Complete Uterine Septum, Double Cervix and Vaginal Septum (U2b C2 V1): Hysteroscopic Management and Fertility Outcomes—A Systematic Review
Abstract
:1. Introduction
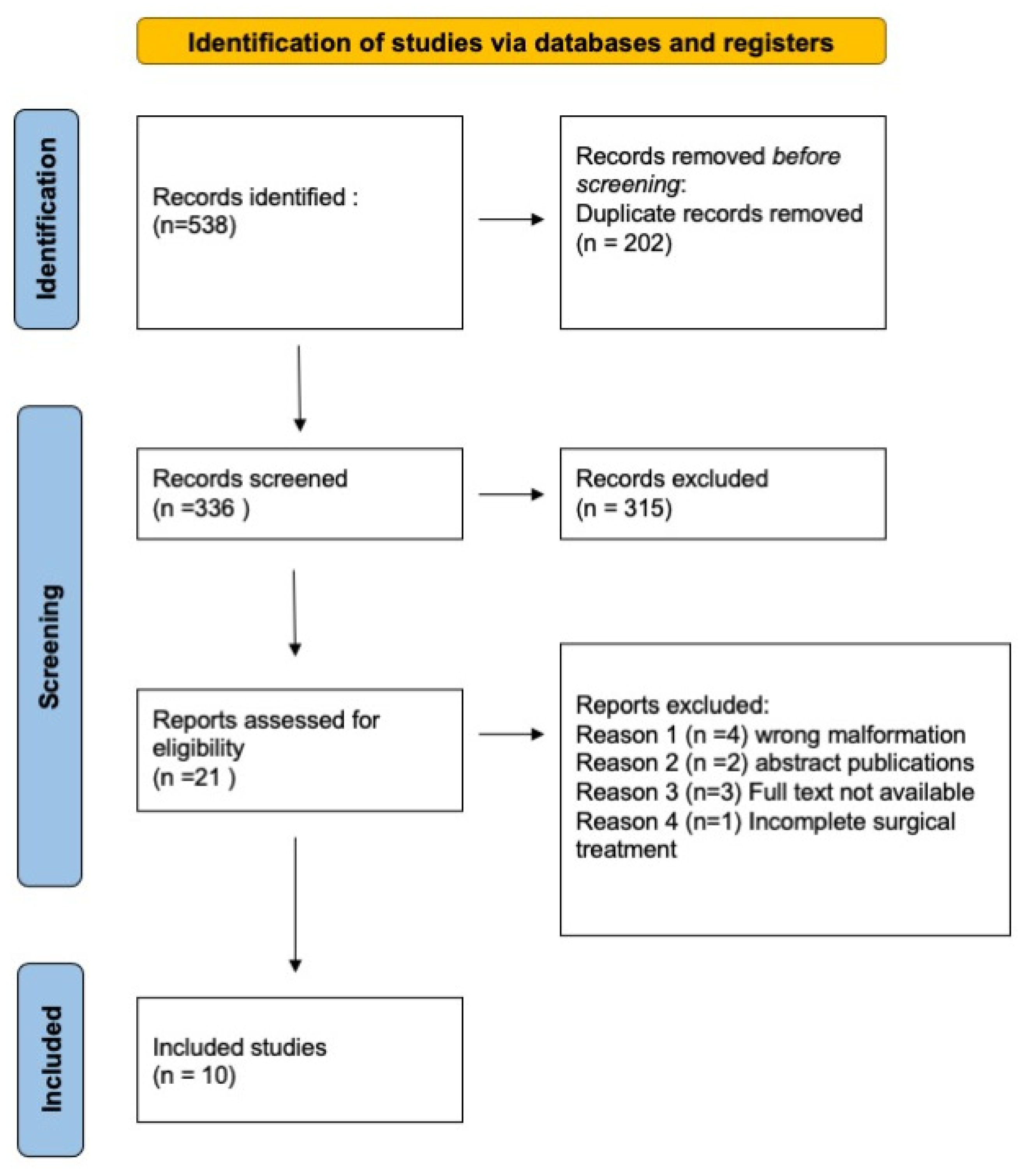
2. Materials and Methods
2.1. Literature Research
2.2. Quality Assessment
3. Results
3.1. Diagnosis and Classification
3.2. Surgical Technique
3.3. Fertility Outcomes
4. Discussion
4.1. Strengths
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grimbizis, G.F.; Gordts, S.; Di Spiezio Sardo, A.; Brucker, S.; De Angelis, C.; Gergolet, M.; Li, T.C.; Tanos, V.; Brölmann, H.; Gianaroli, L.; et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum. Reprod. 2013, 28, 2032–2044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McBean, J.H.; Brumsted, J.R. Septate uterus with cervical duplication: A rare malformation. Fertil. Steril. 1994, 62, 415–417. [Google Scholar] [CrossRef] [PubMed]
- Grimbizis, G.F.; Camus, M.; Tarlatzis, B.C.; Bontis, J.N.; Devroey, P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum. Reprod. Update 2001, 7, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.Y.; Jayaprakasan, K.; Tan, A.; Thornton, J.G.; Coomarasamy, A.; Raine-Fenning, N.J. Reproductive outcomes in women with congenital uterine anomalies: A systematic review. Ultrasound. Obstet. Gynecol. 2011, 38, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Candiani, G.B.; Fedele, L.; Zamberletti, D.; De Virgiliis, D.; Carinelli, S. Endometrial patterns in malformed uteri. Acta. Eur. Fertil. 1983, 14, 311–318. Available online: http://europepmcorg/abstract/MED/6673450 (accessed on 1 December 2022).
- Sardo, A.D.S.; Zizolfi, B.; Bettocchi, S.; Exacoustos, C.; Nocera, C.; Nazzaro, G.; Vieira, M.D.C.; Nappi, C. Accuracy of Hysteroscopic Metroplasty With the Combination of Presurgical 3-Dimensional Ultrasonography and a Novel Graduated Intrauterine Palpator: A Randomized Controlled Trial. J. Minim. Invasive Gynecol. 2016, 23, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Ludwin, A.; Martins, W.P.; Nastri, C.O.; Ludwin, I.; Coelho Neto, M.A.; Leitão, V.M.; Acién, M.; Alcazar, J.L.; Benacerraf, B.; Condous, G.; et al. Congenital Uterine Malformation by Experts (CUME): Better criteria for distinguishing between normal/arcuate and septate uterus? Ultrasound Obs. Gynecol. 2018, 51, 101–109. [Google Scholar] [CrossRef]
- The National Institute for Health and Care Excellence. In Fertility Problems: Assessment and Treatment; NICE: London, UK, 2017.
- Penzias, A.; Bendikson, K.; Falcone, T.; Hansen, K.; Hill, M.; Jindal, S.; Mersereau, J.; Racowsky, C.; Rebar, R.; Steiner, A.Z.; et al. Evidence-based treatments for couples with unexplained infertility: A guideline. Fertil. Steril. 2020, 113, 305–322. [Google Scholar] [CrossRef]
- National Collaborating Centre for Women’s and Children’s Health (UK). Fertility: Assessment and Treatment for People with Fertility Problems; RCOG Press: London, UK, 2004. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 1–11. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [Green Version]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan–A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Godfrey, C.; Holly, C.; Kahlil, H.; Tungpunkom, P. Checklist for Systematic Reviews and Research Syntheses; Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Phillip E Patton, Miles J Novy, David M Lee, Lee R Hickok, The diagnosis and reproductive outcome after surgical treatment of the complete septate uterus, duplicated cervix and vaginal septum. Am. J. Obstetr. Gynecol. 2004, 190, 1669–1675. [CrossRef] [PubMed]
- Ignatov, A.; Costa, S.D.; Kleinstein, J. Reproductive Outcome of Women with Rare Müllerian Anomaly: Report of 2 Cases. J. Minim. Invasive Gynecol. 2008, 15, 502–504. [Google Scholar] [CrossRef] [PubMed]
- Caliskan, E.; Cakiroglu, Y.; Turkoz, E.; Corakci, A. Leiomyoma on the septum of a septate uterus with double cervix and vaginal septum: A challenge to manage. Fertil. Steril. 2008, 89, e3–e456. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.H.; Xu, K.H.; Lin, J.; Chen, X.Z. Hysteroscopic septum resection of complete septate uterus with cervical duplication, sparing the double cervix in patients with recurrent spontaneous abortions or infertility. Fertil. Steril. 2009, 91, 2643–2649. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.; Zhu, X.; Xu, H.; Liang, Z.; Zhang, X. Reproductive outcome following resectoscope metroplasty in women having a complete uterine septum with double cervix and vagina. Int. J. Gynecol. Obstet. 2009, 105, 25–28. [Google Scholar] [CrossRef]
- Celik, N.Y.; Mulayim, B. A mullerian anomaly ‘without classification’: Septate uterus with double cervix and longitudinal vaginal septum. Taiwan J. Obstet. Gynecol. 2012, 51, 649–650. [Google Scholar] [CrossRef] [Green Version]
- Seet, M.J.; Lau, M.S.K.; Chan, J.K.Y.; Tan, H.H. Management of complete vagino-uterine septum in patients seeking fertility: Report of two cases and review of literature. Gynecol. Minim. Invasive Ther. 2015, 4, 140–145. [Google Scholar] [CrossRef] [Green Version]
- Tajiri, R.; Ueda, T.; Aoyama, Y.; Sakuragi, T.; Tohyama, A.; Okabe, K.; Hitomi Nakagawa, Y.K.; Hachisuga, T. Pregnancy After Hysteroscopic Metroplasty Under Laparoscopy in a Woman with Complete Septate Uterus: A Case Report. J. Univ. Occup. Enviromental Heal. 2015, 1, 17–22. [Google Scholar]
- Gezer, Ş.; Vural, B. Double cervix, septate uterus, and longitudinal vaginal septum: A rare Müllerian anomaly with leiomyoma of the uterus. Clin. Exp. Obstet. Gynecol. 2019, 46, 648–650. [Google Scholar] [CrossRef]
- SEljEflot, E.B.; NytuN, Ø.E.; Kjøtrød, S.B.; GErGolEt, M. A septate uterus with double cervix during two pregnancies: Pregnancy outcome before and after cervix sparing metroplasty. A case report. Fact Views Vis. ObGyn. 2020, 12, 149–152. [Google Scholar]
- Rikken, J.F.W.; Kowalik, C.R.; Emanuel, M.H.; Bongers, M.Y.; Spinder, T.; Jansen, F.W.; Mulders, A.G.M.G.J.; Padmehr, R.; Clark, T.J.; A van Vliet, H.; et al. Septum resection versus expectant management in women with a septate uterus: An international multicentre open-label randomized controlled trial. Hum. Reprod. 2021, 36, 1260–1267. [Google Scholar] [CrossRef] [PubMed]
- Campo, R.; Santangelo, F.; Gordts, S.; Di Cesare, C.; Van Kerrebroeck, H.; De Angelis, M.C.; Di Spiezio Sardo, A. Outpatient hysteroscopy. Facts Views Vis. Obgyn. 2018, 10, 115–122. [Google Scholar] [PubMed]
- Tonguc, E.A.; Var, T.; Batioglu, S. Hysteroscopic metroplasty in patients with a uterine septum and otherwise unexplained infertility. Int. J. Gynecol. Obstet. 2011, 113, 128–130. [Google Scholar] [CrossRef] [PubMed]
- Mollo, A.; De Franciscis, P.; Colacurci, N.; Cobellis, L.; Perino, A.; Venezia, R.; Alviggi, C.; De Placido, G. Hysteroscopic resection of the septum improves the pregnancy rate of women with unexplained infertility: A prospective controlled trial. Fertil. Steril. 2009, 91, 2628–2631. [Google Scholar] [CrossRef] [PubMed]
- Carugno, J.; Grimbizis, G.; Franchini, M.; Alonso, L.; Bradley, L.; Campo, R.; Catena, U.; Carlo, D.A.; Attilio, D.S.S.; Martin, F.; et al. International Consensus Statement for Recommended Terminology Describing Hysteroscopic Procedures. J. Minim. Invasive Gynecol. 2022, 29, 385–391. [Google Scholar] [CrossRef]
- Carugno, J.; Grimbizis, G.; Franchini, M.; Alonso, L.; Bradley, L.; Campo, R.; Catena, U.; De Angelis, C.; Di Spiezio Sardo, A.; Farrugia, M.; et al. International Consensus Statement for recommended terminology describing hysteroscopic procedures. Facts Views Vis Obgyn. 2021, 13, 287–294. [Google Scholar] [CrossRef]
- Nouri, K.; Ott, J.; Huber, J.C.; Fischer, E.M.; Stögbauer, L.; Tempfer, C.B. Reproductive outcome after hysteroscopic septoplasty in patients with septate uterus–A retrospective cohort study and systematic review of the literature. Reprod. Biol. Endocrinol. 2010, 8, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Di Spiezio Sardo, A.; Manzi, A.; Zizolfi, B.; Giampaolino, P.; Carugno, J.; Grimbizis, G. The step-by-step hysteroscopic treatment of patients with vaginal and complete uterine septum with double cervix (U2bC2V1). Fertil. Steril. 2021, 116, 602–604. [Google Scholar] [CrossRef]

| Title | Author, year | Country | Study Design | Symptoms | Population Size | Method of Diagnosis | Type of Surgery | Primary Outcome | Secondary Outcome | IVF | Outcomes (Follow-Up) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| The diagnosis and reproductive outcome after surgical treatment of the complete septate uterus, duplicated cervix and vaginal septum. | Patton et al. 2004 [15] | U.S.A. | Retrospective case series | Dyspareunia, recurrent pregnancy lost | 16 | TVUS, HSG, MRI | Excision of longitudinal vaginal septum. Hysteroscopic resection with operative hysteroscope and loop electrode of the uterine septum. Guidance technique: Foley balloon/ curved plastic Pratt dilator or Tompkins metroplasty (=transabdominal metroplasty). | To evaluate the reproductive outcome after metroplasty | To evaluate the best technique of metroplasty | 1 patient delivered after egg donation procedures. 15 patients: not specified | 12 women conceived. 17 pregnancies (14 live births or ongoing third trimester pregnancies) after hysteroscopic resection (9/12) or abdominal metroplasty (5/5); 3/17 first trimester abortions; 0/17 late abortion; 13/14 term births; 1/14 ongoing pregnancy; 0/14 preterm deliveries |
| Reproductive outcome of women with rare Müllerian anomaly: report of 2 cases. | Ignatov et al. 2008 [16] | Germany | Case report | Primary infertility Secondary infertiity | 2 | TVUS, Hysteroscopy | Vaginal septum resection with Metzenbaum scissors + cervical dilatation to Hegar 10 + incision of the uterine septum hysteroscopically with a loop electrod Guidance technique: Hegars dilators | Whether metroplasty increases pregnancy rate (time between procedure and conception) | Obstetric outcomes (preterm birth; vaginal delivery, CS etc.) | No | Spontaneous conception. 2 Vaginal deliveries: 38 and 35 weeks |
| Leiomyoma on the septum of a septate uterus with double cervix and vaginal septum: a challenge to manage | Caliskan et al. 2008 [17] | Turkey | Case report | Primary infertility, menorrhagia, dyspareunia | 1 | TVUS, HSG, MRI, Hysteroscopy | Two step surgical process: 1. Laparotomic myomectomy + excision of vaginal septum 2. Hysteroscopic metroplasty with loop electrode + resection of the tissue between the two cervixes with Metzenbaum scissors Guidance technique: pediatric Foley catheter into the new single uterine cavity inflated with 50 mL of saline solution. Antibiotic prophylaxis: Cefazolin for 5 days. | Whether metroplasty increases pregnancy rate (time between procedure and conception) | Excision of subserosal leiomyoma of the uterine septum | yes | Pregnant at 26 weeks |
| Hysteroscopic septum resection of complete septate uterus with cervical duplication, sparing the double cervix in patients with recurrent spontaneous abortions or infertility. | Wang et al. 2009 [18] | China | Prospective observational | Infertility, recurrent miscarriage | 25 | TVUS 3D-TVUS | Hysteroscopic septum resection using a 27-Fr hysteroresectoscope with a specific cutting knife electrode or cutting wire loop electrode Guidance technique: bougie as orientation and blockage of internal cervical and laparoscopic control | To evaluate intraoperative and post-operarative complications of hysteroscopic septum resection using Hank bougies (graduated metal dilators) technique | To evaluate the safety and efficacy of hysteroscopic septum resection in patients with recurrent abortions or infertility | Yes (1 pregnancy) No (14 pregnancies) | Total pregnancies. 15 Term deliveries:5; Ongoing pregnancies: 7 Abortions: 2 Preterm deliveries: 1 |
| Reproductive outcome following resectoscope metroplasty in women having a complete uterine septum with double cervix and vagina. | Lin et al. 2009 [19] | China | Retrospective case-control with a concurrent control group of untreated patients | Dysmenorrhea, dyspareunia. 16 women with primary infertility; 20 women with a history of pregnancy loss | 21 treated 15 untreated | 3D US, HSG | Hysteroscopic resection of the uterine septum with resectoscope. Vaginal septum section with Metzenbaum scissors. Guidance technique: Foley balloon and laparoscopic control | To evaluate reproductive outcomes of women who underwent resectoscopic metroplasty: pregnancy rate, miscarriage rate, preterm delivery rate | To evaluate dyspareunia and dysmenorrhea after metroplasty, operative delivery rate, live birth rate, evaluation of adherent placentas and uterine ruptures | Not reported | Treated group: increased pregnancy rate and term delivery rate. Decreased miscarriage rate. No significant effect on primary infertility. 8/20 term deliveries. 1 patient lost to follow up 1/20 spontaneous abortion Preterm delivery: 0/9 |
| A mullerian anomaly ‘‘without classification’’: Septate uterus with double cervix and longitudinal vaginal septum. | Celik et al. 2012 [20] | Turkey | Case report | Primary infertility, Dyspareunia | 1 | TVUS, HSG, MRI | Vaginal septum excision using scissors + hysteroscopic metroplasty (instrument not specified). Guidance technique: Laparoscopic post-procedure control | To establish the true incidence of this anomaly | \ | no | Not conceived after 7 months |
| Management of Complete vagino- Uterine septum in Patients seeking fertility: report of two cases and review of literature. | Seet et al. 2015 [21] | U.K. | Case report | Primary infertility, dysmenorrh ea | 2 | TVUS, MRI, HSG | Resection of vaginal septum with scissors, hysteroscopic transcervical resection of the cervical and uterine septum with thin- gauge bipolar electrocautery Guidance technique: laparoscopic control | To evaluate the reproductive outcome after metroplasty | To evaluate the best technique of metroplasty. In case of cervical septum whether the cervical septum should be preserved or resected | Yes | Pt 1 not specified Pt 2 delivery at term (prophylactic cervical cerclage) |
| Pregnancy after Hysteroscopic metroplasty under laparoscopy in a woman with complete septate uterus: A case report. | Tajiri et al. 2015 [22] | Japan | Case report | Primary infertility | 1 | TVUS, MRI | Vaginal septectomy and hysteroscopic uterine septum resection by a loop type monopoles electrode. Guidance technique: laparoscopy | To evaluate the reproductive outcome after metroplasty | To evaluate the best technique of metroplasty | No | Spontaneous pregnancy ongoing |
| Double cervix, septate uterus and longitudinal vaginal septum: a rare Müllerian anomaly with leiomyoma of the uterus | Gezer et al. 2019 [23] | Turkey | Case report | Primary infertility, dyspareunia | 1 | HSG | Excision of longitudinal vaginal septum + unipolar resection of uterine septum Guidance technique: 12 F Foley catheter + laparoscopy | Whether metroplasty increases pregnancy rate (time between procedure and conception) | Excision of subserosal leiomyoma on the posterior wall of the uterine septum | Not reported | Not conceived after 6 months follow up |
| A septate uterus with double cervix during two pregnancies: pregnancy outcome before and after cervix sparing metroplasty. | Seljeflot et al. 2020 [24] | Slovenia | Case report | Primary infertility | 1 | 3D TVUS, MRI | Surgical excision of the vaginal septum years before + dilatation of the two cervical canals with Hegar dilators+ hysteroscopic resection using resectoscope Guidance technique: Hegars dilators | Whether Metroplasty decreses the risk of preterm birth | To define the best way of diagnosis of this complex anomaly | Yes | Normal vaginal delivery at term after treatment |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parodi, L.; Hoxhaj, I.; Dinoi, G.; Mirandola, M.; Pozzati, F.; Topouzova, G.; Testa, A.C.; Scambia, G.; Catena, U. Complete Uterine Septum, Double Cervix and Vaginal Septum (U2b C2 V1): Hysteroscopic Management and Fertility Outcomes—A Systematic Review. J. Clin. Med. 2023, 12, 189. https://doi.org/10.3390/jcm12010189
Parodi L, Hoxhaj I, Dinoi G, Mirandola M, Pozzati F, Topouzova G, Testa AC, Scambia G, Catena U. Complete Uterine Septum, Double Cervix and Vaginal Septum (U2b C2 V1): Hysteroscopic Management and Fertility Outcomes—A Systematic Review. Journal of Clinical Medicine. 2023; 12(1):189. https://doi.org/10.3390/jcm12010189
Chicago/Turabian StyleParodi, Luca, Ilda Hoxhaj, Giorgia Dinoi, Mariateresa Mirandola, Federica Pozzati, Ghergana Topouzova, Antonia Carla Testa, Giovanni Scambia, and Ursula Catena. 2023. "Complete Uterine Septum, Double Cervix and Vaginal Septum (U2b C2 V1): Hysteroscopic Management and Fertility Outcomes—A Systematic Review" Journal of Clinical Medicine 12, no. 1: 189. https://doi.org/10.3390/jcm12010189
APA StyleParodi, L., Hoxhaj, I., Dinoi, G., Mirandola, M., Pozzati, F., Topouzova, G., Testa, A. C., Scambia, G., & Catena, U. (2023). Complete Uterine Septum, Double Cervix and Vaginal Septum (U2b C2 V1): Hysteroscopic Management and Fertility Outcomes—A Systematic Review. Journal of Clinical Medicine, 12(1), 189. https://doi.org/10.3390/jcm12010189






