Lymph Nodes Evaluation in Rectal Cancer: Where Do We Stand and Future Perspective
Abstract
:1. Introduction
2. MRI Protocol: The Basics
3. Lymph Nodes and Tumor Deposits: Anatomical Considerations
4. Nodal Assessment in Clinical Routine: Morphology
5. Advanced MRI Techniques: Diffusion-Weighted Imaging (DWI)
6. Evolution of DWI Technique: Intravoxel Incoherent Motion (IVIM) and Non-Gaussian Model (Diffusion Kurtosis Imaging, DKI)
7. Dynamic Contrast-Enhanced MRI (DCE-MRI): The Role of Perfusion
8. Positron Emission Tomography (PET): PET/CT and PET/MRI
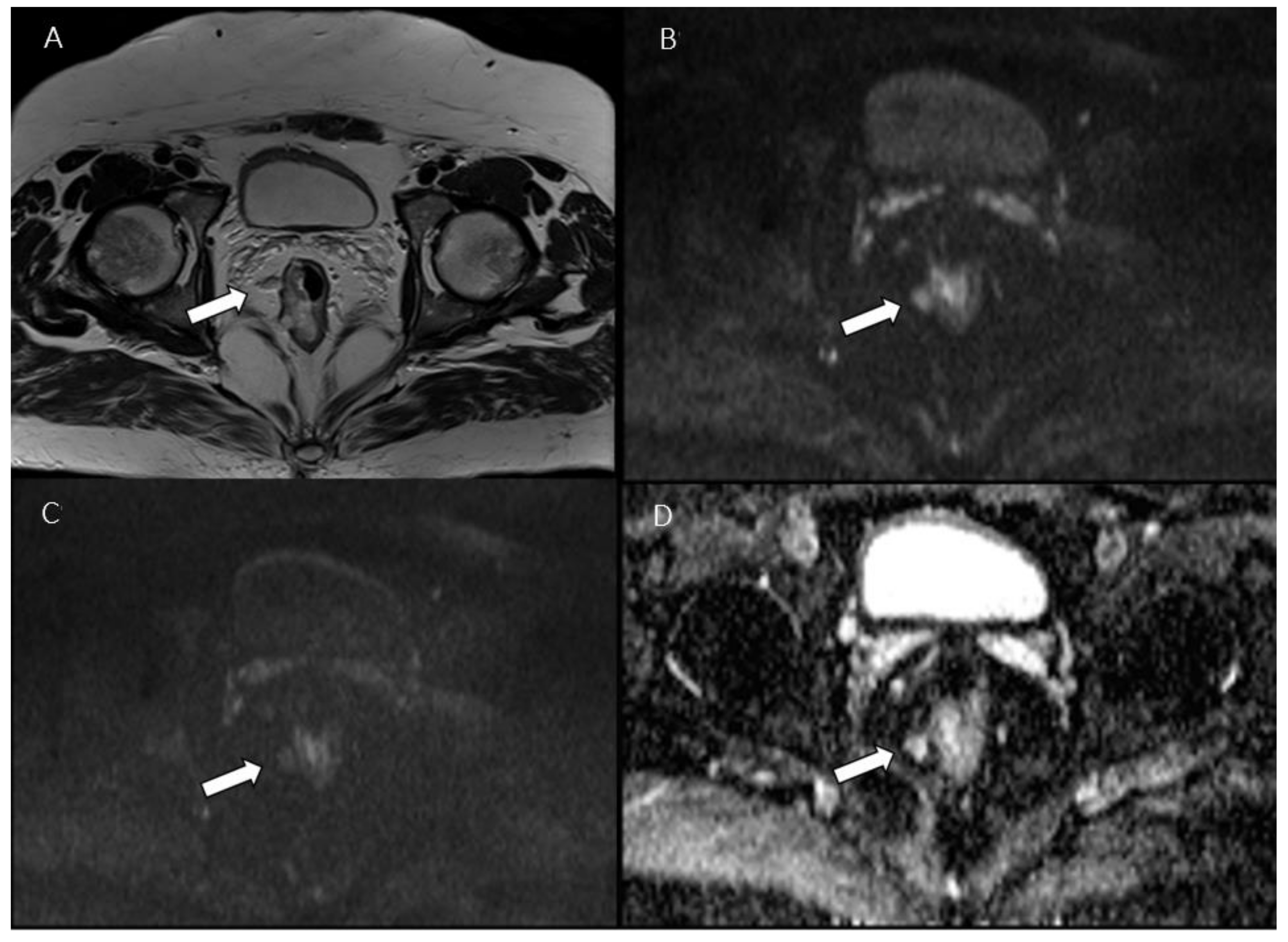
9. Radiomics: Images Are Data
10. Experimental Applications: Ultrasmall Superparamagnetic Iron Oxide (USPIO)
11. Advanced CT Techniques: Dual Energy CT (DECT)
12. Reporting
13. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Colorectal Cancer. Available online: https://seer.cancer.gov/statfacts/html/colorect.html (accessed on 26 February 2022).
- Koh, D.M.; Brown, G.; Temple, L.; Blake, H.; Raja, A.; Toomey, P.; Bett, N.; Farhat, S.; Norman, A.R.; Daniels, I.; et al. Distribution of Mesorectal Lymph Nodes in Rectal Cancer: In Vivo MR Imaging Compared with Histopathological Examination. Initial Observations. Eur. Radiol. 2005, 15, 1650–1657. [Google Scholar] [CrossRef] [PubMed]
- Horvat, N.; Rocha, C.C.T.; Oliveira, B.C.; Petkovska, I.; Gollub, M.J. MRI of Rectal Cancer: Tumor Staging, Imaging Techniques, and Management. RadioGraphics 2019, 39, 367–387. [Google Scholar] [CrossRef] [PubMed]
- Benson, A.B.; Venook, A.P.; Al-Hawary, M.M.; Arain, M.A.; Chen, Y.-J.; Ciombor, K.K.; Cohen, S.; Cooper, H.S.; Deming, D.; Garrido-Laguna, I.; et al. NCCN Guidelines Insights: Rectal Cancer, Version 6.2020: Featured Updates to the NCCN Guidelines. J. Natl. Compr. Cancer Netw. 2020, 18, 806–815. [Google Scholar] [CrossRef]
- Nicholls, R.J.; Zinicola, R.; Haboubi, N. Extramural Spread of Rectal Cancer and the AJCC Cancer Staging Manual 8th Edition. Ann. Oncol. 2019, 30, 1394–1395. [Google Scholar] [CrossRef]
- Glynne-Jones, R.; Wyrwicz, L.; Tiret, E.; Brown, G.; Rödel, C.; Cervantes, A.; Arnold, D.; Committee, on behalf of the E.G. Rectal Cancer: ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2017, 28, iv22–iv40. [Google Scholar] [CrossRef]
- Al-Sukhni, E.; Milot, L.; Fruitman, M.; Beyene, J.; Victor, J.C.; Schmocker, S.; Brown, G.; McLeod, R.; Kennedy, E. Diagnostic Accuracy of MRI for Assessment of T Category, Lymph Node Metastases, and Circumferential Resection Margin Involvement in Patients with Rectal Cancer: A Systematic Review and Meta-Analysis. Ann. Surg. Oncol. 2012, 19, 2212–2223. [Google Scholar] [CrossRef] [Green Version]
- Park, J.S.; Jang, Y.-J.; Choi, G.-S.; Park, S.Y.; Kim, H.J.; Kang, H.; Cho, S.H. Accuracy of Preoperative MRI in Predicting Pathology Stage in Rectal Cancers. Dis. Colon. Rectum. 2014, 57, 32–38. [Google Scholar] [CrossRef]
- Zhuang, Z.; Zhang, Y.; Wei, M.; Yang, X.; Wang, Z. Magnetic Resonance Imaging Evaluation of the Accuracy of Various Lymph Node Staging Criteria in Rectal Cancer: A Systematic Review and Meta-Analysis. Front. Oncol. 2021, 11, 709070. [Google Scholar] [CrossRef]
- Li, X.-T.; Sun, Y.-S.; Tang, L.; Cao, K.; Zhang, X.-Y. Evaluating Local Lymph Node Metastasis with Magnetic Resonance Imaging, Endoluminal Ultrasound and Computed Tomography in Rectal Cancer: A Meta-analysis. Color. Dis. 2015, 17, O129–O135. [Google Scholar] [CrossRef]
- Brown, G.; Richards, C.J.; Bourne, M.W.; Newcombe, R.G.; Radcliffe, A.G.; Dallimore, N.S.; Williams, G.T. Morphologic Predictors of Lymph Node Status in Rectal Cancer with Use of High-Spatial-Resolution MR Imaging with Histopathologic Comparison. Radiology 2003, 227, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Kotanagi, H.; Fukuoka, T.; Shibata, Y.; Yoshioka, T.; Aizawa, O.; Saito, Y.; Tur, G.E.; Koyama, K. The Size of Regional Lymph Nodes Does Not Correlate with the Presence or Absence of Metastasis in Lymph Nodes in Rectal Cancer. J. Surg. Oncol. 1993, 54, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Bertocchi, E.; Barugola, G.; Nicosia, L.; Mazzola, R.; Ricchetti, F.; Dell’Abate, P.; Alongi, F.; Ruffo, G. A Comparative Analysis between Radiation Dose Intensification and Conventional Fractionation in Neoadjuvant Locally Advanced Rectal Cancer: A Monocentric Prospective Observational Study. Radiol. Med. 2020, 125, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Weiser, M.R. AJCC 8th Edition: Colorectal Cancer. Ann. Surg. Oncol. 2018, 25, 1454–1455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beets-Tan, R.G.H.; Lambregts, D.M.J.; Maas, M.; Bipat, S.; Barbaro, B.; Curvo-Semedo, L.; Fenlon, H.M.; Gollub, M.J.; Gourtsoyianni, S.; Halligan, S.; et al. Magnetic Resonance Imaging for Clinical Management of Rectal Cancer: Updated Recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) Consensus Meeting. Eur. Radiol. 2017, 23, 2522. [Google Scholar] [CrossRef] [PubMed]
- Gollub, M.J.; Arya, S.; Beets-Tan, R.G.H.; dePrisco, G.; Gonen, M.; Jhaveri, K.; Kassam, Z.; Kaur, H.; Kim, D.; Knezevic, A.; et al. Use of Magnetic Resonance Imaging in Rectal Cancer Patients: Society of Abdominal Radiology (SAR) Rectal Cancer Disease-Focused Panel (DFP) Recommendations 2017. Abdom. Radiol. 2018, 43, 2893–2902. [Google Scholar] [CrossRef]
- Fusco, R.; Petrillo, M.; Granata, V.; Filice, S.; Sansone, M.; Catalano, O.; Petrillo, A. Magnetic Resonance Imaging Evaluation in Neoadjuvant Therapy of Locally Advanced Rectal Cancer: A Systematic Review. Radiol. Oncol. 2017, 51, 252–262. [Google Scholar] [CrossRef]
- Nougaret, S.; Reinhold, C.; Mikhael, H.W.; Rouanet, P.; Bibeau, F.; Brown, G. The Use of MR Imaging in Treatment Planning for Patients with Rectal Carcinoma: Have You Checked the “DISTANCE”? Radiology 2013, 268, 330–344. [Google Scholar] [CrossRef]
- Kaur, H.; Choi, H.; You, Y.N.; Rauch, G.M.; Jensen, C.T.; Hou, P.; Chang, G.J.; Skibber, J.M.; Ernst, R.D. MR Imaging for Preoperative Evaluation of Primary Rectal Cancer: Practical Considerations. RadioGraphics 2012, 32, 389–409. [Google Scholar] [CrossRef]
- Assadsangabi, R.; Babaei, R.; Songco, C.; Ivanovic, V.; Bobinski, M.; Chen, Y.J.; Nabavizadeh, S.A. Multimodality Oncologic Evaluation of Superficial Neck and Facial Lymph Nodes. Radiol. Med. 2021, 126, 1074–1084. [Google Scholar] [CrossRef]
- Valentini, V.; Gambacorta, M.A.; Barbaro, B.; Chiloiro, G.; Coco, C.; Das, P.; Fanfani, F.; Joye, I.; Kachnic, L.; Maingon, P.; et al. International Consensus Guidelines on Clinical Target Volume Delineation in Rectal Cancer. Radiother. Oncol. 2016, 120, 195–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.M.; Charnsangavej, C.; Yoshimitsu, K.; Herron, D.H.; Robinson, T.J.; Wallace, S. Pathways of Nodal Metastasis from Pelvic Tumors: CT Demonstration. Radiographics 1994, 14, 1309–1321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charnsangavej, C.; Dubrow, R.A.; Varma, D.G.; Herron, D.H.; Robinson, T.J.; Whitley, N.O. CT of the Mesocolon. Part Pathologic Considerations. Radiographics 1993, 13, 1309–1322. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Ernst, R.D.; Rauch, G.M.; Harisinghani, M. Nodal Drainage Pathways in Primary Rectal Cancer: Anatomy of Regional and Distant Nodal Spread. Abdom. Radiol. 2019, 44, 3527–3535. [Google Scholar] [CrossRef]
- Zheng, Y.; Zhou, Z.; Li, L.; Lei, W.; Deng, Y.; Chen, D.; Liu, W. Distribution and Patterns of Lymph Nodes Metastases and Micrometastases in the Mesorectum of Rectal Cancer. J. Surg. Oncol. 2007, 96, 213–219. [Google Scholar] [CrossRef]
- Engelen, S.M.E.; Beets-Tan, R.G.H.; Lahaye, M.J.; Kessels, A.G.H.; Beets, G.L. Location of Involved Mesorectal and Extramesorectal Lymph Nodes in Patients with Primary Rectal Cancer: Preoperative Assessment with MR Imaging. Eur. J. Surg. Oncol. 2008, 34, 776–781. [Google Scholar] [CrossRef]
- Cserni, G.; Tarján, M.; Bori, R. Distance of Lymph Nodes from the Tumor. Arch. Pathol. Lab. Med. 2001, 125, 246–249. [Google Scholar] [CrossRef]
- Steup, W.H.; Moriya, Y.; van de Velde, C.J.H. Patterns of Lymphatic Spread in Rectal Cancer. A Topographical Analysis on Lymph Node Metastases. Eur. J. Cancer 2002, 38, 911–918. [Google Scholar] [CrossRef]
- Gollub, M.J.; Maas, M.; Weiser, M.; Beets, G.L.; Goodman, K.; Berkers, L.; Beets-Tan, R.G.H. Recognition of the Anterior Peritoneal Reflection at Rectal MRI. Am. J. Roentgenol. 2013, 200, 97–101. [Google Scholar] [CrossRef]
- Yao, Y.-F.; Wang, L.; Liu, Y.-Q.; Li, J.-Y.; Gu, J. Lymph Node Distribution and Pattern of Metastases in the Mesorectum Following Total Mesorectal Excision Using the Modified Fat Clearing Technique. J. Clin. Pathol. 2011, 64, 1073. [Google Scholar] [CrossRef]
- Morikawa, E.; Yasutomi, M.; Shindou, K.; Matsuda, T.; Mori, N.; Hida, J.; Kubo, R.; Kitaoka, M.; Nakamura, M.; Fujimoto, K.; et al. Distribution of Metastatic Lymph Nodes in Colorectal Cancer by the Modified Clearing Method. Dis. Colon. Rectum. 1994, 37, 219–223. [Google Scholar] [CrossRef] [PubMed]
- McMahon, C.J.; Rofsky, N.M.; Pedrosa, I. Lymphatic Metastases from Pelvic Tumors: Anatomic Classification, Characterization, and Staging. Radiology 2009, 254, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Lambregts, D.M.J.; Bogveradze, N.; Blomqvist, L.K.; Fokas, E.; Garcia-Aguilar, J.; Glimelius, B.; Gollub, M.J.; Konishi, T.; Marijnen, C.A.M.; Nagtegaal, I.D.; et al. Current Controversies in TNM for the Radiological Staging of Rectal Cancer and How to Deal with Them: Results of a Global Online Survey and Multidisciplinary Expert Consensus. Eur. Radiol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Ogura, A.; Konishi, T.; Beets, G.L.; Cunningham, C.; Garcia-Aguilar, J.; Iversen, H.; Toda, S.; Lee, I.K.; Lee, H.X.; Uehara, K.; et al. Lateral Nodal Features on Restaging Magnetic Resonance Imaging Associated with Lateral Local Recurrence in Low Rectal Cancer After Neoadjuvant Chemoradiotherapy or Radiotherapy. JAMA Surg. 2019, 154, e192172. [Google Scholar] [CrossRef]
- Hope, T.A.; Gollub, M.J.; Arya, S.; Bates, D.D.B.; Ganeshan, D.; Harisinghani, M.; Jhaveri, K.S.; Kassam, Z.; Kim, D.H.; Korngold, E.; et al. Rectal Cancer Lexicon: Consensus Statement from the Society of Abdominal Radiology Rectal & Anal Cancer Disease-Focused Panel. Abdom. Radiol. 2019, 44, 3508–3517. [Google Scholar] [CrossRef]
- Lord, A.C.; Knijn, N.; Brown, G.; Nagtegaal, I.D. Pathways of Spread in Rectal Cancer: A Reappraisal of the True Routes to Distant Metastatic Disease. Eur. J. Cancer 2020, 128, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Nagtegaal, I.D.; Knijn, N.; Hugen, N.; Marshall, H.C.; Sugihara, K.; Tot, T.; Ueno, H.; Quirke, P. Tumor Deposits in Colorectal Cancer: Improving the Value of Modern Staging—A Systematic Review and Meta-Analysis. J. Clin. Oncol. 2017, 35, 1119–1127. [Google Scholar] [CrossRef]
- Lord, A.C.; D’Souza, N.; Pucher, P.H.; Moran, B.J.; Abulafi, A.M.; Wotherspoon, A.; Rasheed, S.; Brown, G. Significance of Extranodal Tumour Deposits in Colorectal Cancer: A Systematic Review and Meta-Analysis. Eur. J. Cancer 2017, 82, 92–102. [Google Scholar] [CrossRef]
- Lord, A.; Brown, G.; Abulafi, M.; Bateman, A.; Frankel, W.; Goldin, R.; Gopal, P.; Kirsch, R.; Loughrey, M.B.; Märkl, B.; et al. Histopathological Diagnosis of Tumour Deposits in Colorectal Cancer: A Delphi Consensus Study. Histopathology 2021, 79, 168–175. [Google Scholar] [CrossRef]
- Lord, A.C.; Moran, B.; Abulafi, M.; Rasheed, S.; Nagtegaal, I.D.; Terlizzo, M.; Brown, G. Can Extranodal Tumour Deposits Be Diagnosed on MRI? Protocol for a Multicentre Clinical Trial (the COMET Trial). BMJ Open 2020, 10, e033395. [Google Scholar] [CrossRef]
- Langman, G.; Patel, A.; Bowley, D.M. Size and Distribution of Lymph Nodes in Rectal Cancer Resection Specimens. Dis. Colon. Rectum. 2015, 58, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Nahas, S.C.; Nahas, C.S.R.; Cama, G.M.; de Azambuja, R.L.; Horvat, N.; Marques, C.F.S.; Menezes, M.R.; Junior, U.R.; Cecconello, I. Diagnostic Performance of Magnetic Resonance to Assess Treatment Response after Neoadjuvant Therapy in Patients with Locally Advanced Rectal Cancer. Abdom. Radiol. 2019, 44, 3632–3640. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhou, Z.-G.; Wang, Z.; Chen, D.-Y.; Zheng, Y.-C.; Zhao, G.-P. Nodal Spread and Micrometastasis within Mesorectum. World J. Gastroenterol. 2005, 11, 3586–3590. [Google Scholar] [CrossRef] [PubMed]
- Sloothaak, D.; Sahami, S.; van der Zaag-Loonen, H.; van der Zaag, E.; Tanis, P.; Bemelman, W.; Buskens, C. The Prognostic Value of Micrometastases and Isolated Tumour Cells in Histologically Negative Lymph Nodes of Patients with Colorectal Cancer: A Systematic Review and Meta-Analysis. Eur. J. Surg. Oncol. 2014, 40, 263–269. [Google Scholar] [CrossRef]
- Dworák, O. Number and Size of Lymph Nodes and Node Metastases in Rectal Carcinomas. Surg. Endosc. 1989, 3, 96–99. [Google Scholar] [CrossRef]
- Beets-Tan, R.G.H.; Lambregts, D.M.J.; Maas, M.; Bipat, S.; Barbaro, B.; Caseiro-Alves, F.; Curvo-Semedo, L.; Fenlon, H.M.; Gollub, M.J.; Gourtsoyianni, S.; et al. Magnetic Resonance Imaging for the Clinical Management of Rectal Cancer Patients: Recommendations from the 2012 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) Consensus Meeting. Eur. Radiol. 2013, 23, 2522–2531. [Google Scholar] [CrossRef]
- Kim, J.H.; Beets, G.L.; Kim, M.-J.; Kessels, A.G.H.; Beets-Tan, R.G.H. High-Resolution MR Imaging for Nodal Staging in Rectal Cancer: Are There Any Criteria in Addition to the Size? Eur. J. Radiol. 2004, 52, 78–83. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, C.; Zheng, Z.; Ye, F.; Liu, Y.; Zou, S.; Zhou, C. Chemical Shift Effect Predicting Lymph Node Status in Rectal Cancer Using High-Resolution MR Imaging with Node-for-Node Matched Histopathological Validation. Eur. Radiol. 2017, 27, 3845–3855. [Google Scholar] [CrossRef]
- Farshchian, N.; Tamari, S.; Farshchian, N.; Madani, H.; Rezaie, M.; Mohammadi-Motlagh, H.-R. Diagnostic Value of Chemical Shift Artifact in Distinguishing Benign Lymphadenopathy. Eur. J. Radiol. 2011, 80, 594–597. [Google Scholar] [CrossRef]
- Chen, Y.; Wen, Z.; Liu, Y.; Yang, X.; Ma, Y.; Lu, B.; Xiao, X.; Yu, S. Value of High-Resolution MRI in Detecting Lymph Node Calcifications in Patients with Rectal Cancer. Acad. Radiol. 2020, 27, 1709–1717. [Google Scholar] [CrossRef]
- Chen, Y.; Wen, Z.; Ma, Y.; Liu, Y.; Que, Y.; Yang, X.; Wu, Y.; Yu, S. Metastatic Lymph Node Calcification in Rectal Cancer: Comparison of CT and High-Resolution MRI. Jpn. J. Radiol. 2021, 39, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Gulevski, S.; Russell, M.M.; Buchwald, P. Significance, Diagnosis and Treatment of Lateral Lymph Nodes in Rectal Cancer: A Systematic Review. Int. J. Surg. Open 2019, 21, 73–82. [Google Scholar] [CrossRef]
- Kim, H.J.; Choi, G.-S.; Park, J.S.; Park, S.Y.; Cho, S.H.; Lee, S.J.; Kang, B.W.; Kim, J.G. Optimal Treatment Strategies for Clinically Suspicious Lateral Pelvic Lymph Node Metastasis in Rectal Cancer. Oncotarget 2017, 8, 100724–100733. [Google Scholar] [CrossRef] [Green Version]
- Atef, Y.; Koedam, T.W.; van Oostendorp, S.E.; Bonjer, H.J.; Wijsmuller, A.R.; Tuynman, J.B. Lateral Pelvic Lymph Node Metastases in Rectal Cancer: A Systematic Review. World J. Surg. 2019, 43, 3198–3206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogawa, S.; Hida, J.; Ike, H.; Kinugasa, T.; Ota, M.; Shinto, E.; Itabashi, M.; Okamoto, T.; Yamamoto, M.; Sugihara, K.; et al. Prediction of Lateral Pelvic Lymph Node Metastasis from Lower Rectal Cancer Using Magnetic Resonance Imaging and Risk Factors for Metastasis: Multicenter Study of the Lymph Node Committee of the Japanese Society for Cancer of the Colon and Rectum. Int. J. Colorectal. Dis. 2017, 32, 1479–1487. [Google Scholar] [CrossRef]
- Ogura, A.; Konishi, T.; Cunningham, C.; Garcia-Aguilar, J.; Iversen, H.; Toda, S.; Lee, I.K.; Lee, H.X.; Uehara, K.; Lee, P.; et al. Neoadjuvant (Chemo)Radiotherapy with Total Mesorectal Excision Only Is Not Sufficient to Prevent Lateral Local Recurrence in Enlarged Nodes: Results of the Multicenter Lateral Node Study of Patients with Low CT3/4 Rectal Cancer. J. Clin. Oncol. 2019, 37, 33–43. [Google Scholar] [CrossRef]
- Heijnen, L.A.; Maas, M.; Beets-Tan, R.G.; Berkhof, M.; Lambregts, D.M.; Nelemans, P.J.; Riedl, R.; Beets, G.L. Nodal Staging in Rectal Cancer: Why Is Restaging after Chemoradiation More Accurate than Primary Nodal Staging? Int. J. Colorectal. Dis. 2016, 31, 1157–1162. [Google Scholar] [CrossRef] [Green Version]
- Almlöv, K.; Woisetschläger, M.; Loftås, P.; Hallböök, O.; Elander, N.O.; Sandström, P. MRI Lymph Node Evaluation for Prediction of Metastases in Rectal Cancer. Anticancer Res. 2020, 40, 2757–2763. [Google Scholar] [CrossRef]
- Lahaye, M.J.; Beets, G.L.; Engelen, S.M.E.; Kessels, A.G.H.; de Bruïne, A.P.; Kwee, H.W.S.; van Engelshoven, J.M.A.; van de Velde, C.J.H.; Beets-Tan, R.G.H. Locally Advanced Rectal Cancer: MR Imaging for Restaging after Neoadjuvant Radiation Therapy with Concomitant Chemotherapy Part II. What Are the Criteria to Predict Involved Lymph Nodes? Radiology 2009, 252, 81–91. [Google Scholar] [CrossRef]
- Bihan, D.L.; Breton, E.; Lallemand, D.; Grenier, P.; Cabanis, E.; Laval-Jeantet, M. MR Imaging of Intravoxel Incoherent Motions: Application to Diffusion and Perfusion in Neurologic Disorders. Radiology 1986, 161, 401–407. [Google Scholar] [CrossRef] [Green Version]
- Qayyum, A. Diffusion-Weighted Imaging in the Abdomen and Pelvis: Concepts and Applications. RadioGraphics 2009, 29, 1797–1810. [Google Scholar] [CrossRef] [PubMed]
- Baliyan, V.; Das, C.J.; Sharma, R.; Gupta, A.K. Diffusion Weighted Imaging: Technique and Applications. World J. Radiol. 2016, 8, 785–798. [Google Scholar] [CrossRef] [PubMed]
- Berardo, S.; Sukhovei, L.; Andorno, S.; Carriero, A.; Stecco, A. Quantitative Bone Marrow Magnetic Resonance Imaging through Apparent Diffusion Coefficient and Fat Fraction in Multiple Myeloma Patients. Radiol. Med. 2021, 126, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Liheng, M.; Guofan, X.; Balzano, R.F.; Yuying, L.; Weifeng, H.; Ning, Y.; Yayun, J.; Mouyuan, L.; Guglielmi, G. The Value of DTI: Achieving High Diagnostic Performance for Brain Metastasis. Radiol. Med. 2021, 126, 291–298. [Google Scholar] [CrossRef]
- Momeni, M.; Asadzadeh, M.; Mowla, K.; Hanafi, M.G.; Gharibvand, M.M.; Sahraeizadeh, A. Sensitivity and Specificity Assessment of DWI and ADC for the Diagnosis of Osteoporosis in Postmenopausal Patients. Radiol. Med. 2020, 125, 68–74. [Google Scholar] [CrossRef]
- Gunbey, H.P.; Has, A.C.; Aslan, K.; Saglam, D.; Avcı, U.; Sayıt, A.T.; Incesu, L. Microstructural White Matter Abnormalities in Hypothyroidism Evaluation with Diffusion Tensor Imaging Tract-Based Spatial Statistical Analysis. Radiol. Med. 2021, 126, 283–290. [Google Scholar] [CrossRef]
- Pietragalla, M.; Nardi, C.; Bonasera, L.; Mungai, F.; Taverna, C.; Novelli, L.; Renzis, A.G.D.D.; Calistri, L.; Tomei, M.; Occhipinti, M.; et al. The Role of Diffusion-Weighted and Dynamic Contrast Enhancement Perfusion-Weighted Imaging in the Evaluation of Salivary Glands Neoplasms. Radiol. Med. 2020, 125, 851–863. [Google Scholar] [CrossRef]
- Albano, D.; Stecco, A.; Micci, G.; Sconfienza, L.M.; Colagrande, S.; Reginelli, A.; Grassi, R.; Carriero, A.; Midiri, M.; Lagalla, R.; et al. Whole-Body Magnetic Resonance Imaging (WB-MRI) in Oncology: An Italian Survey. Radiol. Med. 2021, 126, 299–305. [Google Scholar] [CrossRef]
- Romano, A.; Covelli, E.; Confaloni, V.; Rossi-Espagnet, M.C.; Butera, G.; Barbara, M.; Bozzao, A. Role of Non-Echo-Planar Diffusion-Weighted Images in the Identification of Recurrent Cholesteatoma of the Temporal Bone. Radiol. Med. 2020, 125, 75–79. [Google Scholar] [CrossRef]
- Messina, C.; Bignone, R.; Bruno, A.; Bruno, A.; Bruno, F.; Calandri, M.; Caruso, D.; Coppolino, P.; Robertis, R.D.; Gentili, F.; et al. Diffusion-Weighted Imaging in Oncology: An Update. Cancers 2020, 12, 1493. [Google Scholar] [CrossRef]
- Granata, V.; Grassi, R.; Fusco, R.; Setola, S.V.; Belli, A.; Ottaiano, A.; Nasti, G.; Porta, M.L.; Danti, G.; Cappabianca, S.; et al. Intrahepatic Cholangiocarcinoma and Its Differential Diagnosis at MRI: How Radiologist Should Assess MR Features. Radiol. Med. 2021, 126, 1584–1600. [Google Scholar] [CrossRef] [PubMed]
- Bharwani, N.; Koh, D.M. Diffusion-Weighted Imaging of the Liver: An Update. Cancer Imaging 2013, 13, 171–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taouli, B.; Koh, D.-M. Diffusion-Weighted MR Imaging of the Liver. Radiology 2010, 254, 47–66. [Google Scholar] [CrossRef] [PubMed]
- Fornell-Perez, R.; Vivas-Escalona, V.; Aranda-Sanchez, J.; Gonzalez-Dominguez, M.C.; Rubio-Garcia, J.; Aleman-Flores, P.; Lozano-Rodriguez, A.; Porcel-de-Peralta, G.; Loro-Ferrer, J.F. Primary and Post-Chemoradiotherapy MRI Detection of Extramural Venous Invasion in Rectal Cancer: The Role of Diffusion-Weighted Imaging. Radiol. Med. 2020, 125, 522–530. [Google Scholar] [CrossRef]
- Heijnen, L.A.; Lambregts, D.M.J.; Mondal, D.; Martens, M.H.; Riedl, R.G.; Beets, G.L.; Beets-Tan, R.G.H. Diffusion-Weighted MR Imaging in Primary Rectal Cancer Staging Demonstrates but Does Not Characterise Lymph Nodes. Eur. Radiol. 2013, 23, 3354–3360. [Google Scholar] [CrossRef]
- Lambregts, D.M.J.; Maas, M.; Riedl, R.G.; Bakers, F.C.H.; Verwoerd, J.L.; Kessels, A.G.H.; Lammering, G.; Boetes, C.; Beets, G.L.; Beets-Tan, R.G.H. Value of ADC Measurements for Nodal Staging after Chemoradiation in Locally Advanced Rectal Cancer—a per Lesion Validation Study. Eur. Radiol. 2011, 21, 265–273. [Google Scholar] [CrossRef] [Green Version]
- Nakai, G.; Matsuki, M.; Inada, Y.; Tatsugami, F.; Tanikake, M.; Narabayashi, I.; Yamada, T. Detection and Evaluation of Pelvic Lymph Nodes in Patients with Gynecologic Malignancies Using Body Diffusion-Weighted Magnetic Resonance Imaging. J. Comput. Assist. Tomo. 2008, 32, 764–768. [Google Scholar] [CrossRef]
- Mir, N.; Sohaib, S.; Collins, D.; Koh, D. TECHNICAL ARTICLE: Fusion of High B-value Diffusion-weighted and T2-weighted MR Images Improves Identification of Lymph Nodes in the Pelvis. J. Med. Imaging Radiat. Oncol. 2010, 54, 358–364. [Google Scholar] [CrossRef]
- Mizukami, Y.; Ueda, S.; Mizumoto, A.; Sasada, T.; Okumura, R.; Kohno, S.; Takabayashi, A. Diffusion-Weighted Magnetic Resonance Imaging for Detecting Lymph Node Metastasis of Rectal Cancer. World J. Surg. 2011, 35, 895–899. [Google Scholar] [CrossRef]
- Van Heeswijk, M.M.; Lambregts, D.M.J.; Palm, W.M.; Hendriks, B.; Maas, M.; Beets, G.; Beets-Tan, R.G.H. DWI for Assessment of Rectal Cancer Nodes After Chemoradiotherapy: Is the Absence of Nodes at DWI Proof of a Negative Nodal Status? Am. J. Roentgenol. 2016, 208, W79–W84. [Google Scholar] [CrossRef]
- Bipat, S.; Glas, A.S.; Slors, F.J.M.; Zwinderman, A.H.; Bossuyt, P.M.M.; Stoker, J. Rectal Cancer: Local Staging and Assessment of Lymph Node Involvement with Endoluminal US, CT, and MR Imaging—A Meta-Analysis. Radiology 2004, 232, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Lahaye, M.; Engelen, S.; Nelemans, P.; Beets, G.; van de Velde, C.; van Engelshoven, J.; Beets-Tan, R. Imaging for Predicting the Risk Factors—the Circumferential Resection Margin and Nodal Disease—of Local Recurrence in Rectal Cancer: A Meta-Analysis. Semin. Ultrasound Ct MRI 2005, 26, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Ryu, K.H.; Yoon, J.-H.; Lee, Y.; Paik, J.H.; Kim, S.J.; Jung, H.K.; Lee, K.H. Apparent Diffusion Coefficient for Lymph Node Characterization after Chemoradiation Therapy for Locally Advanced Rectal Cancer. Acta Radiol. 2014, 56, 1446–1453. [Google Scholar] [CrossRef]
- Cho, E.Y.; Kim, S.H.; Yoon, J.-H.; Lee, Y.; Lim, Y.-J.; Kim, S.-J.; Baek, H.J.; Eun, C.K. Apparent Diffusion Coefficient for Discriminating Metastatic from Non-Metastatic Lymph Nodes in Primary Rectal Cancer. Eur. J. Radiol. 2013, 82, e662–e668. [Google Scholar] [CrossRef] [PubMed]
- Kwee, T.C.; Takahara, T.; Luijten, P.R.; Nievelstein, R.A.J. ADC Measurements of Lymph Nodes: Inter- and Intra-Observer Reproducibility Study and an Overview of the Literature. Eur. J. Radiol. 2010, 75, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Surov, A.; Meyer, H.-J.; Pech, M.; Powerski, M.; Omari, J.; Wienke, A. Apparent Diffusion Coefficient Cannot Discriminate Metastatic and Non-Metastatic Lymph Nodes in Rectal Cancer: A Meta-Analysis. Int. J. Colorectal. Dis. 2021, 36, 2189–2197. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.-L.; Chen, G.-W.; Pu, H.; Yin, L.-L.; Li, Z.-L.; Song, B.; Li, H. DWI and T2-Weighted MRI Volumetry in Resectable Rectal Cancer: Correlation with Lymphovascular Invasion and Lymph Node Metastases. Am. J. Roentgenol. 2019, 212, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Taffel, M.T.; Johnson, E.J.; Chandarana, H. Diffusion Quantification in Body Imaging. Top. Magn. Reson. Imaging 2017, 26, 243–249. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; Reginelli, A.; Delrio, P.; Selvaggi, F.; Grassi, R.; Izzo, F.; Petrillo, A. Diffusion Kurtosis Imaging in Patients with Locally Advanced Rectal Cancer: Current Status and Future Perspectives. J. Int. Med. Res. 2019, 47, 2351–2360. [Google Scholar] [CrossRef] [Green Version]
- Bihan, D.L.; Breton, E.; Lallemand, D.; Aubin, M.L.; Vignaud, J.; Laval-Jeantet, M. Separation of Diffusion and Perfusion in Intravoxel Incoherent Motion MR Imaging. Radiology 1988, 168, 497–505. [Google Scholar] [CrossRef]
- Lewin, M.; Fartoux, L.; Vignaud, A.; Arrivé, L.; Menu, Y.; Rosmorduc, O. The Diffusion-Weighted Imaging Perfusion Fraction f Is a Potential Marker of Sorafenib Treatment in Advanced Hepatocellular Carcinoma: A Pilot Study. Eur. Radiol. 2011, 21, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Ogura, A.; Sotome, H.; Asai, A.; Fuju, A. Evaluation of Capillary Blood Volume in the Lower Limb Muscles after Exercise by Intravoxel Incoherent Motion. Radiol. Med. 2020, 125, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Lu, B.; Yang, X.; Xiao, X.; Chen, Y.; Yan, X.; Yu, S. Intravoxel Incoherent Motion Diffusion-Weighted Imaging of Primary Rectal Carcinoma: Correlation with Histopathology. Med. Sci. Monit. 2018, 24, 2429–2436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Surov, A.; Meyer, H.J.; Höhn, A.-K.; Behrmann, C.; Wienke, A.; Spielmann, R.P.; Garnov, N. Correlations between Intravoxel Incoherent Motion (IVIM) Parameters and Histological Findings in Rectal Cancer: Preliminary Results. Oncotarget 2017, 8, 21974–21983. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Xu, Y.; Song, A.; Shi, K.; Wang, W. Intravoxel Incoherent Motion MRI of Rectal Cancer: Correlation of Diffusion and Perfusion Characteristics with Prognostic Tumor Markers. Am. J. Roentgenol. 2018, 210, W139–W147. [Google Scholar] [CrossRef]
- Yu, X.; Wen, L.; Hou, J.; Bi, F.; Hu, P.; Wang, H.; Wang, W. Discrimination between Metastatic and Nonmetastatic Mesorectal Lymph Nodes in Rectal Cancer Using Intravoxel Incoherent Motion Diffusion-Weighted Magnetic Resonance Imaging. Acad. Radiol. 2016, 23, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Qiu, L.; Liu, X.; Liu, S.; Weng, Z.; Chen, X.; Feng, Y.; Cai, X.; Guo, C. Role of Quantitative Intravoxel Incoherent Motion Parameters in the Preoperative Diagnosis of Nodal Metastasis in Patients with Rectal Carcinoma. J. Magn. Reson. Imaging 2016, 44, 1031–1039. [Google Scholar] [CrossRef]
- Long, L.; Zhang, H.; He, X.; Zhou, J.; Guo, D.; Liu, X. Value of Intravoxel Incoherent Motion Magnetic Resonance Imaging for Differentiating Metastatic from Nonmetastatic Mesorectal Lymph Nodes with Different Short-Axis Diameters in Rectal Cancer. J. Cancer Res. Ther. 2019, 15, 1508. [Google Scholar] [CrossRef]
- Minutoli, F.; Pergolizzi, S.; Blandino, A.; Mormina, E.; Amato, E.; Gaeta, M. Effect of Granulocyte Colony-Stimulating Factor on Bone Marrow: Evaluation by Intravoxel Incoherent Motion and Dynamic Contrast-Enhanced Magnetic Resonance Imaging. Radiol. Med. 2020, 125, 280–287. [Google Scholar] [CrossRef]
- Fischbein, N.J.; Noworolski, S.M.; Henry, R.G.; Kaplan, M.J.; Dillon, W.P.; Nelson, S.J. Assessment of Metastatic Cervical Adenopathy Using Dynamic Contrast-Enhanced MR Imaging. Am. J. Neuroradiol. 2003, 24, 301–311. [Google Scholar]
- Zhang, S.; Jia, Q.; Zhang, Z.; Liang, C.; Chen, W.; Qiu, Q.; Li, H. Intravoxel Incoherent Motion MRI: Emerging Applications for Nasopharyngeal Carcinoma at the Primary Site. Eur. Radiol. 2014, 24, 1998–2004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.; Lin, J.; Liu, K.; Chen, C.; Liu, H.; Lv, P.; Fu, C.; Zeng, M. Intravoxel Incoherent Motion Diffusion-Weighted MR Imaging in Differentiation of Lung Cancer from Obstructive Lung Consolidation: Comparison and Correlation with Pharmacokinetic Analysis from Dynamic Contrast-Enhanced MR Imaging. Eur. Radiol. 2014, 24, 1914–1922. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Peng, W.; Zhou, L.; Wang, H. Biexponential Apparent Diffusion Coefficients Values in the Prostate: Comparison among Normal Tissue, Prostate Cancer, Benign Prostatic Hyperplasia and Prostatitis. Korean J. Radiol. 2013, 14, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Sumi, M.; Cauteren, M.V.; Sumi, T.; Obara, M.; Ichikawa, Y.; Nakamura, T. Salivary Gland Tumors: Use of Intravoxel Incoherent Motion MR Imaging for Assessment of Diffusion and Perfusion for the Differentiation of Benign from Malignant Tumors. Radiology 2012, 263, 770–777. [Google Scholar] [CrossRef] [PubMed]
- Lemke, A.; Laun, F.B.; Simon, D.; Stieltjes, B.; Schad, L.R. An in Vivo Verification of the Intravoxel Incoherent Motion Effect in Diffusion-weighted Imaging of the Abdomen. Magnet. Reson. Med. 2010, 64, 1580–1585. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.H.; Helpern, J.A. MRI Quantification of Non-Gaussian Water Diffusion by Kurtosis Analysis. NMR Biomed. 2010, 23, 698–710. [Google Scholar] [CrossRef] [PubMed]
- Sun, K.; Chen, X.; Chai, W.; Fei, X.; Fu, C.; Yan, X.; Zhan, Y.; Chen, K.; Shen, K.; Yan, F. Breast Cancer: Diffusion Kurtosis MR Imaging—Diagnostic Accuracy and Correlation with Clinical-Pathologic Factors. Radiology 2015, 277, 46–55. [Google Scholar] [CrossRef] [Green Version]
- Suo, S.; Chen, X.; Wu, L.; Zhang, X.; Yao, Q.; Fan, Y.; Wang, H.; Xu, J. Non-Gaussian Water Diffusion Kurtosis Imaging of Prostate Cancer. Magn. Reson. Imaging 2014, 32, 421–427. [Google Scholar] [CrossRef]
- Nogueira, L.; Brandão, S.; Matos, E.; Nunes, R.G.; Loureiro, J.; Ramos, I.; Ferreira, H.A. Application of the Diffusion Kurtosis Model for the Study of Breast Lesions. Eur. Radiol. 2014, 24, 1197–1203. [Google Scholar] [CrossRef]
- Rosenkrantz, A.B.; Sigmund, E.E.; Winnick, A.; Niver, B.E.; Spieler, B.; Morgan, G.R.; Hajdu, C.H. Assessment of Hepatocellular Carcinoma Using Apparent Diffusion Coefficient and Diffusion Kurtosis Indices: Preliminary Experience in Fresh Liver Explants. Magn. Reson. Imaging 2012, 30, 1534–1540. [Google Scholar] [CrossRef]
- Cauter, S.V.; Veraart, J.; Sijbers, J.; Peeters, R.R.; Himmelreich, U.; Keyzer, F.D.; Gool, S.W.V.; Calenbergh, F.V.; Vleeschouwer, S.D.; Hecke, W.V.; et al. Gliomas: Diffusion Kurtosis MR Imaging in Grading. Radiology 2012, 263, 492–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raab, P.; Hattingen, E.; Franz, K.; Zanella, F.E.; Lanfermann, H. Cerebral Gliomas: Diffusional Kurtosis Imaging Analysis of Microstructural Differences. Radiology 2010, 254, 876–881. [Google Scholar] [CrossRef] [PubMed]
- Rosenkrantz, A.B.; Sigmund, E.E.; Johnson, G.; Babb, J.S.; Mussi, T.C.; Melamed, J.; Taneja, S.S.; Lee, V.S.; Jensen, J.H. Prostate Cancer: Feasibility and Preliminary Experience of a Diffusional Kurtosis Model for Detection and Assessment of Aggressiveness of Peripheral Zone Cancer. Radiology 2012, 264, 126–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, Z.; Chen, Y.; Yang, X.; Lu, B.; Liu, Y.; Shen, B.; Yu, S. Application of Magnetic Resonance Diffusion Kurtosis Imaging for Distinguishing Histopathologic Subtypes and Grades of Rectal Carcinoma. Cancer Imaging 2019, 19, 8. [Google Scholar] [CrossRef]
- Zhu, L.; Pan, Z.; Ma, Q.; Yang, W.; Shi, H.; Fu, C.; Yan, X.; Du, L.; Yan, F.; Zhang, H. Diffusion Kurtosis Imaging Study of Rectal Adenocarcinoma Associated with Histopathologic Prognostic Factors: Preliminary Findings. Radiology 2017, 284, 66–76. [Google Scholar] [CrossRef]
- Hu, F.; Tang, W.; Sun, Y.; Wan, D.; Cai, S.; Zhang, Z.; Grimm, R.; Yan, X.; Fu, C.; Tong, T.; et al. The Value of Diffusion Kurtosis Imaging in Assessing Pathological Complete Response to Neoadjuvant Chemoradiation Therapy in Rectal Cancer: A Comparison with Conventional Diffusion-Weighted Imaging. Oncotarget 2017, 8, 75597–75606. [Google Scholar] [CrossRef] [Green Version]
- Yu, J.; Xu, Q.; Song, J.-C.; Li, Y.; Dai, X.; Huang, D.-Y.; Zhang, L.; Li, Y.; Shi, H.-B. The Value of Diffusion Kurtosis Magnetic Resonance Imaging for Assessing Treatment Response of Neoadjuvant Chemoradiotherapy in Locally Advanced Rectal Cancer. Eur. Radiol. 2017, 27, 1848–1857. [Google Scholar] [CrossRef]
- Yu, J.; Huang, D.; Li, Y.; Dai, X.; Shi, H. Correlation of Standard Diffusion-weighted Imaging and Diffusion Kurtosis Imaging with Distant Metastases of Rectal Carcinoma. J. Magn. Reson. Imaging 2016, 44, 221–229. [Google Scholar] [CrossRef]
- Cui, Y.; Yang, X.; Du, X.; Zhuo, Z.; Xin, L.; Cheng, X. Whole-Tumour Diffusion Kurtosis MR Imaging Histogram Analysis of Rectal Adenocarcinoma: Correlation with Clinical Pathologic Prognostic Factors. Eur. Radiol. 2017, 28, 1485–1494. [Google Scholar] [CrossRef]
- Yu, J.; Dai, X.; Zou, H.-H.; Song, J.-C.; Li, Y.; Shi, H.-B.; Xu, Q.; Shen, H. Diffusion Kurtosis Imaging in Identifying the Malignancy of Lymph Nodes during the Primary Staging of Rectal Cancer. Color. Dis. 2018, 20, 116–125. [Google Scholar] [CrossRef]
- Zhao, L.; Liang, M.; Yang, Y.; Xie, L.; Zhang, H.; Zhao, X. Value of Multiple Models of Diffusion-Weighted Imaging for Improving the Nodal Staging of Preoperatively Node-Negative Rectal Cancer. Abdom. Radiol. 2021, 46, 4548–4555. [Google Scholar] [CrossRef] [PubMed]
- Petralia, G.; Summers, P.E.; Agostini, A.; Ambrosini, R.; Cianci, R.; Cristel, G.; Calistri, L.; Colagrande, S. Dynamic Contrast-Enhanced MRI in Oncology: How We Do It. Radiol. Med. 2020, 125, 1288–1300. [Google Scholar] [CrossRef] [PubMed]
- Albano, D.; Bruno, F.; Agostini, A.; Angileri, S.A.; Benenati, M.; Bicchierai, G.; Cellina, M.; Chianca, V.; Cozzi, D.; Danti, G.; et al. Dynamic Contrast-Enhanced (DCE) Imaging: State of the Art and Applications in Whole-Body Imaging. Jpn. J. Radiol. 2021, 40, 341–366. [Google Scholar] [CrossRef] [PubMed]
- Bordonaro, V.; Ciancarella, P.; Ciliberti, P.; Curione, D.; Napolitano, C.; Santangelo, T.P.; Natali, G.L.; Rollo, M.; Guccione, P.; Pasquini, L.; et al. Dynamic Contrast-Enhanced Magnetic Resonance Lymphangiography in Pediatric Patients with Central Lymphatic System Disorders. Radiol. Med. 2021, 126, 737–743. [Google Scholar] [CrossRef]
- Coppola, A.; Platania, G.; Ticca, C.; Mattia, C.D.; Bortolato, B.; Palazzi, M.F.; Vanzulli, A. Sensitivity of CE-MRI in Detecting Local Recurrence after Radical Prostatectomy. Radiol. Med. 2020, 125, 683–690. [Google Scholar] [CrossRef]
- Gentili, F.; Guerrini, S.; Mazzei, F.G.; Volterrani, L.; Mazzei, M.A. MRL as One-Shot Examination for Patients Suffering from Lymphedema. Radiol. Med. 2020, 125, 798–799. [Google Scholar] [CrossRef]
- Brancato, V.; Costanzo, G.D.; Basso, L.; Tramontano, L.; Puglia, M.; Ragozzino, A.; Cavaliere, C. Assessment of DCE Utility for PCa Diagnosis Using PI-RADS v2.1: Effects on Diagnostic Accuracy and Reproducibility. Diagnostics 2020, 10, 164. [Google Scholar] [CrossRef] [Green Version]
- Qiu, J.; Tao, Z.-C.; Deng, K.-X.; Wang, P.; Chen, C.-Y.; Xiao, F.; Luo, Y.; Yuan, S.-Y.; Chen, H.; Huang, H. Diagnostic Accuracy of Dynamic Contrast-Enhanced Magnetic Resonance Imaging for Distinguishing Pseudoprogression from Glioma Recurrence: A Meta-Analysis. Chin. Med. J. 2021, 134, 2535–2543. [Google Scholar] [CrossRef]
- Scialpi, M.; Scialpi, P.; Martorana, E.; Torre, R.; Mancioli, F.A.; D’Andrea, A.; Blasi, A.D. Biparametric MRI with Simplified PI-RADS (S-PI-RADS) for Prostate Cancer Detection and Management: What Do Radiologist Need to Know. Radiol. Med. 2021, 126, 1660–1661. [Google Scholar] [CrossRef]
- Danti, G.; Flammia, F.; Matteuzzi, B.; Cozzi, D.; Berti, V.; Grazzini, G.; Pradella, S.; Recchia, L.; Brunese, L.; Miele, V. Gastrointestinal neuroendocrine neoplasms (GI-NENs): Hot topics in morphological, functional, and prognostic imaging. Radiol. Med. 2021, 126, 1497–1507. [Google Scholar] [CrossRef]
- Hansford, B.G.; Peng, Y.; Jiang, Y.; Vannier, M.W.; Antic, T.; Thomas, S.; McCann, S.; Oto, A. Dynamic Contrast-Enhanced MR Imaging Curve-Type Analysis: Is It Helpful in the Differentiation of Prostate Cancer from Healthy Peripheral Zone? Radiology 2015, 275, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Daniel, B.L.; Yen, Y.F.; Glover, G.H.; Ikeda, D.M.; Birdwell, R.L.; Sawyer-Glover, A.M.; Black, J.W.; Plevritis, S.K.; Jeffrey, S.S.; Herfkens, R.J. Breast Disease: Dynamic Spiral MR Imaging. Radiology 1998, 209, 499–509. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, A.; Orlandi, A.; Bufi, E.; Mercogliano, S.; Belli, P.; Manfredi, R. Automated Breast Volume Scanner (ABVS) Compared to Handheld Ultrasound (HHUS) and Contrast-Enhanced Magnetic Resonance Imaging (CE-MRI) in the Early Assessment of Breast Cancer during Neoadjuvant Chemotherapy: An Emerging Role to Monitoring Tumor Response? Radiol. Med. 2021, 126, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Khouli, R.H.E.; Macura, K.J.; Jacobs, M.A.; Khalil, T.H.; Kamel, I.R.; Dwyer, A.; Bluemke, D.A. Dynamic Contrast-Enhanced MRI of the Breast: Quantitative Method for Kinetic Curve Type Assessment. Am. J. Roentgenol. 2009, 193, W295–W300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moon, M.; Cornfeld, D.; Weinreb, J. Dynamic Contrast-Enhanced Breast MR Imaging. Magn. Reson. Imaging C 2009, 17, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Petrillo, A.; Fusco, R.; Petrillo, M.; Granata, V.; Bianco, F.; Marzo, M.D.; Delrio, P.; Tatangelo, F.; Botti, G.; Pecori, B.; et al. DCE-MRI Time–Intensity Curve Visual Inspection to Assess Pathological Response after Neoadjuvant Therapy in Locally Advanced Rectal Cancer. Jpn. J. Radiol. 2018, 36, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Hayes, C.; Padhani, A.R.; Leach, M.O. Assessing Changes in Tumour Vascular Function Using Dynamic Contrast-enhanced Magnetic Resonance Imaging. NMR Biomed. 2002, 15, 154–163. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.M.; Yu, D.; Zhang, H.L.; Dai, Y.; Bi, D.; Liu, Z.; Prince, M.R.; Li, C. 3D Dynamic Contrast-enhanced MRI of Rectal Carcinoma at 3T: Correlation with Microvascular Density and Vascular Endothelial Growth Factor Markers of Tumor Angiogenesis. J. Magn. Reson. Imaging 2008, 27, 1309–1316. [Google Scholar] [CrossRef]
- Intven, M.; Reerink, O.; Philippens, M.E.P. Dynamic Contrast Enhanced MR Imaging for Rectal Cancer Response Assessment after Neo-adjuvant Chemoradiation. J. Magn. Reson. Imaging 2015, 41, 1646–1653. [Google Scholar] [CrossRef]
- Alberda, W.J.; Dassen, H.P.N.; Dwarkasing, R.S.; Willemssen, F.E.J.A.; van der Pool, A.E.M.; de Wilt, J.H.W.; Burger, J.W.A.; Verhoef, C. Prediction of Tumor Stage and Lymph Node Involvement with Dynamic Contrast-Enhanced MRI after Chemoradiotherapy for Locally Advanced Rectal Cancer. Int. J. Color. Dis. 2012, 28, 573–580. [Google Scholar] [CrossRef]
- Mungai, F.; Verrone, G.B.; Bonasera, L.; Bicci, E.; Pietragalla, M.; Nardi, C.; Berti, V.; Mazzoni, L.N.; Miele, V. Imaging Biomarkers in the Diagnosis of Salivary Gland Tumors: The Value of Lesion/Parenchyma Ratio of Perfusion-MR Pharmacokinetic Parameters. Radiol. Med. 2021, 126, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Petrillo, A.; Fusco, R.; Petrillo, M.; Granata, V.; Sansone, M.; Avallone, A.; Delrio, P.; Pecori, B.; Tatangelo, F.; Ciliberto, G. Standardized Index of Shape (SIS): A Quantitative DCE-MRI Parameter to Discriminate Responders by Non-Responders after Neoadjuvant Therapy in LARC. Eur. Radiol. 2015, 25, 1935–1945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fusco, R.; Petrillo, A.; Petrillo, M.; Sansone, M. Use of Tracer Kinetic Models for Selection of Semi-Quantitative Features for DCE-MRI Data Classification. Appl. Magn. Reson. 2013, 44, 1311–1324. [Google Scholar] [CrossRef]
- Fusco, R.; Granata, V.; Sansone, M.; Rega, D.; Delrio, P.; Tatangelo, F.; Romano, C.; Avallone, A.; Pupo, D.; Giordano, M.; et al. Validation of the Standardized Index of Shape Tool to Analyze DCE-MRI Data in the Assessment of Neo-Adjuvant Therapy in Locally Advanced Rectal Cancer. Radiol. Med. 2021, 126, 1044–1054. [Google Scholar] [CrossRef]
- Armbruster, M.; D’Anastasi, M.; Holzner, V.; Kreis, M.E.; Dietrich, O.; Brandlhuber, B.; Graser, A.; Brandlhuber, M. Improved Detection of a Tumorous Involvement of the Mesorectal Fascia and Locoregional Lymph Nodes in Locally Advanced Rectal Cancer Using DCE-MRI. Int. J. Color. Dis. 2018, 33, 901–909. [Google Scholar] [CrossRef]
- Grøvik, E.; Redalen, K.R.; Storås, T.H.; Negård, A.; Holmedal, S.H.; Ree, A.H.; Meltzer, S.; Bjørnerud, A.; Gjesdal, K.-I. Dynamic Multi-Echo DCE- and DSC-MRI in Rectal Cancer: Low Primary Tumor K(Trans) and ΔR2* Peak Are Significantly Associated with Lymph Node Metastasis. J. Magn. Reson. Imaging 2016, 46, 194–206. [Google Scholar] [CrossRef] [Green Version]
- Yu, X.; Wen, L.; Hou, J.; Wang, H.; Lu, Q. Discrimination of Metastatic from Non-Metastatic Mesorectal Lymph Nodes in Rectal Cancer Using Quantitative Dynamic Contrast-Enhanced Magnetic Resonance Imaging. J. Huazhong Univ. Sci. Technol. Med. Sci. 2016, 36, 594–600. [Google Scholar] [CrossRef]
- Yoon, J.; Chung, Y.E.; Lim, J.S.; Kim, M.-J. Quantitative Assessment of Mesorectal Fat: New Prognostic Biomarker in Patients with Mid-to-Lower Rectal Cancer. Eur. Radiol. 2018, 29, 1240–1247. [Google Scholar] [CrossRef]
- Kluza, E.; Kleijnen, J.-P.J.E.; Martens, M.H.; Rennspiess, D.; Maas, M.; Jeukens, C.R.L.P.N.; Riedl, R.G.; Hausen, A.Z.; Beets, G.; Beets-Tan, R.G.H. Non-Invasive MR Assessment of Macroscopic and Microscopic Vascular Abnormalities in the Rectal Tumour-Surrounding Mesorectum. Eur. Radiol. 2015, 26, 1311–1319. [Google Scholar] [CrossRef]
- Yang, X.; Liu, Y.; Chen, Y.; Wen, Z.; Lin, B.; Quan, X.; Yu, S. Evaluation of Mesorectal Microcirculation with Quantitative Dynamic Contrast-Enhanced MRI. Am. J. Roentgenol. 2020, 215, 1370–1376. [Google Scholar] [CrossRef]
- Li, M.; Xu, X.; Xia, K.; Jiang, H.; Jiang, J.; Sun, J.; Lu, Z. Comparison of Diagnostic Performance between Perfusion-Related Intravoxel Incoherent Motion DWI and Dynamic Contrast-Enhanced MRI in Rectal Cancer. Comput. Math. Methods Med. 2021, 2021, 5095940. [Google Scholar] [CrossRef] [PubMed]
- Kim, H. Variability in Quantitative DCE-MRI: Sources and Solutions. J. Nat. Sci. 2018, 4, e484. [Google Scholar] [PubMed]
- Petrillo, A.; Fusco, R.; Petrillo, M.; Granata, V.; Delrio, P.; Bianco, F.; Pecori, B.; Botti, G.; Tatangelo, F.; Caracò, C.; et al. Standardized Index of Shape (DCE-MRI) and Standardized Uptake Value (PET/CT): Two Quantitative Approaches to Discriminate Chemo-Radiotherapy Locally Advanced Rectal Cancer Responders under a Functional Profile. Oncotarget 2016, 8, 8143–8153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, A.; Song, J.; Ma, Z.; Chen, T. Combined Dynamic Contrast-Enhanced Magnetic Resonance Imaging and Diffusion-Weighted Imaging to Predict Neoadjuvant Chemotherapy Effect in FIGO Stage IB2–IIA2 Cervical Cancers. Radiol. Med. 2020, 125, 1233–1242. [Google Scholar] [CrossRef] [PubMed]
- Taylor, F.G.M.; Swift, R.I.; Blomqvist, L.; Brown, G. A Systematic Approach to the Interpretation of Preoperative Staging MRI for Rectal Cancer. Am. J. Roentgenol. 2008, 191, 1827–1835. [Google Scholar] [CrossRef] [PubMed]
- Gollub, M.J.; Lakhman, Y.; McGinty, K.; Weiser, M.R.; Sohn, M.; Zheng, J.; Shia, J. Does Gadolinium-Based Contrast Material Improve Diagnostic Accuracy of Local Invasion in Rectal Cancer MRI? A Multireader Study. Am. J. Roentgenol. 2015, 204, W160–W167. [Google Scholar] [CrossRef] [Green Version]
- Maas, M.; Lambregts, D.M.J.; Lahaye, M.J.; Beets, G.L.; Backes, W.; Vliegen, R.F.A.; Jong, M.O.; Wildberger, J.E.; Beets-Tan, R.G.H. T-Staging of Rectal Cancer: Accuracy of 3.0 Tesla MRI Compared with 1.5 Tesla. Abdominal. Imaging 2011, 37, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Tsunoda, Y.; Ito, M.; Fujii, H.; Kuwano, H.; Saito, N. Preoperative Diagnosis of Lymph Node Metastases of Colorectal Cancer by FDG-PET/CT. Jpn. J. Clin. Oncol. 2008, 38, 347–353. [Google Scholar] [CrossRef] [Green Version]
- Tateishi, U.; Maeda, T.; Morimoto, T.; Miyake, M.; Arai, Y.; Kim, E.E. Non-Enhanced CT versus Contrast-Enhanced CT in Integrated PET/CT Studies for Nodal Staging of Rectal Cancer. Eur. J. Nucl. Med. Mol. I 2007, 34, 1627–1634. [Google Scholar] [CrossRef]
- Chang, C.; Sun, X.; Zhao, W.; Wang, R.; Qian, X.; Lei, B.; Wang, L.; Liu, L.; Ruan, M.; Xie, W.; et al. Minor Components of Micropapillary and Solid Subtypes in Lung Invasive Adenocarcinoma (≤ 3 Cm): PET/CT Findings and Correlations with Lymph Node Metastasis. Radiol. Med. 2020, 125, 257–264. [Google Scholar] [CrossRef]
- Husby, J.A.; Reitan, B.C.; Biermann, M.; Trovik, J.; Bjørge, L.; Magnussen, I.J.; Salvesen, Ø.O.; Salvesen, H.B.; Haldorsen, I.S. Metabolic Tumor Volume on 18F-FDG PET/CT Improves Preoperative Identification of High-Risk Endometrial Carcinoma Patients. J. Nucl. Med. 2015, 56, 1191–1198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.-J.; Chang, S. Volumetric Parameters Changes of Sequential 18F-FDG PET/CT for Early Prediction of Recurrence and Death in Patients with Locally Advanced Rectal Cancer Treated with Preoperative Chemoradiotherapy. Clin. Nucl. Med. 2015, 40, 930–935. [Google Scholar] [CrossRef] [PubMed]
- Marcus, C.; Wray, R.; Taghipour, M.; Marashdeh, W.; Ahn, S.J.; Mena, E.; Subramaniam, R.M. JOURNAL CLUB: Value of Quantitative FDG PET/CT Volumetric Biomarkers in Recurrent Colorectal Cancer Patient Survival. Am. J. Roentgenol. 2016, 207, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Jo, H.J.; Kim, S.-J.; Kim, I.J.; Kim, S. Predictive Value of Volumetric Parameters Measured by F-18 FDG PET/CT for Lymph Node Status in Patients with Surgically Resected Rectal Cancer. Ann. Nucl. Med. 2014, 28, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.H.; Kim, S.-J.; Kim, K.; Kim, H.; Kim, S.J.; Kim, W.J.; Jeon, Y.K.; Kim, S.S.; Kim, Y.K.; Kim, I.J. High Metabolic Tumor Volume and Total Lesion Glycolysis Are Associated with Lateral Lymph Node Metastasis in Patients with Incidentally Detected Thyroid Carcinoma. Ann. Nucl. Med. 2015, 29, 721–729. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.H.; Song, B.-I.; Kim, B.W.; Kim, H.W.; Won, K.S.; Bae, S.U.; Jeong, W.K.; Baek, S.K. Predictive Value of [18F]FDG PET/CT for Lymph Node Metastasis in Rectal Cancer. Sci. Rep. 2019, 9, 4979. [Google Scholar] [CrossRef]
- Lu, Y.-Y.; Chen, J.-H.; Ding, H.-J.; Chien, C.-R.; Lin, W.-Y.; Kao, C.-H. A Systematic Review and Meta-Analysis of Pretherapeutic Lymph Node Staging of Colorectal Cancer by 18F-FDG PET or PET/CT. Nucl. Med. Commun. 2012, 33, 1127–1133. [Google Scholar] [CrossRef]
- Raman, S.P.; Chen, Y.; Fishman, E.K. Evolution of Imaging in Rectal Cancer: Multimodality Imaging with MDCT, MRI, and PET. J. Gastrointest. Oncol. 2015, 6, 172–184. [Google Scholar] [CrossRef]
- Catalano, O.A.; Lee, S.I.; Parente, C.; Cauley, C.; Furtado, F.S.; Striar, R.; Soricelli, A.; Salvatore, M.; Li, Y.; Umutlu, L.; et al. Improving Staging of Rectal Cancer in the Pelvis: The Role of PET/MRI. Eur. J. Nucl. Med. Mol. I 2021, 48, 1235–1245. [Google Scholar] [CrossRef]
- Bailey, J.J.; Jordan, E.J.; Burke, C.; Ohliger, M.A.; Wang, Z.J.; Loon, K.V.; Varma, M.G.; Hope, T.A. Does Extended PET Acquisition in PET/MRI Rectal Cancer Staging Improve Results? Am. J. Roentgenol. 2018, 211, 896–900. [Google Scholar] [CrossRef]
- Hope, T.A.; Kassam, Z.; Loening, A.; McNamara, M.M.; Paspulati, R. The Use of PET/MRI for Imaging Rectal Cancer. Abdom. Radiol. 2019, 44, 3559–3568. [Google Scholar] [CrossRef] [PubMed]
- Crimì, F.; Spolverato, G.; Lacognata, C.; Garieri, M.; Cecchin, D.; Urso, E.D.; Zucchetta, P.; Pucciarelli, S.; Pomerri, F. 18F-FDG PET/MRI for Rectal Cancer TNM Restaging After Preoperative Chemoradiotherapy: Initial Experience. Dis. Colon. Rectum. 2020, 63, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Kang, B.; Lee, J.M.; Song, Y.S.; Woo, S.; Hur, B.Y.; Jeon, J.H.; Paeng, J.C. Added Value of Integrated Whole-Body PET/MRI for Evaluation of Colorectal Cancer: Comparison with Contrast-Enhanced MDCT. Am. J. Roentgenol. 2016, 206, W10–W20. [Google Scholar] [CrossRef] [PubMed]
- Gillies, R.J.; Kinahan, P.E.; Hricak, H. Radiomics: Images Are More than Pictures, They Are Data. Radiology 2016, 278, 563–577. [Google Scholar] [CrossRef] [Green Version]
- Scapicchio, C.; Gabelloni, M.; Barucci, A.; Cioni, D.; Saba, L.; Neri, E. A Deep Look into Radiomics. Radiol. Med. 2021, 126, 1296–1311. [Google Scholar] [CrossRef]
- Parekh, V.S.; Jacobs, M.A. Deep Learning and Radiomics in Precision Medicine. Expert Rev. Precis. Med. Drug Dev. 2019, 4, 59–72. [Google Scholar] [CrossRef] [Green Version]
- Nazari, M.; Shiri, I.; Hajianfar, G.; Oveisi, N.; Abdollahi, H.; Deevband, M.R.; Oveisi, M.; Zaidi, H. Noninvasive Fuhrman Grading of Clear Cell Renal Cell Carcinoma Using Computed Tomography Radiomic Features and Machine Learning. Radiol. Med. 2020, 125, 754–762. [Google Scholar] [CrossRef] [Green Version]
- Nardone, V.; Reginelli, A.; Grassi, R.; Boldrini, L.; Vacca, G.; D’Ippolito, E.; Annunziata, S.; Farchione, A.; Belfiore, M.P.; Desideri, I.; et al. Delta Radiomics: A Systematic Review. Radiol. Med. 2021, 126, 1571–1583. [Google Scholar] [CrossRef]
- Chianca, V.; Albano, D.; Messina, C.; Vincenzo, G.; Rizzo, S.; Grande, F.D.; Sconfienza, L.M. An Update in Musculoskeletal Tumors: From Quantitative Imaging to Radiomics. Radiol. Med. 2021, 126, 1095–1105. [Google Scholar] [CrossRef]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.T.H.M.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The Bridge between Medical Imaging and Personalized Medicine. Nat. Publ. Group 2017, 14, 749–762. [Google Scholar] [CrossRef]
- Liu, Z.; Wang, S.; Dong, D.; Wei, J.; Fang, C.; Zhou, X.; Sun, K.; Li, L.; Li, B.; Wang, M.; et al. The Applications of Radiomics in Precision Diagnosis and Treatment of Oncology: Opportunities and Challenges. Theranostics 2019, 9, 1303–1322. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, D.P.; Dietzel, M.; Baessler, B. A Decade of Radiomics Research: Are Images Really Data or Just Patterns in the Noise? Eur. Radiol. 2021, 31, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Kirienko, M.; Ninatti, G.; Cozzi, L.; Voulaz, E.; Gennaro, N.; Barajon, I.; Ricci, F.; Carlo-Stella, C.; Zucali, P.; Sollini, M.; et al. Computed Tomography (CT)-Derived Radiomic Features Differentiate Prevascular Mediastinum Masses as Thymic Neoplasms versus Lymphomas. Radiol. Med. 2020, 125, 951–960. [Google Scholar] [CrossRef] [PubMed]
- Karmazanovsky, G.; Gruzdev, I.; Tikhonova, V.; Kondratyev, E.; Revishvili, A. Computed Tomography-Based Radiomics Approach in Pancreatic Tumors Characterization. Radiol. Med. 2021, 126, 1388–1395. [Google Scholar] [CrossRef]
- Calabrese, A.; Santucci, D.; Landi, R.; Zobel, B.B.; Faiella, E.; de Felice, C. Radiomics MRI for Lymph Node Status Prediction in Breast Cancer Patients: The State of Art. J. Cancer Res. Clin. 2021, 147, 1587–1597. [Google Scholar] [CrossRef]
- Benedetti, G.; Mori, M.; Panzeri, M.M.; Barbera, M.; Palumbo, D.; Sini, C.; Muffatti, F.; Andreasi, V.; Steidler, S.; Doglioni, C.; et al. CT-Derived Radiomic Features to Discriminate Histologic Characteristics of Pancreatic Neuroendocrine Tumors. Radiol. Med. 2021, 126, 745–760. [Google Scholar] [CrossRef]
- Qin, H.; Que, Q.; Lin, P.; Li, X.; Wang, X.; He, Y.; Chen, J.; Yang, H. Magnetic Resonance Imaging (MRI) Radiomics of Papillary Thyroid Cancer (PTC): A Comparison of Predictive Performance of Multiple Classifiers Modeling to Identify Cervical Lymph Node Metastases before Surgery. Radiol. Med. 2021, 126, 1312–1327. [Google Scholar] [CrossRef]
- Agazzi, G.M.; Ravanelli, M.; Roca, E.; Medicina, D.; Balzarini, P.; Pessina, C.; Vermi, W.; Berruti, A.; Maroldi, R.; Farina, D. CT Texture Analysis for Prediction of EGFR Mutational Status and ALK Rearrangement in Patients with Non-Small Cell Lung Cancer. Radiol. Med. 2021, 126, 786–794. [Google Scholar] [CrossRef]
- Litvin, A.A.; Burkin, D.A.; Kropinov, A.A.; Paramzin, F.N. Radiomics and Digital Image Texture Analysis in Oncology (Review). Mod. Technol. Med. 2021, 13, 97–104. [Google Scholar] [CrossRef]
- Crimì, F.; Capelli, G.; Spolverato, G.; Bao, Q.R.; Florio, A.; Rossi, S.M.; Cecchin, D.; Albertoni, L.; Campi, C.; Pucciarelli, S.; et al. MRI T2-Weighted Sequences-Based Texture Analysis (TA) as a Predictor of Response to Neoadjuvant Chemo-Radiotherapy (NCRT) in Patients with Locally Advanced Rectal Cancer (LARC). Radiol. Med. 2020, 125, 1216–1224. [Google Scholar] [CrossRef]
- Horvat, N.; Bates, D.D.B.; Petkovska, I. Novel Imaging Techniques of Rectal Cancer: What Do Radiomics and Radiogenomics Have to Offer? A Literature Review. Abdom. Radiol. 2019, 44, 3764–3774. [Google Scholar] [CrossRef] [PubMed]
- Lubner, M.G.; Smith, A.D.; Sandrasegaran, K.; Sahani, D.V.; Pickhardt, P.J. CT Texture Analysis: Definitions, Applications, Biologic Correlates, and Challenges. RadioGraphics 2017, 37, 1483–1503. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.-N.; Ge, X.-L.; Liu, X.-S.; Xu, L.-L. Histogram Analysis of DCE-MRI for Chemoradiotherapy Response Evaluation in Locally Advanced Esophageal Squamous Cell Carcinoma. Radiol. Med. 2020, 125, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Lian, S.; Zhang, C.; Chi, J.; Huang, Y.; Shi, F.; Xie, C. Differentiation between Nasopharyngeal Carcinoma and Lymphoma at the Primary Site Using Whole-Tumor Histogram Analysis of Apparent Diffusion Coefficient Maps. Radiol. Med. 2020, 125, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Liu, Y.; Xu, L.; Li, Z.; Lv, H.; Dong, N.; Li, W.; Yang, Z.; Wang, Z.; Jin, E. Application of Texture Analysis Based on Apparent Diffusion Coefficient Maps in Discriminating Different Stages of Rectal Cancer. J. Magn. Reson. Imaging 2017, 45, 1798–1808. [Google Scholar] [CrossRef]
- Yang, L.; Liu, D.; Fang, X.; Wang, Z.; Xing, Y.; Ma, L.; Wu, B. Rectal Cancer: Can T2WI Histogram of the Primary Tumor Help Predict the Existence of Lymph Node Metastasis? Eur. Radiol. 2019, 29, 6469–6476. [Google Scholar] [CrossRef]
- Zhang, L.; Kang, L.; Li, G.; Zhang, X.; Ren, J.; Shi, Z.; Li, J.; Yu, S. Computed Tomography-Based Radiomics Model for Discriminating the Risk Stratification of Gastrointestinal Stromal Tumors. Radiol. Med. 2020, 125, 465–473. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhu, Y.; Zhang, K.; Liu, Y.; Cui, J.; Tao, J.; Wang, Y.; Wang, S. Invasive Ductal Breast Cancer: Preoperative Predict Ki-67 Index Based on Radiomics of ADC Maps. Radiol. Med. 2019, 125, 109–116. [Google Scholar] [CrossRef]
- Huang, Y.-Q.; Liang, C.-H.; He, L.; Tian, J.; Liang, C.-S.; Chen, X.; Ma, Z.-L.; Liu, Z.-Y. Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. J. Clin. Oncol. 2016, 34, 2157–2164. [Google Scholar] [CrossRef]
- Chen, L.-D.; Liang, J.-Y.; Wu, H.; Wang, Z.; Li, S.-R.; Li, W.; Zhang, X.-H.; Chen, J.-H.; Ye, J.-N.; Li, X.; et al. Multiparametric Radiomics Improve Prediction of Lymph Node Metastasis of Rectal Cancer Compared with Conventional Radiomics. Life Sci. 2018, 208, 55–63. [Google Scholar] [CrossRef]
- Ma, X.; Shen, F.; Jia, Y.; Xia, Y.; Li, Q.; Lu, J. MRI-Based Radiomics of Rectal Cancer: Preoperative Assessment of the Pathological Features. BMC Med. Imaging 2019, 19, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, J.-D.; Song, L.-R.; Lu, H.-C.; Zheng, X. Prediction of Different Stages of Rectal Cancer: Texture Analysis Based on Diffusion-Weighted Images and Apparent Diffusion Coefficient Maps. World J. Gastroenterol. 2020, 26, 2082–2096. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Zhang, X.; Li, X.; Shi, Y.; Zhu, H.; Sun, Y. Prediction of Pathological Nodal Stage of Locally Advanced Rectal Cancer by Collective Features of Multiple Lymph Nodes in Magnetic Resonance Images before and after Neoadjuvant Chemoradiotherapy. Chin. J. Cancer Res. 2019, 31, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhou, Y.; Wang, X.; Zhou, M.; Chen, X.; Luan, K. An MRI-Based Multi-Objective Radiomics Model Predicts Lymph Node Status in Patients with Rectal Cancer. Abdom. Radiol. 2020, 46, 1816–1824. [Google Scholar] [CrossRef]
- Zhou, X.; Yi, Y.; Liu, Z.; Zhou, Z.; Lai, B.; Sun, K.; Li, L.; Huang, L.; Feng, Y.; Cao, W.; et al. Radiomics-Based Preoperative Prediction of Lymph Node Status Following Neoadjuvant Therapy in Locally Advanced Rectal Cancer. Front. Oncol. 2020, 10, 604. [Google Scholar] [CrossRef]
- Orsatti, G.; Zucchetta, P.; Varotto, A.; Crimì, F.; Weber, M.; Cecchin, D.; Bisogno, G.; Spimpolo, A.; Giraudo, C.; Stramare, R. Volumetric Histograms-Based Analysis of Apparent Diffusion Coefficients and Standard Uptake Values for the Assessment of Pediatric Sarcoma at Staging: Preliminary Results of a PET/MRI Study. Radiol. Med. 2021, 126, 878–885. [Google Scholar] [CrossRef]
- Hu, H.; Shan, Q.; Chen, S.; Li, B.; Feng, S.; Xu, E.; Li, X.; Long, J.; Xie, X.; Lu, M.; et al. CT-Based Radiomics for Preoperative Prediction of Early Recurrent Hepatocellular Carcinoma: Technical Reproducibility of Acquisition and Scanners. Radiol. Med. 2020, 125, 697–705. [Google Scholar] [CrossRef]
- Traverso, A.; Wee, L.; Dekker, A.; Gillies, R. Repeatability and Reproducibility of Radiomic Features: A Systematic Review. Int. J. Radiat. Oncol. Biology Phys. 2018, 102, 1143–1158. [Google Scholar] [CrossRef] [Green Version]
- Horvat, N.; Veeraraghavan, H.; Khan, M.; Blazic, I.; Zheng, J.; Capanu, M.; Sala, E.; Garcia-Aguilar, J.; Gollub, M.J.; Petkovska, I. MR Imaging of Rectal Cancer: Radiomics Analysis to Assess Treatment Response after Neoadjuvant Therapy. Radiology 2018, 287, 833–843. [Google Scholar] [CrossRef] [Green Version]
- Cusumano, D.; Meijer, G.; Lenkowicz, J.; Chiloiro, G.; Boldrini, L.; Masciocchi, C.; Dinapoli, N.; Gatta, R.; Casà, C.; Damiani, A.; et al. A Field Strength Independent MR Radiomics Model to Predict Pathological Complete Response in Locally Advanced Rectal Cancer. Radiol. Med. 2021, 126, 421–429. [Google Scholar] [CrossRef]
- Gourtsoyianni, S.; Doumou, G.; Prezzi, D.; Taylor, B.; Stirling, J.J.; Taylor, N.J.; Siddique, M.; Cook, G.J.R.; Glynne-Jones, R.; Goh, V. Primary Rectal Cancer: Repeatability of Global and Local-Regional MR Imaging Texture Features. Radiology 2017, 284, 161375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badic, B.; Desseroit, M.C.; Hatt, M.; Visvikis, D. Potential Complementary Value of Noncontrast and Contrast Enhanced CT Radiomics in Colorectal Cancers. Acad. Radiol. 2019, 26, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Neri, E.; Coppola, F.; Miele, V.; Bibbolino, C.; Grassi, R. Artificial Intelligence: Who Is Responsible for the Diagnosis? Radiol. Med. 2020, 125, 517–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neri, E.; Miele, V.; Coppola, F.; Grassi, R. Use of CT and Artificial Intelligence in Suspected or COVID-19 Positive Patients: Statement of the Italian Society of Medical and Interventional Radiology. Radiol. Med. 2020, 125, 505–508. [Google Scholar] [CrossRef]
- Koh, D.-M.; Brown, G.; Temple, L.; Raja, A.; Toomey, P.; Bett, N.; Norman, A.R.; Husband, J.E. Rectal Cancer: Mesorectal Lymph Nodes at MR Imaging with USPIO versus Histopathologic Findings—Initial Observations. Radiology 2004, 231, 91–99. [Google Scholar] [CrossRef]
- Simon, G.H.; Bauer, J.; Saborovski, O.; Fu, Y.; Corot, C.; Wendland, M.F.; Daldrup-Link, H.E. T1 and T2 Relaxivity of Intracellular and Extracellular USPIO at 1.5T and 3T Clinical MR Scanning. Eur. Radiol. 2005, 16, 738–745. [Google Scholar] [CrossRef]
- Will, O.; Purkayastha, S.; Chan, C.; Athanasiou, T.; Darzi, A.W.; Gedroyc, W.; Tekkis, P.P. Diagnostic Precision of Nanoparticle-Enhanced MRI for Lymph-Node Metastases: A Meta-Analysis. Lancet Oncol. 2006, 7, 52–60. [Google Scholar] [CrossRef]
- Harisinghani, M.G.; Barentsz, J.; Hahn, P.F.; Deserno, W.M.; Tabatabaei, S.; Van De Kaa, C.H.; De La Rosette, J.; Weissleder, R. Noninvasive Detection of Clinically Occult Lymph-Node Metastases in Prostate Cancer. N. Engl. J. Med. 2003, 348, 2491–2499. [Google Scholar] [CrossRef] [Green Version]
- Stijns, R.C.; Philips, B.W.; Nagtegaal, I.D.; Polat, F.; de Wilt, J.H.; Wauters, C.A.; Zamecnik, P.; Fütterer, J.J.; Scheenen, T.W. USPIO-Enhanced MRI of Lymph Nodes in Rectal Cancer: A Node-to-Node Comparison with Histopathology. Eur. J. Radiol. 2021, 138, 109636. [Google Scholar] [CrossRef]
- Agostini, A.; Kircher, M.; Do, R.; Borgheresi, A.; Monti, S.; Giovagnoni, A.; Mannelli, L. MR Imaging of the Liver (Including Biliary Contrast Agents) Part 1_ Technical Considerations and Contrast Materials. Semin. Roentgenol. 2016, 51, 308–316. [Google Scholar] [CrossRef] [Green Version]
- Cicero, G.; Ascenti, G.; Albrecht, M.H.; Blandino, A.; Cavallaro, M.; D’Angelo, T.; Carerj, M.L.; Vogl, T.J.; Mazziotti, S. Extra-Abdominal Dual-Energy CT Applications: A Comprehensive Overview. Radiol. Med. 2020, 125, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Higaki, T.; Honda, Y.; Tatsugami, F.; Tani, C.; Fukumoto, W.; Narita, K.; Kondo, S.; Akagi, M.; Awai, K. Advanced CT Techniques for Assessing Hepatocellular Carcinoma. Radiol. Med. 2021, 126, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Petralia, G.; Zugni, F.; Summers, P.E.; Colombo, A.; Pricolo, P.; Grazioli, L.; Colagrande, S.; Giovagnoni, A.; Padhani, A.R.; Italian Working Group on Magnetic Resonance. Whole-body magnetic resonance imaging (WB-MRI) for cancer screening: Recommendations for use. Radiol. Med. 2021, 126, 1434–1450. [Google Scholar] [CrossRef]
- Foti, G.; Mantovani, W.; Faccioli, N.; Crivellari, G.; Romano, L.; Zorzi, C.; Carbognin, G. Identification of Bone Marrow Edema of the Knee: Diagnostic Accuracy of Dual-Energy CT in Comparison with MRI. Radiol. Med. 2021, 126, 405–413. [Google Scholar] [CrossRef]
- Agostini, A.; Floridi, C.; Borgheresi, A.; Badaloni, M.; Pirani, P.E.; Terilli, F.; Ottaviani, L.; Giovagnoni, A. Proposal of a Low-Dose, Long-Pitch, Dual-Source Chest CT Protocol on Third-Generation Dual-Source CT Using a Tin Filter for Spectral Shaping at 100 KVp for CoronaVirus Disease 2019 (COVID-19) Patients: A Feasibility Study. Radiol. Med. 2020, 125, 365–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bottari, A.; Silipigni, S.; Carerj, M.L.; Cattafi, A.; Maimone, S.; Marino, M.A.; Mazziotti, S.; Pitrone, A.; Squadrito, G.; Ascenti, G. Dual-Source Dual-Energy CT in the Evaluation of Hepatic Fractional Extracellular Space in Cirrhosis. Radiol. Med. 2020, 125, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Yan, F.; Pan, Z.; Lin, X.; Luo, X.; Shi, C.; Chen, X.; Wang, B.; Zhang, H. Evaluation of Dual Energy Spectral CT in Differentiating Metastatic from Non-Metastatic Lymph Nodes in Rectal Cancer: Initial Experience. Eur. J. Radiol. 2015, 84, 228–234. [Google Scholar] [CrossRef]
- Sato, K.; Morohashi, H.; Tsushima, F.; Sakamoto, Y.; Miura, T.; Fujita, H.; Umemura, K.; Suzuki, T.; Tsuruta, S.; Kura, R.; et al. Dual Energy CT Is Useful for the Prediction of Mesenteric and Lateral Pelvic Lymph Node Metastasis in Rectal Cancer. Mol. Clin. Oncol. 2019, 10, 625–630. [Google Scholar] [CrossRef]
- Al-Najami, I.; Lahaye, M.J.; Beets-Tan, R.G.H.; Baatrup, G. Dual-Energy CT Can Detect Malignant Lymph Nodes in Rectal Cancer. Eur. J. Radiol. 2017, 90, 81–88. [Google Scholar] [CrossRef]
- Compagnone, G.; Padovani, R.; D’Ercole, L.; Orlacchio, A.; Bernardi, G.; D’Avanzo, M.A.; Grande, S.; Palma, A.; Campanella, F.; Rosi, A. Provision of Italian Diagnostic Reference Levels for Diagnostic and Interventional Radiology. Radiol. Med. 2021, 126, 99–105. [Google Scholar] [CrossRef]
- Granata, V.; Faggioni, L.; Grassi, R.; Fusco, R.; Reginelli, A.; Rega, D.; Maggialetti, N.; Buccicardi, D.; Frittoli, B.; Rengo, M.; et al. Structured Reporting of Computed Tomography in the Staging of Colon Cancer: A Delphi Consensus Proposal. Radiol. Med. 2022, 127, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, C.; Roberta, F.; Angela, D.L.; Cesare, P.; Alfredo, C.; Giuliano, G.; Giulio, L.; Giuliana, G.; Maria, R.G.; Paola, B.M.; et al. Clinical and Laboratory Data, Radiological Structured Report Findings and Quantitative Evaluation of Lung Involvement on Baseline Chest CT in COVID-19 Patients to Predict Prognosis. Radiol. Med. 2021, 126, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Alvfeldt, G.; Aspelin, P.; Blomqvist, L.; Sellberg, N. Rectal Cancer Staging Using MRI: Adherence in Reporting to Evidence-Based Practice. Acta Radiol. 2020, 61, 1463–1472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krdzalic, J.; Maas, M.; Gollub, M.J.; Beets-Tan, R.G.H. Guidelines for MR Imaging in Rectal Cancer: Europe versus United States. Abdom. Radiol. 2019, 44, 3498–3507. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Grassi, R.; Fusco, R.; Izzo, F.; Brunese, L.; Delrio, P.; Avallone, A.; Pecori, B.; Petrillo, A. Current Status on Response to Treatment in Locally Advanced Rectal Cancer: What the Radiologist Should Know. Eur. Rev. Med. Pharmacol. 2020, 24, 12050–12062. [Google Scholar] [CrossRef]
- Agarwal, M.; van der Pol, C.B.; Patlas, M.N.; Udare, A.; Chung, A.D.; Rubino, J. Optimizing the Radiologist Work Environment: Actionable Tips to Improve Workplace Satisfaction, Efficiency, and Minimize Burnout. Radiol. Med. 2021, 126, 1255–1257. [Google Scholar] [CrossRef]
- Weiss, D.L.; Langlotz, C.P. Structured Reporting: Patient Care Enhancement or Productivity Nightmare? Radiology 2008, 249, 739–747. [Google Scholar] [CrossRef]






| Compartments | Boundaries and Considerations | TNM | ||||
|---|---|---|---|---|---|---|
| Mesenteric | Pararectal/mesorectal LN | Within the mesorectum | The most common pathway of nodal spread (mostly tumors above the PR) | N | ||
| Superior rectal LN | At the level of the superior rectal A | N | ||||
| IMA LN | Between the origin of the left colic artery and immediately below the origin of the IMA | N | ||||
| Principal IMA LN | Origin of the IMA | N | ||||
| Extra mesenteric | Pelvic sidewall LN | Internal iliac/hypogastric LN | Along the hypogastric A | Frequently involved if the tumor is at or/and below the PR (NB outside of the CRM) | N | |
| External iliac LN | Lateral chain | Lateral to the external iliac A it continues in the lateral chain of the common iliac LN | Rarely involved; could be involved if the tumors are at and below the PR or exceptionally in tumor extending below the dentate line (through superficial inguinal LN) | M | ||
| Middle chain | Between the external iliac A and V | M | ||||
| Medial chain | Posterior to the external iliac V | Could be involved if the tumors are at and below the PR Frequently indistinguishable from obturator LN (i.e., along the obturator A), which are frequently involved as well | M | |||
| Common iliac LN | Lateral chain | A continuation of the lateral chain of the external iliac LN | Could be involved if the tumors are at and below the PR | M | ||
| Medial chain | Between the common iliac A at the sacral promontory | M | ||||
| Middle chain | A continuation of the hypogastric/internal iliac region and the lateral sacral region. Sited posteriorly to the common iliac A and V, abutting the L5 nerve root as it passes anterior to the sacral alae | M | ||||
| Retroperitoneal LN | Left para-aortic | To the left of Aorta | M | |||
| Right latero-aortic | Aortocaval, precaval, laterocaval, and retrocaval | M | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borgheresi, A.; De Muzio, F.; Agostini, A.; Ottaviani, L.; Bruno, A.; Granata, V.; Fusco, R.; Danti, G.; Flammia, F.; Grassi, R.; et al. Lymph Nodes Evaluation in Rectal Cancer: Where Do We Stand and Future Perspective. J. Clin. Med. 2022, 11, 2599. https://doi.org/10.3390/jcm11092599
Borgheresi A, De Muzio F, Agostini A, Ottaviani L, Bruno A, Granata V, Fusco R, Danti G, Flammia F, Grassi R, et al. Lymph Nodes Evaluation in Rectal Cancer: Where Do We Stand and Future Perspective. Journal of Clinical Medicine. 2022; 11(9):2599. https://doi.org/10.3390/jcm11092599
Chicago/Turabian StyleBorgheresi, Alessandra, Federica De Muzio, Andrea Agostini, Letizia Ottaviani, Alessandra Bruno, Vincenza Granata, Roberta Fusco, Ginevra Danti, Federica Flammia, Roberta Grassi, and et al. 2022. "Lymph Nodes Evaluation in Rectal Cancer: Where Do We Stand and Future Perspective" Journal of Clinical Medicine 11, no. 9: 2599. https://doi.org/10.3390/jcm11092599
APA StyleBorgheresi, A., De Muzio, F., Agostini, A., Ottaviani, L., Bruno, A., Granata, V., Fusco, R., Danti, G., Flammia, F., Grassi, R., Grassi, F., Bruno, F., Palumbo, P., Barile, A., Miele, V., & Giovagnoni, A. (2022). Lymph Nodes Evaluation in Rectal Cancer: Where Do We Stand and Future Perspective. Journal of Clinical Medicine, 11(9), 2599. https://doi.org/10.3390/jcm11092599








