A Modified Approach for Ultrasound-Guided Thoracic Paravertebral Block via Thoracic Intervertebral Foramen in an Adolescent Patient: A Case Report
Abstract
:1. Introduction
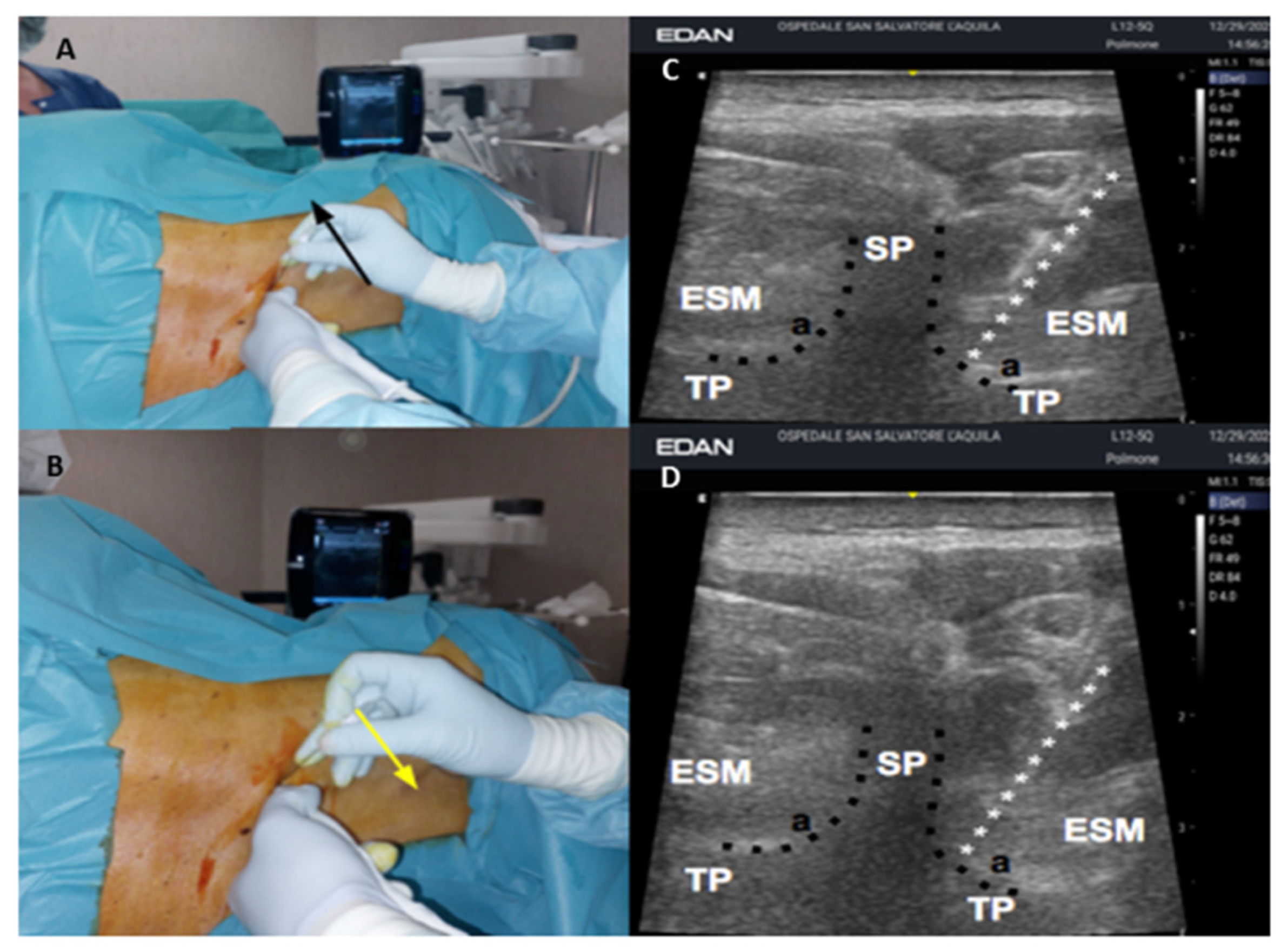
2. Case Presentation
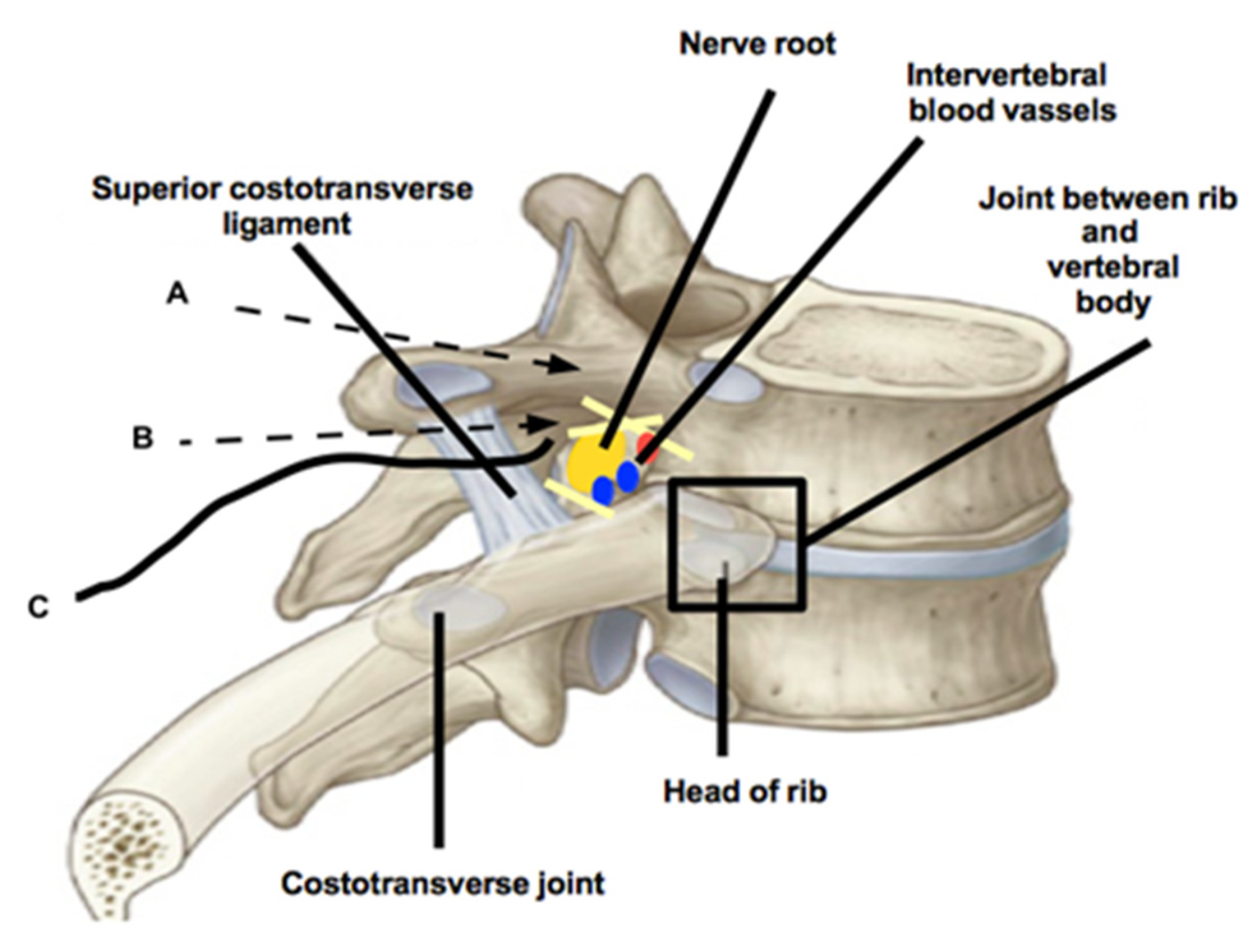
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andreae, M.H.; Andreae, D.A. Regional anaesthesia to prevent chronic pain after surgery: A cochrane systematic review and meta-analysis. Br. J. Anaesth. 2013, 111, 711–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cuomo, A.; Bimonte, S.; Forte, C.A.; Botti, G.; Cascella, M. Multimodal approaches and tailored therapies for pain management: The trolley analgesic model. J. Pain Res. 2019, 12, 711–714. [Google Scholar] [CrossRef] [PubMed]
- Chia, P.A.; Cannesson, M.; Bui, C.C.M. Opioid free anesthesia: Feasible? Curr. Opin. Anaesthesiol. 2020, 33, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Chitnis, S.S.; Tang, R.; Mariano, E.R. The role of regional analgesia in personalized postoperative pain management. Korean J. Anesthesiol. 2020, 73, 363–371. [Google Scholar] [CrossRef]
- Kehlet, H.; Rung, G.W.; Callesen, T. Postoperative opioid analgesia: Time for a reconsideration? J. Clin. Anesth. 1996, 8, 441–445. [Google Scholar] [CrossRef]
- Krediet, A.C.; Moayeri, N.; van Geffen, G.-J.; Bruhn, J.; Renes, S.; Bigeleisen, P.E.; Groen, G.J. Different approaches to ultrasound-guided thoracic paravertebral block: An illustrated review. Anesthesiology 2015, 123, 459–474. [Google Scholar] [CrossRef] [Green Version]
- Petrucci, E.; Vittori, A.; Cascella, M.; Vergallo, A.; Fiore, G.; Luciani, A.; Pizzi, B.; Degan, G.; Fineschi, V.; Marinangeli, F. Litigation in anesthesia and intensive care units: An Italian retrospective study. Healthcare 2021, 9, 1012. [Google Scholar] [CrossRef]
- Madafferi, S.; Accinni, A.; Martucci, C.; Voglino, V.; Frediani, S.; Picardo, S.; Inserra, A. Paraplegia after thoracotomy: A single center experience with pediatric patients and a review of the literature. Ann. Ital. Chir. 2022, 92, 27–32. [Google Scholar]
- Boscolo-Berto, R.; Tortorella, C.; Porzionato, A.; Stecco, C.; Picardi, E.E.E.; Macchi, V.; De Caro, R. The additional role of virtual to traditional dissection in teaching anatomy: A randomised controlled trial. Surg. Radiol. Anat. 2021, 43, 469–479. [Google Scholar] [CrossRef]
- Lin, J.-A.; Blanco, R.; Shibata, Y.; Nakamoto, T.; Lin, K.-H. Corrigendum to “advances of techniques in deep regional blocks”. Biomed. Res. Int. 2018, 2018, 5151645. [Google Scholar] [CrossRef]
- Tsui, B.C.H.; Li, L.X.Y.; Pillay, J.J. Compressed air injection technique to standardize block injection pressures. Can. J. Anaesth. 2006, 53, 1098–1102. [Google Scholar] [CrossRef]
- Standards for Basic Anesthetic Monitoring. Available online: https://www.asahq.org/standards-and-guidelines/standards-for-basic-anesthetic-monitoring (accessed on 2 April 2022).
- Aldrete, J.A. The post-anesthesia recovery score revisited. J. Clin. Anesth. 1995, 7, 89–91. [Google Scholar] [CrossRef]
- Wolfler, A.M.; De Silvestri, A.; Camporesi, A.; Ivani, G.; Vittori, A.; Zadra, N.; Pasini, L.; Astuto, M.; Locatelli, B.G.; Cortegiani, A.; et al. Pediatric anesthesia practice in Italy: A multicenter national prospective observational study derived from the apricot trial. Minerva Anestesiol. 2020, 86, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Holland, E.L.; Bosenberg, A.T. Early experience with erector spinae plane blocks in children. Paediatr. Anaesth. 2020, 30, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.V.; Moriggl, B.; Hoermann, R.; Nielsen, T.D.; Bendtsen, T.F.; Børglum, J. Are single-injection erector spinae plane block and multiple-injection costotransverse block equivalent to thoracic paravertebral block? Acta Anaesthesiol. Scand. 2019, 63, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Bouman, E.A.C.; Sieben, J.M.; Balthasar, A.J.R.; Joosten, E.A.; Gramke, H.-F.; van Kleef, M.; Lataster, A. Boundaries of the thoracic paravertebral space: Potential risks and benefits of the thoracic paravertebral block from an anatomical perspective. Surg. Radiol. Anat. 2017, 39, 1117–1125. [Google Scholar] [CrossRef] [Green Version]
- Gkasdaris, G.; Tripsianis, G.; Kotopoulos, K.; Kapetanakis, S. Clinical anatomy and significance of the thoracic intervertebral foramen: A cadaveric study and review of the literature. J. Craniovertebral Junction Spine 2016, 7, 228–235. [Google Scholar] [CrossRef]
- Bozkurt, M.; Canbay, S.; Neves, G.F.; Aktüre, E.; Fidan, E.; Salamat, M.S.; Başkaya, M.K. Microsurgical anatomy of the dorsal thoracic rootlets and dorsal root entry zones. Acta Neurochir. 2012, 154, 1235–1239. [Google Scholar] [CrossRef]
- Cui, X.; Cai, J.; Sun, J.; Jiang, Z. Morphology study of thoracic transverse processes and its significance in pedicle-rib unit screw fixation. J. Spinal Disord. Tech. 2015, 28, E74–E77. [Google Scholar] [CrossRef]
- Chen, F.; Liu, X.; Wang, G.; Sun, J.; Cui, X. Anatomic relationship of bony structures in pedicle-rib unit and its significance. World Neurosurg. 2020, 139, e691–e699. [Google Scholar] [CrossRef]
- Shibata, Y.; Kampitak, W.; Tansatit, T. The novel costotransverse foramen block technique: Distribution characteristics of injectate compared with erector spinae plane block. Pain Physician 2020, 23, E305–E314. [Google Scholar] [PubMed]
- Cowie, B.; McGlade, D.; Ivanusic, J.; Barrington, M.J. Ultrasound-guided thoracic paravertebral blockade: A cadaveric study. Anesth. Analg. 2010, 110, 1735–1739. [Google Scholar] [CrossRef] [PubMed]
- Vallières, E. The costovertebral angle. Thorac. Surg. Clin. 2007, 17, 503–510. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrucci, E.; Marinangeli, F.; Pizzi, B.; Sciorio, F.; Marrocco, G.; Innamorato, M.A.; Cascella, M.; Vittori, A. A Modified Approach for Ultrasound-Guided Thoracic Paravertebral Block via Thoracic Intervertebral Foramen in an Adolescent Patient: A Case Report. J. Clin. Med. 2022, 11, 2646. https://doi.org/10.3390/jcm11092646
Petrucci E, Marinangeli F, Pizzi B, Sciorio F, Marrocco G, Innamorato MA, Cascella M, Vittori A. A Modified Approach for Ultrasound-Guided Thoracic Paravertebral Block via Thoracic Intervertebral Foramen in an Adolescent Patient: A Case Report. Journal of Clinical Medicine. 2022; 11(9):2646. https://doi.org/10.3390/jcm11092646
Chicago/Turabian StylePetrucci, Emiliano, Franco Marinangeli, Barbara Pizzi, Francesco Sciorio, Gioele Marrocco, Massimo Antonio Innamorato, Marco Cascella, and Alessandro Vittori. 2022. "A Modified Approach for Ultrasound-Guided Thoracic Paravertebral Block via Thoracic Intervertebral Foramen in an Adolescent Patient: A Case Report" Journal of Clinical Medicine 11, no. 9: 2646. https://doi.org/10.3390/jcm11092646
APA StylePetrucci, E., Marinangeli, F., Pizzi, B., Sciorio, F., Marrocco, G., Innamorato, M. A., Cascella, M., & Vittori, A. (2022). A Modified Approach for Ultrasound-Guided Thoracic Paravertebral Block via Thoracic Intervertebral Foramen in an Adolescent Patient: A Case Report. Journal of Clinical Medicine, 11(9), 2646. https://doi.org/10.3390/jcm11092646








