Non-Hormonal Treatment Options for Regulation of Menstrual Cycle in Adolescents with PCOS
Abstract
:1. Introduction
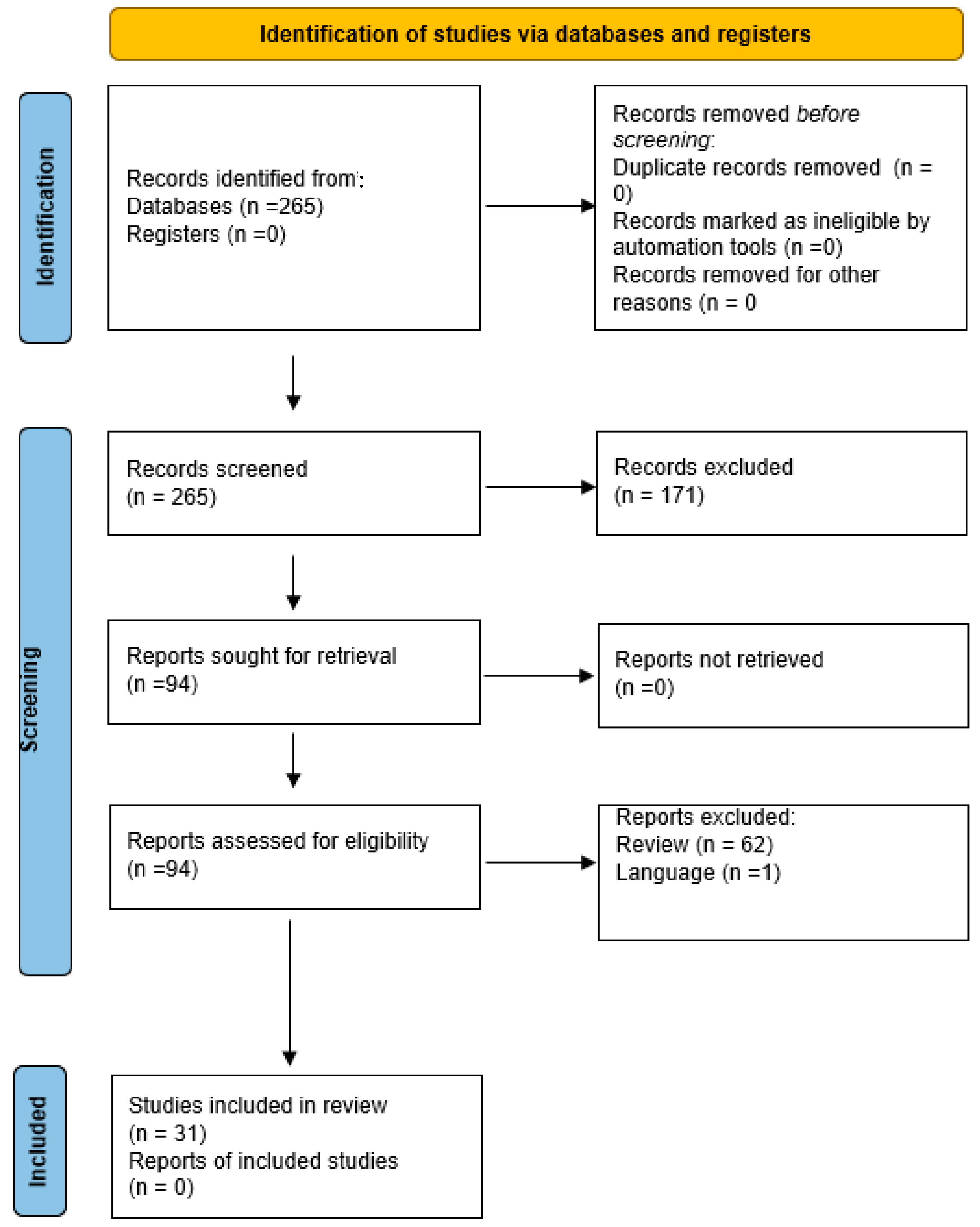
2. Methods and Materials
3. Results
3.1. Metformin
3.2. Glucagon-like Peptide 1 Receptor Agonists
3.3. Thiazolidinediones: Rosiglitazone and Pioglitazone
3.4. Antiandrogens Flutamide, Finasteride, Spironolactone and SPIOMET
3.5. Flutamide
3.6. Finasteride
3.7. Spironolactone
3.8. SPIOMET
3.9. Supplements
3.10. Myo-Inositol
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| COC | Combined oral contraceptives |
| d | per day |
| FDA | Food and Drug Administration |
| HOMA-IR | Homeostasis Model Assessment-Insulin Resistance |
| LIRA | Liraglutid |
| MEN | Multiple Endocrine Neoplasia |
| MET | Metformin |
| Mo | months |
| MYO | Myoinositol |
| NICHD | National Institute of Child Health and Human Development |
| NIH | National Institute of Health |
| PCOS | Polycystic Ovary Syndrome |
| PPAR | Peroxisome Proliferator activated receptor |
| ROS | Rosiglitazone |
| SDS | standard deviation score |
| SPIOMET | Spironolactone, pioglitazone, metformin |
| SPIRO | Spironolactone |
| we | weeks |
References
- Hickey, M.; Doherty, D.A.; Atkinson, H.; Sloboda, D.M.; Franks, S.; Norman, R.J.; Hart, R. Clinical, ultrasound and biochemical features of polycystic ovary syndrome in adolescents: Implications for diagnosis. Hum. Reprod. 2011, 26, 1469–1477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christensen, S.B.; Black, M.H.; Smith, N.; Martinez, M.M.; Jacobsen, S.J.; Porter, A.H.; Koebnick, C. Prevalence of polycystic ovary syndrome in adolescents. Fertil. Steril. 2013, 100, 470–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Youngster, M.; Ward, V.L.; Blood, E.A.; Barnewolt, C.E.; Emans, S.J.; Divasta, A.D. Utility of ultrasound in the diagnosis of polycystic ovary syndrome in adolescents. Fertil. Steril. 2014, 102, 1432–1438. [Google Scholar] [CrossRef] [PubMed]
- Peña, A.S.; Codner, E.; Witchel, S. Criteria for Diagnosis of Polycystic Ovary Syndrome during Adolescence: Literature Review. Diagnostics 2022, 12, 1931. [Google Scholar] [CrossRef]
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil. Steril. 2018, 110, 364–379. [Google Scholar] [CrossRef] [Green Version]
- Ibáñez, L.; Oberfield, S.E.; Witchel, S.; Auchus, R.J.; Chang, R.J.; Codner, E.; Dabadghao, P.; Darendeliler, F.; Elbarbary, N.S.; Gambineri, A.; et al. An International Consortium Update: Pathophysiology, Diagnosis, and Treatment of Polycystic Ovarian Syndrome in Adolescence. Horm. Res. Paediatr. 2017, 88, 371–395. [Google Scholar] [CrossRef]
- Vitek, W.; Alur, S.; Hoeger, K.M. Off-label drug use in the treatment of polycystic ovary syndrome. Fertil. Steril. 2015, 103, 605–611. [Google Scholar] [CrossRef]
- Oppelt, P.G.; Baier, F.; Fahlbusch, C.; Heusinger, K.; Hildebrandt, T.; Breuel, C.; Dittrich, R. What do patients want to know about contraception and which method would they prefer? Arch. Gynecol. Obstet. 2017, 295, 1483–1491. [Google Scholar] [CrossRef]
- Allen, H.F.; Mazzoni, C.; Heptulla, R.A.; Murray, M.A.; Miller, N.; Koenigs, L.; Reiter, E.O. Randomized controlled trial evaluating response to metformin versus standard therapy in the treatment of adolescents with polycystic ovary syndrome. J. Pediatr. Endocrinol. Metab. 2005, 18, 761–768. [Google Scholar] [CrossRef]
- El Maghraby, H.A.; Nafee, T.; Guiziry, D.; Elnashar, A. Randomized controlled trial of the effects of metformin versus combined oral contraceptives in adolescent PCOS women through a 24month follow up period. Middle East Fertil. Soc. J. 2015, 20, 131–137. [Google Scholar] [CrossRef]
- De Leo, V.; Musacchio, M.C.; Morgante, G.; Piomboni, P.; Petraglia, F. Metformin treatment is effective in obese teenage girls with PCOS. Hum. Reprod. 2006, 21, 2252–2256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoeger, K.; Davidson, K.; Kochman, L.; Cherry, T.; Kopin, L.; Guzick, D.S. The impact of metformin, oral contraceptives, and lifestyle modification on polycystic ovary syndrome in obese adolescent women in two randomized, placebo-controlled clinical trials. J. Clin. Endocrinol. Metab. 2008, 93, 4299–4306. [Google Scholar] [CrossRef] [PubMed]
- Glueck, C.J.; Wang, P.; Fontaine, R.; Tracy, T.; Sieve-Smith, L. Metformin to restore normal menses in oligo-amenorrheic teenage girls with polycystic ovary syndrome (PCOS). J. Adolesc. Health 2001, 29, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Glueck, C.J.; Aregawi, D.; Winiarska, M.; Agloria, M.; Luo, G.; Sieve, L.; Wang, P. Metformin-diet ameliorates coronary heart disease risk factors and facilitates resumption of regular menses in adolescents with polycystic ovary syndrome. J. Pediatr. Endocrinol. Metab. 2006, 19, 831–842. [Google Scholar] [CrossRef]
- Glueck, C.J.; Goldenberg, N.; Wang, P. Metformin-diet ameliorates coronary heart disease risk factors and facilitates resumption of regular menses in adolescents with polycystic ovary syndrome. J. Pediatr. Endocrinol. Metab. 2009, 22, 815–826. [Google Scholar] [CrossRef]
- Al-Zubeidi, H.; Klein, K.O. Randomized clinical trial evaluating metformin versus oral contraceptive pills in the treatment of adolescents with polycystic ovarian syndrome. J. Pediatr. Endocrinol. Metab. 2015, 28, 853–858. [Google Scholar] [CrossRef]
- Ladson, G.; Dodson, W.C.; Sweet, S.D.; Archibong, A.E.; Kunselman, A.R.; Demers, L.M.; Lee, P.A.; Williams, N.I.; Coney, P.; Legro, R.S. Effects of metformin in adolescents with polycystic ovary syndrome undertaking lifestyle therapy: A pilot randomized double-blind study. Fertil. Steril. 2011, 95, 2595–2598.e6. [Google Scholar] [CrossRef] [Green Version]
- Ibáñez, L.; Valls, C.; Potau, N.; Marcos, M.V.; de Zegher, F. Sensitization to insulin in adolescent girls to normalize hirsutism, hyperandrogenism, oligomenorrhea, dyslipidemia, and hyperinsulinism after precocious pubarche. J. Clin. Endocrinol. Metab. 2000, 85, 3526–3530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cirillo, F.; Catellani, C.; Lazzeroni, P.; Sartori, C.; Tridenti, G.; Vezzani, C.; Fulghesu, A.M.; Madeddu, E.; Amarri, S.; Street, M.E. HMGB1 is increased in adolescents with polycystic ovary syndrome (PCOS) and decreases after treatment with myo-inositol (MYO) in combination with alpha-lipoic acid (ALA). Gynecol. Endocrinol. 2020, 36, 588–593. [Google Scholar] [CrossRef]
- Narsing Rao, L.; Jacob, J.J.; Paul, T.V.; Rajarathinam, S.; Thomas, N.; Seshadri, M.S. Effects of pioglitazone on menstrual frequency, hyperandrogenism and insulin resistance in adoloscents and young adults with polycystic ovary syndrome. J. Pediatr. Adolesc. Gynecol. 2009, 22, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Stabile, G.; Borrielli, I.; Artenisio, A.C.; Bruno, L.M.; Benvenga, S.; Giunta, L.; La Marca, A.; Volpe, A.; Pizzo, A. Effects of the insulin sensitizer pioglitazone on menstrual irregularity, insulin resistance and hyperandrogenism in young women with polycystic ovary syndrome. J. Pediatr. Adolesc. Gynecol. 2014, 27, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Tfayli, H.; Ulnach, J.W.; Lee, S.; Sutton-Tyrrell, K.; Arslanian, S. Drospirenone/ethinyl estradiol versus rosiglitazone treatment in overweight adolescents with polycystic ovary syndrome: Comparison of metabolic, hormonal, and cardiovascular risk factors. J. Clin. Endocrinol. Metab. 2011, 96, 1311–1319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Leo, V.; Lanzetta, D.; D’Antona, D.; la Marca, A.; Morgante, G. Hormonal effects of flutamide in young women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 1998, 83, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, L.; Potau, N.; Marcos, M.V.; de Zegher, F. Treatment of hirsutism, hyperandrogenism, oligomenorrhea, dyslipidemia, and hyperinsulinism in nonobese, adolescent girls: Effect of flutamide. J. Clin. Endocrinol. Metab. 2000, 85, 3251–3255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganie, M.A.; Khurana, M.L.; Eunice, M.; Gupta, N.; Gulati, M.; Dwivedi, S.N.; Ammini, A.C. Comparison of efficacy of spironolactone with metformin in the management of polycystic ovary syndrome: An open-labeled study. J. Clin. Endocrinol. Metab. 2004, 89, 2756–2762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ibáñez, L.; Díaz, M.; García-Beltrán, C.; Malpique, R.; Garde, E.; López-Bermejo, A.; de Zegher, F. Toward a Treatment Normalizing Ovulation Rate in Adolescent Girls With Polycystic Ovary Syndrome. J. Endocr. Soc. 2020, 4, bvaa032. [Google Scholar] [CrossRef] [Green Version]
- Amr, N.; Abdel-Rahim, H.E. The effect of chromium supplementation on polycystic ovary syndrome in adolescents. J. Pediatr. Adolesc. Gynecol. 2015, 28, 114–118. [Google Scholar] [CrossRef]
- De Leo, V.; la Marca, A.; Petraglia, F. Insulin-lowering agents in the management of polycystic ovary syndrome. Endocr. Rev. 2003, 24, 633–667. [Google Scholar] [CrossRef] [Green Version]
- Papaleo, E.; Unfer, V.; Baillargeon, J.P.; De Santis, L.; Fusi, F.; Brigante, C.; Marelli, G.; Cino, I.; Redaelli, A.; Ferrari, A. Myo-inositol in patients with polycystic ovary syndrome: A novel method for ovulation induction. Gynecol. Endocrinol. 2007, 23, 700–703. [Google Scholar] [CrossRef]
- Genazzani, A.D.; Lanzoni, C.; Ricchieri, F.; Jasonni, V.M. Myo-inositol administration positively affects hyperinsulinemia and hormonal parameters in overweight patients with polycystic ovary syndrome. Gynecol. Endocrinol. 2008, 24, 139–144. [Google Scholar] [CrossRef]
- Knudsen, L.B.; Lau, J. The Discovery and Development of Liraglutide and Semaglutide. Front. Endocrinol. 2019, 10, 155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Can, J.; Sloth, B.; Jensen, C.B.; Flint, A.; Blaak, E.E.; Saris, W.H. Effects of the once-daily GLP-1 analog liraglutide on gastric emptying, glycemic parameters, appetite and energy metabolism in obese, non-diabetic adults. Int. J. Obes. (Lond) 2014, 38, 784–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quinn, C.E.; Hamilton, P.K.; Lockhart, C.J.; McVeigh, G.E. Thiazolidinediones: Effects on insulin resistance and the cardiovascular system. Br. J. Pharmacol. 2008, 153, 636–645. [Google Scholar] [CrossRef] [PubMed]
- Giorgetti, R.; di Muzio, M.; Giorgetti, A.; Girolami, D.; Borgia, L.; Tagliabracci, A. Flutamide-induced hepatotoxicity: Ethical and scientific issues. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 69–77. [Google Scholar]
- Tartagni, M.; Schonauer, M.M.; Cicinelli, E.; Petruzzelli, F.; De Pergola, G.; De Salvia, M.A.; Loverro, G. Intermittent low-dose finasteride is as effective as daily administration for the treatment of hirsute women. Fertil. Steril. 2004, 82, 752–755. [Google Scholar] [CrossRef]
- Piotrowska, A.; Pilch, W.; Czerwińska-Ledwig, O.; Zuziak, R.; Siwek, A.; Wolak, M.; Nowak, G. The Possibilities of Using Chromium Salts as an Agent Supporting Treatment of Polycystic Ovary Syndrome. Biol. Trace Elem. Res. 2019, 192, 91–97. [Google Scholar] [CrossRef] [Green Version]
- Saxenda 6 mg/mL Solution for Injection in Pre-Filled Pen Prescribing Information. Available online: https://www.ema.europa.eu/en/documents/product-information/saxenda-epar-product-information_en.pdf (accessed on 25 November 2022).
- Saxenda (Liraglutide 3.0 mg) Prescribing Information. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/206321Orig1s000lbl.pdf (accessed on 25 November 2022).
- Abdalla, M.A.; Deshmukh, H.; Atkin, S.; Sathyapalan, T. The potential role of incretin-based therapies for polycystic ovary syndrome: A narrative review of the current evidence. Ther. Adv. Endocrinol. Metab. 2021, 12, 2042018821989238. [Google Scholar] [CrossRef]
- Ornstein, R.M.; Copperman, N.M.; Jacobson, M.S. Effect of weight loss on menstrual function in adolescents with polycystic ovary syndrome. J. Pediatr. Adolesc. Gynecol. 2011, 24, 161–165. [Google Scholar] [CrossRef]
- Cataldo, N.A.; Abbasi, F.; McLaughlin, T.L.; Basina, M.; Fechner, P.Y.; Giudice, L.C.; Reaven, G.M. Metabolic and ovarian effects of rosiglitazone treatment for 12 weeks in insulin-resistant women with polycystic ovary syndrome. Hum. Reprod. 2006, 21, 109–120. [Google Scholar] [CrossRef] [Green Version]
- Al Khalifah, R.A.; Florez, I.D.; Zoratti, M.J.; Dennis, B.; Thabane, L.; Bassilious, E. Efficacy of Treatments for Polycystic Ovarian Syndrome Management in Adolescents. J. Endocr. Soc. 2021, 5, bvaa155. [Google Scholar] [CrossRef]
- Paradisi, R.; Venturoli, S. Retrospective observational study on the effects and tolerability of flutamide in a large population of patients with various kinds of hirsutism over a 15-year period. Eur. J. Endocrinol. 2010, 163, 139–147. [Google Scholar] [CrossRef] [PubMed]
- de Zegher, F.; Ibáñez, L. Therapy: Low-dose flutamide for hirsutism: Into the limelight, at last. Nat. Rev. Endocrinol. 2010, 6, 421–422. [Google Scholar] [CrossRef] [PubMed]
- Tartagni, M.V.; Alrasheed, H.; Damiani, G.R.; Montagnani, M.; De Salvia, M.A.; De Pergola, G.; Tartagni, M.; Loverro, G. Intermittent low-dose finasteride administration is effective for treatment of hirsutism in adolescent girls: A pilot study. J. Pediatr. Adolesc. Gynecol. 2014, 27, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Moini Jazani, A.; Nasimi Doost Azgomi, H.; Nasimi Doost Azgomi, A.; Nasimi Doost Azgomi, R. A comprehensive review of clinical studies with herbal medicine on polycystic ovary syndrome (PCOS). Daru 2019, 27, 863–877. [Google Scholar] [CrossRef] [PubMed]
- Cabrera-Cruz, H.; Oróstica, L.; Plaza-Parrochia, F.; Torres-Pinto, I.; Romero, C.; Vega, M. The insulin-sensitizing mechanism of myo-inositol is associated with AMPK activation and GLUT-4 expression in human endometrial cells exposed to a PCOS environment. Am. J. Physiol. Endocrinol. Metab. 2020, 318, E237–E248. [Google Scholar] [CrossRef]
- Carlomagno, G.; Unfer, V.; Roseff, S. The D-chiro-inositol paradox in the ovary. Fertil. Steril. 2011, 95, 2515–2516. [Google Scholar] [CrossRef]
- Bevilacqua, A.; Carlomagno, G.; Gerli, S.; Montanino Oliva, M.; Devroey, P.; Lanzone, A.; Soulange, C.; Facchinetti, F.; Carlo Di Renzo, G.; Bizzarri, M.; et al. Results from the International Consensus Conference on myo-inositol and D-chiro-inositol in Obstetrics and Gynecology--assisted reproduction technology. Gynecol. Endocrinol. 2015, 31, 441–446. [Google Scholar] [CrossRef]
- Facchinetti, F.; Bizzarri, M.; Benvenga, S.; D’Anna, R.; Lanzone, A.; Soulage, C.; Di Renzo, G.C.; Hod, M.; Cavalli, P.; Chiu, T.T.; et al. Results from the International Consensus Conference on Myo-inositol and d-chiro-inositol in Obstetrics and Gynecology: The link between metabolic syndrome and PCOS. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 195, 72–76. [Google Scholar] [CrossRef]
- Brower, M.; Brennan, K.; Pall, M.; Azziz, R. The severity of menstrual dysfunction as a predictor of insulin resistance in PCOS. J. Clin. Endocrinol. Metab. 2013, 98, E1967–E1971. [Google Scholar] [CrossRef] [Green Version]
- Elkind-Hirsch, K.E.; Chappell, N.; Shaler, D.; Storment, J.; Bellanger, D. Liraglutide 3 mg on weight, body composition, and hormonal and metabolic parameters in women with obesity and polycystic ovary syndrome: A randomized placebo-controlled-phase 3 study. Fertil. Steril. 2022, 118, 371–381. [Google Scholar] [CrossRef]
- Nylander, M.; Frøssing, S.; Clausen, H.V.; Kistorp, C.; Faber, J.; Skouby, S.O. Effects of liraglutide on ovarian dysfunction in polycystic ovary syndrome: A randomized clinical trial. Reprod. Biomed. Online 2017, 35, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Jensterle Sever, M.; Kocjan, T.; Pfeifer, M.; Kravos, N.A.; Janez, A. Short-term combined treatment with liraglutide and metformin leads to significant weight loss in obese women with polycystic ovary syndrome and previous poor response to metformin. Eur. J. Endocrinol. 2014, 170, 451–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensterle, M.; Kravos, N.A.; Pfeifer, M.; Kocjan, T.; Janez, A. A 12-week treatment with the long-acting glucagon-like peptide 1 receptor agonist liraglutide leads to significant weight loss in a subset of obese women with newly diagnosed polycystic ovary syndrome. Hormones 2015, 14, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Ganie, M.A.; Khurana, M.L.; Nisar, S.; Shah, P.A.; Shah, Z.A.; Kulshrestha, B.; Gupta, N.; Zargar, M.A.; Wani, T.A.; Mudasir, S.; et al. Improved efficacy of low-dose spironolactone and metformin combination than either drug alone in the management of women with polycystic ovary syndrome (PCOS): A six-month, open-label randomized study. J. Clin. Endocrinol. Metab. 2013, 98, 3599–3607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elenis, E.; Desroziers, E.; Persson, S.; Sundström Poromaa, I.; Campbell, R.E. Early initiation of anti-androgen treatment is associated with increased probability of spontaneous conception leading to childbirth in women with polycystic ovary syndrome: A population-based multiregistry cohort study in Sweden. Hum. Reprod. 2021, 36, 1427–1435. [Google Scholar] [CrossRef] [PubMed]
- Wuttke, W.; Jarry, H.; Christoffel, V.; Spengler, B.; Seidlová-Wuttke, D. Chaste tree (Vitex agnus-castus)--pharmacology and clinical indications. Phytomedicine 2003, 10, 348–357. [Google Scholar] [CrossRef] [Green Version]
- Shahnazi, M.; Khalili, A.F.; Hamdi, K.; Ghahremaninasab, P. The Effects of Combined Low-Dose Oral Contraceptives and Vitex Agnus on the Improvement of Clinical and Paraclinical Parameters of Polycystic Ovarian Syndrome: A Triple-Blind, Randomized, Controlled Clinical Trial. Iran. Red Crescent Med. J. 2016, 18. [Google Scholar] [CrossRef]
- Arentz, S.; Abbott, J.A.; Smith, C.A.; Bensoussan, A. Herbal medicine for the management of polycystic ovary syndrome (PCOS) and associated oligo/amenorrhoea and hyperandrogenism; a review of the laboratory evidence for effects with corroborative clinical findings. BMC Complement. Altern. Med. 2014, 14, 511. [Google Scholar] [CrossRef]
| Author, Year | PCOS Criteria | Age (Years) | BMI (kg/m2) | Intervention | Sample Size (Trial/ Control Group) | Length (Months (mo) or Weeks (we)) | Outcome (Menstrual Cyclicity) | Other Outcomes |
|---|---|---|---|---|---|---|---|---|
| Allen, 2005 [9] | clinical/biochemical hyperandrogenism and oligomenorrhoea | 12–21 | 40.1 ± 2.1 (COC) 37.3 ± 1.3 (MET) | MET 1000 mg/d COC: 30 μg EE and norgestiate 0.25 mg | 16/15 | 6 mo | Regular menstrual cycle in both groups | Weight/BMI ↓ * Acne score ↓ * Testosterone ↓ * Hirsutism ↓ * |
| El Maghraby, 2015 [10] | Rotterdam criteria | 17.2 ± 2.0 | - | MET 1700 mg/d COC: 30 µg EE and 15 mg progestin Placebo | 40/40/39 | 24 mo | Regular menstrual cycle in MET/COC group | Weight/BMI (only MET group) ↓ * Hirsutism ↓ * |
| De Leo, 2006 [11] | Rotterdam criteria | 15–18 | 25.5–27.0 | MET 1700 mg/d | 18 | 12 mo | Regular menstrual cycle | Weight/BMI ↓ Androgen levels ↓ Hirsutism ↓ * |
| Hoeger, 2008 [12] | Menstrual irregularity (<eight menses in the preceding year) and clinical or biochemical evidence of hyperandrogenism | 12–18 | 34.3–37.8 | MET 1700 mg/d COC: 30 μg EE and desogestrel 0.15 mg lifestyle modification placebo | 16/21/21/19 | 8 mo | Regular menstrual cycle in COC group/no difference in other groups MET group 75% of cycles with ovulation | Weight/BMI ↓ * |
| Glueck, 2001 [13] | Oligo-/amenorrhoea + clinical or biochemical evidence of hyperandrogenism | 14–18.9 | 33.6 | MET 1500–2550 g/d | 11 | 9 mo | 91% regular menstrual cycle during MET | Weight ↓ |
| Glueck, 2006 [14] | Rotterdam criteria | <20 | 30.8 | MET 1500–2550 g/d + diet | 35 | 12 mo | 74% with regular menstrual cycle | Weight ↓ * Cholesterol ↓ * Triglyceride ↓ * HOMA↓ * Testosterone ↓ * |
| Glueck, 2009 [15] | Rotterdam criteria | 14–17 | 30.4 | MET 1500–2550 g/d + diet | 20 | 12 mo | 82% with regular menstrual cycle | Weight/BMI ↓ * Testosterone ↓ * Cholesterol ↓ * Triglyceride ↓ * HOMA↓ * |
| Al-Zubeidi and Klein, 2014 [16] | NIH criteria | 14–18 | 33.7 | MET 2000 mg/d COC: 30 μg EE and 1 mg norethindrone acetate | 10/12 | 6 mo | Number of cycles higher in COC group | Androgen (only COC group) ↓ * BMI/ weight ↓ * HOMA ↓ |
| Ladson, 2010 [17] | NIH/NICHD criteria | 16.1 ± 1.5 | 35.9–37.1 | MET 2000 mg/d ± lifestyle modification | 22 | 6 mo | No difference | Acne score ↓ * |
| Ibáñez, 2000 [18] | Hirsutism and/or biochemical hyperandrogenemia, and oligoamenorrhea + precocious pubarche | 13–20 | 21.9 ± 0.9 | MET 1275 mg/d | 8 | 6 mo | Regular menstrual in all patients, irregular within 3 months after withdrawal | Hirsutism ↓ * Testosterone levels ↓ * |
| Cirillo, 2019 [19] | Rotterdam criteria | 17.2 ± 0.7 | - | Alpha-Lipoic Acid (ALA) 400 mg and MYO 1000 mg/2×/d placebo | 23/21 | 3 mo | Improved menstrual frequency | hirsutism acne |
| Narsing, 2009 [20] | Clinical features of PCOS (Chronically anovulating, oligo-/amenorrhea, hyperandrogenism) | 15–25 | 29.5 ± 7.9 | Pioglitazone 30 mg/d | 22 | 6 mo | Improved menstrual frequency (91% with regular cycles at the end of therapy) | Body weight/BMI Insulin resistance ↓ * |
| Stabile, 2014 [21] | Rotterdam criteria | 19.4 ± 3.8 | 25.2 ± 5.1 | Pioglitazone 30 mg/d | 15/15 | 6 mo | Improved menstrual frequency | Body weight ↑ * Hirsutism and acne ↓ * Insulin resistance ↓ * |
| Tfayli, 2011 [22] | NIH criteria | 10–20 | 35.6 ± 1.5 | COC: 30 μg EE and drospirenone 3 mg ROS 4 mg/d | 23/23 | 6 mo | No changes in menstrual cyclicity | Body weight/BMI glucose tolerance status visceral adiposity ↓ * (With rosiglitazone) |
| De Leo, 1998 [23] | Clinical diagnosis of PCOS based on hyperandrogenism, chronic anovulation, polycystic ovaries by ultrasound | 16–19 | - | Flutamide 500 mg/d | 8 | 6 mo | Improved menstrual frequency | Hirsutism ↓ * Androgen levels↓ * Ovulatory cycles ↑ * Ovarian volume ↓ * |
| Ibáñez, 2000 [24] | Clinical features of PCOS (oligo-/amenorrhea, hyperandrogenism) | 16.8 ± 0.3 | - | Flutamide 250 mg/d | 18 | 18 mo | No changes in menstrual cyclicity | Hirsutism ↓ * BMI |
| Ganie, 2004 [25] | NIH criteria | 22.6 ± 5.0 | 26.8 ± 4.0 (SPIRO) 26.5 ± 5.6 (MET) | MET 1000 mg/d SPIRO 50 mg/d | 35/34 | 6 mo | Improved menstrual frequency | Hirsutism ↓ * Serum Testosteron Levels ↓ * |
| Ibáñez, 2020 [26] | Clinical diagnosis of PCOS based on hirsutism (score > 8 on modified Ferriman-Gallwey scale) and oligomenorrhea (menstrual intervals >45 days) | 15.9 ± 0.2 (EE and Levonorgestrel) 15.7 ± 0.2 (SPIOMET) | 24.9 ± 0.8 (EE and Levonorgestrel) 24.2 ± 0.7 (SPIOMET) | COC: 20 μg EE and 100 mg levonorgestrel SPIOMET: spironolactone 50 mg/d, pioglitazone 7.5 mg/d and metformin 850 mg/d | 31/31 | 12 mo of treatment and 12 mo follow-up without treatment | Improved menstrual frequency (with SPIOMET even in the follow-up year) | Ovulation rates ↑ * (with SPIOMET) Hepatic-visceral-fat-excess ↓ * (with SPIOMET) HOMA-IR ↓ * (with SPIOMET) |
| Amr, 2005 [27] | Rotterdam criteria | 14–17 | BMI SDS 1.9 ± 0.7 | Chromium (III) picolinate 1000 µg/d | 35 | 6 mo | Improved menstrual frequency | Acne and hirsutism Free testosterone levels ↓ * |
| Medication | Mechanism(s) of Action | Off-Label Reproductive Use | Dosage | Main Side Effects | Teratogenic Effects (FDA Pregnancy Category) | Contraindications | Treatment Costs (per Year) |
|---|---|---|---|---|---|---|---|
| Treatment | Mode of Action | Indication | Dose | Side Effects | Safety during Pregnancy | Contraindications | Costs |
| Metformin [28] | Enhancement of insulin sensitivity Inhibition of hepatic glucose production Increased glucose uptake in the muscle Hyperandrogenemia ↓ | Improvement of ovulation rates, menstrual regulation, hirsutism, weight loss | 850–2550 mg/d | Nausea/vomiting/abdominal pain/ diarrhea | Pregnancy category B | Severe liver/kidney/heart insufficiency | 58.4 Euro (1500 mg/d) |
| Myo-Inositol [29,30] | Increased MYO levels improve D-chiro-inositol/MYO ratio and reduce androgen production | Nutritional supplement | 2000 mg/d | No | Unknown | No data available | 197.1 Euro (2000 mg/d) |
| Glucagon-like peptide receptor agonists: exenatide, liraglutide [31,32] | Insulinotropic effects: hepatic glucagon release ↓, delays gastric emptying, intestinal motility ↓, glycemic control ↑, stimulates the hypothalamic satiety center, appetite↓, weight loss | Weight loss, menstrual regulation | Liraglutide: 1.2–3 mg/d Exenatide: 20 µg/d | Nausea/vomiting/abdominal pain/ diarrhea/injection site reaction/headache | Pregnancy category C | History of medullary thyroid carcinoma/ MEN 2/pancreatitis/renal impairment | LIRA 25,301.8 Euro (3 mg/d) Exenatide 91,417.9 Euro (20 µg/d) |
| Thiazolidinediones: rosiglitazone, pioglitazone [33] | PPAR-g receptor agonist: enhances cellular responsiveness to insulin, insulin-dependent glucose disposal ↑, glycaemic control ↑ | Improvement of ovulation rates, menstrual regulation | Pioglitazone: 30 mg/d rosiglitazone: 4–8 mg/d | Weight gain/ abnormal vision, respiratory infection, numbness | Pregnancy category C | Heart failure/liver failure/bladder cancer (pioglitazone) | Pioglitazone 164.25 Euro (30 mg/d) |
| Flutamide [34] | Competitively binds androgen receptors → inhibits androgen uptake and/or nuclear binding of androgen | Treatment of signs of hyperandrogenism (e.g., acne, hirsutism) | <250 mg/d | Breast swelling or tenderness/nausea/vomiting/abnormal liver function | Pregnancy category D | Liver and kidney problems/ heart disease | 262,8 Euro (250 mg/d) |
| Finasteride [35] | Inhibitor of 5-alpha reductase → antiandrogenic effects | Treatment of signs of hyperandrogenism (hirsutism) | 2.5–5 mg/d | Reduced libido/ depression/ headaches/ gastrointestinal disorders | Pregnancy category X | Pregnancy/ liver disease/ | 153.3 Euro (5 mg/d) |
| Spironolactone [25] | Aldosterone antagonist, diuretic with antiandrogen properties | Treatment of signs of hyperandrogenism (e.g., acne, hirsutism) | 50 mg/d | Gastrointestinal problems/ headache/ tenderness of the breasts/ menstrual disorders/dizziness | Pregnancy category C | Hyperkalemia/ chronic adrenal insufficiency | 315.35 Euro (50 mg/d) |
| Chromium (III) picolinate [36] | The exact mechanism of action is not known → improved insulin sensitivity | Menstrual regulation and ovulation rates | 200–1000 µg/d | No data available | Unknown | No data available | 30 Euro |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reiser, E.; Lanbach, J.; Böttcher, B.; Toth, B. Non-Hormonal Treatment Options for Regulation of Menstrual Cycle in Adolescents with PCOS. J. Clin. Med. 2023, 12, 67. https://doi.org/10.3390/jcm12010067
Reiser E, Lanbach J, Böttcher B, Toth B. Non-Hormonal Treatment Options for Regulation of Menstrual Cycle in Adolescents with PCOS. Journal of Clinical Medicine. 2023; 12(1):67. https://doi.org/10.3390/jcm12010067
Chicago/Turabian StyleReiser, Elisabeth, Julia Lanbach, Bettina Böttcher, and Bettina Toth. 2023. "Non-Hormonal Treatment Options for Regulation of Menstrual Cycle in Adolescents with PCOS" Journal of Clinical Medicine 12, no. 1: 67. https://doi.org/10.3390/jcm12010067
APA StyleReiser, E., Lanbach, J., Böttcher, B., & Toth, B. (2023). Non-Hormonal Treatment Options for Regulation of Menstrual Cycle in Adolescents with PCOS. Journal of Clinical Medicine, 12(1), 67. https://doi.org/10.3390/jcm12010067






