Eye Involvement in Wilson’s Disease: A Review of the Literature
Abstract
:1. Introduction
2. Materials and Methods
3. Results
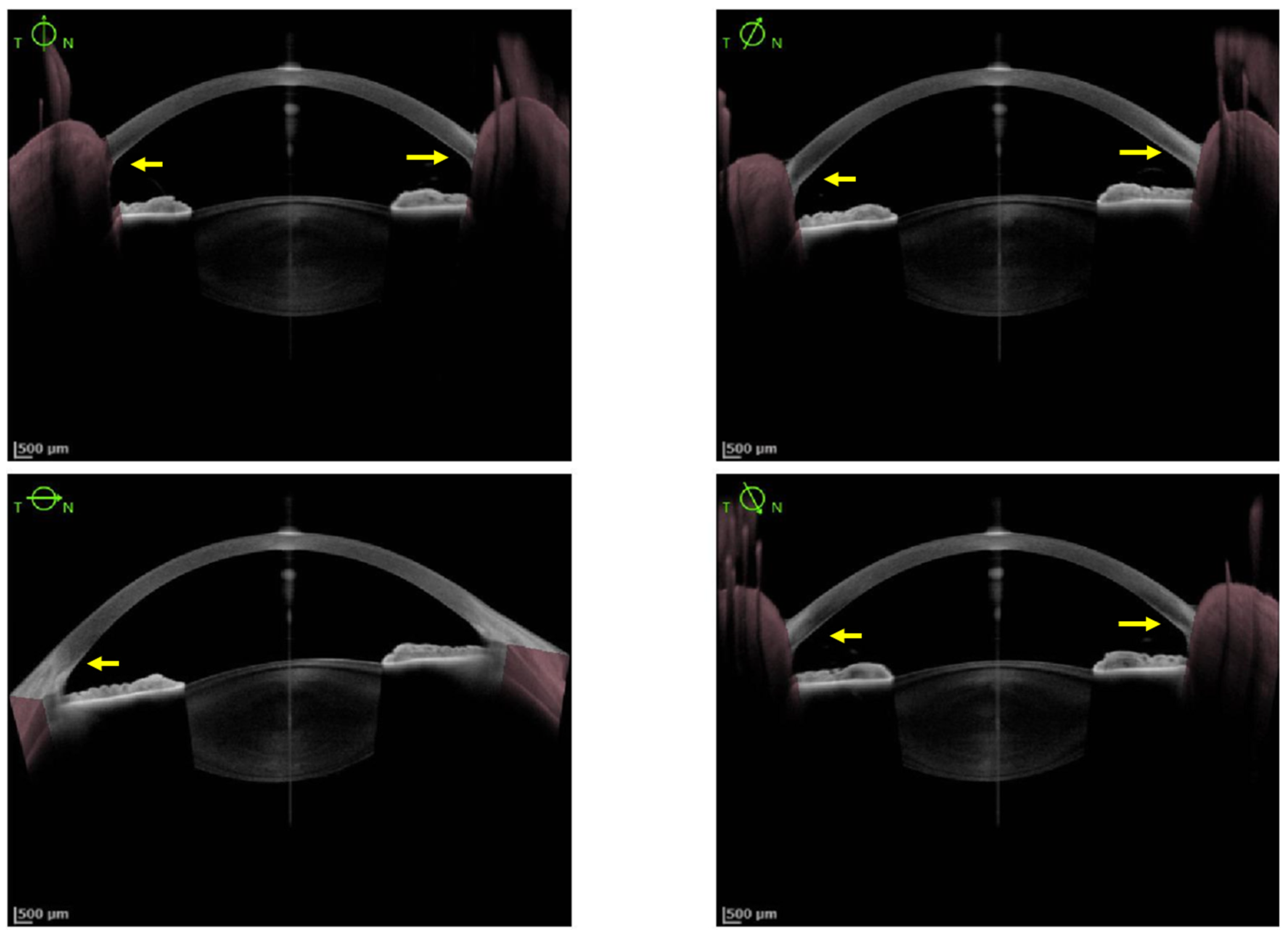
3.1. Cornea Involvement
3.2. Lens Involvement
3.3. Macula, Retinal Nerve Fiber Layer and Visual Pathways Involvement
3.4. Eye Mobility
3.5. Other Ocular Abnormalities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Poujois, A.; Woimant, F.; Samson, S.; Chaine, P.; Girardot-Tinant, N.; Tuppin, P. Characteristics and prevalence of Wilson’s disease: A 2013 observational population-based study in France. Clin. Res. Hepatol. Gastroenterol. 2018, 42, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Roberts, E.A.; Schilsky, M.L.; American Association for Study of Liver Diseases (AASLD). Diagnosis and treatment of Wilson disease: An update. Hepatology 2008, 47, 2089–2111. [Google Scholar] [CrossRef] [PubMed]
- Broniek-Kowalik, K.; Dzieżyc, K.; Litwin, T.; Członkowska, A.; Szaflik, J.P. Anterior segment optical coherence tomography (AS-OCT) as a new method of detecting copper deposits forming the Kayser–Fleischer ring in patients with Wilson disease. Acta Ophthalmol. 2019, 97, e757–e760. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.; Pericleous, M. Wilson disease: More than meets the eye. Postgrad. Med. J. 2018, 94, 335–347. [Google Scholar] [CrossRef]
- Pfeiffer, R.F. Wilson’s Disease. Skull Base 2007, 27, 123–132. [Google Scholar] [CrossRef] [Green Version]
- Fenu, M.; Liggi, M.; Demelia, E.; Sorbello, O.; Civolani, A. Kayser–Fleischer ring in Wilson’s disease: A cohort study. Eur. J. Intern. Med. 2012, 23, e150–e156. [Google Scholar] [CrossRef]
- Prasad, D.; Bhriguvanshi, A. Ocular manifestations of liver disease in children: Clinical aspects and implications. Ann. Hepatol. 2020, 19, 608–613. [Google Scholar] [CrossRef]
- Vitiello, L.; De Bernardo, M.; Nuzio, S.G.; Mandato, C.; Rosa, N.; Vajro, P. Pediatric liver diseases and ocular changes: What hepatologists and ophthalmologists should know and share with each other. Dig. Liver Dis. 2019, 52, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Walshe, J.M. The eye in Wilson disease. QJM 2010, 104, 451–453. [Google Scholar] [CrossRef] [Green Version]
- Członkowska, A.; Litwin, T.; Chabik, G. Wilson Disease. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2017; Volume 142, pp. 101–119. ISBN 978-0-444-63625-6. [Google Scholar]
- Innes, J.R.; Strachan, I.M.; Triger, D.R. Unilateral Kayser-Fleischer ring. Br. J. Ophthalmol. 1986, 70, 469–470. [Google Scholar] [CrossRef] [Green Version]
- Al-Khaier, A.; Nischal, K.K. The eye in metabolic disease. Hosp. Med. 2003, 64, 609–612. [Google Scholar] [CrossRef] [PubMed]
- Alakus, M.F.; Caglayan, M.; Ekin, N.; Oncul, H.; Arac, E.; Dag, U.; Diri, H. Investigation of corneal topographic and densitometric properties of Wilson’s disease patients with or without a Kayser-Fleischer ring. Eye Vis. 2021, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gitlin, J.D. Wilson disease. Gastroenterology 2003, 125, 1868–1877. [Google Scholar] [CrossRef] [PubMed]
- Walshe, J.M. The Kayser–Fleischer Ring. Br. J. Hosp. Med. 2014, 75, 2. [Google Scholar] [CrossRef]
- Sridhar, U.; Tripathy, K. Commentary: Kayser-Fleischer-like rings in patients with hepatic disease. Indian J. Ophthalmol. 2021, 69, 1088. [Google Scholar] [CrossRef]
- Langwińska-Wośko, E.; Litwin, T.; Dzieżyc, K.; Członkowska, A. The sunflower cataract in Wilson’s disease: Pathognomonic sign or rare finding? Acta Neurol. Belg. 2015, 116, 325–328. [Google Scholar] [CrossRef] [Green Version]
- Youn, J.; Kim, J.S.; Kim, H.-T.; Lee, J.-Y.; Lee, P.H.; Ki, C.-S.; Cho, J.W. Characteristics of neurological Wilson’s disease without Kayser–Fleischer ring. J. Neurol. Sci. 2012, 323, 183–186. [Google Scholar] [CrossRef]
- Demirkiran, M.; Jankovic, J.; Lewis, R.A.; Cox, D.W. Neurologic presentation of Wilson disease without Kayser-Fleischer rings. Neurology 1996, 46, 1040–1043. [Google Scholar] [CrossRef]
- Medici, V.; Rossaro, L.; Sturniolo, G. Wilson disease—A practical approach to diagnosis, treatment and follow-up. Dig. Liver Dis. 2007, 39, 601–609. [Google Scholar] [CrossRef]
- Willeit, J.; Kiechl, S. Wilson’s disease with neurological impairment but no Kayser-Fleischer rings. Lancet 1991, 337, 1426. [Google Scholar] [CrossRef]
- Imam, L.; Haboubi, H.N. G-Eye: Ocular manifestations of gastrointestinal disease. Front. Gastroenterol. 2019, 11, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Lorincz, M.T. Neurologic Wilson’s disease. Ann. N. Y. Acad. Sci. 2010, 1184, 173–187. [Google Scholar] [CrossRef] [PubMed]
- Couchonnal, E.; Lion-François, L.; Guillaud, O.; Habes, D.; Debray, D.; Lamireau, T.; Broué, P.; Fabre, A.; Vanlemmens, C.; Sobesky, R.; et al. Pediatric Wilson’s Disease: Phenotypic, Genetic Characterization and Outcome of 182 Children in France. J. Pediatr. Gastroenterol. Nutr. 2021, 73, e80–e86. [Google Scholar] [CrossRef]
- Merle, U.; Schaefer, M.; Ferenci, P.; Stremmel, W. Clinical presentation, diagnosis and long-term outcome of Wilson’s disease: A cohort study. Gut 2007, 56, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Grupchev, D.I.; Radeva, M.N.; Georgieva, M.; Grupcheva, C.N. In vivo confocal microstructural analysis of corneas presenting Kayser-Fleischer rings in patients with Wilson’s disease. Arq. Bras. Oftalmol. 2018, 81, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Poujois, A.; Trocello, J.-M.; Djebrani-Oussedik, N.; Poupon, J.; Collet, C.; Girardot-Tinant, N.; Sobesky, R.; Habès, D.; Debray, D.; Vanlemmens, C.; et al. Exchangeable copper: A reflection of the neurological severity in Wilson’s disease. Eur. J. Neurol. 2016, 24, 154–160. [Google Scholar] [CrossRef] [Green Version]
- European Association for Study of Liver. EASL Clinical Practice Guidelines: Wilson’s disease. J. Hepatol. 2012, 56, 671–685. [Google Scholar] [CrossRef] [Green Version]
- Socha, P.; Janczyk, W.; Dhawan, A.; Baumann, U.; D’Antiga, L.; Tanner, S.; Iorio, R.; Vajro, P.; Houwen, R.; Fischler, B.; et al. Wilson’s Disease in Children: A Position Paper by the Hepatology Committee of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 334–344. [Google Scholar] [CrossRef]
- Sridhar, M.S. Advantages of Anterior Segment Optical Coherence Tomography Evaluation of the Kayser–Fleischer Ring in Wilson Disease. Cornea 2017, 36, 343–346. [Google Scholar] [CrossRef]
- Sridhar, M.S.; Rangaraju, A.; Anbarasu, K.; Reddy, S.P.; Daga, S.; Jayalakshmi, S.; Shaik, B. Evaluation of Kayser–Fleischer ring in Wilson disease by anterior segment optical coherence tomography. Indian J. Ophthalmol. 2017, 65, 354–357. [Google Scholar] [CrossRef]
- Sridhar, M.S.; Pineda, R. Anterior segment optical coherence tomography to look for Kayser-Fleischer rings. Pract. Neurol. 2017, 17, 222–223. [Google Scholar] [CrossRef] [PubMed]
- Telinius, N.; Ott, P.; Hjortdal, J. Detection of Kayser-Fleischer ring using Scheimpflug imaging. Acta Ophthalmol. 2016, 95, e248–e249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, T.; Fang, Z.; Tian, J.; Liu, J.; Xiao, Y.; Li, H.; Chen, B. Imaging Kayser-Fleischer Ring in Wilson Disease Using In Vivo Confocal Microscopy. Cornea 2018, 38, 332–337. [Google Scholar] [CrossRef]
- Ceresara, G.; Fogagnolo, P.; Zuin, M.; Zatelli, S.; Bovet, J.; Rossetti, L. Study of Corneal Copper Deposits in Wilson’s Disease by in vivo Confocal Microscopy. Ophthalmologica 2014, 231, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Rathi, A.; Takkar, B.; Gaur, N.; Maharana, P.K. Optical coherence tomography of the Kayser-Fleischer ring: An ancillary diagnostic tool for Wilson’s disease in children. BMJ Case Rep. 2017, 2017, bcr-2017-220007. [Google Scholar] [CrossRef] [PubMed]
- Telinius, N.; Ott, P.; Sandahl, T.D.; Hjortdal, J. Scheimpflug Imaging of the Danish Cohort of Patients With Wilson Disease. Cornea 2019, 38, 998–1002. [Google Scholar] [CrossRef] [PubMed]
- Degirmenci, C.; Palamar, M. Evaluation and grading of Kayser–Fleischer ring in Wilson disease by Scheimpflug camera. Eur. J. Ophthalmol. 2020, 31, 2116–2120. [Google Scholar] [CrossRef]
- Belkin, M.; Zeimer, R.; Chajek, T.; Friedman, G.; Melamed, E. Non-invasive quantitation of corneal copper in hepatolenticular degeneration (wilson’s disease). Lancet 1976, 307, 391–392. [Google Scholar] [CrossRef]
- Sturniolo, G.C.; Lazzarini, D.; Bartolo, O.; Berton, M.; Leonardi, A.; Fregona, I.A.; Parrozzani, R.; Midena, E. Small Fiber Peripheral Neuropathy in Wilson Disease: An In Vivo Documentation by Corneal Confocal Microscopy. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1390–1395. [Google Scholar] [CrossRef] [Green Version]
- Siemerling, E.; Oloff, H. Pseudosklerose (Westphal-Strümpell). Klin. Wochenschr. 1922, 1, 1087–1089. [Google Scholar] [CrossRef]
- Jang, H.J.; Kim, J.M.; Choi, C.Y. Elemental analysis of sunflower cataract in Wilson’s disease: A study using scanning transmission electron microscopy and energy dispersive spectroscopy. Exp. Eye Res. 2014, 121, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Litwin, T.; Langwińska-Wośko, E.; Dzieżyc, K.; Członkowska, A. Sunflower cataract: Do not forget Wilson’s disease. Pract. Neurol. 2015, 15, 385–386. [Google Scholar] [CrossRef] [PubMed]
- Langwińska-Wośko, E.; Litwin, T.; Szulborski, K.; Członkowska, A. Optical coherence tomography and electrophysiology of retinal and visual pathways in Wilson’s disease. Metab. Brain Dis. 2015, 31, 405–415. [Google Scholar] [CrossRef] [Green Version]
- Albrecht, P.; Müller, A.-K.; Ringelstein, M.; Finis, D.; Geerling, G.; Cohn, E.; Aktas, O.; Hartung, H.-P.; Hefter, H.; Methner, A. Retinal Neurodegeneration in Wilson’s Disease Revealed by Spectral Domain Optical Coherence Tomography. PLoS ONE 2012, 7, e49825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Satishohandra, P.; Naik, K.R. Visual pathway abnormalities Wilson’s disease: An electrophysiological study using electroretinography and visual evoked potentials. J. Neurol. Sci. 2000, 176, 13–20. [Google Scholar] [CrossRef]
- Langwińska-Wośko, E.; Litwin, T.; Dzieżyc, K.; Karlinski, M.; Czlonkowska, A. Optical coherence tomography as a marker of neurodegeneration in patients with Wilson’s disease. Acta Neurol. Belg. 2017, 117, 867–871. [Google Scholar] [CrossRef] [PubMed]
- Svetel, M.; Božić, M.; Vitković, J.; Jovanović, Č.; Dragašević, N.; Pekmezović, T.; Svetel, M.; Tomić, A.; Kresojević, N.; Kostić, V. Optical coherence tomography in patients with Wilson’s disease. Acta Neurol. Scand. 2021, 144, 149–154. [Google Scholar] [CrossRef]
- Jung, H.-K.; Choi, S.Y.; Kim, J.-M.; Kim, J.-S. Selective slowing of downward saccades in Wilson’s disease. Park. Relat. Disord. 2013, 19, 134–135. [Google Scholar] [CrossRef]
- Kirkham, T.H.; Kamin, D.F. Slow saccadic eye movements in Wilson’s disease. J. Neurol. Neurosurg. Psychiatry 1974, 37, 191–194. [Google Scholar] [CrossRef] [Green Version]
- Ingster-Moati, I.; Quoc, E.B.; Pless, M.; Djomby, R.; Orssaud, C.; Guichard, J.P.; Woimant, F. Ocular motility and Wilson’s disease: A study on 34 patients. J. Neurol. Neurosurg. Psychiatry 2007, 78, 1199–1201. [Google Scholar] [CrossRef] [Green Version]
- Leśniak, M.; Członkowska, A.; Seniów, J.S. Abnormal antisaccades and smooth pursuit eye movements in patients with Wilson’s disease. Mov. Disord. 2008, 23, 2067–2073. [Google Scholar] [CrossRef] [PubMed]
- Hanuška, J.; Dušek, P.; Rusz, J.; Ulmanová, O.; Burgetová, A.; Růžička, E. Eye movement abnormalities are associated with brainstem atrophy in Wilson disease. Neurol. Sci. 2020, 41, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Lalla, R.; Patil, T. Is blinking of the eyes affected in extrapyramidal disorders? An interesting observation in a patient with Wilson disease. BMJ Case Rep. 2012, bcr2012007367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Cock, V.C.; Lacombe, S.; Woimant, F.; Poujois, A. Sleep disorders in Wilson’s disease. Sleep Med. 2020, 83, 299–303. [Google Scholar] [CrossRef]
- Ala, A.; Walker, A.P.; Ashkan, K.; Dooley, J.S.; Schilsky, M.L. Wilson’s disease. Lancet 2007, 369, 397–408. [Google Scholar] [CrossRef]
- Alkhuraimi, W.M.; Alqahtani, W.; Alqahtani, A.S. Challenges in Management of Rhegmatogenous Retinal Detachment in a Patient With Wilson’s Disease: A Case Report and Literature Review. Cureus 2021, 13, 12921. [Google Scholar] [CrossRef]
- Chou, L.T.; Horkey, D.; Slabaugh, M. Acute-Onset Optic Neuropathy in Wilson’s Disease. Case Rep. Ophthalmol. 2019, 9, 520–525. [Google Scholar] [CrossRef]
- Gow, P.J.; Peacock, S.E.; Chapman, R.W. Wilson’s disease presenting with rapidly progressive visual loss: Another neurologic manifestation of Wilson’s disease? J. Gastroenterol. Hepatol. 2001, 16, 699–701. [Google Scholar] [CrossRef]
- Rukunuzzaman, M.; Karim, M.B.; Rahman, M.M.; Islam, M.S.; Mazumder, M.W. Wilson’s disease in children with blindness: An atypical presentation. Mymensingh Med. J. 2013, 22, 176–179. [Google Scholar]
- Li, X.; Ye, T.; Li, Y.; Zhang, X. Secondary glaucoma with copper deposition in trabecular meshwork in Wilson disease: Letter to the Editor. Clin. Exp. Ophthalmol. 2013, 42, 204–205. [Google Scholar] [CrossRef]
- Hamid, G.; Taher, S.; Reza, A. Double Corneal Ring: Report of Simultaneous Coincidence of Kayser-Fleischer Ring and Fleischer Ring in a Keratoconus Patient Prior to Appearance of Wilson’s Disease. Iran. J. Ophtalmol. 2012, 24, 57–62. [Google Scholar]
- Hu, P.; Lin, L.; Wu, Z.; Jin, X.; Ni, H. Kayser–Fleischer ring with keratoconus: A coincidence? A case report. BMC Ophthalmol. 2020, 20, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Kara, N.; Seyyar, S.A.; Saygili, O.; Seyyar, M.; Gulsen, M.T.; Gungor, K. Anterior Segment Parameters in Patients With Wilson Disease. Cornea 2018, 37, 466–469. [Google Scholar] [CrossRef] [PubMed]
- Doğuizi, S.; Özateş, S.; Hoşnut, F.; Şahin, G.E.; Şekeroğlu, M.A.; Yılmazbaş, P. Assessment of corneal and lens clarity in children with Wilson disease. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2019, 23, 147.e1–147.e8. [Google Scholar] [CrossRef]
- Goyal, V. Sunflower cataract in Wilson’s disease. J. Neurol. Neurosurg. Psychiatry 2000, 69, 133. [Google Scholar] [CrossRef] [Green Version]
- Negahban, K.; Chern, K. Cataracts associated with systemic disorders and syndromes. Curr. Opin. Ophthalmol. 2002, 13, 419–422. [Google Scholar] [CrossRef]
- Ferenci, P.; Caca, K.; Loudianos, G.; Mieli-Vergani, G.; Tanner, S.; Sternlieb, I.; Schilsky, M.; Cox, D.; Berr, F. Diagnosis and phenotypic classification of Wilson disease1: Diagnosis and Phenotypic Classification of Wilson Disease. Liver Int. 2003, 23, 139–142. [Google Scholar] [CrossRef]
- Ting, D.S.J.; Foo, V.H.; Yang, L.W.Y.; Sia, J.T.; Ang, M.; Lin, H.; Chodosh, J.; Mehta, J.S.; Ting, D.S.W. Artificial intelligence for anterior segment diseases: Emerging applications in ophthalmology. Br. J. Ophthalmol. 2020, 105, 158–168. [Google Scholar] [CrossRef]
- Elsawy, A.; Eleiwa, T.; Chase, C.; Ozcan, E.; Tolba, M.; Feuer, W.; Abdel-Mottaleb, M.; Shousha, M.A. Multidisease Deep Learning Neural Network for the Diagnosis of Corneal Diseases. Am. J. Ophthalmol. 2021, 226, 252–261. [Google Scholar] [CrossRef]
- Dahrouj, M.; Miller, J.B. Artificial Intelligence (AI) and Retinal Optical Coherence Tomography (OCT). Semin. Ophthalmol. 2021, 36, 341–345. [Google Scholar] [CrossRef]



| Pediatric Population [24] | Adult Population [25] | |
|---|---|---|
| Patients undergoing SLE | 149 | 163 |
| Neurological patients | 19 | 55 |
| Hepatic patients | 129 | 96 |
| Incidence of KFR | 58 (38.9%) | 108 (66.3%) |
| Neurological patients | 18 (94.7%) | 47 (85.5%) |
| Hepatic patients | 40 (31.0%) | 50 (52.1%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chevalier, K.; Mauget-Faÿsse, M.; Vasseur, V.; Azar, G.; Obadia, M.A.; Poujois, A. Eye Involvement in Wilson’s Disease: A Review of the Literature. J. Clin. Med. 2022, 11, 2528. https://doi.org/10.3390/jcm11092528
Chevalier K, Mauget-Faÿsse M, Vasseur V, Azar G, Obadia MA, Poujois A. Eye Involvement in Wilson’s Disease: A Review of the Literature. Journal of Clinical Medicine. 2022; 11(9):2528. https://doi.org/10.3390/jcm11092528
Chicago/Turabian StyleChevalier, Kevin, Martine Mauget-Faÿsse, Vivien Vasseur, Georges Azar, Michaël Alexandre Obadia, and Aurélia Poujois. 2022. "Eye Involvement in Wilson’s Disease: A Review of the Literature" Journal of Clinical Medicine 11, no. 9: 2528. https://doi.org/10.3390/jcm11092528
APA StyleChevalier, K., Mauget-Faÿsse, M., Vasseur, V., Azar, G., Obadia, M. A., & Poujois, A. (2022). Eye Involvement in Wilson’s Disease: A Review of the Literature. Journal of Clinical Medicine, 11(9), 2528. https://doi.org/10.3390/jcm11092528






