Single-Position Oblique Lumbar Interbody Fusion and Percutaneous Pedicle Screw Fixation under O-Arm Navigation: A Retrospective Comparative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Data Collection
2.3. Surgical Technique
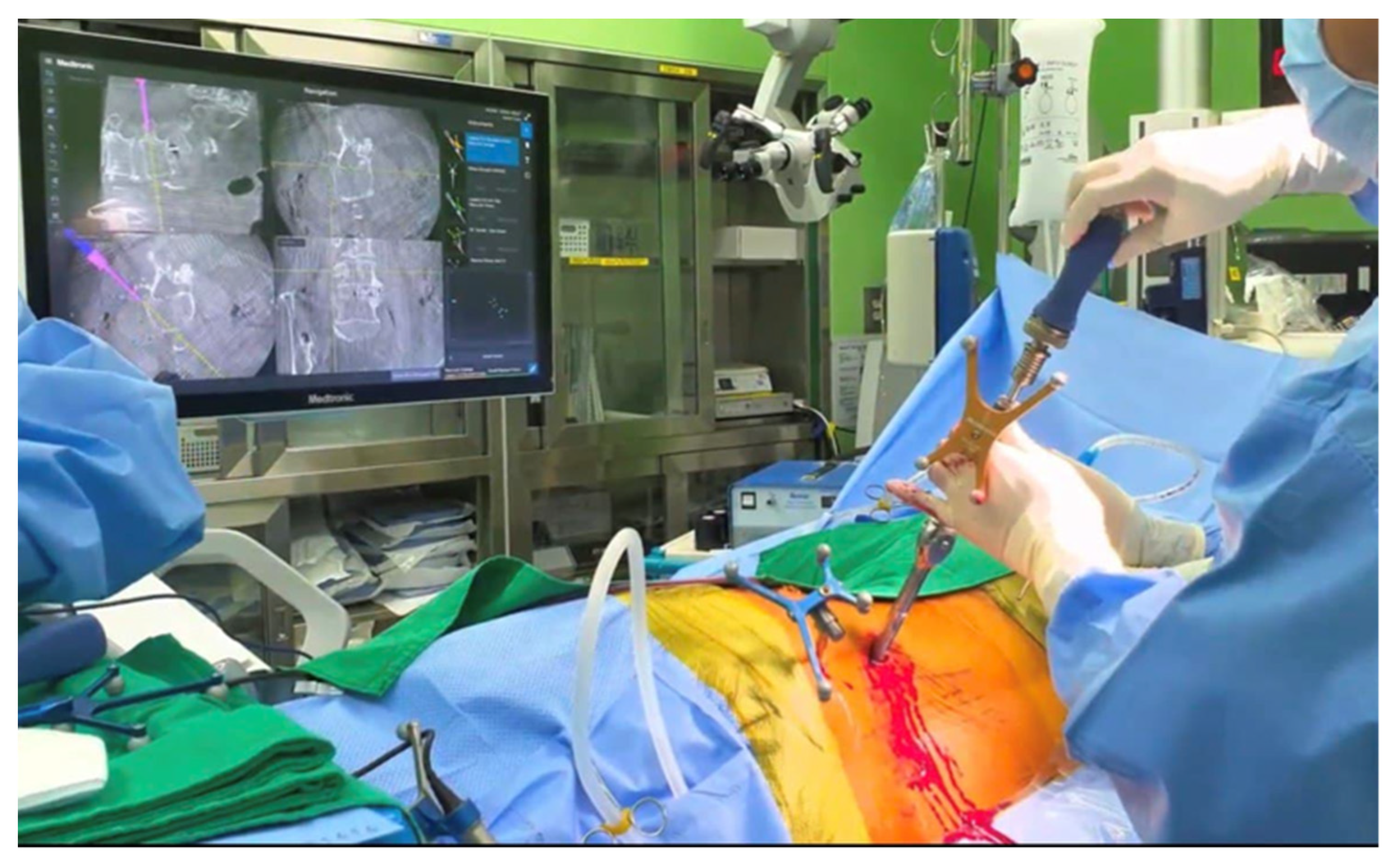
2.3.1. SP-OLIF
2.3.2. C-OLIF
2.4. Radiologic Outcomes
2.5. Clinical Outcomes
2.6. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Radiologic Outcomes
3.2.1. Pedicle Screw Accuracy
3.2.2. Radiologic Parameters and Fusion Rates
3.3. Clinical Outcomes
3.4. Surgical Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nomura, H.; Yamashita, A.; Watanabe, T.; Shirasawa, K. Quantitative analysis of indirect decompression in extreme lateral interbody fusion and posterior spinal fusion with a percutaneous pedicle screw system for lumbar spinal stenosis. J. Spine Surg. 2019, 5, 266–272. [Google Scholar] [CrossRef]
- Castellvi, A.E.; Nienke, T.W.; Marulanda, G.A.; Murtagh, R.D.; Santoni, B.G. Indirect decompression of lumbar stenosis with transpsoas interbody cages and percutaneous posterior instrumentation. Clin. Orthop. Relat. Res. 2014, 472, 1784–1791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soegaard, R.; Bünger, C.E.; Christiansen, T.; Høy, K.; Eiskjaer, S.P.; Christensen, F.B. Circumferential fusion is dominant over posterolateral fusion in a long-term perspective: Cost-utility evaluation of a randomized controlled trial in severe, chronic low back pain. Spine 2007, 32, 2405–2414. [Google Scholar] [PubMed]
- Bassani, R.; Morselli, C.; Querenghi, A.M.; Nuara, A.; Sconfienza, L.M.; Peretti, G.M. Functional and radiological outcome of anterior retroperitoneal versus posterior transforaminal interbody fusion in the management of single-level lumbar degenerative disease. Neurosurg. Focus 2020, 49, E2. [Google Scholar] [CrossRef] [PubMed]
- Fritzell, P.; Hägg, O.; Wessberg, P.; Nordwall, A. Chronic low back pain and fusion: A comparison of three surgical techniques: A prospective multicenter randomized study from the swedish lumbar spine study group. Spine 2002, 27, 1131–1141. [Google Scholar] [CrossRef]
- Holly, L.T.; Foley, K.T. Image guidance in spine surgery. Orthop. Clin. N. A. 2007, 38, 451–461, abstract viii. [Google Scholar]
- Costa, F.; Cardia, A.; Ortolina, A.; Fabio, G.; Zerbi, A.; Fornari, M. Spinal navigation: Standard preoperative versus intraoperative computed tomography data set acquisition for computer-guidance system: Radiological and clinical study in 100 consecutive patients. Spine 2011, 36, 2094–2098. [Google Scholar]
- Mason, A.; Paulsen, R.; Babuska, J.M.; Rajpal, S.; Burneikiene, S.; Nelson, E.L.; Villavicencio, A.T. The accuracy of pedicle screw placement using intraoperative image guidance systems. J. Neurosurg. Spine 2014, 20, 196–203. [Google Scholar] [CrossRef] [Green Version]
- Gelalis, I.D.; Paschos, N.K.; Pakos, E.E.; Politis, A.N.; Arnaoutoglou, C.M.; Karageorgos, A.C.; Ploumis, A.; Xenakis, T.A. Accuracy of pedicle screw placement: A systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur. Spine J. 2012, 21, 247–255. [Google Scholar]
- Tang, J.; Zhu, Z.; Sui, T.; Kong, D.; Cao, X. Position and complications of pedicle screw insertion with or without image-navigation techniques in the thoracolumbar spine: A meta-analysis of comparative studies. J. Biomed. Res. 2014, 28, 228–239. [Google Scholar]
- Zhang, Y.H.; White, I.; Potts, E.; Mobasser, J.P.; Chou, D. Comparison perioperative factors during minimally invasive pre-psoas lateral interbody fusion of the lumbar spine using either navigation or conventional fluoroscopy. Glob. Spine J. 2017, 7, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Xi, Z.; Chou, D.; Mummaneni, P.V.; Burch, S. The navigated oblique lumbar interbody fusion: Accuracy rate, effect on surgical time, and complications. Neurospine 2020, 17, 260–267. [Google Scholar] [PubMed] [Green Version]
- Blizzard, D.J.; Thomas, J.A. Mis single-position lateral and oblique lateral lumbar interbody fusion and bilateral pedicle screw fixation: Feasibility and perioperative results. Spine 2018, 43, 440–446. [Google Scholar] [CrossRef]
- Ouchida, J.; Kanemura, T.; Satake, K.; Nakashima, H.; Ishikawa, Y.; Imagama, S. Simultaneous single-position lateral interbody fusion and percutaneous pedicle screw fixation using o-arm-based navigation reduces the occupancy time of the operating room. Eur. Spine J. 2020, 29, 1277–1286. [Google Scholar] [CrossRef] [PubMed]
- Kotani, Y.; Koike, Y.; Ikeura, A.; Tokunaga, H.; Saito, T. Clinical and radiologic comparison of anterior-posterior single-position lateral surgery versus mis-tlif for degenerative lumbar spondylolisthesis. J. Orthop. Sci. 2021, 26, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Mills, E.S.; Treloar, J.; Idowu, O.; Shelby, T.; Alluri, R.K.; Hah, R.J. Single position lumbar fusion: A systematic review and meta-analysis. Spine J. 2022, 22, 429–443. [Google Scholar]
- Hiyama, A.; Katoh, H.; Sakai, D.; Sato, M.; Tanaka, M.; Watanabe, M. Comparison of radiological changes after single- position versus dual-position for lateral interbody fusion and pedicle screw fixation. BMC Musculoskelet. Disord. 2019, 20, 601. [Google Scholar] [CrossRef] [Green Version]
- Meyerding, H.W. Low backache and sciatic pain associated with spondylolisthesis and protruded intervertebral disc: Incidence, significance, and treatment. JBJS 1941, 23, 461–470. [Google Scholar]
- Gertzbein, S.D.; Robbins, S.E. Accuracy of pedicular screw placement in vivo. Spine 1990, 15, 11–14. [Google Scholar] [CrossRef]
- Amiot, L.P.; Labelle, H.; DeGuise, J.A.; Sati, M.; Brodeur, P.; Rivard, C.H. Computer-assisted pedicle screw fixation. A feasibility study. Spine 1995, 20, 1208–1212. [Google Scholar]
- Kalfas, I.H. Machine vision navigation in spine surgery. Front. Surg. 2021, 8, 640554. [Google Scholar] [CrossRef] [PubMed]
- Pham, M.H.; Diaz-Aguilar, L.D.; Shah, V.; Brandel, M.; Loya, J.; Lehman, R.A. Simultaneous robotic single position oblique lumbar interbody fusion with bilateral sacropelvic fixation in lateral decubitus. Neurospine 2021, 18, 406–412. [Google Scholar] [CrossRef]
- Wang, T.Y.; Park, C.; Dalton, T.; Rajkumar, S.; McCray, E.; Owolo, E.; Than, K.D.; Abd-El-Barr, M.M. Robotic navigation in spine surgery: Where are we now and where are we going? J. Clin. Neurosci. 2021, 94, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Sielatycki, J.A.; Mitchell, K.; Leung, E.; Lehman, R.A. State of the art review of new technologies in spine deformity surgery-robotics and navigation. Spine Deform. 2022, 10, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Wu, D.; Wang, Q.; Wei, Y.; Yuan, F. Pedicle screw insertion: Is o-arm-based navigation superior to the conventional freehand technique? A systematic review and meta-analysis. World Neurosurg. 2020, 144, e87–e99. [Google Scholar] [CrossRef] [PubMed]
- Mayer, H.M. A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine 1997, 22, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Choy, W.; Mayer, R.R.; Mummaneni, P.V.; Chou, D. Oblique lumbar interbody fusion with stereotactic navigation: Technical note. Glob. Spine J. 2020, 10, 94S–100S. [Google Scholar] [CrossRef]
- Pierce, K.E.; Kapadia, B.H.; Bortz, C.; Brown, A.; Alas, H.; Naessig, S.; Ahmad, W.; Vasquez-Montes, D.; Manning, J.; Wang, E.; et al. Operative fusion of patients with metabolic syndrome increases risk for perioperative complications. J. Clin. Neurosci. 2020, 72, 142–145. [Google Scholar] [CrossRef]
- Hiyama, A.; Sakai, D.; Sato, M.; Watanabe, M. The analysis of percutaneous pedicle screw technique with guide wire-less in lateral decubitus position following extreme lateral interbody fusion. J. Orthop. Surg. Res. 2019, 14, 304. [Google Scholar] [CrossRef] [Green Version]
- Drazin, D.; Kim, T.T.; Johnson, J.P. Simultaneous lateral interbody fusion and posterior percutaneous instrumentation: Early experience and technical considerations. Biomed. Res. Int. 2015, 2015, 458284. [Google Scholar] [CrossRef] [Green Version]
- Tian, N.F.; Xu, H.Z. Image-guided pedicle screw insertion accuracy: A meta-analysis. Int. Orthop. 2009, 33, 895–903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, W.; Wang, W.; Chen, S.; Wu, K.; Wang, H. O-arm navigation versus c-arm guidance for pedicle screw placement in spine surgery: A systematic review and meta-analysis. Int. Orthop. 2020, 44, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, A.; Katoh, H.; Nomura, S.; Sakai, D.; Watanabe, M. Intraoperative computed tomography-guided navigation versus fluoroscopy for single-position surgery after lateral lumbar interbody fusion. J. Clin. Neurosci. 2021, 93, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Park, P. Impact of spinal navigation on the oblique lumbar interbody fusion. Neurospine 2020, 17, 268–269. [Google Scholar] [CrossRef] [PubMed]
- DiGiorgio, A.M.; Edwards, C.S.; Virk, M.S.; Mummaneni, P.V.; Chou, D. Stereotactic navigation for the prepsoas oblique lateral lumbar interbody fusion: Technical note and case series. Neurosurg. Focus 2017, 43, E14. [Google Scholar] [CrossRef] [Green Version]
- Mehren, C.; Mayer, H.M.; Zandanell, C.; Siepe, C.J.; Korge, A. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin. Orthop. Relat. Res. 2016, 474, 2020–2027. [Google Scholar] [CrossRef] [Green Version]
- Mobbs, R.J.; Phan, K.; Malham, G.; Seex, K.; Rao, P.J. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including plif, tlif, mi-tlif, olif/atp, llif and alif. J. Spine Surg. 2015, 1, 2–18. [Google Scholar]
- Woods, K.R.; Billys, J.B.; Hynes, R.A. Technical description of oblique lateral interbody fusion at l1-l5 (olif25) and at l5-s1 (olif51) and evaluation of complication and fusion rates. Spine J. 2017, 17, 545–553. [Google Scholar] [CrossRef]
- He, W.; He, D.; Sun, Y.; Xing, Y.; Liu, M.; Wen, J.; Wang, W.; Xi, Y.; Tian, W.; Ye, X. Quantitative analysis of paraspinal muscle atrophy after oblique lateral interbody fusion alone vs. Combined with percutaneous pedicle screw fixation in patients with spondylolisthesis. BMC Musculoskelet. Disord. 2020, 21, 30. [Google Scholar] [CrossRef] [Green Version]
- Tai-bang, C.; Xiao-qing, H.E.; Liang, J.-l. Comparison of oblique lateral interbody fusion and transforaminal lumbar interbody fusion for degenerative lumbar disease: A meta-analysis. Res. Sq. 2021. [Google Scholar] [CrossRef]
- Teng, I.; Han, J.; Phan, K.; Mobbs, R. A meta-analysis comparing alif, plif, tlif and llif. J. Clin. Neurosci. 2017, 44, 11–17. [Google Scholar] [CrossRef]
- Parajón, A.; Alimi, M.; Navarro-Ramirez, R.; Christos, P.; Torres-Campa, J.M.; Moriguchi, Y.; Lang, G.; Härtl, R. Minimally invasive transforaminal lumbar interbody fusion: Meta-analysis of the fusion rates. What is the optimal graft material? Neurosurgery 2017, 81, 958–971. [Google Scholar] [CrossRef] [Green Version]
- Lowe, T.G.; Tahernia, A.D.; O’Brien, M.F.; Smith, D.A. Unilateral transforaminal posterior lumbar interbody fusion (tlif): Indications, technique, and 2-year results. J. Spinal. Disord. Tech. 2002, 15, 31–38. [Google Scholar] [CrossRef]


| SP-OLIF (O-Arm) | C-OLIF (C-Arm) | p-Value | 95% C.I of the Difference | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Total number | 36 | 20 | - | ||
| Sex (male:female) | 16:20 | 6:14 | 0.255 | ||
| Mean age (years) | 61.78 ± 8.33 | 64.30 ± 7.01 | 0.258 | −6.950 | 1.906 |
| BMI (kg/m2) | 25.67 ± 5.02 | 25.00 ± 2.67 | 0.579 | −1.752 | 3.103 |
| BMD (T-score; mean ± SD) | −0.98 ± 1.03 | −1.43 ± 1.38 | 0.169 | −0.199 | 1.105 |
| ASA class | 2.50 ± 0.66 | 2.20 ± 0.52 | 0.084 | −0.042 | 0.642 |
| Operative time (mins) | 185.00 ± 36.46 | 198.30 ± 41.75 | 0.220 | −34.773 | 8.173 |
| Estimated blood loss (mL) | 131.94 ± 95.40 | 270.00 ± 238.64 | 0.003 | −228.103 | −48.008 |
| Hospital stays (days) | 7.97 ± 2.43 | 5.40 ± 1.00 | 0.000 | 1.429 | 3.716 |
| Pre-operative diagnosis, n (%) | 0.963 | ||||
| Spinal stenosis | 21 (58.3%) | 11 | - | - | - |
| Degenerative SPL | 12 (33.3%) | 7 | - | - | - |
| Spondylolytic SPL | 3 (8.3%) | 2 | - | - | - |
| Distribution of instrumented levels, n (%) | 0.362 | ||||
| L3/4 | 4 (11.1%) | 4 (20.0%) | - | - | - |
| L4/5 | 32 (88.9%) | 16 (80.0%) | - | - | - |
| Grade | Breach Distance (mm) |
|---|---|
| A | 0 |
| B | <2 |
| C | <4 |
| D | <6 |
| E | >6 |
| GRS Grade | SP-OLIF (O-Arm) | C-OLIF (C-Arm) | p-Value |
|---|---|---|---|
| Grade A | 139/144 (96.5%) | 77/80 (96.3%) | 0.915 |
| Grade B | 5/144 (3.5%) | 3/80 (3.8%) | 0.915 |
| Grade C | 0/144 (0%) | 1/80 (1.3%) | 0.179 |
| Grade D, E | 0/144 (0%) | 0/80 (0%) | 1.000 |
| SP-OLIF (O-Arm) | C-OLIF (C-Arm) | p-Value | |
|---|---|---|---|
| Flexion (°) | 9.94 ± 5.64 | 8.05 ± 3.11 | 0.171 |
| Extension (°) | 11.39 ± 5.96 | 9.98 ± 3.01 | 0.324 |
| Dynamic (flexion minus extension, °) | 1.45 ± 3.98 | 1.95 ± 1.53 | 0.598 |
| The number of BTB formation (by CT) | 33/36 (91.7%) | 17/20 (85.0%) | 0.930 |
| Fusion rates | 94.4% (34/36) | 90.0% (18/20) | 0.536 |
| SP-OLIF (O-Arm) | C-OLIF (C-Arm) | p-Value | |
|---|---|---|---|
| Pre_VAS | 7.31 ± 1.31 | 7.25 ± 1.94 | 0.899 |
| Pre_ODI | 45.69 ± 14.60 | 46.55 ± 18.77 | 0.850 |
| Pre_PCS of SF-36 | 34.53 ± 16.69 | 41.15 ± 16.61 | 0.160 |
| Pre_MCS of SF-36 | 52.50 ± 18.35 | 51.46 ± 21.20 | 0.848 |
| Post_VAS | 2.56 ± 2.04 | 3.30 ± 2.27 | 0.214 |
| Post_ODI | 18.81 ± 10.99 | 28.20 ± 17.06 | 0.015 |
| Post_PCS of SF-36 | 62.22 ± 14.09 | 47.63 ± 15.03 | 0.000 |
| Post_MCS of SF-36 | 74.17 ± 13.82 | 52.89 ± 15.68 | 0.000 |
| Type of Complication | SP-OLIF (O-Arm) | C-OLIF (C-Arm) | p-Value |
|---|---|---|---|
| Revision | None (0%) | 1 (5%) | 0.176 |
| Surgical site infection | None (0%) | None (0%) | 1.000 |
| Ipsilateral weakness | 1 (2.8%) | None (0%) | 0.452 |
| Radicular pain or numbness | 3 (8.3%) | 2 (10%) | 0.788 |
| Overall complication rate | 4 (11.1%) | 3 (15%) | 0.673 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.C.; Jeong, Y.H.; Oh, S.H.; Lee, J.M.; Lee, C.K.; Yi, S.; Ha, Y.; Kim, K.N.; Shin, D.A. Single-Position Oblique Lumbar Interbody Fusion and Percutaneous Pedicle Screw Fixation under O-Arm Navigation: A Retrospective Comparative Study. J. Clin. Med. 2023, 12, 312. https://doi.org/10.3390/jcm12010312
Kim HC, Jeong YH, Oh SH, Lee JM, Lee CK, Yi S, Ha Y, Kim KN, Shin DA. Single-Position Oblique Lumbar Interbody Fusion and Percutaneous Pedicle Screw Fixation under O-Arm Navigation: A Retrospective Comparative Study. Journal of Clinical Medicine. 2023; 12(1):312. https://doi.org/10.3390/jcm12010312
Chicago/Turabian StyleKim, Hyung Cheol, Yeong Ha Jeong, Sung Han Oh, Jong Min Lee, Chang Kyu Lee, Seong Yi, Yoon Ha, Keung Nyun Kim, and Dong Ah Shin. 2023. "Single-Position Oblique Lumbar Interbody Fusion and Percutaneous Pedicle Screw Fixation under O-Arm Navigation: A Retrospective Comparative Study" Journal of Clinical Medicine 12, no. 1: 312. https://doi.org/10.3390/jcm12010312
APA StyleKim, H. C., Jeong, Y. H., Oh, S. H., Lee, J. M., Lee, C. K., Yi, S., Ha, Y., Kim, K. N., & Shin, D. A. (2023). Single-Position Oblique Lumbar Interbody Fusion and Percutaneous Pedicle Screw Fixation under O-Arm Navigation: A Retrospective Comparative Study. Journal of Clinical Medicine, 12(1), 312. https://doi.org/10.3390/jcm12010312





