Computed Tomography Morphology of Affected versus Unaffected Sides in Patients with Unilateral Primary Acquired Nasolacrimal Duct Obstruction
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Ethics
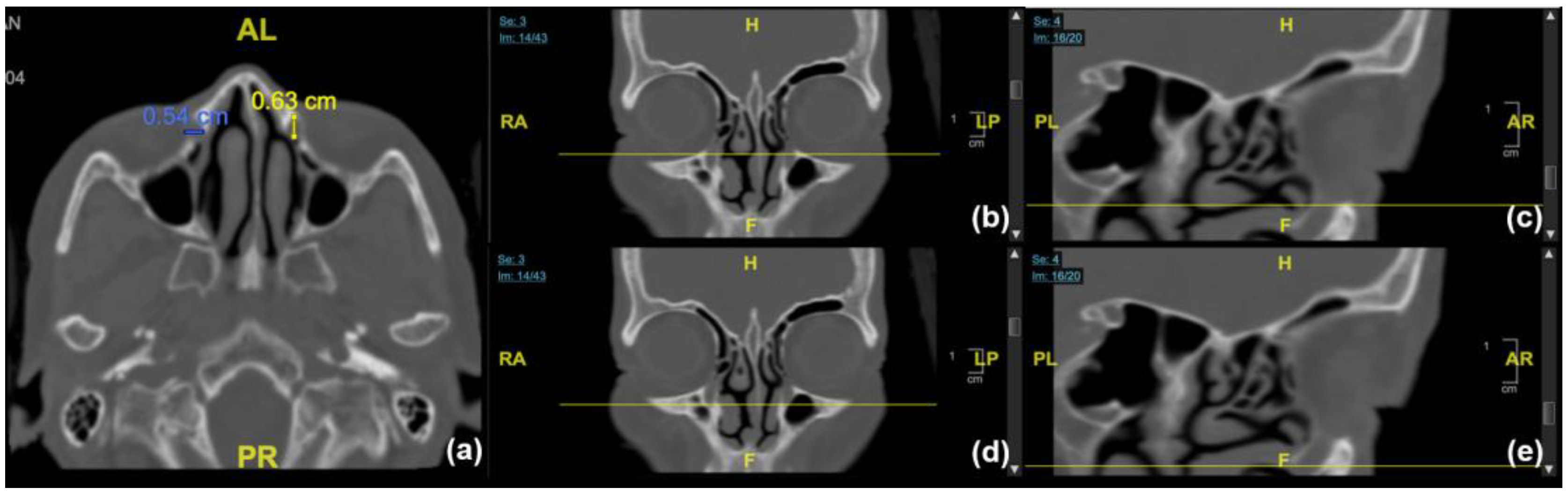
2.2. Data Retrieval and Processing
2.3. Statistical Analyses
3. Results
Patient Characteristics and Measurement Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Linberg, J.V.; McCormick, S.A. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology 1986, 93, 1055–1063. [Google Scholar] [CrossRef]
- Bartley, G.B. Acquired lacrimal drainage obstruction: An etiologic classification system, case reports, and a review of the literature. Part 3. Ophthalmic Plast Reconstr. Surg. 1993, 9, 11–26. [Google Scholar] [CrossRef] [PubMed]
- Steinkogler, F.J. The postsaccal, idiopathic dacryostenosis—Experimental and clinical aspects. Doc. Ophthalmol. 1986, 63, 265–286. [Google Scholar] [CrossRef] [PubMed]
- Kashkouli, M.B.; Sadeghipour, A.; Kaghazkanani, R.; Bayat, A.; Pakdel, F.; Aghai, G.H. Pathogenesis of primary acquired nasolacrimal duct obstruction. Orbit 2010, 29, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Ohtomo, K.; Ueta, T.; Toyama, T.; Nagahara, M. Predisposing factors for primary acquired nasolacrimal duct obstruction. Graefes Arch. Clin. Exp. Ophthalmol. 2013, 251, 1835–1839. [Google Scholar] [CrossRef] [PubMed]
- Seider, N.; Miller, B.; Beiran, I. Topical glaucoma therapy as a risk factor for nasolacrimal duct obstruction. Am. J. Ophthalmol. 2008, 145, 120–123. [Google Scholar] [CrossRef] [PubMed]
- Janssen, A.G.; Mansour, K.; Bos, J.J.; Castelijns, J.A. Diameter of the bony lacrimal canal: Normal values and values related to nasolacrimal duct obstruction: Assessment with CT. AJNR Am. J. Neuroradiol. 2001, 22, 845–850. [Google Scholar] [PubMed]
- Lee, H.; Ha, S.; Lee, Y.; Park, M.; Baek, S. Anatomical and morphometric study of the bony nasolacrimal canal using computed tomography. Ophthalmologica 2012, 227, 153–159. [Google Scholar] [CrossRef]
- McCormick, A.; Sloan, B. The diameter of the nasolacrimal canal measured by computed tomography: Gender and racial differences. Clin. Exp. Ophthalmol. 2009, 37, 357–361. [Google Scholar] [CrossRef]
- Takahashi, Y.; Nakamura, Y.; Nakano, T.; Asamoto, K.; Iwaki, M.; Selva, D.; Leibovitch, I.; Kakizaki, H. The narrowest part of the bony nasolacrimal canal: An anatomical study. Ophthalmic Plast Reconstr. Surg. 2013, 29, 318–322. [Google Scholar] [CrossRef]
- Fasina, O.; Ogbole, G.I. CT assessment of the nasolacrimal canal in a black African Population. Ophthalmic Plast Reconstr. Surg. 2013, 29, 231–233. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Nakata, K.; Miyazaki, H.; Ichinose, A.; Kakizaki, H. Comparison of bony nasolacrimal canal narrowing with or without primary acquired nasolacrimal duct obstruction in a Japanese population. Ophthalmic Plast Reconstr. Surg. 2014, 30, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Bulbul, E.; Yazici, A.; Yanik, B.; Yazici, H.; Demirpolat, G. Morphometric Evaluation of Bony Nasolacrimal Canal in a Caucasian Population with Primary Acquired Nasolacrimal Duct Obstruction: A Multidetector Computed Tomography Study. Korean J. Radiol. 2016, 17, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.J.; Paulsen, F. Etiopathogenesis of Primary Acquired Nasolacrimal Duct Obstruction: What We Know and What We Need to Know. Ophthalmic Plast Reconstr. Surg. 2019, 35, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Yazici, H.; Bulbul, E.; Yazici, A.; Kaymakci, M.; Tiskaoglu, N.; Yanik, B.; Ermis, S. Primary acquired nasolacrimal duct obstruction: Is it really related to paranasal abnormalities? Surg. Radiol. Anat. 2015, 37, 579–584. [Google Scholar] [CrossRef]
- Gul, A.; Aslan, K.; Karli, R.; Ariturk, N.; Can, E. A Possible Cause of Nasolacrimal Duct Obstruction: Narrow Angle between Inferior Turbinate and Upper Part of the Medial Wall of the Maxillary Sinus. Curr. Eye Res. 2016, 41, 729–733. [Google Scholar] [CrossRef] [PubMed]
- Habesoglu, M.; Eriman, M.; Habesoglu, T.E.; Kinis, V.; Surmeli, M.; Deveci, I.; Deveci, S. Co-occurrence and possible role of sinonasal anomalies in primary acquired nasolacrimal duct obstruction. J. Craniofac. Surg. 2013, 24, 497–500. [Google Scholar] [CrossRef]
- Dikici, O.; Ulutas, H.G. Relationship between Primary Acquired Nasolacrimal Duct Obstruction, Paranasal Abnormalities and Nasal Septal Deviation. J. Craniofac. Surg. 2020, 31, 782–786. [Google Scholar] [CrossRef]
- Kallman, J.E.; Foster, J.A.; Wulc, A.E.; Yousem, D.M.; Kennedy, D.W. Computed tomography in lacrimal outflow obstruction. Ophthalmology 1997, 104, 676–682. [Google Scholar] [CrossRef]
- Dalgic, A.; Ceylan, M.E.; Celik, C.; Aliyeva, A.; Aksoy, G.Y.; Edizer, D.T. Outcomes of Endoscopic Powered Revision Dacryocystorhinostomy. J. Craniofac. Surg. 2018, 29, 1960–1962. [Google Scholar] [CrossRef]
- Lin, G.C.; Brook, C.D.; Hatton, M.P.; Metson, R. Causes of dacryocystorhinostomy failure: External versus endoscopic approach. Am. J. Rhinol. Allergy 2017, 31, 181–185. [Google Scholar] [CrossRef] [PubMed]


| / | PANDO Side | Non-PANDO Side | p-Value | |||
|---|---|---|---|---|---|---|
| A-P Diameter | Transverse Diameter | A-P Diameter | Transverse Diameter | |||
| Mean ± SD (mm) | ||||||
| Entrance | 5.77 ± 1.39 | 4.49 ± 1.32 | 5.76 ± 1.30 | 4.58 ± 1.31 | 0.439 | 0.188 |
| Exit | 7.06 ± 1.94 | 4.22 ± 1.15 | 7.00 ± 1.79 | 4.37 ± 1.05 | 0.357 | 0.085 |
| Minimum | 3.63 ± 1.08 | 4.07 ± 1.13 | 0.002 * | |||
| PANDO Side | Non-PANDO Side | p-Value | ||||
|---|---|---|---|---|---|---|
| Diameter | A-P | Transverse | A-P | Transverse | ||
| Mean ± SD (mm) | Mean ± SD (mm) | |||||
| Female (n = 46) | ||||||
| Entrance | 5.77 ± 1.39 | 4.37 ± 1.24 | 5.73± 1.29 | 4.46 ± 1.24 | 0.444 | 0.353 |
| Exit | 7.03± 2.01 | 4.19 ± 1.19 | 6.90 ± 1.78 | 4.27 ± 1.01 | 0.263 | 0.076 |
| Minimum | 3.57 ± 1.08 | 3.98 ± 1.11 | 0.016 * | |||
| Male (n = 4) | ||||||
| Entrance | 5.83 ± 1.62 | 5.95 ± 1.51 | 6.10± 1.51 | 5.93 ± 1.44 | 0.406 | 0.491 |
| Exit | 7.38± 0.85 | 4.60 ± 0.39 | 8.08 ± 1.65 | 5.48 ± 0.92 | 0.240 | 0.066 |
| Minimum | 4.70 ± 0.55 | 5.10 ± 0.85 | 0.023 * | |||
| p-value | ||||||
| Entrance | 0.474 | 0.062 | 0.331 | 0.066 | ||
| Exit | 0.263 | 0.076 | 0.127 | 0.073 | ||
| Minimum | 0.014 ** | 0.036 ** | ||||
| Entrance Level | Minimum Transverse Diameter | Exit Level | |||
|---|---|---|---|---|---|
| A-P Diameter | Transverse Diameter | A-P Diameter | Transverse Diameter | ||
| r (correlation coefficient) | |||||
| PANDO side | 0.170 | 0.202 | 0.179 | 0.194 | 0.057 |
| non-PANDO side | 0.273 | 0.225 | 0.205 | 0.211 | 0.206 |
| PANDO Side | Non-PANDO Side | |||
|---|---|---|---|---|
| n | (%) | n | (%) | |
| Columnar | 24 | 48 | 33 | 66 |
| Flare | 17 | 34 | 11 | 22 |
| Funnel | 4 | 8 | 2 | 4 |
| Hourglass | 5 | 10 | 4 | 8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, P.-Y.; Wang, J.-K.; Chang, S.-W. Computed Tomography Morphology of Affected versus Unaffected Sides in Patients with Unilateral Primary Acquired Nasolacrimal Duct Obstruction. J. Clin. Med. 2023, 12, 340. https://doi.org/10.3390/jcm12010340
Su P-Y, Wang J-K, Chang S-W. Computed Tomography Morphology of Affected versus Unaffected Sides in Patients with Unilateral Primary Acquired Nasolacrimal Duct Obstruction. Journal of Clinical Medicine. 2023; 12(1):340. https://doi.org/10.3390/jcm12010340
Chicago/Turabian StyleSu, Pei-Yuan, Jia-Kang Wang, and Shu-Wen Chang. 2023. "Computed Tomography Morphology of Affected versus Unaffected Sides in Patients with Unilateral Primary Acquired Nasolacrimal Duct Obstruction" Journal of Clinical Medicine 12, no. 1: 340. https://doi.org/10.3390/jcm12010340
APA StyleSu, P.-Y., Wang, J.-K., & Chang, S.-W. (2023). Computed Tomography Morphology of Affected versus Unaffected Sides in Patients with Unilateral Primary Acquired Nasolacrimal Duct Obstruction. Journal of Clinical Medicine, 12(1), 340. https://doi.org/10.3390/jcm12010340




