Incidence, Size and Orientation of Maxillary Sinus Septa—A Retrospective Clinical Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
- -
- Age > 18 years, with no other age or gender restrictions;
- -
- Partial (hemimaxilla) or total CBCTs comprising at least 2/3 of the floor of the sinus cavity;
- -
- CBCTs of the upper arch.
- -
- CBCTs with exposure errors (because of patient’s movement, other artefacts);
- -
- Maxillary sinus cavities with previous sinus grafts;
- -
- CBCTs which do not comprise entirely, anteroposteriorly the sinus cavity;
- -
- CBCTs with a field of view of 40 × 40 (for endodontic purposes);
- -
- Absence of patient’s informed consent;
- -
- Panoramic radiographies.
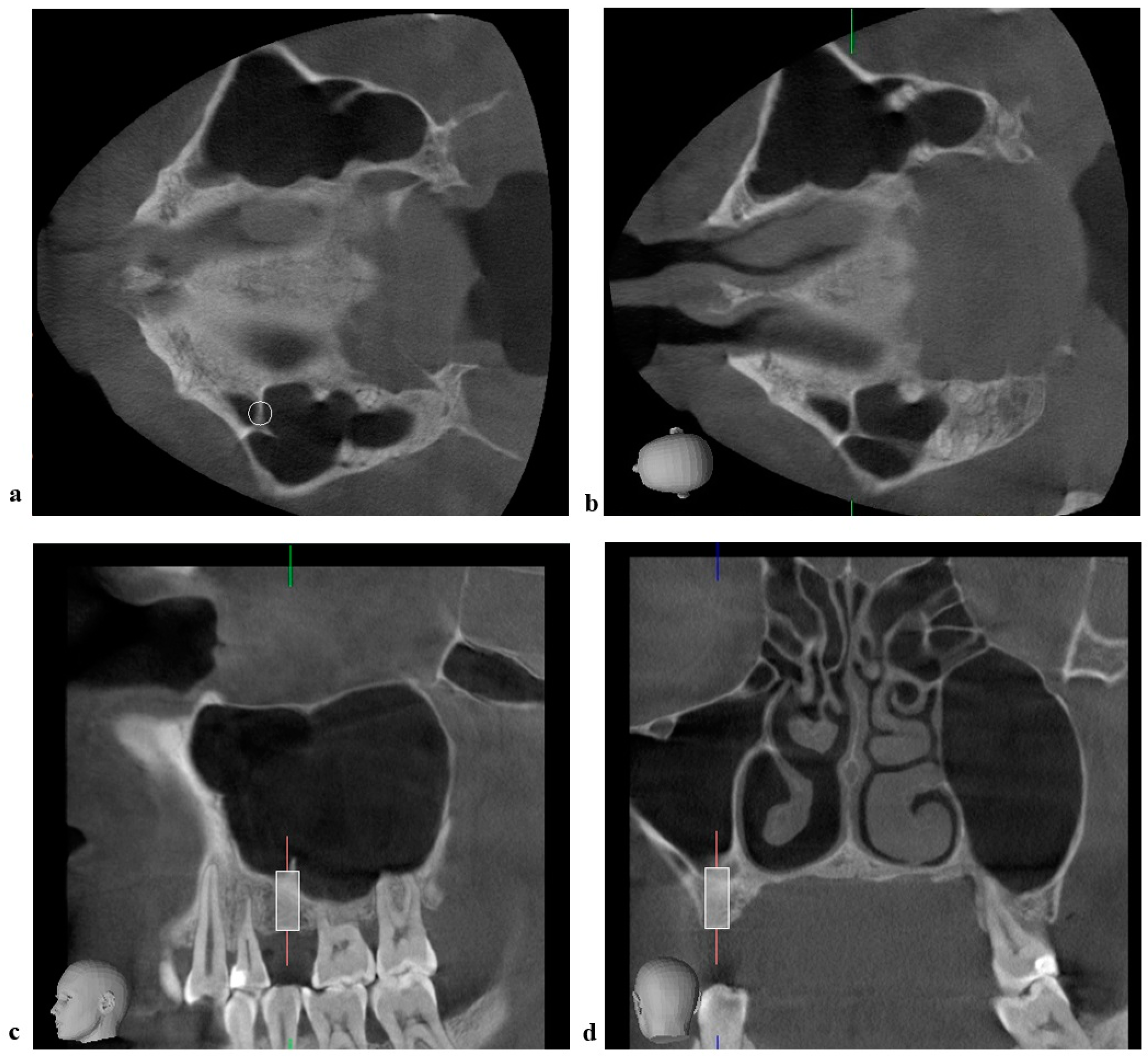
2.3. Radiographic Measurements
2.4. Statistical Analysis
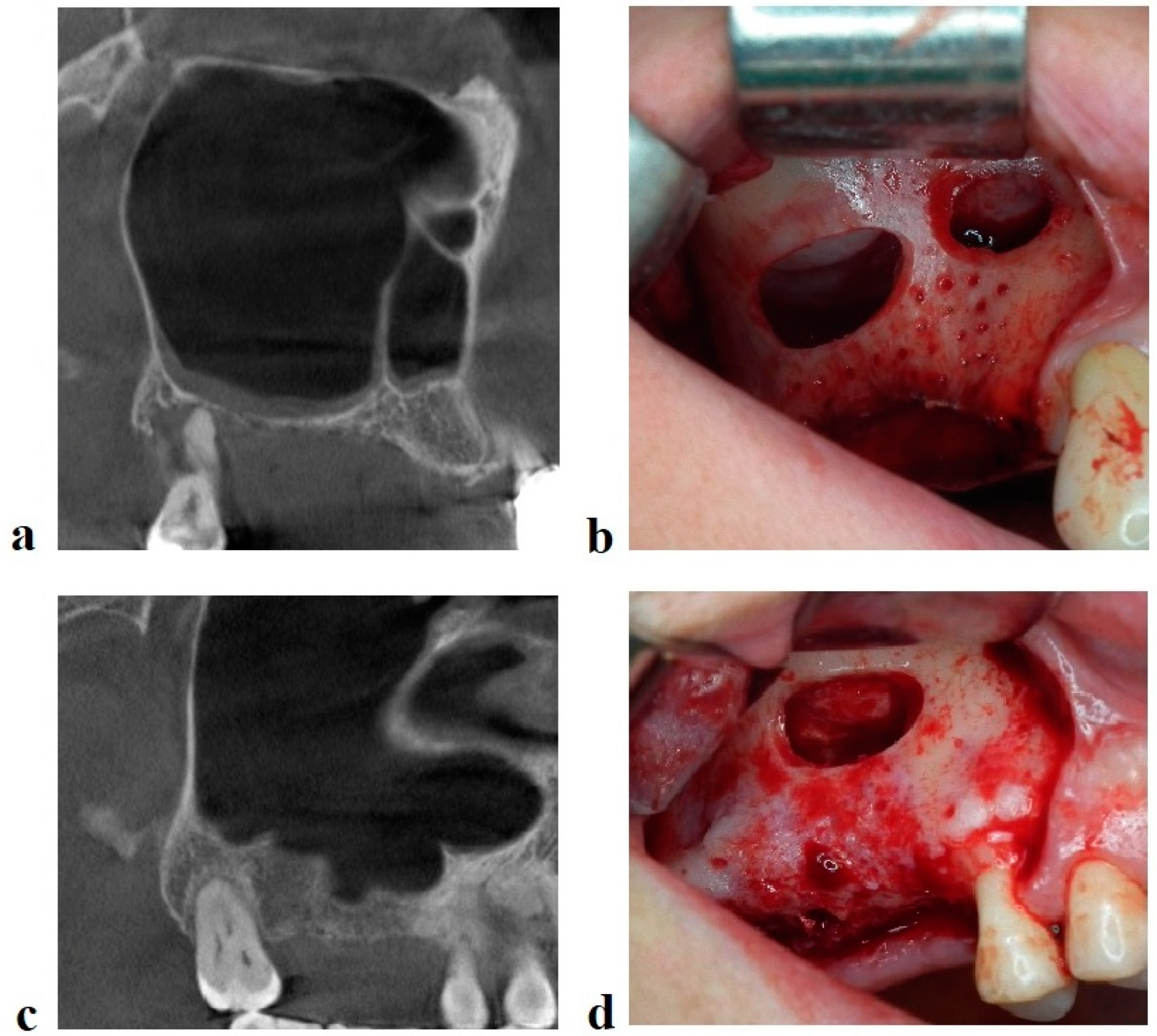
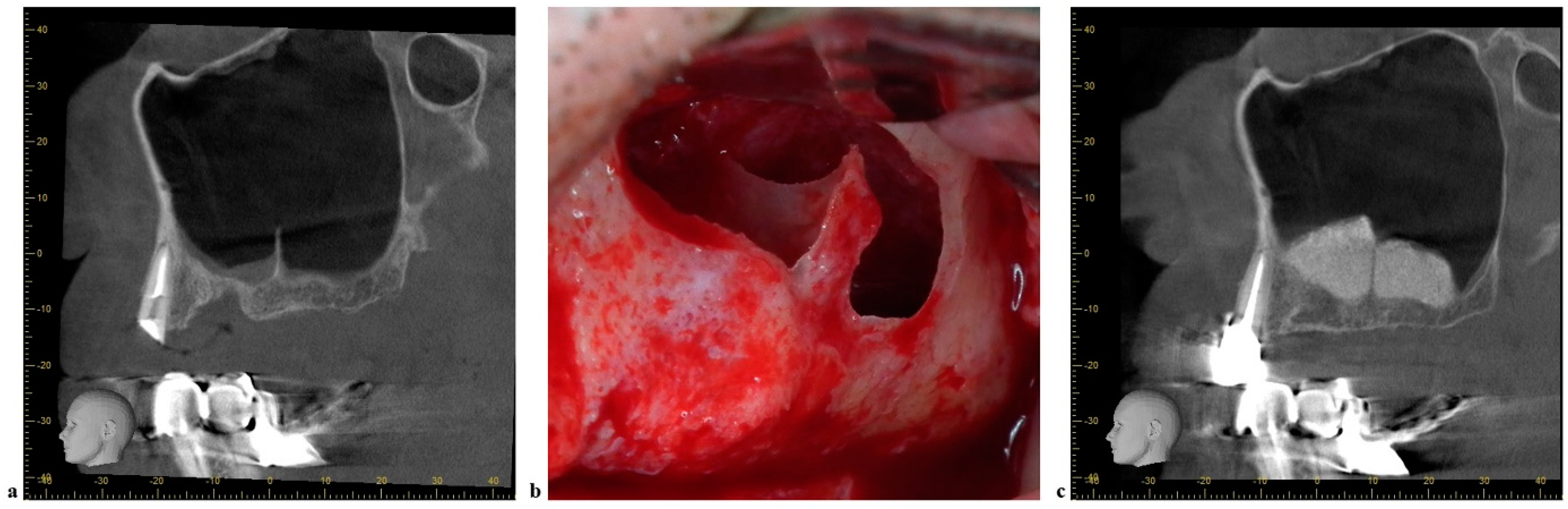
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wen, S.C.; Chan, H.L.; Wang, H.L. Classification and management of antral septa for maxillary sinus augmentation. Int. J. Periodontics Restor. Dent. 2013, 33, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Aşantoğrol, F.; Coşgunarslan, A. The effect of anatomical variations of the sinonasal region on maxillary sinus volume and dimensions: A three-dimensional study. Braz. J. Otorhinolaryngol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Whyte, A.; Boeddinghaus, R. The maxillary sinus: Physiology, development and imaging anatomy. Dentomaxillo Facial Radiol. 2019, 48, 20190205. [Google Scholar] [CrossRef] [PubMed]
- Malec, M.; Smektała, T.; Trybek, G.; Sporniak-Tutak, K. Maxillary sinus septa: Prevalence, morphology, diagnostics and implantological implications. Systematic review. Folia Morphol. 2013, 73, 259–266. [Google Scholar] [CrossRef]
- Tadinada, A.; Jalali, E.; Al-Salman, W.; Jambhekar, S.; Katechia, B.; Almas, K. Prevalence of bony septa, antral pathology, and dimensions of the maxillary sinus from a sinus augmentation perspective: A retrospective cone-beam computed tomography study. Imaging Sci. Dent. 2016, 46, 109–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reda, R.; Zanza, A.; Mazzoni, A.; Cicconetti, A.; Testarelli, L.; Di Nardo, D. An Update of the Possible Applications of Magnetic Resonance Imaging (MRI) in Dentistry: A Literature Review. J. Imaging 2021, 7, 75. [Google Scholar] [CrossRef]
- Patil, S.; Alkahtani, A.; Bhandi, S.; Mashyakhy, M.; Alvarez, M.; Alroomy, R.; Hendi, A.; Varadarajan, S.; Reda, R.; Raj, A.T.; et al. Ultrasound Imaging versus Radiographs in Differentiating Periapical Lesions: A Systematic Review. Diagnostics 2021, 11, 1208. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.C.; Sheng, C.; Ho, C.Y. Efficacy of sinus ultrasound in diagnosis of acute and subacute maxillary sinusitis. J. Chin. Med. Assoc. 2018, 81, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Shokri, A.; Jamalpour, M.; Jafariyeh, B.; Poorolajal, J.; Sabet, N.K. Comparison of Ultrasonography, Magnetic Resonance Imaging and Cone Beam Computed Tomography for Detection of Foreign Bodies in Maxillofacial Region. J. Clin. Diagn. Res. 2017, 11, TC15–TC19. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, K.; Sakamoto, Y.; Naruse, T.; Kawakita, A.; Yanamoto, S.; Furukawa, K.; Umeda, M. Intraoral extraction of an ectopic mandibular third molar detected in the subcondylar region without a pathological cause: A case report and literature review. CRANIO®—J. Craniomandib. Sleep Pract. 2017, 35, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, L.; Schiebel, V.; Hof, M.; Ulm, C.; Watzek, G.; Pommer, B. Risk Factors of Membrane Perforation and Postoperative Complications in Sinus Floor Elevation Surgery: Review of 407 Augmentation Procedures. J. Oral Maxillofac. Surg. 2015, 73, 1275–1282. [Google Scholar] [CrossRef]
- Qian, L.; Tian, X.M.; Zeng, L.; Gong, Y.; Wei, B. Analysis of the Morphology of Maxillary Sinus Septa on Reconstructed Cone-Beam Computed Tomography Images. J. Oral Maxillofac. Surg. 2016, 74, 729–737. [Google Scholar] [CrossRef]
- Jang, S.Y.; Chung, K.; Jung, S.; Park, H.J.; Oh, H.K.; Kook, M.S. Comparative study of the sinus septa between dentulous and edentulous patients by cone beam computed tomography. Implant Dent. 2014, 23, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Barbu, H.M.; Iancu, S.A.; Jarjour Mirea, I.; Mignogna, M.D.; Samet, N.; Calvo-Guirado, J.L. Management of Schneiderian Membrane Perforations during Sinus Augmentation Procedures: A Preliminary Comparison of Two Different Approaches. J. Clin. Med. 2019, 8, 1491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bathla, S.C.; Fry, R.R.; Majumdar, K. Maxillary sinus augmentation. J. Indian Soc. Periodontol. 2018, 22, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Stacchi, C.; Lombardi, T.; Cusimano, P.; Berton, F.; Lauritano, F.; Cervino, G.; Di Lenarda, R.; Cicciù, M. Bone Scrapers Versus Piezoelectric Surgery in the Lateral Antrostomy for Sinus Floor Elevation. J. Craniofac. Surg. 2017, 28, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Al-Dajani, M. Incidence, Risk Factors, and Complications of Schneiderian Membrane Perforation in Sinus Lift Surgery: A Meta-Analysis. Implant Dent. 2016, 25, 409–415. [Google Scholar] [CrossRef] [PubMed]
- von Arx, T.; Fodich, I.; Bornstein, M.M.; Jensen, S.S. Perforation of the sinus membrane during sinus floor elevation: A retrospective study of frequency and possible risk factors. Int. J. Oral Maxillofac. Implant. 2014, 29, 718–726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sigaroudi, A.K.; Kajan, Z.D.; Rastgar, S.; Asli, H.N. Frequency of different maxillary sinus septal patterns found on cone-beam computed tomography and predicting the associated risk of sinus membrane perforation during sinus lifting. Imaging Sci. Dent. 2017, 47, 261–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tükel, H.C.; Tatli, U. Risk factors and clinical outcomes of sinus membrane perforation during lateral window sinus lifting: Analysis of 120 patients. Int. J. Oral Maxillofac. Surg. 2018, 47, 1189–1194. [Google Scholar] [CrossRef] [PubMed]
- Marin, S.; Kirnbauer, B.; Rugani, P.; Payer, M.; Jakse, N. Potential risk factors for maxillary sinus membrane perforation and treatment outcome analysis. Clin. Implant Dent. Relat. Res. 2019, 21, 66–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krennmair, S.; Malek, M.; Forstner, T.; Krennmair, G.; Weinländer, M.; Hunger, S. Risk Factor Analysis Affecting Sinus Membrane Perforation During Lateral Window Maxillary Sinus Elevation Surgery. Int. J. Oral Maxillofac. Implant. 2020, 35, 789–798. [Google Scholar] [CrossRef]
- Pizzini, A.; Basma, H.S.; Li, P.; Geurs, N.C.; Abou-Arraj, R.V. The impact of anatomic, patient and surgical factors on membrane perforation during lateral wall sinus floor elevation. Clin. Oral Implants Res. 2021, 32, 274–284. [Google Scholar] [CrossRef] [PubMed]
- Testori, T.; Yu, S.H.; Tavelli, L.; Wang, H.L. Perforation Risk Assessment in Maxillary Sinus Augmentation with Lateral Wall Technique. Int. J. Periodontics Restor. Dent. 2020, 40, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, S.; Zamiri, B.; Danaei, S.M.; Salehi, S.; Hamedani, S. Evaluation of Anatomic Variations in Maxillary Sinus with the Aid of Cone Beam Computed Tomography (CBCT) in a Population in South of Iran. J. Dent. 2016, 17, 7–15. [Google Scholar]
- Orhan, K.; Seker, B.K.; Aksoy, S.; Bayindir, H.; Berberoğlu, A.; Seker, E. Cone beam CT evaluation of maxillary sinus septa prevalence, height, location and morphology in children and an adult population. Med. Princ. Pract. 2013, 22, 47–53. [Google Scholar] [CrossRef]
- Dobele, I.; Kise, L.; Apse, P.; Kragis, G.; Bigestans, A. Radiographic assessment of findings in the maxillary sinus using cone-beam computed tomography. Stomatologija 2013, 15, 119–122. [Google Scholar] [PubMed]
- Lana, J.P.; Carneiro, P.M.; Machado, V.; de Souza, P.E.; Manzi, F.R.; Horta, M.C. Anatomic variations and lesions of the maxillary sinus detected in cone beam computed tomography for dental implants. Clin. Oral Implant. Res. 2012, 23, 1398–1403. [Google Scholar] [CrossRef] [PubMed]
- Nasseh, I.; Aoun, G.; El-Outa, A.; Nassar, J.; Nasseh, P.; Hayek, E. Mapping Maxillary Sinus Septa in a Lebanese Sample: A Radio-anatomical Study. Acta Inform. Med. 2020, 28, 214–218. [Google Scholar] [CrossRef]
- Faramarzie, M.; Babaloo, A.R.; Oskouei, S.G. Prevalence, height, and location of antral septa in Iranian patients undergoing maxillary sinus lift. J. Adv. Periodontol. Implant. Dent. 2009, 1, 43–47. [Google Scholar]
- Demirkol, M.; Demirkol, N. The effects of posterior alveolar bone height on the height of maxillary sinus septa. Surg. Radiol. Anat. 2019, 41, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, M.M.; Seiffert, C.; Maestre-Ferrín, L.; Fodich, I.; Jacobs, R.; Buser, D.; von Arx, T. An Analysis of Frequency, Morphology, and Locations of Maxillary Sinus Septa Using Cone Beam Computed Tomography. Int. J. Oral Maxillofac. Implant. 2016, 31, 280–287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Zahrani, M.S.; Al-Ahmari, M.M.; Al-Zahrani, A.A.; Al-Mutairi, K.D.; Zawawi, K.H. Prevalence and morphological variations of maxillary sinus septa in different age groups: A CBCT analysis. Ann. Saudi Med. 2020, 40, 200–206. [Google Scholar] [CrossRef]
- Yildirim, T.T.; Güncü, G.N.; Colak, M.; Nares, S.; Tözüm, T.F. Evaluation of maxillary sinus septa: A retrospective clinical study with cone beam computerized tomography (CBCT). Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 5306–5314. [Google Scholar]
- Schriber, M.; von Arx, T.; Sendi, P.; Jacobs, R.; Suter, V.G.; Bornstein, M.M. Evaluating Maxillary Sinus Septa Using Cone Beam Computed Tomography: Is There a Difference in Frequency and Type Between the Dentate and Edentulous Posterior Maxilla? Int. J. Oral Maxillofac. Implant. 2017, 32, 1324–1332. [Google Scholar] [CrossRef] [PubMed]
- Takeda, D.; Hasegawa, T.; Saito, I.; Arimoto, S.; Akashi, M.; Komori, T. A radiologic evaluation of the incidence and morphology of maxillary sinus septa in Japanese dentate maxillae. Oral Maxillofac. Surg. 2019, 23, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Park, J.S.; Hong, S.J.; Kim, G.T.; Kwon, Y.D. Axial Triangle of the Maxillary Sinus, and its Surgical Implication With the Position of Maxillary Sinus Septa During Sinus Floor Elevation: A CBCT Analysis. J. Oral Implant. 2020, 46, 415–422. [Google Scholar] [CrossRef]
- Toprak, M.E.; Ataç, M.S. Maxillary sinus septa and anatomical correlation with the dentition type of sinus region: A cone beam computed tomographic study. Br. J. Oral Maxillofac. Surg. 2021, 59, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Rancitelli, D.; Borgonovo, A.E.; Cicciù, M.; Re, D.; Rizza, F.; Frigo, A.C.; Maiorana, C. Maxillary Sinus Septa and Anatomic Correlation With the Schneiderian Membrane. J. Craniofac. Surg. 2015, 26, 1394–1398. [Google Scholar] [CrossRef] [PubMed]
- Sakhdari, S.; Panjnoush, M.; Eyvazlou, A.; Niktash, A. Determination of the Prevalence, Height, and Location of the Maxillary Sinus Septa Using Cone Beam Computed Tomography. Implant Dent. 2016, 25, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.Z.; Xie, Y.F.; Xie, H.; Wang, G.H.; He, J.C. Cone-beam CT study of bone septa during maxillary sinus lift among Changzhou population. Shanghai J. Stomatol. 2016, 25, 77–81. [Google Scholar]
- Taleghani, F.; Tehranchi, M.; Shahab, S.; Zohri, Z. Prevalence, Location, and Size of Maxillary Sinus Septa: Computed Tomography Scan Analysis. J. Contemp. Dent. Pract. 2017, 18, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Shen, E.C.; Fu, E.; Chiu, T.J.; Chang, V.; Chiang, C.Y.; Tu, H.P. Prevalence and location of maxillary sinus septa in the Taiwanese population and relationship to the absence of molars. Clin. Oral Implant. Res. 2012, 23, 741–745. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.J.; Shin, S.I.; Herr, Y.; Kwon, Y.H.; Kim, G.T.; Chung, J.H. Anatomical structures in the maxillary sinus related to lateral sinus elevation: A cone beam computed tomographic analysis. Clin. Oral Implant. Res. 2013, 24, 75–81. [Google Scholar] [CrossRef]
- Li, J.; Zhou, Z.X.; Yuan, Z.Y.; Yuan, H.; Sun, C.; Chen, N. An anatomical study of maxillary sinus septum of Han population in Jiangsu region using cone-beam CT. Shanghai J. Stomatol. 2013, 22, 52–57. [Google Scholar]
- Hungerbühler, A.; Rostetter, C.; Lübbers, H.T.; Rücker, M.; Stadlinger, B. Anatomical characteristics of maxillary sinus septa visualized by cone beam computed tomography. Int. J. Oral Maxillofac. Surg. 2019, 48, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Irinakis, T.; Dabuleanu, V.; Aldahlawi, S. Complications During Maxillary Sinus Augmentation Associated with Interfering Septa: A New Classification of Septa. Open Dent. J. 2017, 11, 140–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okada, T.; Kawana, H. Two-Step Procedure for the Treatment of a Maxillary Sinus with Complex Sinus Septa: A Highly Predictive Method for Sinus Floor Augmentation After Perforation of the Maxillary Sinus Membrane. Int. J. Periodontics Restor. Dent. 2019, 39, e175–e180. [Google Scholar] [CrossRef]
- Martins, M.; Vieira, W.A.; Paranhos, L.R.; Motta, R.H.; da Silva, C.S.; Rodriguez, C.; Ramacciato, J.C. Comparison of piezosurgery and conventional rotary instruments in schneider’s membrane sinus lifting: A pilot randomized trial. J. Clin. Exp. Dent. 2021, 13, e802–e808. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Hwang, B.Y.; Kim, B.S.; Lee, J.W. Floating septum technique: Easy and safe method maxillary sinus septa in sinus lifting procedure. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 54. [Google Scholar] [CrossRef] [PubMed]
- Osman, A.H.; Mansour, H.; Atef, M.; Hakam, M. Computer guided sinus floor elevation through lateral window approach with simultaneous implant placement. Clin. Implant Dent. Relat. Res. 2018, 20, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, K.N.; Sakurada, M.A.; Philippi, A.G.; Gonçalves, T. Use of a stackable surgical guide to improve the accuracy of the lateral wall approach for sinus grafting in the presence of a sinus septum. Int. J. Oral Maxillofac. Surg. 2021, 50, 1383–1385. [Google Scholar] [CrossRef] [PubMed]

| No. Sinuses | Incidence of Septa | |
|---|---|---|
| Completely dentate patients (group A) | 192 | 38.54% |
| Single edentulism (group B) | 320 | 47.19% |
| Partial edentulism (group C) | 596 | 42.62% |
| Total edentulism (group D) | 84 | 32.14% |
| Wen Sinus Septum Classification | Number of Sinuses | Percentage |
|---|---|---|
| Easy/A | 77 | 15.28% |
| Easy/B | 34 | 6.75% |
| Medium/A | 161 | 31.94% |
| Medium/B | 73 | 14.48% |
| Difficult/A | 35 | 6.95% |
| Difficult/B | 18 | 3.57% |
| Difficult/C | 106 | 21.03% |
| Classification | Subclass | Location | Number | Orientation | Size (mm) | Proposed Treatment Approach |
|---|---|---|---|---|---|---|
| (D) Difficult | A | Anterior or posterior to zygomatic process | ≥2 | Medio-lateral | Multiple windows and/or wall-gone technique | |
| B | 1 | Antero-posterior | ≤6 | One window from the lateral approach | ||
| Highly Difficult (HD) | A | Anterior or posterior to zygomatic process | 1 | Antero-posterior | >6 | One window from the crestal approach & the wall gone technique |
| B | Combination of medio-lateral and antero-posterior septa | One window from the lateral approach and removal of the septum; most likely second surgery for sinus floor augmentation |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schiller, L.A.; Barbu, H.M.; Iancu, S.A.; Brad, S. Incidence, Size and Orientation of Maxillary Sinus Septa—A Retrospective Clinical Study. J. Clin. Med. 2022, 11, 2393. https://doi.org/10.3390/jcm11092393
Schiller LA, Barbu HM, Iancu SA, Brad S. Incidence, Size and Orientation of Maxillary Sinus Septa—A Retrospective Clinical Study. Journal of Clinical Medicine. 2022; 11(9):2393. https://doi.org/10.3390/jcm11092393
Chicago/Turabian StyleSchiller, Laura Andreea, Horia Mihail Barbu, Stefania Andrada Iancu, and Silviu Brad. 2022. "Incidence, Size and Orientation of Maxillary Sinus Septa—A Retrospective Clinical Study" Journal of Clinical Medicine 11, no. 9: 2393. https://doi.org/10.3390/jcm11092393
APA StyleSchiller, L. A., Barbu, H. M., Iancu, S. A., & Brad, S. (2022). Incidence, Size and Orientation of Maxillary Sinus Septa—A Retrospective Clinical Study. Journal of Clinical Medicine, 11(9), 2393. https://doi.org/10.3390/jcm11092393







