Effect of Body Mass Index Percentile on Clinical and Radiographic Outcome and Risk of Complications after Posterior Instrumented Fusion for Adolescent Idiopathic Scoliosis: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
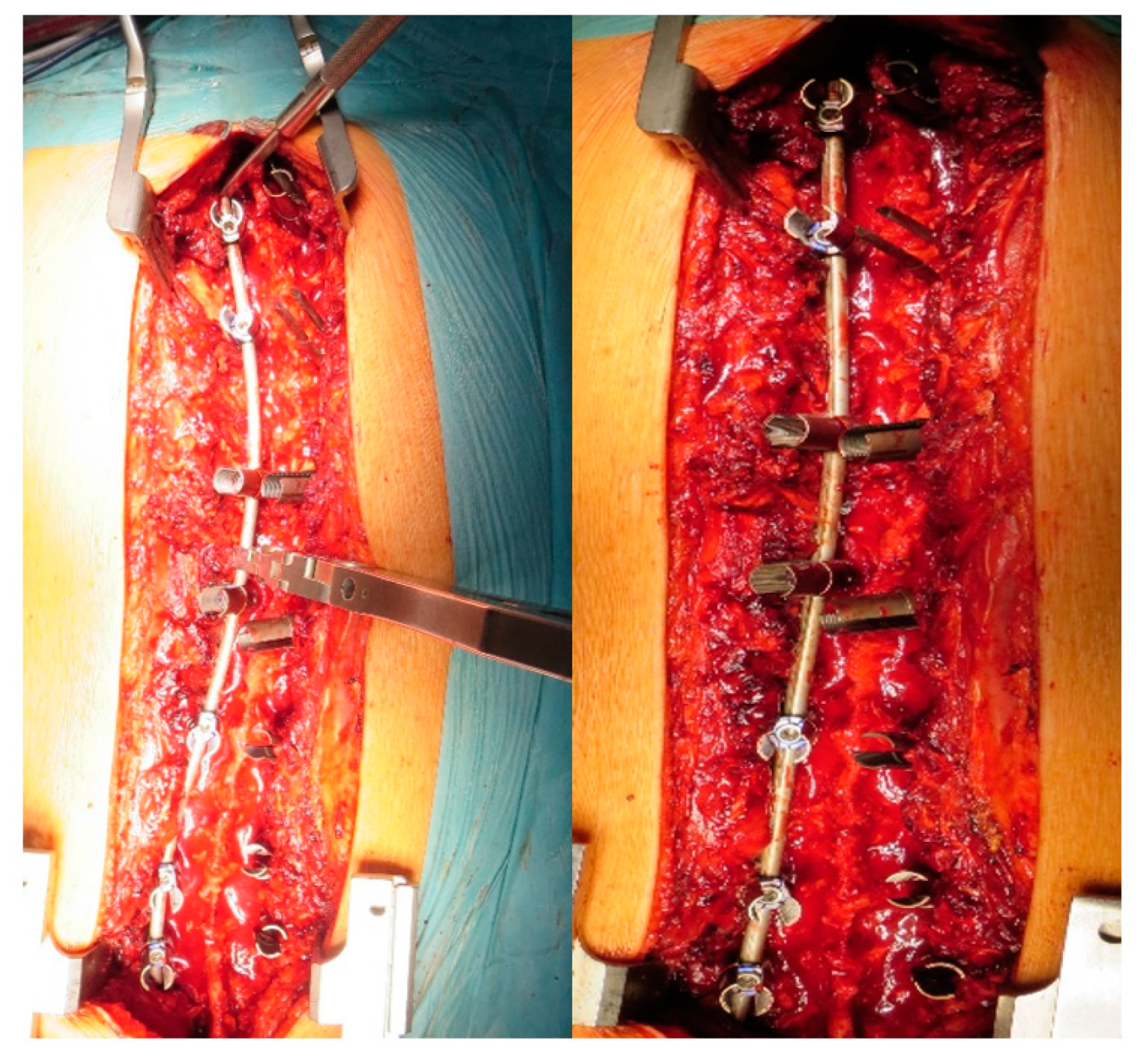
2.1. Surgical Technique
2.2. Statistical Analysis
3. Results
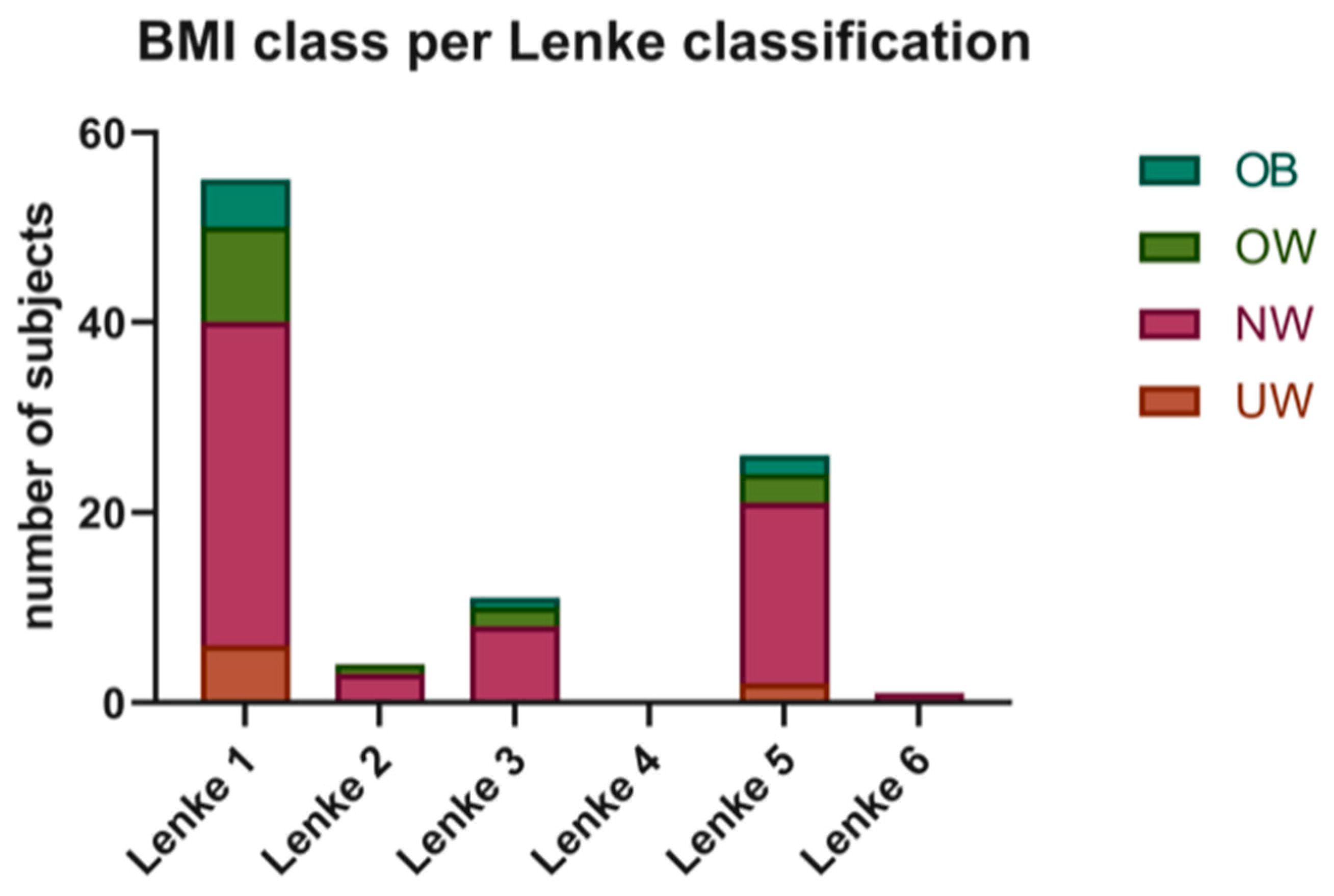
3.1. Patients’ Demographics
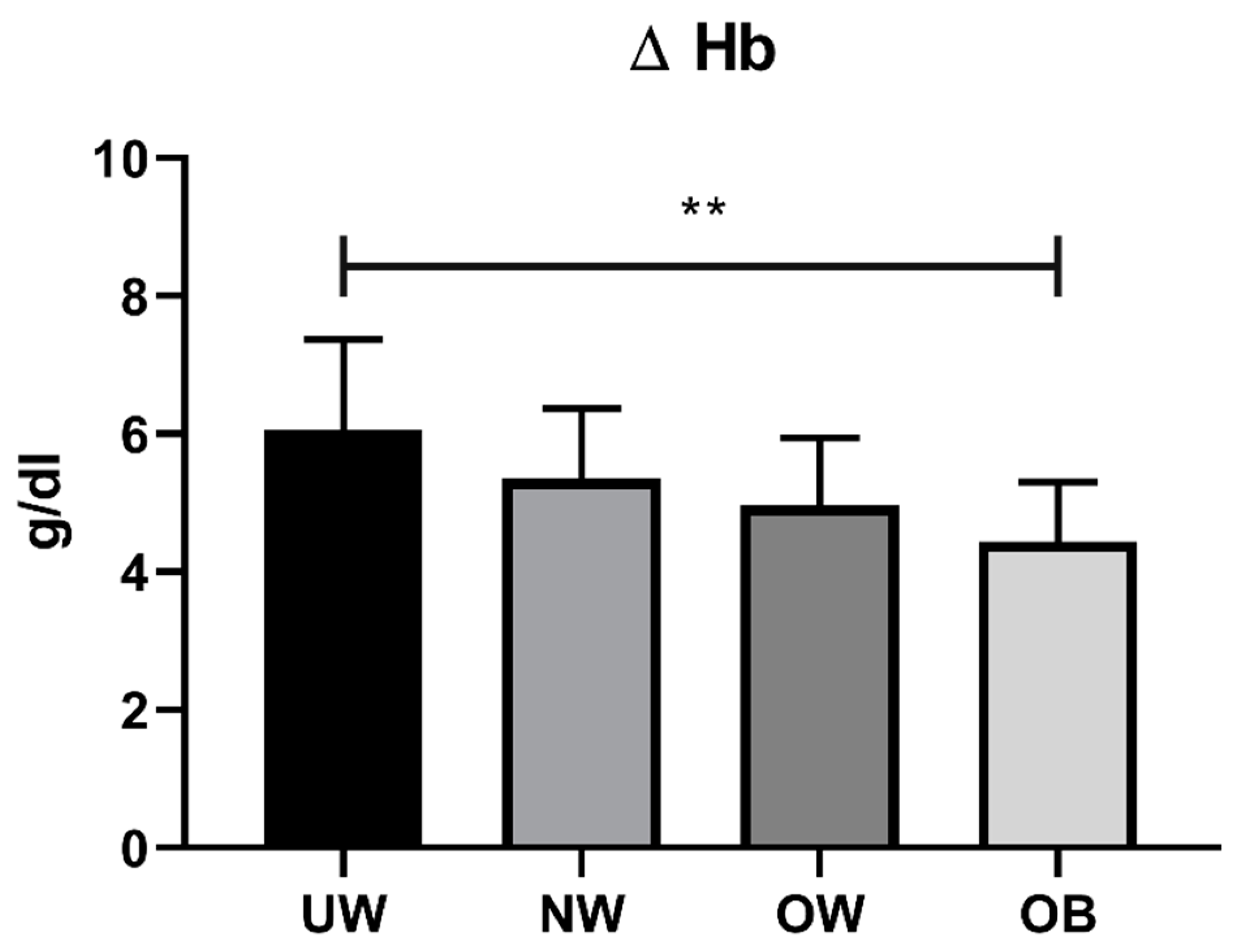
3.2. Surgical and Clinical Outcomes
3.3. Radiographic Evaluation
4. Discussion
5. Conclusions
- Higher surgical time.
- Higher intraoperative blood loss.
- Major hemoglobin decrease.
- Longer recovery time.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Konieczny, M.R.; Senyurt, H.; Krauspe, R. Epidemiology of adolescent idiopathic scoliosis. J. Child. Orthop. 2013, 7, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Tarrant, R.C.; Queally, J.M.; Moore, D.P.; Kiely, P.J. Prevalence and impact of low body mass index on outcomes in patients with adolescent idiopathic scoliosis: A systematic review. Eur. J. Clin. Nutr. 2018, 72, 1463–1484. [Google Scholar] [CrossRef] [PubMed]
- Ogilvie, J.W.; Braun, J.; Argyle, V.; Nelson, L.; Meade, M.; Ward, K. The search for idiopathic scoliosis gene. Spine (Phila PA 1976) 2006, 31, 679–681. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Guo, C.; Tang, M.; Liu, S.; Li, J.; Guo, Q.; Zhao, S. Prevalence of scoliosis among primary and middle school students in Mainland China: A systematic review and meta-analysis. Spine 2015, 40, 41–49. [Google Scholar] [CrossRef]
- Matusik, E.; Durmala, J.; Matusik, P. Association of body composition with curve severity in children and adolescents with idiopathic scoliosis (IS). Nutrients 2016, 28, 71. [Google Scholar] [CrossRef]
- Hardesty, C.K.; Poe-Kochert, C.; Son-Hing, J.P.; Thompson, G.H. Obesity negatively affects spinal surgery in idiopathic scoliosis. Clin. Orthop. Relat. Res. 2013, 471, 1230–1235. [Google Scholar] [CrossRef]
- Goodbody, C.M.; Asztalos, I.B.; Sankar, W.N.; Flynn, J.M. It’s not just the big kids: Both high and low BMI impact bracing success for adolescent idiopathic scoliosis. J. Child. Orthop. 2016, 10, 395–404. [Google Scholar] [CrossRef]
- Upasani, V.V.; Caltoum, C.; Petcharaporn, M.; Bastrom, T.; Pawelek, J.; Marks, M.; Betz, R.; Lenke, L.; Newton, P. Does obesity affect surgical outcomes in adolescent idiopathic scoliosis? Spine (Phila PA 1976) 2008, 33, 295–300. [Google Scholar] [CrossRef]
- Bjerke, B.T.; Saiyed, R.; Cheung, Z.B.; Uppstrom, T.J.; Shifflett, G.D.; Cunningham, M.E. Does adolescent obesity affect surgical presentation and radiographic outcome for patients with adolescent idiopathic scoliosis? J. Pediatr. Orthop. B 2016, 26, 53–58. [Google Scholar] [CrossRef]
- Farahani, F.; Riccio, A.I.; Ramo, B.A. Low BMI (<10th percentile) increases complications and readmissions after posterior spinal fusion in adolescent idiopathic scoliosis. Spine Deform. 2021, 9, 1533–1540. [Google Scholar]
- Laplaza, F.J.; Widman, R.F.; Fealy, S.; Moustafellos, E.; Illueca, M.; Burke, S.W.; Boachie-Adjei, O. Pancreatitis after surgery in adolescent idiopathic scoliosis: Incidence and risk factors. J. Pediatr. Orthop. 2002, 22, 80–83. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Prieto, D.; Sánchez-Soler, J.F.; Martínez-Llorens, J.; Mojal, S.; Bagó, J.; Cáceres, E.; Ramírez, M. Poor outcomes and satisfaction in adolescent idiopathic scoliosis surgery: The relevance of the body mass index and self-image. Eur. Spine J. 2015, 24, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.O.; Harrast, J.J.; Kuklo, T.R.; Polly, D.W.; Bridwell, K.H.; Diab, M.; Dormans, J.; Drummond, D.; Emans, J.; Johnston, C.; et al. The Spinal Appearance Questionnaire: Results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine(Phila PA 1976) 2007, 32, 2719–2722. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Betz, R.R.; Harms, J.; Bridwell, K.H.; Clements, D.H.; Lowe, T.G.; Blanke, K. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg. Am. 2001, 83, 1169–1181. [Google Scholar] [CrossRef]
- De la Garza Ramos, R.; Nakhla, J.; Nasser, R.; Schulz, J.F.; Purvis, T.E.; Sciubba, D.M.; Kinon, M.D.; Yassari, R. Effect of body mass index on surgical outcomes after posterior spinal fusion for adolescent idiopathic scoliosis. Neurosurg. Focus 2017, 43, E5. [Google Scholar] [CrossRef]
- Tarrant, R.C.; Lynch, S.; Sheeran, P.; O’Loughlin, P.F.; Harrington, M.; Moore, D.P.; Kiely, P.J. Low body mass index in adolescent idiopathic scoliosis: Relationship with pre- and postsurgical factors. Spine (Phila PA 1976) 2014, 39, 140–148. [Google Scholar] [CrossRef]
- Basques, B.A.; Bohl, D.D.; Golinvaux, N.S.; Smith, B.G.; Grauer, J.N. Patient factors are associated with poor short-term outcomes after posterior fusion for adolescent idiopathic scoliosis. Clin. Orthop. Relat. Res. 2015, 473, 286–294. [Google Scholar] [CrossRef]
- Sun, W.; Zhou, J.; Sun, M.; Qin, X.; Qiu, Y.; Zhu, Z.; Xu, L. Low body mass index can be predictive of bracing failure in patients with adolescent idiopathic scoliosis: A retrospective study. Eur. Spine J. 2017, 26, 1665–1669. [Google Scholar] [CrossRef]
- Goodbody, C.M.; Sankar, W.N.; Flynn, J.M. Presentation of Adolescent Idiopathic Scoliosis: The Bigger the Kid, the Bigger the Curve. J. Pediatr. Orthop. 2017, 37, 41–46. [Google Scholar] [CrossRef]
- Margalit, A.; McKean, G.; Constantine, A.; Thompson, C.B.; Lee, R.J.; Sponseller, P.D. Body Mass Hides the Curve: Thoracic Scoliometer Readings Vary by Body Mass Index Value. J. Pediatr. Orthop. 2017, 37, 255–260. [Google Scholar] [CrossRef]
- Wang, W.; Wang, Z.; Zhu, Z.; Zhu, F.; Qiu, Y. Body composition in males with adolescent idiopathic scoliosis: A case-control study with dual-energy X-ray absorptiometry. BMC Musculosk. Disord. 2016, 17, 107. [Google Scholar] [CrossRef] [PubMed]
- Briguglio, M.; Gianola, S.; Aguirre, M.-F.I.; Sirtori, P.; Perazzo, P.; Pennestri, F.; Bruno, M.B.; Sansone, V.; Banfi, G. Nutritional support for enhanced recovery programs in orthopedics: Future perspectives for implementing clinical practice. Nutr. Clin. Metab. 2019, 33, 190–198. [Google Scholar] [CrossRef]
- Stratton, R.J.; Hackston, A.; Longmore, D.; Dixon, R.; Price, S.; Stroud, M.; King, C.; Elia, M. Malnutrition in hospital outpatients and inpatients: Prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br. J. Nutr. 2004, 92, 799–808. [Google Scholar] [CrossRef] [PubMed]



| Underweight (BMI% ≤ 5) | Normal Weight (5 < BMI% ≤ 84) | Overweight (84 < BMI% < 95) | Obese (BMI% ≥ 95) | p-Value | |
|---|---|---|---|---|---|
| N patients | 8 | 55 | 14 | 10 | |
| Mean Age | 14.37 ± 2.07 | 14.84 ± 2.23 | 13.6 ± 1.65 | 15.5 ± 2.99 | 0.129 |
| Gender | F: 7, M: 1 | F: 42, M: 13 | F: 11, M: 3 | F: 8, M: 2 | 0.911 |
| Underweight (BMI% ≤ 5) | Normal Weight (5 < BMI% ≤ 84) | Overweight (84 < BMI% < 95) | Obese (BMI% ≥ 95) | p-Value | |
|---|---|---|---|---|---|
| Patients (N) | 8 | 55 | 14 | 10 | |
| Mean surgical time (minutes) | 244.62 ± 88.42 | 199.62 ± 42.23 | 195.64 ± 32.58 | 238.9 ± 34.85 | 0.008 |
| Intraoperative blood loss (mL) | 774.62 ± 365.79 | 627.35 ± 331.54 | 651.57 ± 244.77 | 765 ± 316.27 | 0.450 |
| Delta Hb (g/dL) | 6.05 ± 1.32 | 5.36 ± 1.01 | 4.96 ± 0.98 | 4.44 ± 0.86 | 0.007 |
| Complications (N) | 1 | 2 | 0 | 0 | 0.158 |
| Fused vertebra (N) | 11.5 (8–13) | 10 (7–24) | 11 (7–13) | 10.0 (6–13) | 0.225 |
| Risser (median, IQR) | 4 (2.75–4.25) | 4 (3–4) | 4 (2–4) | 4 (3–4) | 0.868 |
| SRS 22 Domain | Underweight (BMI% ≤ 5) | Normal Weight (6 < BMI% < 84) | Overweight (85 < BMI% < 94) | Obese (BMI% ≥ 95) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Last FU | Pre-op | Post-op | Last FU | Pre-op | Post-op | Last FU | Pre-op | Post-op | Last FU | |
| Pain | 22.2 ± 1.6 | 22.4 ± 0.5 | 23.4 ± 0.7 | 22.1 ± 1.6 | 22.6 ± 1.0 | 23.6 ± 0.8 ***### | 22.4 ± 1.7 | 22.4 ± 0.6 | 23.4 ± 0.6 *** | 22.2 ± 1.4 | 23.4 ± 0.7 | 24.1 ± 0.9 **## |
| Mental Health | 21.0 ± 1.8 | 23.2 ± 1.0 ** | 23.5 ± 0.9 ** | 21.8 ± 1.9 | 23.1 ± 1.1 *** | 23.6 ± 0.9 *** | 21.3 ± 1.5 | 23.1 ± 1.5 ** | 23.6 ± 0.9 *** | 21.8 ± 2.1 | 23.6 ± 1.1 * | 24.2 ± 0.8 ** |
| Self-Image | 9.7 ± 2.7 | 23.0 ± 1.8 *** | 23.6 ± 0.9 *** | 11.2 ± 2.3 | 23.1 ± 1.6 *** | 23.6 ± 1.1 *** | 10.3 ± 2.1 | 23.1 ± 1.7 *** | 23.6 ± 1.1 *** | 12.2 ± 2.6 | 23.1 ± 1.4 *** | 23.9 ± 0.7 *** |
| Function | 21.1 ± 2.3 | 22.2 ± 1.4 | 23.7 ± 0.9 * | 21.7 ± 1.6 | 22.7 ± 0.9 *** | 23.6 ± 0.8 ***### | 20.6 ± 1.6 | 22.9 ± 0.9 *** | 23.8 ± 0.9 *** | 21.3 ± 2.6 | 22.7 ± 0.8 | 24.3 ± 0.8 ** |
| Satisfaction | 8.6 ± 1.1 | 9.1 ± 0.6 | 8.9 ± 0.8 | 9.1 ± 0.7 | 9.0 ± 1.0 | 9.1 ± 0.7 | 9.0 ± 1.0 | 9.4 ± 0.7 | ||||
| Total | 3.7 ± 0.3 | 4.5 ± 0.2 *** | 4.7 ± 0.1 *** | 3.8 ± 0.3 | 4.6 ± 0.2 *** | 4.7 ± 0.1 ***## | 3.7 ± 0.2 | 4.6 ± 0.2 *** | 4.7 ± 0.1 *** | 3.9 ± 0.3 | 4.6 ± 0.2 *** | 4.8 ± 0.1 *** |
| Underweight (BMI% ≤ 5) | Normal Weight (6 < BMI% < 84) | Overweight (85 < BMI% < 94) | Obese (BMI% ≥ 95) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Last FU | Pre-op | Post-op | Last FU | Pre-op | Post-op | Last FU | Pre-op | Post-op | Last FU | |
| Thoracic Cobb angle (°) | 53.7 ± 15.4 | 21.1 ± 12.3 *** | 19.6 ± 10.3 *** | 53.2 ± 15.9 | 23.0 ± 11.9 *** | 22.35 ± 12.1 *** | 60.8 ± 16.0 | 23.9 ± 12.5 *** | 23.9 ± 13.1 *** | 51.7 ± 23.7 | 21.4 ± 11.7 ** | 20.9 ± 11.0 *** |
| Lumbar Cobb angle (°) | 39.2 ± 12.2 | 13.7 ± 8.6 *** | 13.1 ± 8.2 *** | 35.0 ± 14.4 | 11.9 ± 9.1 *** | 11.6 ± 8.7 *** | 45.0 ± 17.1 | 14.2 ± 8.2 *** | 12.7 ± 13.3 *** | 43.4 ± 13.4 | 12.6 ± 8.7 *** | 12.3 ± 7.7 *** |
| Thoracic Kyphosis (°) | 25.2 ± 14.3 | 23.1 ± 12.7 | 25.4 ± 12.8 | 26.4 ± 12.9 | 27.4 ± 9.2 | 28.1 ± 8.9 | 34.2 ± 19.7 | 27.7 ± 9.9 | 28.6 ± 10.3 | 34.8 ± 17.5 | 31.3 ± 17.5 | 32.2 ± 11.0 |
| Lumbar Lordosis (°) | 48.0 ± 17.9 | 45.7 ± 10.2 | 47.1 ± 9.8 | 55.1 ± 11.6 | 50.4 ± 8.5 * | 50.8 ± 8.2 | 53.0 ± 10.3 | 47.8 ± 13.2 | 49.5 ± 15.5 | 61.2 ± 16.8 | 48.6 ± 13.9 | 48.6 ± 14.4 |
| % Correction | Underweight (BMI% ≤ 5) | Normal Weight (5 < BMI% ≤ 84) | Overweight (84 < BMI% < 95) | Obese (BMI% ≥ 95) | ||||
|---|---|---|---|---|---|---|---|---|
| Post-op vs. Baseline | Last FU vs. Post-op | Post-op vs. Baseline | Last FU vs. Post-op | Post-op vs. Baseline | Last FU vs. Post-op | Post-op vs. Baseline | Last FU vs. Post-op | |
| Thoracic Cobb Angle (%) | −62.0 (−78.0, −51.2) | 0.0 (−1.9, 0.0) | −58.3 (−68.7, −51.1) | 0.0 (−4.5, 0.0) | −64.6 (−71.0, −53.6) | 0.0 (−2.6, 2.7) | −55.5 (−71.5, −49.2) | 0.0 (−3.7, 0.0) |
| Lumbar Cobb Angle (%) | −65.7 (−75.1, −52.3) | 0.0 (0.0, 0.0) | −72.1 (−77.7, −55.6) | 0.0 (0.0, 0.0) | −74.4 (−81.7, −50.4) | −3.1 (−20.8, 0.0) † | −59.7 (−82.4, −57.9) | 0.0 (−10.3, 0.0) |
| Thoracic Kyphosis (%) | −10.2 (−31.8, +10.0) | +5.5 (0.0, +14.4) | +6.2 (−12.6, +30.9) | 0.0 (0.0, 0.0) | −22.5 (−36.5, +8.8) † | 0.0 (0.0, 0.0) | −14.4 (−25.5, −0.7) | 0.0 (0.0, +3.7) |
| Lumbar Lordosis (%) | −5.3 (−11.7, +3.4) | 0.0 (0.0, +2.9) | −9.4 (−16.7, +4.7) | 0.0 (0.0, 0.0) | −2.2 (−27.9, +9.1) | 0.0 (0.0, +1.3) | −15.8 (−23.2, −10.3) | 0.0 (−2.4, 0.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scaramuzzo, L.; Giudici, F.; Barone, G.; Pironti, P.; Viganò, M.; Ravier, D.; Minoia, L.; Archetti, M.; Zagra, A. Effect of Body Mass Index Percentile on Clinical and Radiographic Outcome and Risk of Complications after Posterior Instrumented Fusion for Adolescent Idiopathic Scoliosis: A Retrospective Cohort Study. J. Clin. Med. 2023, 12, 76. https://doi.org/10.3390/jcm12010076
Scaramuzzo L, Giudici F, Barone G, Pironti P, Viganò M, Ravier D, Minoia L, Archetti M, Zagra A. Effect of Body Mass Index Percentile on Clinical and Radiographic Outcome and Risk of Complications after Posterior Instrumented Fusion for Adolescent Idiopathic Scoliosis: A Retrospective Cohort Study. Journal of Clinical Medicine. 2023; 12(1):76. https://doi.org/10.3390/jcm12010076
Chicago/Turabian StyleScaramuzzo, Laura, Fabrizio Giudici, Giuseppe Barone, Pierluigi Pironti, Marco Viganò, Domenico Ravier, Leone Minoia, Marino Archetti, and Antonino Zagra. 2023. "Effect of Body Mass Index Percentile on Clinical and Radiographic Outcome and Risk of Complications after Posterior Instrumented Fusion for Adolescent Idiopathic Scoliosis: A Retrospective Cohort Study" Journal of Clinical Medicine 12, no. 1: 76. https://doi.org/10.3390/jcm12010076
APA StyleScaramuzzo, L., Giudici, F., Barone, G., Pironti, P., Viganò, M., Ravier, D., Minoia, L., Archetti, M., & Zagra, A. (2023). Effect of Body Mass Index Percentile on Clinical and Radiographic Outcome and Risk of Complications after Posterior Instrumented Fusion for Adolescent Idiopathic Scoliosis: A Retrospective Cohort Study. Journal of Clinical Medicine, 12(1), 76. https://doi.org/10.3390/jcm12010076







