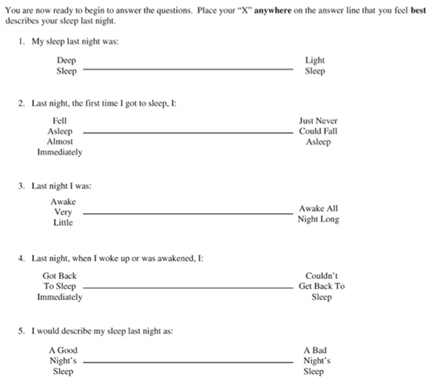
Appendix A
References
- Hilton, B.A. Quantity and Quality of Patients’ Sleep and Sleep-Disturbing Factors in a Respiratory Intensive Care Unit. J. Adv. Nurs. 1976, 1, 453–468. [Google Scholar] [CrossRef] [PubMed]
- Freedman, N.S.; Gazendam, J.; Levan, L.; Pack, A.I.; Schwab, R.J. Abnormal Sleep/Wake Cycles and the Effect of Environmental Noise on Sleep Disruption in the Intensive Care Unit. Am. J. Respir. Crit. Care Med. 2001, 163, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Aurell, J.; Elmqvist, D. Sleep in the Surgical Intensive Care Unit: Continuous Polygraphic Recording of Sleep in Nine Patients Receiving Postoperative Care. Br. Med. J. (Clin. Res. Ed.) 1985, 290, 1029–1032. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.B.; Thornley, K.S.; Young, G.B.; Slutsky, A.S.; Stewart, T.E.; Hanly, P.J. Sleep in Critically Ill Patients Requiring Mechanical Ventilation. Chest 2000, 117, 809–818. [Google Scholar] [CrossRef]
- Broughton, R.; Baron, R. Sleep Patterns in the Intensive Care Unit and on the Ward after Acute Myocardial Infarction. Electroencephalogr. Clin. Neurophysiol. 1978, 45, 348–360. [Google Scholar] [CrossRef]
- Bentley, S.; Murphy, F.; Dudley, H. Perceived Noise in Surgical Wards and an Intensive Care Area: An Objective Analysis. Br. Med. J. 1977, 2, 1503–1506. [Google Scholar] [CrossRef]
- Meyer, T.J.; Eveloff, S.E.; Bauer, M.S.; Schwartz, W.A.; Hill, N.S.; Millman, R.P. Adverse Environmental Conditions in the Respiratory and Medical ICU Settings. Chest 1994, 105, 1211–1216. [Google Scholar] [CrossRef]
- Redding, J.S.; Hargest, T.S.; Minsky, S.H. How Noisy Is Intensive Care? Crit. Care Med. 1977, 5, 275–276. [Google Scholar] [CrossRef]
- Telias, I.; Wilcox, M.E. Sleep and Circadian Rhythm in Critical Illness. Crit. Care 2019, 23, 2–5. [Google Scholar] [CrossRef]
- Beecroft, J.M.; Ward, M.; Younes, M.; Crombach, S.; Smith, O.; Hanly, P.J. Sleep Monitoring in the Intensive Care Unit: Comparison of Nurse Assessment, Actigraphy and Polysomnography. Intensive Care Med. 2008, 34, 2076–2083. [Google Scholar] [CrossRef]
- Friese, R.S.; Diaz-Arrastia, R.; McBride, D.; Frankel, H.; Gentilello, L.M. Quantity and Quality of Sleep in the Surgical Intensive Care Unit: Are Our Patients Sleeping? J. Trauma Inj. Infect. Crit. Care 2007, 63, 1210–1214. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.C.; French, D.G. Sleep and Healing in Intensive Care Settings. Dimens. Crit. Care Nurs. 1995, 14, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Edell-Gustafsson, U.M.; Gustavsson, G.; Yngman Uhlin, P. Effects of Sleep Loss in Men and Women with Insufficient Sleep Suffering from Chronic Disease: A Model for Supportive Nursing Care. Int. J. Nurs. Pract. 2003, 9, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Korompeli, A.; Muurlink, O.; Kavrochorianou, N.; Katsoulas, T.; Fildissis, G.; Baltopoulos, G. Circadian Disruption of ICU Patients: A Review of Pathways, Expression, and Interventions. J. Crit. Care 2017, 38, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Delaney, L.J.; Van Haren, F.; Lopez, V. Sleeping on a Problem: The Impact of Sleep Disturbance on Intensive Care Patients—A Clinical Review. Ann. Intensive Care 2015, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Hale, L.; Moore, M.; Patel, N.P. Mortality Associated with Short Sleep Duration: The Evidence, the Possible Mechanisms, and the Future. Sleep Med. Rev. 2010, 14, 191–203. [Google Scholar] [CrossRef]
- Gallicchio, L.; Kalesan, B. Sleep Duration and Mortality: A Systematic Review and Meta-Analysis. J. Sleep Res. 2009, 18, 148–158. [Google Scholar] [CrossRef]
- Friese, R.S.; Bruns, B.; Sinton, C.M. Sleep Deprivation After Septic Insult Increases Mortality Independent of Age. J. Trauma Inj. Infect. Crit. Care 2009, 66, 50–54. [Google Scholar] [CrossRef]
- Horsten, S.; Reinke, L.; Absalom, A.R.; Tulleken, J.E. Systematic Review of the Effects of Intensive-Care-Unit Noise on Sleep of Healthy Subjects and the Critically Ill. Br. J. Anaesth. 2018, 120, 443–452. [Google Scholar] [CrossRef]
- Elbaz, M.; Léger, D.; Sauvet, F.; Champigneulle, B.; Rio, S.; Strauss, M.; Chennaoui, M.; Guilleminault, C.; Mira, J.P. Sound Level Intensity Severely Disrupts Sleep in Ventilated ICU Patients throughout a 24-h Period: A Preliminary 24-h Study of Sleep Stages and Associated Sound Levels. Ann. Intensive Care 2017, 7, 25. [Google Scholar] [CrossRef]
- Freedman, N.S.; Kotzer, N.; Schwab, R.J. Patient Perception of Sleep Quality and Etiology of Sleep Disruption in the Intensive Care Unit. Am. J. Respir. Crit. Care Med. 1999, 159, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Kamdar, B.B.; Shah, P.A.; King, L.M.; Kho, M.E.; Zhou, X.; Colantuoni, E.; Collop, N.A.; Needham, D.M. Patient-Nurse Interrater Reliability and Agreement of the Richards-Campbell Sleep Questionnaire. Crit. Care Eval. 2012, 21, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Boyko, Y.; Ørding, H.; Jennum, P. Sleep Disturbances in Critically Ill Patients in ICU: How Much Do We Know? Acta Anaesthesiol. Scand. 2012, 56, 950–958. [Google Scholar] [CrossRef] [PubMed]
- Aitken, L.M.; Elliott, R.; Mitchell, M.; Davis, C.; Macfarlane, B.; Ullman, A.; Wetzig, K.; Datt, A.; McKinley, S. Sleep Assessment by Patients and Nurses in the Intensive Care: An Exploratory Descriptive Study. Aust. Crit. Care 2017, 30, 59–66. [Google Scholar] [CrossRef]
- Guisasola-Rabes, M.; Solà-Enriquez, B.; Vélez-Pereira, A.M.; De Nadal, M. Effectiveness of a Visual Noise Warning System on Noise Levels in a Surgical ICU: A Quality Improvement Programme. Eur. J. Anaesthesiol. 2019, 36, 857–862. [Google Scholar] [CrossRef]
- Simons, K.S.; Verweij, E.; Lemmens, P.M.C.; Jelfs, S.; Park, M.; Spronk, P.E.; Sonneveld, J.P.C.; Feijen, H.-M.; van der Steen, M.S.; Kohlrausch, A.G.; et al. Noise in the Intensive Care Unit and Its Influence on Sleep Quality: A Multicenter Observational Study in Dutch Intensive Care Units. Crit. Care 2018, 22, 250. [Google Scholar] [CrossRef]
- Garrido Galindo, A.P.; Camargo Caicedo, Y.; Velez-Pereira, A.M. Noise Level in a Neonatal Intensive Care Unit in Santa Marta—Colombia. Colomb. Med. 2017, 48, 120–125. [Google Scholar] [CrossRef]
- Fortes-Garrido, J.; Velez-Pereira, A.; Gázquez, M.; Hidalgo-Hidalgo, M.; Bolívar, J. The Characterization of Noise Levels in a Neonatal Intensive Care Unit and the Implications for Noise Management. J. Environ. Health Sci. Eng. 2014, 12, 104. [Google Scholar] [CrossRef]
- Shahid, A.; Wilkinson, K.; Marcu, S.; Shapiro, C.M. STOP, THAT and One Hundred Other Sleep Scales; Richards–Campbell Sleep Questionnaire (RCSQ); Springer: New York, NY, USA, 2011; ISBN 978-1-4419-9892-7. [Google Scholar]
- Le Guen, M.; Nicolas-Robin, A.; Lebard, C.; Arnulf, I.; Langeron, O. Earplugs and Eye Masks vs Routine Care Prevent Sleep Impairment in Post-Anaesthesia Care Unit: A Randomized Study. Br. J. Anaesth. 2014, 112, 89–95. [Google Scholar] [CrossRef]
- Jones, J.; Hoggart, B.; Withey, J.; Donaghue, K.; Ellis, B.W. What the Patients Say: A Study of Reactions to an Intensive Care Unit. Intensive Care Med. 1979, 5, 89–92. [Google Scholar] [CrossRef]
- Richardson, A.; Allsop, M.; Coghill, E.; Turnock, C. Earplugs and Eye Masks: Do They Improve Critical Care Patients’ Sleep? Nurs. Crit. Care 2007, 12, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Hweidi, I.M. Jordanian Patients’ Perception of Stressors in Critical Care Units: A Questionnaire Survey. Int. J. Nurs. Stud. 2007, 44, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Aaron, J.N.; Carlisle, C.C.; Carskadon, M.A.; Meyer, T.J.; Hill, N.S.; Millman, R.P. Environmental Noise as a Cause of Sleep Disruption in an Intermediate Respiratory Care Unit. Sleep 1996, 19, 707–710. [Google Scholar] [CrossRef]
- Sandoval, C.P. Nonpharmacological Interventions for Sleep Promotion in the Intensive Care Unit. Crit. Care Nurse 2017, 37, 100–102. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.; Jiang, X.; Zeng, Y.; Chen, X.; Zhang, Y. Effects of Earplugs and Eye Masks on Nocturnal Sleep, Melatonin and Cortisol in a Simulated Intensive Care Unit Environment. Crit. Care 2010, 14, R66. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.F.; Jiang, X.Y.; Hegadoren, K.M.; Zhang, Y.H. Effects of Earplugs and Eye Masks Combined with Relaxing Music on Sleep, Melatonin and Cortisol Levels in ICU Patients: A Randomized Controlled Trial. Crit. Care 2015, 19, 115. [Google Scholar] [CrossRef] [PubMed]
- Arık, E.; Dolgun, H.; Hanalioglu, S.; Sahin, O.S.; Ucar, F.; Yazicioglu, D.; Dogan, I.; Yilmaz, E.R. Prospective Randomized Study on the Effects of Improved Sleep Quality After Craniotomy on Melatonin Concentrations and Inflammatory Response in Neurosurgical Intensive Care Patients. World Neurosurg. 2020, 140, e253–e259. [Google Scholar] [CrossRef]
- Younis, M.B.; Hayajneh, F.; Batiha, A.M. Measurement and Nonpharmacologic Management of Sleep Disturbance in the Intensive Care Units: A Literature Review. Crit. Care Nurs. Q. 2019, 42, 75–80. [Google Scholar] [CrossRef]
- Fang, C.S.; Wang, H.H.; Wang, R.H.; Chou, F.H.; Chang, S.L.; Fang, C.J. Effect of Earplugs and Eye Masks on the Sleep Quality of Intensive Care Unit Patients: A Systematic Review and Meta-Analysis. J. Adv. Nurs. 2021, 77, 4321–4331. [Google Scholar] [CrossRef]
- Elysa, M.J.; Hinkley, N. NIH Public Access. Bone 2011, 72, 132–135. [Google Scholar] [CrossRef]
- Schwab, K.E.; Ronish, B.; Needham, D.M.; To, A.Q.; Martin, J.L.; Kamdar, B.B. Actigraphy to Evaluate Sleep in the Intensive Care Unit: A Systematic Review. Ann. Am. Thorac. Soc. 2018, 15, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Giménez, S.; Romero, S.; Alonso, J.F.; Mañanas, M.Á.; Pujol, A.; Baxarias, P.; Antonijoan, R.M. Monitoring Sleep Depth: Analysis of Bispectral Index (BIS) Based on Polysomnographic Recordings and Sleep Deprivation. J. Clin. Monit. Comput. 2017, 31, 103–110. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | |
|---|---|
| Patient characteristics | Patient included (n = 148) |
| Male sex (n; %) | 89; 60.1% |
| Age (mean ± SD) | 63 ± 15 year |
| Weight (mean ± SD) | 73 ± 16.8 kg |
| Height (mean ± SD) | 170 ± 8.9 cm |
| Type of surgery | |
| Abdominal (%) | 44.59 |
| Urologic (%) | 14.86 |
| Vascular: extremities/carotid (%) | 13.51 |
| Other (%) | 10.81 |
| Thoracic (%) | 9.46 |
| Spinal (%) | 5.41 |
| ENT or maxillofacial (%) | 1.35 |
| Surgery characteristics | |
| Urgent surgery, yes (%) | 23.7 |
| Nasogastric tube, yes (%) | 22.3 |
| Urinary catheter, yes (%) | 88.6 |
| Medical care | |
| Drain changes, yes (%) | 39.2 |
| Hypnotic drug administration, yes (%) | 36.5 |
| Initiate drinking water, yes (%) | 53.4 |
| Night hygiene, yes (%) | 71.0 |
| Postural changes, yes (%) | 33.4 |
| VAS pain score | |
| Maximum (mean ± SD) | (2.5 ± 2.8) |
| Minimum (mean ± SD) | (0.2 ± 0.6) |
| No. of hours VAS was >3 (mean ± SD) | (0.9 ± 1.5) |
| LAFeq | LAFpeak | LAFmin | LAF90 | LAFmax | |
|---|---|---|---|---|---|
| Mean | 57.3 dB | 75.6 dB | 52.1 dB | 52.7 dB | 61.6 dB |
| Median | 58.3 dB | 76.6 dB | 52.7 dB | 53.3 dB | 62.7 dB |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guisasola-Rabes, M.; Solà-Enriquez, B.; Vélez-Pereira, A.M.; de Nadal, M. Noise Levels and Sleep in a Surgical ICU. J. Clin. Med. 2022, 11, 2328. https://doi.org/10.3390/jcm11092328
Guisasola-Rabes M, Solà-Enriquez B, Vélez-Pereira AM, de Nadal M. Noise Levels and Sleep in a Surgical ICU. Journal of Clinical Medicine. 2022; 11(9):2328. https://doi.org/10.3390/jcm11092328
Chicago/Turabian StyleGuisasola-Rabes, Maria, Berta Solà-Enriquez, Andrés M. Vélez-Pereira, and Miriam de Nadal. 2022. "Noise Levels and Sleep in a Surgical ICU" Journal of Clinical Medicine 11, no. 9: 2328. https://doi.org/10.3390/jcm11092328
APA StyleGuisasola-Rabes, M., Solà-Enriquez, B., Vélez-Pereira, A. M., & de Nadal, M. (2022). Noise Levels and Sleep in a Surgical ICU. Journal of Clinical Medicine, 11(9), 2328. https://doi.org/10.3390/jcm11092328






