Transesophageal Echocardiography-Guided Transseptal Left Atrial Access to Improve Safety in Patients Undergoing Pulmonary Vein Isolation
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Anesthesia
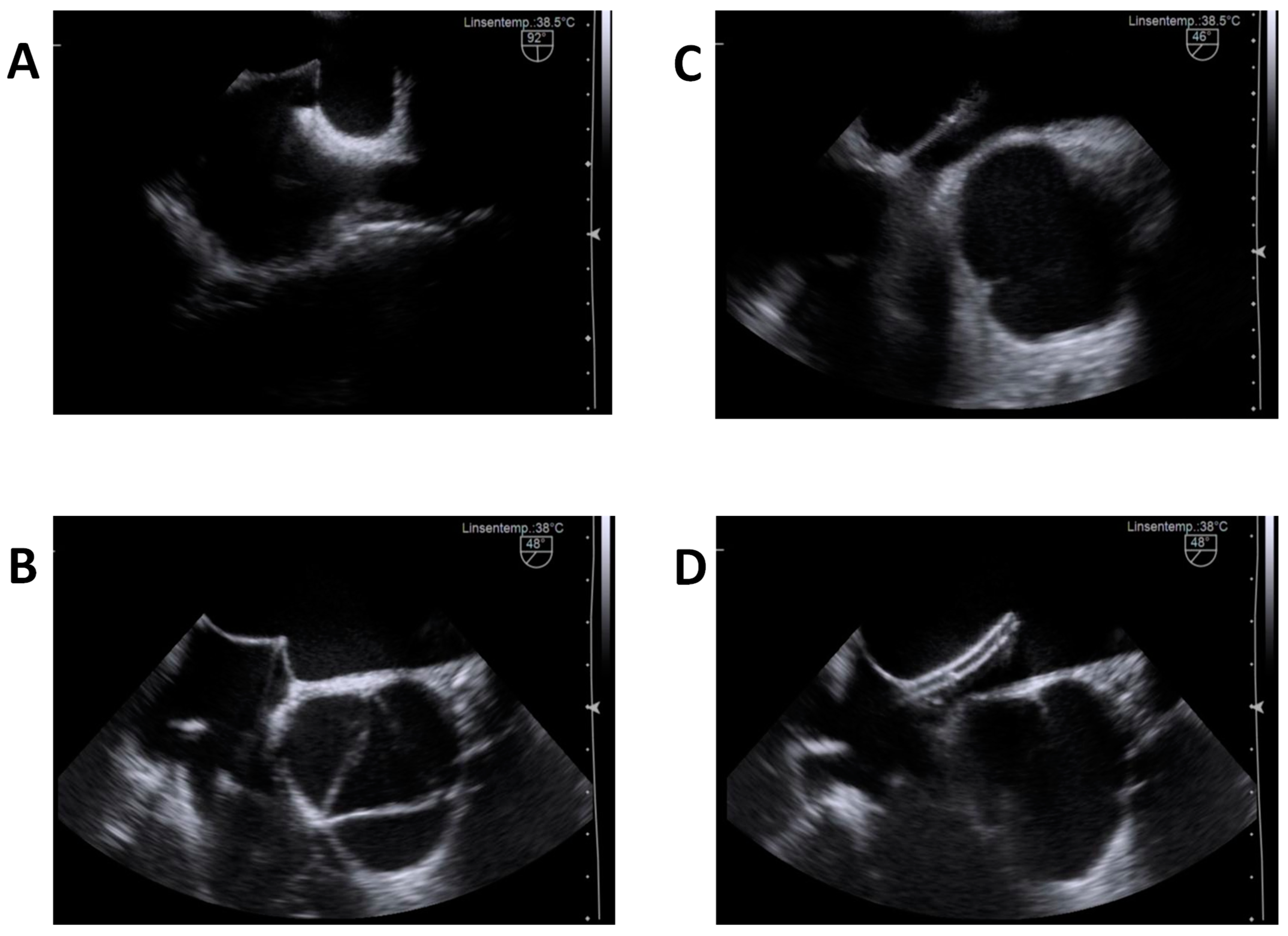
2.3. 2D-TEE Procedure
2.4. Ablation Procedure
2.5. Postinterventional Monitoring
2.6. Data Collection
2.7. Statistics
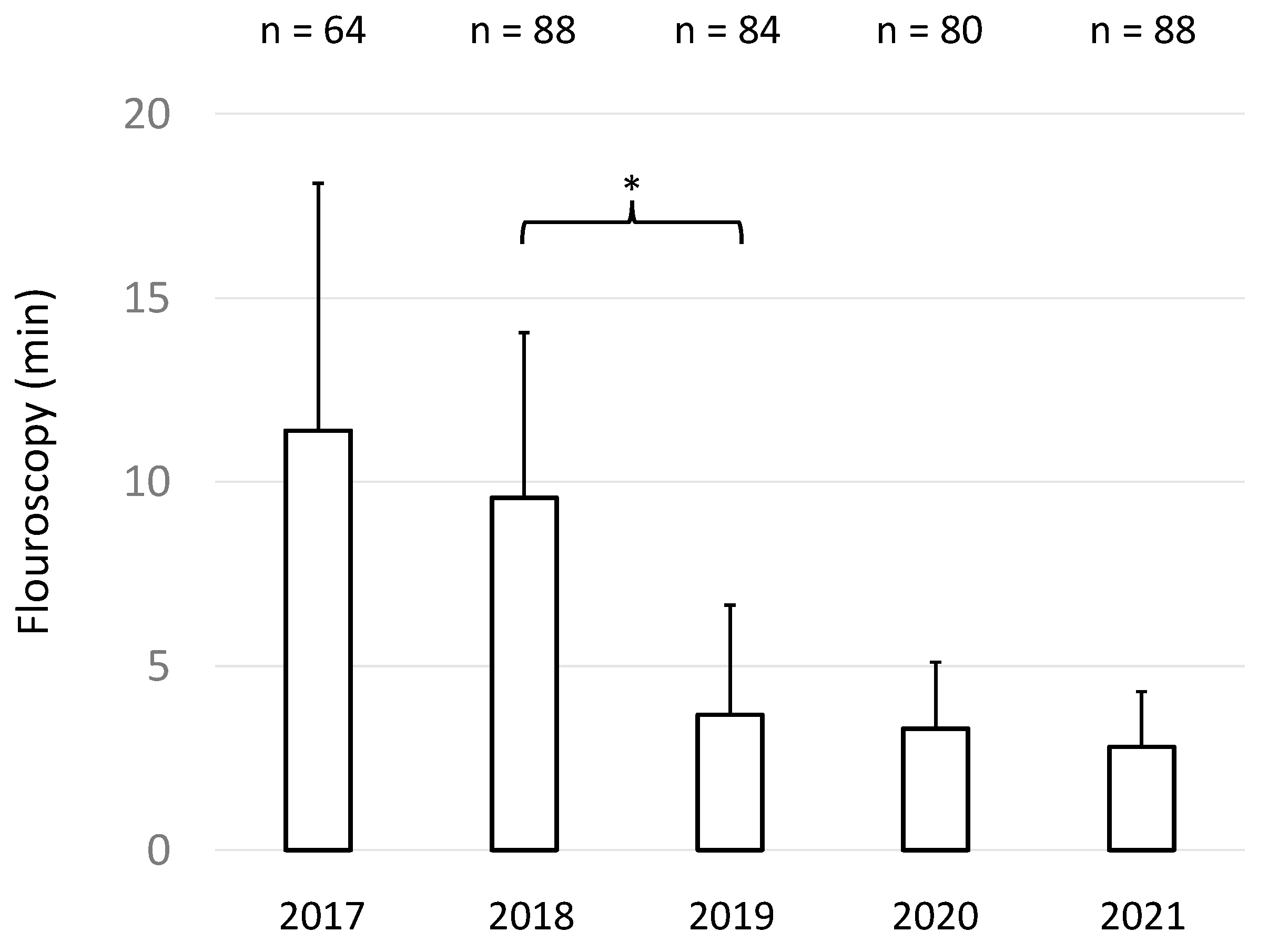
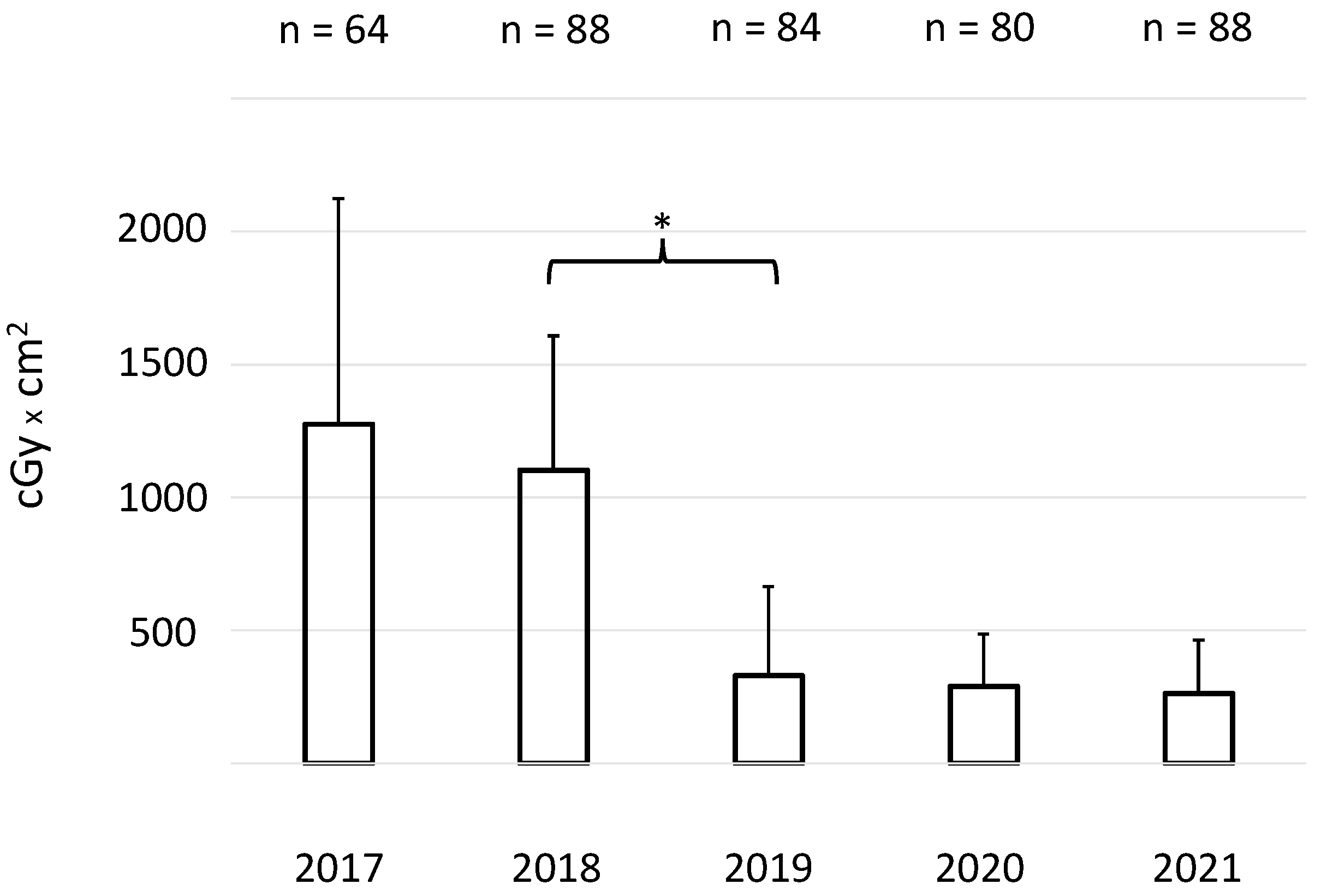
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviation
| ACT | Activated clotting time |
| AF | Atrial fibrillation |
| CA | Catheter ablation |
| CT | Computed Tomography |
| ECG | Electrocardiogram |
| EHRA | European Heart Rhythm Association |
| LVEF | Left ventricular ejection fraction |
| NOACs | New oral anticoagulants |
| NYHA | New York Heart Association |
| SEM | Standard Error of the mean |
| TEE | Transesophageal echocardiography |
| TTE | Transthoracic echocardiography |
| TSP | Transseptal puncture |
| PVI | Pulmonary vein isolation |
References
- Andrade, J.; Khairy, P.; Dobrev, D.; Nattel, S. The Clinical Profile and Pathophysiology of Atrial Fibrillation: Relationships Among Clinical Features, Epidemiology, and Mechanisms. Circ. Res. 2014, 114, 1453–1468. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed]
- Calkins, H.; Reynolds, M.R.; Spector, P.; Sondhi, M.; Xu, Y.; Martin, A.; Williams, C.J.; Sledge, I. Treatment of Atrial Fibrillation with Antiarrhythmic Drugs or Radiofrequency Ablation: Two Systematic Literature Reviews and Meta-Analyses. Circ. Arrhythmia Electrophysiol. 2009, 2, 349–361. [Google Scholar] [CrossRef] [PubMed]
- Mujović, N.; Marinković, M.; Lenarczyk, R.; Tilz, R.; Potpara, T.S. Catheter Ablation of Atrial Fibrillation: An Overview for Clinicians. Adv. Ther. 2017, 34, 1897–1917. [Google Scholar] [CrossRef] [PubMed]
- Marrouche, N.F.; Brachmann, J.; Andresen, D.; Siebels, J.; Boersma, L.; Jordaens, L.; Merkely, B.; Pokushalov, E.; Sanders, P.; Proff, J.; et al. Catheter Ablation for Atrial Fibrillation with Heart Failure. N. Engl. J. Med. 2018, 378, 417–427. [Google Scholar] [CrossRef]
- Manolis, A.S. Transseptal Access to the Left Atrium: Tips and Tricks to Keep it Safe Derived from Single Operator Experience and Review of the Literature. Curr. Cardiol. Rev. 2017, 13, 305–318. [Google Scholar] [CrossRef]
- De Ponti, R.; Cappato, R.; Curnis, A.; Della Bella, P.; Padeletti, L.; Raviele, A.; Santini, M.; Salerno-Uriarte, J.A. Trans-Septal Catheterization in the Electrophysiology Laboratory. J. Am. Coll. Cardiol. 2006, 47, 1037–1042. [Google Scholar] [CrossRef]
- F Fagundes, R.L.; Mantica, M.; De Luca, L.; Forleo, G.; Pappalardo, A.; Avella, A.; Fraticelli, A.; Dello Russo, A.; Casella, M.; Pelargonio, G.; et al. Safety of Single Transseptal Puncture for Ablation of Atrial Fibrillation: Retrospective Study from a Large Cohort of Patients. J. Cardiovasc. Electrophysiol. 2007, 18, 1277–1281. [Google Scholar] [CrossRef]
- Cappato, R.; Calkins, H.; Chen, S.A.; Davies, W.; Iesaka, Y.; Kalman, J.; Kim, Y.H.; Klein, G.; Natale, A.; Packer, D.; et al. Updated Worldwide Survey on the Methods, Efficacy, and Safety of Catheter Ablation for Human Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 2010, 3, 32–38. [Google Scholar] [CrossRef]
- Gupta, A.; Perera, T.; Ganesan, A.; Sullivan, T.; Lau, D.H.; Roberts-Thomson, K.C.; Brooks, A.G.; Sanders, P. Complications of Catheter Ablation of Atrial Fibrillation: A Systematic Review. Circ. Arrhythmia Electrophysiol. 2013, 6, 1082–1088. [Google Scholar] [CrossRef]
- Heeger, C.H.; Bellmann, B.; Fink, T.; Bohnen, J.E.; Wissner, E.; Wohlmuth, P.; Rottner, L.; Sohns, C.; Tilz, R.R.; Mathew, S.; et al. Efficacy and safety of cryoballoon ablation in the elderly: A multicenter study. Int. J. Cardiol. 2019, 278, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Leitz, P.; Güner, F.; Wasmer, K.; Foraita, P.; Pott, C.; Dechering, D.G.; Zellerhoff, S.; Kochhäuser, S.; Lange, P.S.; Eckardt, L.; et al. Data on procedural handling and complications of pulmonary vein isolation using the pulmonary vein ablation catheter GOLD ®. EP Eur. 2016, 18, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Matoshvili, Z.; Bastani, H.; Bourke, T.; Braunschweig, F.; Drca, N.; Gudmundsson, K.; Insulander, P.; Jemtrén, A.; Kennebäck, G.; Saluveer, O. Safety of fluoroscopy-guided transseptal approach for ablation of left-sided arrhythmias. EP Eur. 2017, 19, 2023–2026. [Google Scholar] [CrossRef]
- Cappato, R.; Calkins, H.; Chen, S.A.; Davies, W.; Iesaka, Y.; Kalman, J.; Kim, Y.H.; Klein, G.; Packer, D.; Skanes, A. Worldwide Survey on the Methods, Efficacy, and Safety of Catheter Ablation for Human Atrial Fibrillation. Circulation 2005, 111, 1100–1105. [Google Scholar] [CrossRef] [PubMed]
- Mathur, S.K.; Singh, P. Transoesophageal Echocardiography Related Complications. Indian J. Anaesth. 2009, 53, 567. [Google Scholar]
- Piercy, M.; McNicol, L.; Dinh, D.T.; Story, D.A.; Smith, J.A. Major Complications Related to the Use of Transesophageal Echocardiography in Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2009, 23, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Freitas-Ferraz, A.B.; Rodés-Cabau, J.; Vega, L.J.; Beaudoin, J.; O’Connor, K.; Turgeon, P.Y.; Paradis, J.M.; Ferreira-Neto, A.; Asmarats, L.; Champagne, J.; et al. Transesophageal echocardiography complications associated with interventional cardiology procedures. Am. Heart J. 2020, 221, 19–28. [Google Scholar] [CrossRef]
- Sobolev, M.; Shiloh, A.L.; Di Biase, L.; Slovut, D.P. Ultrasound-guided cannulation of the femoral vein in electrophysiological procedures: A systematic review and meta-analysis. EP Eur. 2016, 19, 850–855. [Google Scholar] [CrossRef]
- Wiles, B.M.; Child, N.; Roberts, P.R. How to achieve ultrasound-guided femoral venous access: The new standard of care in the electrophysiology laboratory. J. Interv. Card. Electrophysiol. 2017, 49, 3–9. [Google Scholar] [CrossRef]
- Rodriguez Munoz, D.; Franco Diez, E.; Moreno, J.; Lumia, G.; Carbonell San Roman, A.; Segura De La Cal, T.; Matia Frances, R.; Hernandez Madrid, A.; Zamorano Gomez, J.L. Wireless Ultrasound Guidance for Femoral Venous Cannulation in Electrophysiology: Impact on Safety, Efficacy, and Procedural Delay. Pacing Clin. Electrophysiol. 2015, 38, 1058–1065. [Google Scholar] [CrossRef]
- Knuuti, K.S.; Saraste, A. 2014 ESC/ESA Guidelines on non-cardiac surgery: Cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: Cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur. Heart J. 2014, 35, 2383–2431. [Google Scholar] [CrossRef]
| Demographics | |||
|---|---|---|---|
| Age (years, mean ± STD) | 65.8 ± 0.6 | ||
| Gender (% female) | 38.9% | ||
| BMI (mean ± STD) | 28.2 ± 0.3 | ||
| Atrial fibrillation | |||
| Paroxysmal | 320 | (79.2%) | |
| Persistent | 71 | (17.6%) | |
| Long persistent | 13 | (3.2%) | |
| CHA2DS2-VASc | |||
| 0 | 59 | (14.6%) | |
| 1 | 75 | (18.6%) | |
| 2 | 113 | (28%) | |
| 3 | 87 | (21.5%) | |
| 4 | 51 | (12.6%) | |
| 5 | 11 | (2.7%) | |
| 6 | 8 | (2%) | |
| 7 | 0 | (0%) | |
| 8 | 0 | (0%) | |
| 9 | 0 | (0%) | |
| EHRA I | 48 | (11.9%) | |
| EHRA II | 282 | (69.8%) | |
| EHRA III | 67 | (16.6%) | |
| EHRA IV | 7 | (1.7%) | |
| Primary intervention | 302 | (79.2%) | |
| Re-do intervention | 104 | (20.8%) | |
| Anticoagulation | |||
| Vitamin K antagonists | 23 | (5.7%) | |
| Thrombin inhibitors | 16 | (4%) | |
| Factor Xa antagonists | 329 | (81.4%) | |
| None | 36 | (8.9%) | |
| Venous-Access-Related | ||
|---|---|---|
| Hematoma * | 10 | 2.4% |
| - AV-fistula | 4 | 1% |
| - Pseudoaneurysm | 5 | 1.2% |
| Thrombosis | 1 | 0.2% |
| Infection | 0 | 0% |
| Transseptal-access-related | ||
| Aortic root puncture | 0 | 0% |
| Aortic dissection | 0 | 0% |
| Pericardial effusion | 0 | 0% |
| - Tamponade | 0 | 0% |
| Cardiac perforation | 0 | 0% |
| Myocardial infarction | 0 | 0% |
| Embolism | 0 | 0% |
| - Stroke or transient ischemic attack | 0 | 0% |
| - Peripheral arterial occlusion | 0 | 0% |
| Ablation-related | ||
| Pulmonary vein stenosis | 0 | 0% |
| Phrenic nerve palsy | 0 | 0% |
| Atrio-esophageal fistula | 0 | 0% |
| Valvular lesions | 0 | 0% |
| AV-Block | 0 | 0% |
| TEE-related | ||
| Gastroesophageal bleeding | 1 | 0.2% |
| Gastroesophageal rupture | 0 | 0% |
| Major complications | ||
| Death | 0 | 0% |
| Myocardial infarction | 0 | 0% |
| Stroke | 0 | 0% |
| Emergency vascular, cardiac or visceral surgery | 0 | 0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zuercher, R.; Herling, A.; Schmidt, M.T.; Bachmann, M.; Winnik, S.; Duru, F.; Eriksson, U. Transesophageal Echocardiography-Guided Transseptal Left Atrial Access to Improve Safety in Patients Undergoing Pulmonary Vein Isolation. J. Clin. Med. 2022, 11, 2546. https://doi.org/10.3390/jcm11092546
Zuercher R, Herling A, Schmidt MT, Bachmann M, Winnik S, Duru F, Eriksson U. Transesophageal Echocardiography-Guided Transseptal Left Atrial Access to Improve Safety in Patients Undergoing Pulmonary Vein Isolation. Journal of Clinical Medicine. 2022; 11(9):2546. https://doi.org/10.3390/jcm11092546
Chicago/Turabian StyleZuercher, Rahel, Anique Herling, Marc T. Schmidt, Marta Bachmann, Stephan Winnik, Firat Duru, and Urs Eriksson. 2022. "Transesophageal Echocardiography-Guided Transseptal Left Atrial Access to Improve Safety in Patients Undergoing Pulmonary Vein Isolation" Journal of Clinical Medicine 11, no. 9: 2546. https://doi.org/10.3390/jcm11092546
APA StyleZuercher, R., Herling, A., Schmidt, M. T., Bachmann, M., Winnik, S., Duru, F., & Eriksson, U. (2022). Transesophageal Echocardiography-Guided Transseptal Left Atrial Access to Improve Safety in Patients Undergoing Pulmonary Vein Isolation. Journal of Clinical Medicine, 11(9), 2546. https://doi.org/10.3390/jcm11092546







