ENDO_STAGE Magnetic Resonance Imaging: Classification to Screen Endometriosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. MRI Technique
2.3. MRI Evaluation
2.4. Surgical and Pathological Findings
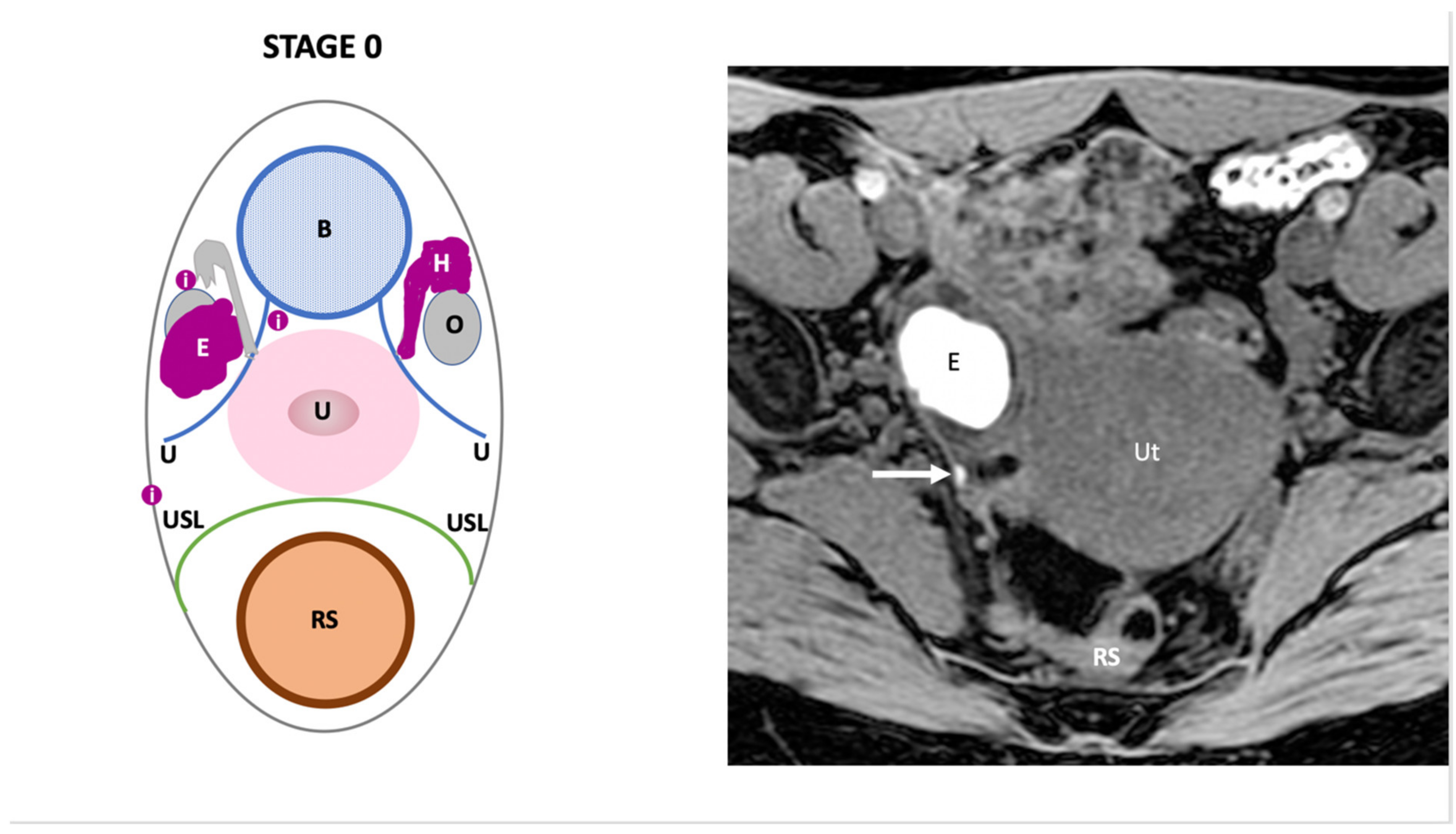
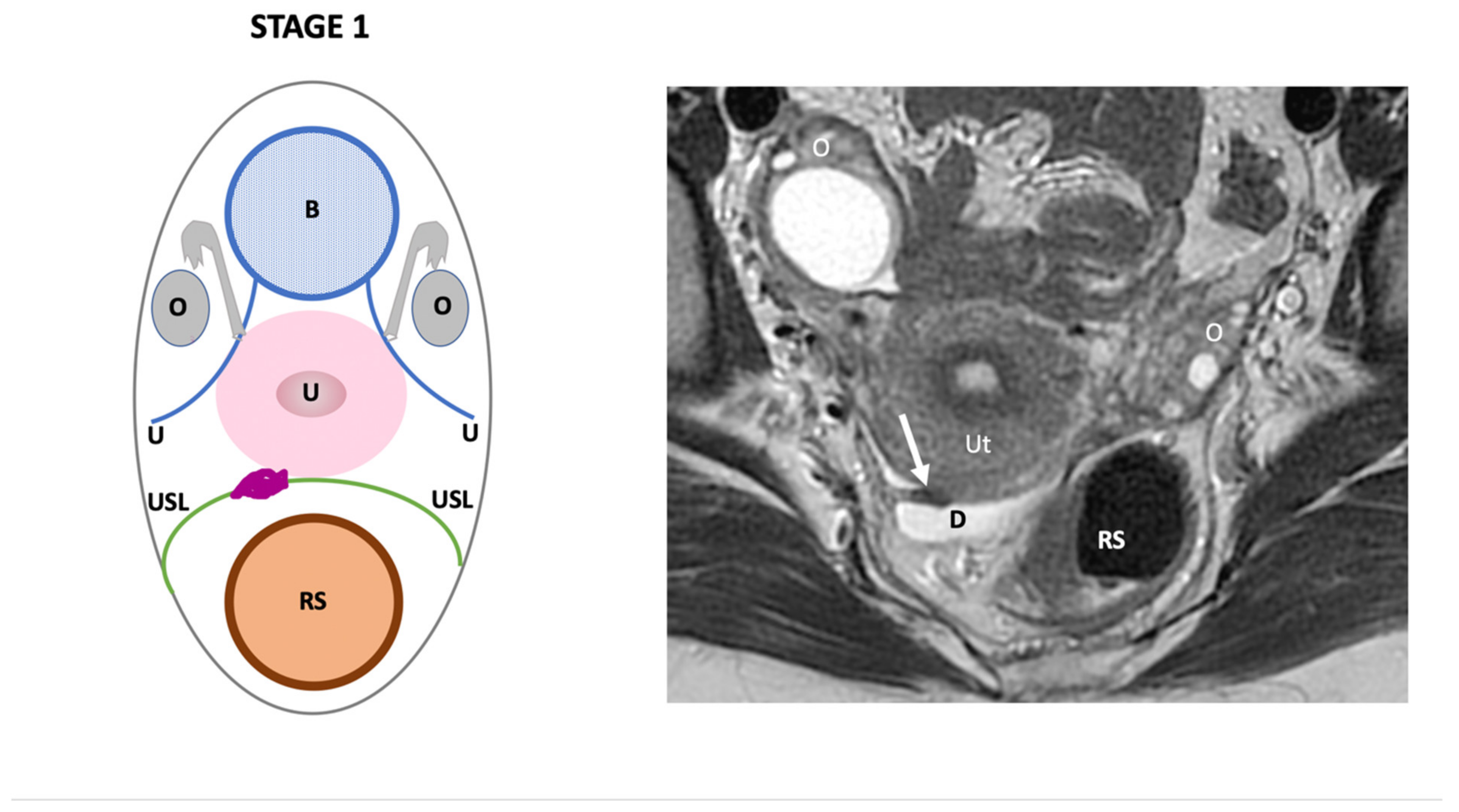
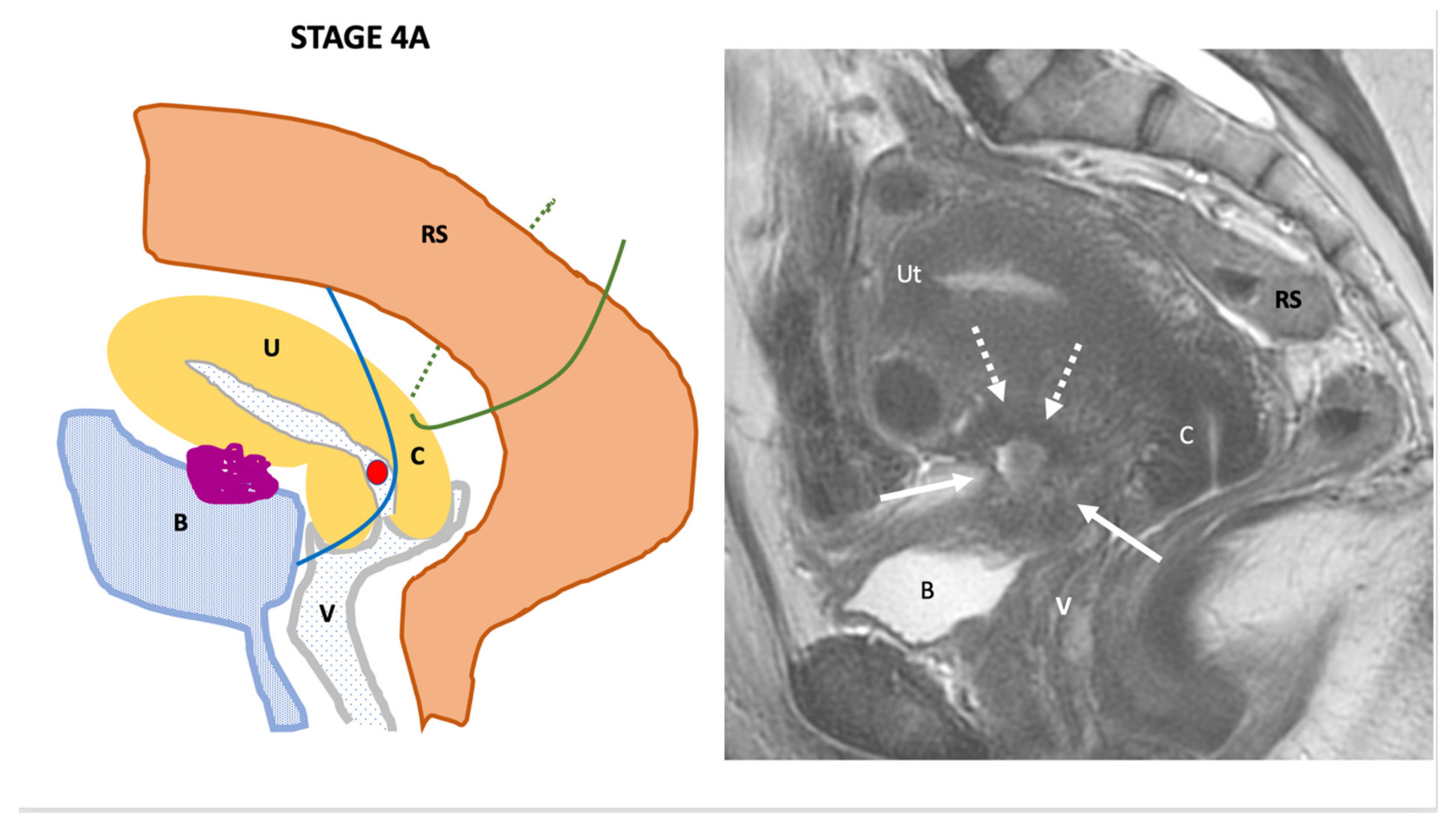
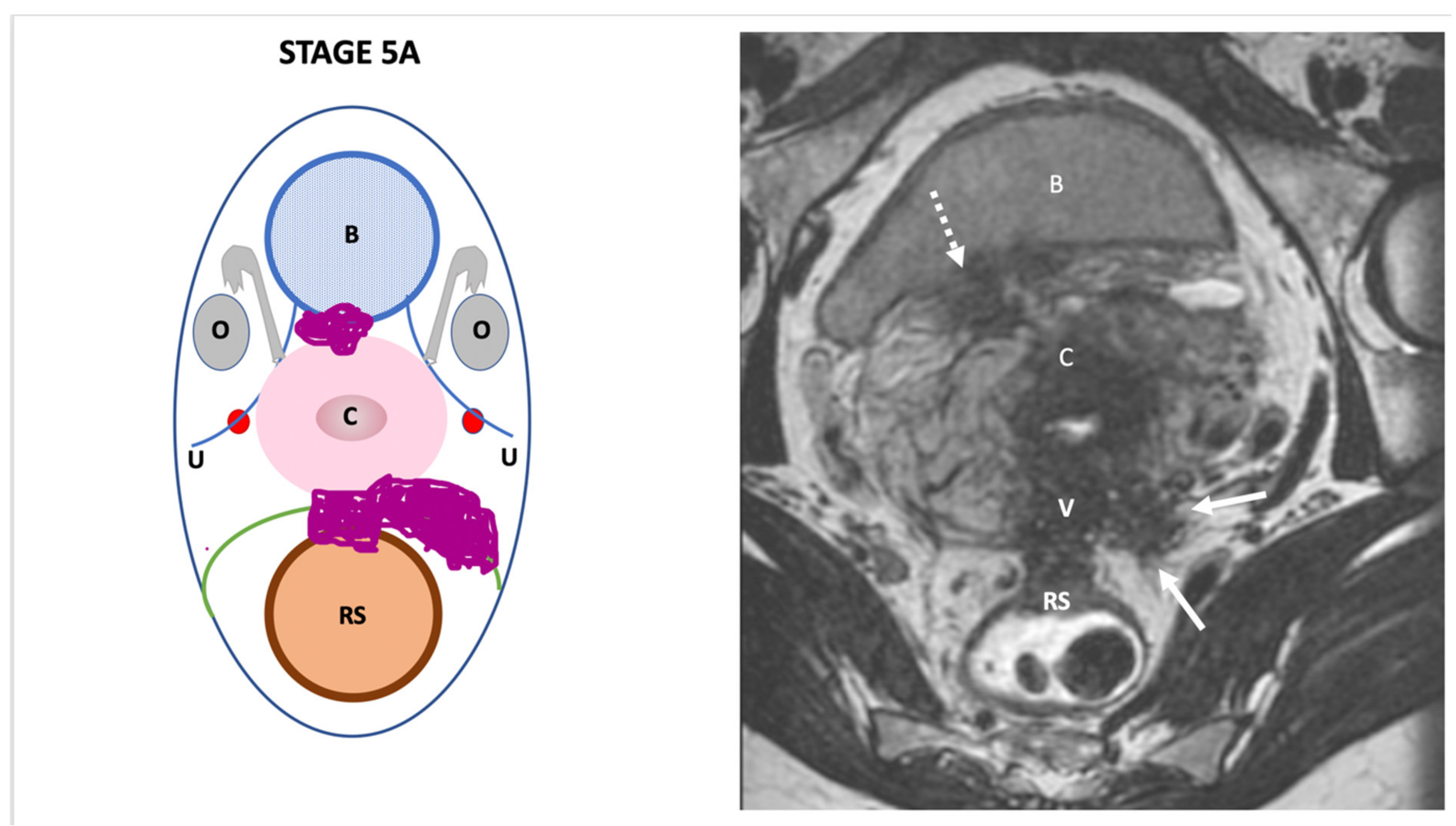
3. The Endo-Stage Mri Classification
4. Statistical Analysis
4.1. End Points
4.2. Predictive Value
4.3. Comparison of Classifications
5. Results
5.1. Epidemiological and Surgical Characteristics of the Population
5.2. Complications Rates According to Endo-Stage MRI Classification and System of Triage
5.3. Accuracy
5.3.1. Predictive Value of Endo-Stage MRI Classification
5.3.2. Endo-Stage MRI and rASRM Classifications
6. Comment
6.1. Principal Findings
6.2. Results in the Context of What Is Known
6.3. Clinical Implications
6.4. Research Implications
6.5. Strengths and Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Vercellini, P.; Aimi, G.; Panazza, S.; Vicentini, S.; Pisacreta, A.; Crosignani, P.G. Deep endometriosis conundrum: Evidence in favor of a peritoneal origin. Fertil. Steril. 2000, 73, 1043–1046. [Google Scholar] [CrossRef]
- Parazzini, F.; Roncella, E.; Cipriani, S.; Trojano, G.; Barbera, V.; Herranz, B.; Colli, E. The frequency of endometriosis in the general and selected populations: A systematic review. J. Endometr. Pelvic Pain Disord. 2020, 12, 176–189. [Google Scholar] [CrossRef]
- Bazot, M.; Lafont, C.; Rouzier, R.; Roseau, G.; Thomassin-Naggara, I.; Daraï, E. Diagnostic accuracy of physical examination, transvaginal sonography, rectal endoscopic sonography, and magnetic resonance imaging to diagnose deep infiltrating endometriosis. Fertil. Steril. 2009, 92, 1825–1833. [Google Scholar] [CrossRef] [PubMed]
- Celli, V.; Ciulla, S.; Dolciami, M.; Satta, S.; Ercolani, G.; Porpora, M.G.; Catalano, C.; Manganaro, L. Magnetic Resonance Imaging in endometriosis-associated pain. Minerva Obstet. Gynecol. 2021, 73. [Google Scholar] [CrossRef]
- Tong, A.; VanBuren, W.M.; Chamié, L.; Feldman, M.; Hindman, N.; Huang, C.; Jha, P.; Kilcoyne, A.; Laifer-Narin, S.; Nicola, R.; et al. Recommendations for MRI technique in the evaluation of pelvic endometriosis: Consensus statement from the Society of Abdominal Radiology endometriosis disease-focused panel. Abdom. Radiol. 2020, 45, 1569–1586. [Google Scholar] [CrossRef]
- Canis, M.; Donnez, J.G.; Guzick, D.S.; Halme, J.K.; Rock, J.A.; Schenken, R.S.; Vernon, M.W. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil. Steril. 1997, 67, 817–821. [Google Scholar] [CrossRef]
- Tuttlies, F.; Keckstein, J.; Ulrich, U.; Possover, M.; Schweppe, K.W.; Wustlich, M.; Buchweitz, O.; Greb, R.; Kandolf, O.; Mangold, R.; et al. [ENZIAN-score, a classification of deep infiltrating endometriosis]. Zentralbl. Gynakol. 2005, 127, 275–281. [Google Scholar] [CrossRef]
- Haas, D.; Shebl, O.; Shamiyeh, A.; Oppelt, P. The rASRM score and the Enzian classification for endometriosis: Their strengths and weaknesses: The rASRM score and the Enzian classification. Acta Obstet. Et Gynecol. Scand. 2012, 92, 3–7. [Google Scholar] [CrossRef]
- Working Group of ESGE, ESHRE, and WES; Keckstein, J.; Becker, C.M.; Canis, M.; Feki, A.; Grimbizis, G.F.; Hummelshoj, L.; Nisolle, M.; Roman, H.; Saridogan, E.; et al. Recommendations for the surgical treatment of endometriosis. Part 2: Deep endometriosis. Hum. Reprod. Open 2020, 2020, hoaa002. [Google Scholar] [CrossRef]
- Thomassin-Naggara, I.; Lamrabet, S.; Crestani, A.; Bekhouche, A.; Wahab, C.A.; Kermarrec, E.; Touboul, C.; Daraï, E. Magnetic resonance imaging classification of deep pelvic endometriosis: Description and impact on surgical management. Hum. Reprod. 2020, 35, 1589–1600. [Google Scholar] [CrossRef]
- Bazot, M.; Bharwani, N.; Huchon, C.; Kinkel, K.; Cunha, T.M.; Guerra, A.; Manganaro, L.; Buñesch, L.; Kido, A.; Togashi, K.; et al. European society of urogenital radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur. Radiol. 2016, 27, 2765–2775. [Google Scholar] [CrossRef]
- Togashi, K.; Nishimura, K.; Kimura, I.; Tsuda, Y.; Yamashita, K.; Shibata, T.; Nakano, Y.; Konishi, J.; Konishi, I.; Mori, T. Endometrial cysts: Diagnosis with MR imaging. Radiology 1991, 180, 73–78. [Google Scholar] [CrossRef]
- Bazot, M.; Darai, E.; Hourani, R.; Thomassin, I.; Cortez, A.; Uzan, S.; Buy, J.-N. Deep Pelvic Endometriosis: MR Imaging for Diagnosis and Prediction of Extension of Disease. Radiology 2004, 232, 379–389. [Google Scholar] [CrossRef]
- Bazot, M.; Jarboui, L.; Ballester, M.; Touboul, C.; Thomassin-Naggara, I.; Daraï, E. The value of MRI in assessing parametrial involvement in endometriosis. Hum. Reprod. 2012, 27, 2352–2358. [Google Scholar] [CrossRef]
- Daraï, E.; Ballester, M.; Chéreau, E.; Coutant, C.; Rouzier, R.; Wafo, E. Laparoscopic versus laparotomic radical en bloc hysterectomy and colorectal resection for endometriosis. Surg. Endosc. 2010, 24, 3060–3067. [Google Scholar] [CrossRef]
- Daraï, E.; Dubernard, G.; Coutant, C.; Frey, C.; Rouzier, R.; Ballester, M. Randomized trial of laparoscopically assisted versus open colorectal resection for endometriosis: Morbidity, symptoms, quality of life, and fertility. Ann. Surg. 2010, 251, 1018–1023. [Google Scholar] [CrossRef]
- Ballester, M.; Chereau, E.; Dubernard, G.; Coutant, C.; Bazot, M.; Daraï, E. Urinary dysfunction after colorectal resection for endometriosis: Results of a prospective randomized trial comparing laparoscopy to open surgery. Am. J. Obstet. Gynecol. 2011, 204, 303.e1–303.e6. [Google Scholar] [CrossRef]
- Ballester, M.; Santulli, P.; Bazot, M.; Coutant, C.; Rouzier, R.; Daraï, E. Preoperative Evaluation of Posterior Deep-Infiltrating Endometriosis Demonstrates a Relationship with Urinary Dysfunction and Parametrial Involvement. J. Minim. Invasive Gynecol. 2011, 18, 36–42. [Google Scholar] [CrossRef]
- Jayot, A.; Timoh, K.N.; Bendifallah, S.; Ballester, M.; Darai, E. Comparison of Laparoscopic Discoid Resection and Segmental Resection for Colorectal Endometriosis Using a Propensity Score Matching Analysis. J. Minim. Invasive Gynecol. 2018, 25, 440–446. [Google Scholar] [CrossRef]
- Poupon, C.; Owen, C.; Arfi, A.; Cohen, J.; Bendifallah, S.; Daraï, E. Nomogram predicting the likelihood of complications after surgery for deep endometriosis without bowel involvement. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2019, 3, 100028. [Google Scholar] [CrossRef]
- Pecorelli, S.; Benedet, J.; Creasman, W.; Shepherd, J.H. FIGO staging of gynecologic cancer. 1994–1997 FIGO Committee on Gynecologic Oncology. International Federation of Gynecology and Obstetrics. Int. J. Gynecol. Obstet. 1999, 65, 243–249. [Google Scholar] [CrossRef]
- Royal College of Obstetricians and Gynaecologists (RCOG). Classification of Laparoscopic Procedures per Level of Difficulty; Royal College of Obstetricians and Gynaecologists (RCOG): London, UK, 2001. [Google Scholar]
- Nisolle, M.; Donnez, J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil. Steril. 1997, 68, 585–596. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo Classification of Surgical Complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Harrell, F.E.; Lee, K.L.; Mark, D.B. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat. Med. 1996, 15, 361–387. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Eijkemans, M.J.; Harrell, F.E.; Habbema, J.D. Prognostic modelling with logistic regression analysis: A comparison of selection and estimation methods in small data sets. Stat. Med. 2000, 19, 1059–1079. [Google Scholar] [CrossRef]
- Hanley, J.A.; McNeil, B.J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982, 143, 29–36. [Google Scholar] [CrossRef]
- Heagerty, P.J.; Zheng, Y. Survival Model Predictive Accuracy and ROC Curves. Biometrics 2005, 61, 92–105. [Google Scholar] [CrossRef]
- Menakaya, U.; Reid, S.; Lü, C.; Bassem, G.; Infante, F.; Condous, G. Performance of ultrasound-based endometriosis staging system (UBESS) for predicting level of complexity of laparoscopic surgery for endometriosis: Ultrasound-based endometriosis staging system. Ultrasound Obstet. Gynecol. 2016, 48, 786–795. [Google Scholar] [CrossRef]
- Foti, P.V.; Farina, R.; Palmucci, S.; Vizzini, I.A.A.; Libertini, N.; Coronella, M.; Spadola, S.; Caltabiano, R.; Iraci, M.; Basile, A.; et al. Endometriosis: Clinical features, MR imaging findings and pathologic correlation. Insights Imaging 2018, 9, 149–172. [Google Scholar] [CrossRef]
- Haas, D.; Chvátal, R.; Habelsberger, A.; Wurm, P.; Schimetta, W.; Oppelt, P. Comparison of revised American Fertility Society and ENZIAN staging: A critical evaluation of classifications of endometriosis on the basis of our patient population. Fertil. Steril. 2011, 95, 1574–1578. [Google Scholar] [CrossRef]
- Adamson, G.D. Endometriosis classification: An update. Curr. Opin. Obstet. Gynecol. 2011, 23, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Owoeye, O.B.A.; Rauvola, R.S.; Brownson, R.C. Dissemination and implementation research in sports and exercise medicine and sports physical therapy: Translating evidence to practice and policy. BMJ Open Sport Exerc. Med. 2020, 6, e000974. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, R.J.; E Hollyock, V. Observations on the anatomy of the rectovaginal pouch and septum. Obstet. Gynecol. 1982, 59, 445–447. [Google Scholar] [PubMed]






| 1.5 T | 3 T | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sagittal 2DT2W | Axial 2DT2W | 3DT2W | Axial T1W | Oblique Axial 2DT2W | Sagittal 2DT2W | Axial 2DT2W | 3DT2W | Axial T1W | Oblique Axial 2DT2W | |
| TR | 6000 | 6300 | 1400 | 6 | 4100 | 10,800 | 7000 | 1600 | 7 | 7300 |
| TE | 100 | 100 | 110 | 3 | 100 | 110 | 130 | 110 | 1 | 110 |
| Angle | 140 | 160 | 90 | 15 | 160 | 142 | 111 | 90 | 15 | 150 |
| Matrix | 320 × 320 | 320 × 320 | 260 × 260 | 320 × 320 | 320 × 320 | 480 × 480 | 352 × 352 | 320 × 320 | 320 × 320 | 340 × 340 |
| FOV Phase FOV | 24 24 | 30 30 | 26 22.1 | 32 32 | 24 24 | 28 28 | 32 32 | 28 16.8 | 32 32 | 24 24 |
| Nex | 3.09 | 1 | 2 | 1.4 | 3.82 | 1.72 | 1.54 | 2 | 1.21 | 2.21 |
| BW (Hz) | 41.7 | 41.7 | 41.7 | 90.9 | 41.7 | 83.3 | 50 | 62.5 | 166.7 | 41.7 |
| Voxel size (mm) | 0.5 | 1 | 0.5 | 1 | 0.3 | 0.5 | 1 | 0.5 | 1 | 3 |
| Slice thickness (mm) | 4 | 5 | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 |
| Acquisition time | 3:00 | 3:20 | 5:00 | 2:30 | 2:30 | 10,800 | 7000 | 1600 | 7 | 7300 |
| Endo-Stage MRI | Location | Extent | Risk Stratification |
|---|---|---|---|
| Endo-Stage MRI 0 | Superficial endometriosis |
| Low |
| Endometriosis is strictly confined to the ovaries |
| ||
| Endo-Stage MRI I | Endometriosis is strictly confined to the retrocervical area |
| |
| Endo-Stage MRI II | Endometriosis invades beyond the retrocervical area, but not to the pelvic side-wall |
| |
| Endo-Stage MRI III | Endometriosis extends to the pelvic side-wall and/or causes hydronephrosis or non-functioning kidney |
| Intermediate |
| Endo-Stage MRI IV | Endometriosis has involved the bladder or rectosigmoid colon |
| |
| Endo-Stage MRI V | Multiple deep endometrioticlocations |
| High |
| Patient Characteristic (n = 751) | ||
| Age (years) | Average ± SD Median/range | 33.7 ± 6.55 33/19–60 |
| BMI (kg/m2) | Average ± SD Median/range | 23.3 ± 4.27 22.5/12–42 |
| Smoking | Yes | 6.4% (48) |
| Surgical indication | Pain | 71% (534) |
| Pain and/or Infertility | 28% (211) | |
| NA | 1% (6) | |
| Prior pregnancy | Yes | 26.5% (199) |
| History of surgery | Yes | 43% (312) |
| Surgical characteristics (n = 751) | ||
| Surgical route | Laparoscopy Laparotomy Laparo-conversion | 87% (651) 10% (76) 3% (24) |
| ASRM | Mean ± SD Median | 66.72 ± 43.31 64 |
| Endometrioma surgery | Yes Cystectomy Salpingo-oophorectomy | 34.2% (258) 14.4% (108) 16.2% (122) |
| Salpingectomy | Yes | 26.5% (200) |
| Torus uterinum resection | Yes | 78.9% (594) |
| USL resection | Yes | 90% (678) |
| Partial colpectomy | Yes | 26.9% (203) |
| Hysterectomy | Yes | 26.5% (200) |
| Ureterolysis | Yes | 75.4% (568) |
| Parametrectomy | Yes | 37.5% (282) |
| Ureteral re-implantation | Yes | 3.3% (25) |
| Partial bladder resection | Yes | 3.9% (30) |
| Rectosigmoid colon surgery | Absent Shaving Discoid Segmental resection | 19% (142) 14% (104) 16% (119) 51% (386) |
| Protective stomia | Yes | 15.8% (119) |
| Ileal/cecal resection | Yes | 5.4% (41) |
| Appendectomy | Yes | 8.1% (61) |
| Endo-MRI classification | Endo-MRI stage 0 Endo-MRI stage 1 Endo-MRI stage 2 Endo-MRI stage 3 Endo-MRI stage 4 Endo-MRI stage 5 | 3% (26) 21% (156) 5% (40) 3% (22) 39% (290) 29% (217) |
| Endo-MRI stratification | Low Intermediate High | 30% (222) 41% (312) 29% (217) |
| Frequency | Complications Rates According to ENDO-MRI Classification | |||||||
|---|---|---|---|---|---|---|---|---|
| Low Risk Group (n = 222) | Intermediate Risk Group (n = 312) | High Risk Group (n = 217) | p-Value | |||||
| Stage 0 (n = 26) | Stage 1 (n = 156) | Stage 2 (n = 40) | Stage 3 (n = 22) | Stage 4 (n = 290) | Stage 5 (n = 217) | |||
| Overall complications rate (n = 751) | 32% (241) | 12% (3) | 13% (20) | 15% (6) | 32% (7) | 35% (102) | 47% (103) | p < 0.001 |
| Clavien-Dindo 3–4 complications (n = 751) | 11% (82) | 0% (0) | 3% (5) | 8% (3) | 9% (2) | 10% (30) | 19% (42) | p < 0.001 |
| Self-catheterization at 1 month (n = 579) | 16% (92) | 15% (3) | 5% (7) | 17% (6) | 13% (2) | 13% (28) | 31% (46) | p < 0.001 |
| Variable | Overall Complications | Clavien-Dindo 3–4 Complications | Self-Catheterization > 1 Month | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-Value | Odds Ratio | 95 % CI | p-Value | Odds Ratio | 95 % CI | p-Value | ||
| Age | 1.01 | 0.98–1.03 | 0.72 | 1.04 | 0.99–1.08 | 0.06 | 0.99 | 0.95–1.03 | 0.47 | |
| BMI | 0.97 | 0.93–1.01 | 0.21 | 0.96 | 0.90–1.02 | 0.19 | 0.98 | 0.92–1.04 | 0.43 | |
| History of surgery | 2.05 | 1.40–2.98 | <0.001 | 1.69 | 1.01–2.84 | 0.04 | 1.35 | 0.83–2.21 | 0.23 | |
| Surgical route | Reference = Laparoscopy Laparotomy Laparo-conversion | 2.22 9.37 | 1.24–3.97 2.51–34.92 | <0.001 | 1.65 3.16 | 0.83–3.27 1.11–9.02 | 0.06 | 1.20 1.79 | 0.58–2.46 0.55–5.86 | 0.59 |
| Endo-MRI stratification | Reference = low-risk Intermediate High | 3.30 6.83 | 1.97–5.53 3.96–11.78 | <0.001 | 2.48 6.39 | 1.04–5.88 2.73–14.99 | <0.001 | 1.48 3.73 | 0.75–2.92 1.92–7.25 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bazot, M.; Daraï, E.; Benagiano, G.P.; Reinhold, C.; Favier, A.; Roman, H.; Donnez, J.; Bendifallah, S. ENDO_STAGE Magnetic Resonance Imaging: Classification to Screen Endometriosis. J. Clin. Med. 2022, 11, 2443. https://doi.org/10.3390/jcm11092443
Bazot M, Daraï E, Benagiano GP, Reinhold C, Favier A, Roman H, Donnez J, Bendifallah S. ENDO_STAGE Magnetic Resonance Imaging: Classification to Screen Endometriosis. Journal of Clinical Medicine. 2022; 11(9):2443. https://doi.org/10.3390/jcm11092443
Chicago/Turabian StyleBazot, Marc, Emile Daraï, Giuseppe P. Benagiano, Caroline Reinhold, Amelia Favier, Horace Roman, Jacques Donnez, and Sofiane Bendifallah. 2022. "ENDO_STAGE Magnetic Resonance Imaging: Classification to Screen Endometriosis" Journal of Clinical Medicine 11, no. 9: 2443. https://doi.org/10.3390/jcm11092443
APA StyleBazot, M., Daraï, E., Benagiano, G. P., Reinhold, C., Favier, A., Roman, H., Donnez, J., & Bendifallah, S. (2022). ENDO_STAGE Magnetic Resonance Imaging: Classification to Screen Endometriosis. Journal of Clinical Medicine, 11(9), 2443. https://doi.org/10.3390/jcm11092443







